Back to Journals » International Journal of General Medicine » Volume 15
The Vicissitude of Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Order During COVID-19 Pandemic in Japan – A Retrospective Cohort Study
Authors Morishita N, Iwata K
Received 15 February 2022
Accepted for publication 6 April 2022
Published 11 April 2022 Volume 2022:15 Pages 3943—3950
DOI https://doi.org/10.2147/IJGM.S361582
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Naomi Morishita,1 Kentaro Iwata2
1Division of Nursing, Hyogo Prefectural Kakogawa Medical Center, Kakogawa, Hyogo, Japan; 2Division of Infectious Diseases Therapeutics, Kobe University Graduate School of Medicine, Kobe, Hyogo, Japan
Correspondence: Kentaro Iwata, Division of Infectious Diseases Therapeutics, Kobe University Graduate School of Medicine, 7-5-2 Kusunokicho, Chuoku, Kobe, Hyogo, 650-0017, Japan, Tel +81-78-382-6296, Fax +81-78-382-6298, Email [email protected]
Introduction: Japan went through five surges of coronavirus disease 2019 (COVID-19) or “waves”. However, their impacts on the do not attempt cardiopulmonary resuscitation (DNACPR) of the patients are not known.
Methods: A retrospective single-center cohort study was conducted for all hospitalized patients with COVID-19 from March 1, 2020, to September 30, 2021. Their code status was retrieved, and its association with the waves and other parameters, such as in-hospital mortality, was investigated. The relationship between DNACPR status and each wave was examined, as well as the effect on in-hospital mortality.
Results: A total of 1153 patients were hospitalized with the diagnosis of COVID-19 during the study period. On admission, 117 patients (10.1%) had DNACPR orders, 373 patients (32.4%) were on full code, 45 patients (3.9%) stated that they cannot decide code status. DNACPR rate appeared to increase at the summit of each wave. Subsequently, 160 patients (13.9%) became DNACPR status, 385 patients (33.4%) became full code, and 12 patients (1.0%) stated that they remained unable to decide code status. There was no association between DNACPR status and each wave, and DNACPR status was not associated with higher mortality (P = 0.87), both by logistic regression analysis.
Conclusion: DNACPR status among hospitalized COVID-19 patients appeared to have changed over multiple waves in Japan, but it is more likely due to the change of the patients’ demographics, particularly their age. DNACPR was common among the elderly, but it was not independently associated with higher mortality.
Keywords: COVID-19, do not attempt cardiopulmonary resuscitation, DNACPR, Japan
Corrigendum for this paper has been published
Introduction
Coronavirus diseases 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has posed a significant threat to all countries on earth. As of this writing, Japan has gone through five surges of COVID-19 outbreak. These surges were called “waves”, or “Nami” in Japanese, and each wave has jeopardized the healthcare system of Japan. Even though the number of infected persons and deaths caused by COVID-19 in Japan has been relatively low, with a cumulative number of cases of 1,723,413 and cumulative deaths of 18,359 as of December 7, 2021 (https://corona.go.jp/en/dashboard/), the large size of the waves did not allow all sick people to be hospitalized, particularly during the latest three waves.1–3
Advance care planning, or ACP, is not commonplace in Japan. According to a survey, only 28.7% of physicians and 27.6% of nurses engage their patients in ACP.4 There are no universally accepted protocols, laws, or evidence-based guidelines in regard to the procedure of ascertaining do not attempt cardiopulmonary resuscitation (DNACPR) in Japan.5 Commonly, DNACPR is provided by the patient to the treating physician, sometimes with an aid of other healthcare personnel such as nurses, and it can also be given by the family member, but there is no standard process accepted to all for the reason described above. Therefore, when acutely ill patients are hospitalized, early decision-making regarding whether or not to have DNACPR order can be difficult.
This is particularly true to COVID-19 patients since patients are placed in isolation, communication between healthcare workers and the patients/family members can be more difficult than one with the other diseases, and fear or panic to the novel disease among patients and family, even among healthcare workers, might make it even more challenging.
With each wave in Japan, the treatment measures have changed significantly, and so were the cognition of the patients and the healthcare workers towards COVID-19. We hypothesized that this could influence and change the way DNACPR decision-making is taken, and therefore conducted a retrospective cohort study to see the change of DNACPR over five waves of COVID-19 surges.
