Back to Journals » Open Access Emergency Medicine » Volume 15
The Utility of Transvaginal Ultrasound After Intrauterine Pregnancy Identification on Transabdominal Ultrasound in Emergency Department Patients
Authors Thom C, Kongkatong M, Moak J
Received 14 March 2023
Accepted for publication 20 May 2023
Published 29 May 2023 Volume 2023:15 Pages 207—216
DOI https://doi.org/10.2147/OAEM.S409920
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Christopher Thom, Matthew Kongkatong, James Moak
Emergency Medicine, University of Virginia Health System, Charlottesville, VA, USA
Correspondence: Christopher Thom, Email [email protected]
Introduction: Ultrasonography has an important role in the evaluation of Emergency Department (ED) patients presenting with early pregnancy complaints. Both transabdominal (TAUS) and transvaginal ultrasound (TVUS) can be utilized. While TVUS generally allows for greater detail, it is unclear how much added benefit exists in performing TVUS once an intrauterine pregnancy (IUP) has been identified on TAUS.
Methods: This was a retrospective study utilizing Radiology Department ultrasound examinations obtained in first trimester pregnancy ED patients during a consecutive four month period in 2019. Studies wherein both TAUS and TVUS were both performed were included. Two ED physicians with specialized training in point of care ultrasound reviewed only the TAUS images from these studies. Their findings were compared to the Radiologist interpretation, which was inclusive of both TAUS and TVUS components of the study.
Results: 108 studies met inclusion criteria. Amongst these, 82 had IUP’s identified on the radiologist report. 69 studies had an IUP identified by ED physician review of the TAUS images, with 1 false positive. Each case of intrauterine fetal demise (IUFD) was identified on ED physician review of TAUS. Two ectopic pregnancies were present, neither of which was mistaken for IUP on ED physician TAUS review. There were 15 studies with subchorionic hemorrhage and 3 studies with an ovarian cyst noted on the radiologist report.
Conclusion: Following the identification of an IUP on TAUS, the added diagnostic value of TVUS amongst this cohort of ED patients was low. Given the added time and cost of TVUS, selective instead of routine usage should be encouraged.
Keywords: ectopic pregnancy, ultrasound, threatened miscarriage, spontaneous miscarriage, yolk sac, subchorionic hemorrhage
Plain Language Summary
Both transvaginal (TVUS) and transabdominal (TAUS) ultrasound are used in the evaluation of first trimester pregnancy complaints amongst Emergency Department (ED) patients. TVUS provides higher resolution and more detail than TAUS, but involves increased cost and patient discomfort. Guidelines are not definitive on the question of whether TVUS is needed in cases where an intrauterine pregnancy (IUP) can be seen on TAUS. Our study explored the value of routine TVUS amongst the patient cohort where an intrauterine pregnancy (IUP) is identified on TAUS. In this cohort, our study found the value of routine TVUS to be low.
Introduction
Ultrasonography plays an important role in the diagnostic evaluation of ED patients presenting with early pregnancy complaints. The American College of Emergency Physicians (ACEP), American College of Obstetrics and Gynecology (ACOG), American Academy of Family Practitioners (AAFP), and the American College of Radiology (ACR) all recommend the utilization of ultrasound for patients with early pregnancy who present with abdominal pain or pelvic bleeding.1–4 These patients commonly present to Emergency Departments for care and the ultrasound they receive can either be a point of care ultrasound performed at the bedside by the ED physician or a comprehensive ultrasound in the Department of Radiology.3 Pregnancy ultrasound is one of the core modalities of emergency ultrasound, as noted in the ACEP clinical ultrasound guidelines.5
Early pregnancy can be evaluated by both transabdominal (TAUS) and transvaginal ultrasound (TVUS). Transvaginal ultrasound has several advantages over transabdominal ultrasound, which result from the usage of a higher frequency transducer and the positioning of the probe closer to the cervix and uterus.2 TVUS has been well established as a superior test for the evaluation of early pregnancy and related complaints.6,7 It is more sensitive for the identification of intrauterine pregnancy and can more readily identify ectopic pregnancies and adnexal structures.8,9 Given this, transvaginal ultrasound is often favored as the diagnostic imaging choice for evaluation of early pregnancy patients, often in concert with transabdominal imaging.2,10 However, transvaginal ultrasound does carry significant drawbacks as well, which include increased cost and the need for high level disinfection.11,12 There is also the potential for increased patient discomfort based on the invasive nature of transvaginal ultrasound, as compared with transabdominal ultrasound.