Methods
Study Design and Participants
All patients admitted to Kakogawa Medical Center, Kakogawa, Japan, from March 1, 2020, to September 30, 2021, were included in the analysis. All were discharged, alive or dead, by the time the current study was conducted, and we were able to measure in-hospital mortality as a variable in all the patients. Kakogawa Medical Center is located in Hyogo prefecture, Japan, and it has taken care of the largest number of COVID-19 patients during the pandemic in the prefecture. It has general medical wards for mild-to-moderate COVID-19, and also an intensive care unit (ICU) to take care of severely ill patients, with the availability of advanced care such as mechanical ventilation, vasopressors, and extracorporeal membrane oxygenation, or ECMO.
The status of DNACPR on admission and during the hospitalization was derived from the clinical chart review. Age, sex, and hospital mortality were also derived from the same source.
There is no official definition of so-called “waves”, surges of COVID-19 outbreaks in Japan. In fact, some waves did not come to end and continuously led to the other. We therefore arbitrarily defined these waves as a monthly increase of newly admitted patients in our cohort to the lowest number of patients monthly before the advent of the next wave. With this definition, the first wave was defined as the period from March to June 2020, the second as the period from July to September 2020, the third as the period from October 2020 to February 2021, the fourth from March to June 2021, and the fifth from July to September 2021. The relationship between each wave and DNACPR status, both on admission and afterward, was investigated, and we also evaluated the relationship between DNACPR status and in-hospital mortality.
Statistical Analysis
Statistical analysis included Fisher-exact test for comparison of two categorical variables and Fisher-exact test with Benjamini-Hochberg multiple-testing correction for comparisons of categorical variables ranging from the five waves. For continuous variables, Kruskal–Wallis rank sum test was conducted as a non-parametric test, followed by Steel-Dwass test. Logistic regression analysis was conducted for the association between DNACPR status and in-hospital mortality.
Ethical Consideration
The Ethics Committee of Kakogawa Medical Center approved the current study and accepted a waiver to the requirement to obtain individual informed consent, given the retrospective nature of the current study, with no intervention provided to the patients, the confidentiality of the patients remained kept, and we were compliant with the Declaration of Helsinki.
Results
A total of 1153 patients were hospitalized with the diagnosis of COVID-19 during the study period. The characteristics of the patients at each wave are provided in Table 1. Monthly admitted patients are shown in Figure 1., and the age distribution during the study period is provided in Figure 2.
 |
Table 1 The Characteristics of the Patients at Each Wave |
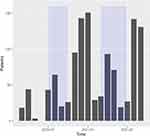 |
Figure 1 A histogram of COVID-19 patients admitted to Kakogawa Medical Center. The rectangular changes of background color suggest each “wave”. Abbreviation: COVID-19, coronavirus disease 2019. |
The mean age of the cohort was 59.4 years old (range 10–101), and 39.3% were female (Table 1). There were significant differences in age distribution among wave groups by Kruskal–Wallis rank sum test (P < 0.0001). Subsequent Steel-Dwass test found significant differences between the waves (Figure 2).
On admission, 117 patients (10.1%) had DNACPR order, 373 patients (32.4%) were on full code, 45 patients (3.9%) stated that they cannot decide code status, and the remaining 617 patients (53.5%) did not have code status documented. Distributions of the number of DNACPR per admitted patients monthly over time are shown in Figure 3A and B. DNACPR per patient appeared to increase at the summit of each wave.
During the hospitalization, some changed their code status, and 160 patients (13.9) became DNACPR, 385 patients (33.4%) became full code, 12 patients (1.0%) stated that they still could not decide their code status, and the remaining 594 patients (51.5%) did not have code status documented.
For DNACPR status among the code status is known upon admission (either DNACPR or full code), there was a significant difference among the waves (P < 0.0001). Fisher-exact test with Benjamini-Hochberg multiple-testing correction found that there was a significant difference in DNACPR status between specific waves (Figure 3A).
For DNACPR status among the code status is known after admission, there were significant differences among the waves (P < 0.0001). Fisher-exact test with Benjamini-Hochberg multiple-testing correction found that there was a significant difference in DNAR between waves (Figure 3B).
By age, those who have DNACPR orders and those who cannot decide their code status tended to be older (Figure 4A and B).
 |
Figure 4 (A) A histogram of code status on admission by age. (B) A histogram of code status after admission by age. Abbreviation: DNACPR, do not attempt cardiopulmonary resuscitation. |
However, logistic regression analysis using age among those code status was known revealed that there was no relationship between DNACPR status after the admission and each wave (Table 2).
 |
Table 2 Logistic Regression Analysis for DNACPR After Admission Among Those Patients Whose Code Status Were Known |
Overall, 93 patients died during the hospitalization (8.1%). The mean age of those who died was older than those who survived (76.5 (range 46–98) vs 57.9 (range 10–101) years old, P < -0.0001). Males were more likely to die than females (mortality 9.6% vs 5.7%, P = 0.02).
There was a significant difference in mortality among the waves (P < 0.0001). Fisher-exact test with Benjamini-Hochberg multiple-testing correction found that there was a significant difference in mortality between the first and fifth waves, the third wave and the fourth wave, and the fourth wave and the fifth wave (P < 0.0001 for all), but the other combinations did not have significant differences.
Among those who had confirmed code status after admission, the mortality was higher among those who were given DNACPR orders than those on full code (52.7% vs 23.8%, P < 0.0001). However, logistic regression analysis using age, sex, and the waves revealed that having DNACPR was not independently associated with higher mortality (Table 3, P = 0.87), with male sex, age, and the first wave was also independently associated with higher mortality.
 |
Table 3 Logistic Regression Analysis for Mortality Among Those Patients Whose Code Status Were Known |
Discussion
It appeared that there were significant differences in DNACPR status between and within the waves. The patients during the third and the fourth wave were more likely to be given DNACPR status, and the patients during the fifth wave were less likely to receive DNACPR orders. When the wave reaches its summit, the proportion of the patients with DNACPR status also increased, whereas it was less likely to have DNACPR during the time between the waves (Figure 3A and B). In addition, elderly patients tended to have more DNACPR status than younger patients (Figure 4A and B).
It is not surprising to see more DNACPR among the elderly than young, but how do we explain the higher DNACPR during the summit of each wave? It is possible that the hospital was not able to admit all patients with COVID-19 who needed hospital-level care during the peak of each wave, especially during the third and the fourth wave. Those who could be admitted during the time might have been those who were the sickest, while the patients who were relatively well could have ended up either staying home or being admitted to hospitals without ICU. The increased number of the sickest could have led to a higher DNACPR proportion among the admitted. It is also possible that the ICU was full or nearly full during the summit of each wave, and people could be admitted only if they declared DNACPR since there was no capability to provide intensive care such as mechanical ventilation. We did not investigate the reason why the DNACPR rate changed over time within the waves, and further studies will be needed to explain the phenomenon better.
Although DNACPR status appeared different among the waves, logistic regression analysis adjusting the age found there was no difference in DNACPR status rate among the waves. Since the ages of the third and the fourth wave were higher than the other waves, so was the DNACPR status. The age of the fifth wave was lower than the preceding two waves, most likely due to the widespread vaccination program among the elderly in Japan by the time the fifth wave arrived.6
The patients with DNACPR status appeared to die more than those who were full code, but the logistic regression analysis showed that there was no increased mortality depending on DNACPR status after adjusting age, sex, and the waves. Older age and male sex are known to be risk factors associated with higher mortality among those with COVID-19, both in Japan and other countries,7–12 and our cohort was similar to those patients reported previously.
A previous study conducted at hospitals in New Jersey, USA, showed the DNACPR status was independently associated with higher mortality among COVID-19 patients.13 We are not sure why the discrepancy occurred between the two studies, but it may be related to the differences in how DNACPR order was given in the USA and Japan. As stated above, ACP is not commonplace in Japan, the majority of our cohort did not have code status during the hospitalization, and 3.9% of the patients were not able to provide code status preference on admission in our cohort. In another study, Asian ethnicity was associated with the reduced recording of early DNACPR among COVID-19 patients in the United Kingdom.14 The attitude among healthcare workers for DNACPR of patients might also be different among different countries, ethnicities, or cultures, and their attitudes towards the code status might influence the preference of the patients. Further studies to identify the reasons for the difference will also be necessary.
In addition, it is suggested that cardiopulmonary resuscitation (CPR) could be delayed to COVID-19 patients, partly due to the status of strict isolation of the patients.15 Lower survival after CPR could potentially influence the impact of DNACPR on the outcome, by lowering the survival of those with full code.
Apart from DNACPR, our study found that the first wave was associated with higher mortality, and the latter wave was associated with lower mortality than the first. This can be explained by the advance in treatment and prevention, particularly the use of dexamethasone and vaccinations to decrease mortality.16,17
Our study has inherent limitations. First, it is a single-center study conducted in Japan, and our findings might not apply to the other settings. Second, because of the retrospective nature of our study, other confounding factors not measured in our study could have influenced our findings. Third, even though we were able to identify several characteristics of DNACPR status among hospitalized COVID-19 patients in Japan, we were not able to delineate the reasons for these findings. Further studies will be needed to investigate the remaining issues regarding DNACPR status for COVID-19 patients.
Conclusion
Our retrospective study found that DNACPR status among hospitalized COVID-19 patients appeared to have changed over multiple waves in Japan, but it is more likely due to the change of the patients’ demographics, particularly their age. DNACPR rate appeared higher at the summit of each wave. DNACPR was common among the elderly, but it was not independently associated with higher mortality.
Data Sharing Statement
Data from our cohort study can be available to those who requested it for sound reasons.
Ethics Approval and Informed Consent
The Ethics Committee of Kakogawa Medical Center approved the current study and accepted a waiver to the requirement to obtain individual informed consent, given the retrospective nature of the current study
Consent for Publication
All authors consented to publish any content of the current manuscript.
Acknowledgments
We are indebted to Dr. Chisato Miyakoshi for valuable suggestions and methodological insights.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study is self-funded.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Osaki T. Access denied: virus third wave forces hand of Japan’s medical system [Internet]. The Japan Times; 2021 [
2. At-home care for infections proved nightmare in fourth wave | the Asahi Shimbun: breaking News, Japan News and Analysis [Internet]. The Asahi Shimbun. [
3. COVID-19 “5th wave” engulfs hospitals in Tokyo area | the Asahi Shimbun: breaking News, Japan News and Analysis [Internet]. The Asahi Shimbun. [
4. Inoue M, Hanari K, Hamano J, Gallagher J, Tamiya N. Current engagement in advance care planning in japan and its associated factors. Gerontol Geriatr Med. 2019;5:2333721419892694. doi:10.1177/2333721419892694
5. Nakagawa Y, Inokuchi S, Kobayashi N, Ohkubo Y. Do not attempt resuscitation order in Japan. Acute Med Surg. 2017;4:286–292. doi:10.1002/ams2.271
6. Severe COVID-19 cases increase among middle-aged amid 5th wave in Tokyo. Mainichi Daily News [Internet]; 2021 [
7. Tsuchihashi Y, Arima Y, Takahashi T, et al. Clinical characteristics and risk factors for severe outcomes of novel coronavirus infection, January-March 2020, Japan. J Epidemiol. 2021;31:487–494. doi:10.2188/jea.JE20200519
8. Suleyman G, Fadel RA, Malette KM, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan detroit. JAMA Netw Open. 2020;3:e2012270. doi:10.1001/jamanetworkopen.2020.12270
9. Bonnet G, Weizman O, Trimaille A, et al. Characteristics and outcomes of patients hospitalized for COVID-19 in France: the critical COVID-19 France (CCF) study. Arch Cardiovasc Dis. 2021;114:352–363. doi:10.1016/j.acvd.2021.01.003
10. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi:10.1001/jamainternmed.2020.0994
11. Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345–1355. doi:10.1001/jamainternmed.2020.3539
12. da Silva PV, de Oliveira SB, Escalante JJC, et al. Risk factors for death among 120,804 hospitalized patients with confirmed COVID-19 in São Paulo, Brazil. Am J Trop Med Hyg;2021. tpmd201598. doi:10.4269/ajtmh.20-1598
13. Alhatem A, Spruijt O, Heller DS, Chokshi RJ, Schwartz RA, Lambert WC. “Do-not-resuscitate (DNR)” status determines mortality in patients with COVID-19. Clin Dermatol. 2021;39:510–516. doi:10.1016/j.clindermatol.2020.11.013
14. Sutton L, Goodacre S, Thomas B, Connelly S. Do not attempt cardiopulmonary resuscitation (DNACPR) decisions in people admitted with suspected COVID-19: secondary analysis of the PRIEST observational cohort study. Resuscitation. 2021;164:130–138. doi:10.1016/j.resuscitation.2021.04.028
15. Modes ME, Lee RY, Curtis JR. Outcomes of cardiopulmonary resuscitation in patients with COVID-19—limited data, but further reason for action. JAMA Intern Med. 2021;181:281–282. doi:10.1001/jamainternmed.2020.4779
16. Dhasmana DJ. Dexamethasone in hospitalized patients with Covid-19. New Engl J Med. 2021;384:693–704. doi:10.1056/NEJMoa2021436
17. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373:n1088. doi:10.1136/bmj.n1088
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