While TVUS provides higher overall diagnostic value as compared to TAUS, it is not always felt to be necessary in the evaluation of ED patients with early pregnancy related complaints. Specifically, when one identifies an IUP on TAUS, the utility of a subsequent TVUS is reduced, as the rate of missing an ectopic pregnancy at that juncture would be low. Indeed, the rate of heterotopic pregnancy is felt to occur in an estimated 1:10,000 pregnancies.13 Given this, an evaluation of the pregnancy and adnexa with TVUS might be of limited diagnostic benefit once an IUP has been identified on TAUS. Importantly, patients on fertility treatments are at higher risk of heterotopic pregnancy,14 making the evaluation of the adnexa more important, even in those cases where intrauterine pregnancy has been identified on transabdominal imaging.
Congruent with this, ACOG notes that the first trimester ultrasound examination can be performed transabdominally or transvaginally and that a transvaginal scan is recommended if the transabdominal examination is inconclusive.1 ACEP and AAFP do not provide a specific recommendation on whether TVUS is still indicated if TAUS definitively identifies an IUP. ACR notes that TAUS only may be adequate in some patients but notes that this should involve the visualization of the IUP and normal adnexa. They further note that the adnexa should be routinely evaluated.2 The Society of Radiologists in Ultrasound note that ultrasound imaging in early pregnancy should be primarily transvaginal, with TAUS “used for adnexal masses high in the pelvis and documentation of the amount of free fluid”.10 Importantly, detailed evidence regarding the exact utility of employing transvaginal ultrasound following the identification of an intrauterine pregnancy on TAUS in ED patients is lacking. Such evidence would have potential implications for several stakeholders that routinely perform first trimester ultrasound in symptomatic patients. In the current study, we sought to investigate the findings that are identified in the radiologist interpretation report, which is inclusive of both transabdominal and transvaginal ultrasonography, in cases where an ED physician identifies an IUP on the transabdominal images from those studies. The objective is to ascertain the perceived value of both TVUS and TAUS imaging in cases where an IUP is evident on TAUS. We evaluated for rates of ectopic pregnancy, subchorionic hemorrhage, intrauterine fetal demise, significant ovarian or adnexal masses, and any other significant findings that were identified on the final radiology report in cases where the ED physician identified an IUP on TAUS.
Materials and Methods
Design and Setting
This was a cross-sectional diagnostic study of previously obtained first trimester pregnancy ultrasound studies on ED patients that were performed by the Department of Radiology. The study setting was a level 1 academic ED with an annual census of 70,000 patients. The protocol was reviewed and approved by the University of Virginia Institutional Review Board, who determined that informed consent was not required given the retrospective nature of the study design. Inclusion criteria were all first trimester pregnancy ultrasound studies performed amongst ED patients by the Department of Radiology within a four month time period dating from 1 January 2019 to 30 April, 2019. The picture archiving and communication system (PACS) database was queried for all pregnancy ultrasounds performed on ED patients within the specified time period. Studies were excluded if the gestational age was calculated at greater than or equal to 13 weeks on the ultrasound study. Additionally, studies were excluded in cases where both transvaginal and transabdominal imaging did not occur.
A total of 119 ultrasound studies were performed during this time period. Of these, 108 studies met inclusion criteria. The allocation diagram shown in Figure 1 illustrates which patients were excluded amongst the initial 119 identified.
 |
Figure 1 Allocation diagram demonstrating the patients who were excluded from the study cohort. |
Two emergency physicians with extensive background in ultrasound were then recruited. ED physician 1 (EP 1) is an emergency ultrasound fellowship trained with 4 years of post fellowship experience. ED physician 2 (EP 2) has over ten years of experience in the point of care ultrasound field, including over 5 years as an emergency ultrasound fellowship director. Each ED physician individually reviewed the transabdominal ultrasound images only from each study within PACS. They did not review any of the transvaginal images that were obtained from these studies. They were blinded to the radiologist interpretation, the electronic medical record, and all clinical information.
Outcomes
The primary outcome was the comparison of findings on the radiologist interpretation with findings on ED physician review of TAUS. Specifically, we sought to determine if there was any additive value from the radiologist report, which was inclusive of both transvaginal and transabdominal portions of the ultrasounds, in the subset of cases wherein the ED physician identified an intrauterine pregnancy on TAUS. We also sought to identify the number of TVUS studies that could be avoided if one were to follow a practice pattern common in point of care ultrasound, wherein one does not pursue TVUS if an IUP is identified on TAUS.
The two ED physicians recorded their findings on a standardized reporting sheet. They noted whether an intrauterine pregnancy was present or absent. They also noted whether a concerning ovarian cyst, subchorionic hemorrhage (SCH), and/or intrauterine fetal demise were present. They also noted any additional concerning findings that were present.
These results were compared to the radiologist report, which was inclusive of both the transabdominal and transvaginal imaging (eg - one report is provided for both sets of images within a study). We evaluated the radiologist report for presence or absence of an intrauterine pregnancy, presence or absence of fetal demise, presence or absence of a SCH, presence or absence of a significant ovarian cyst that was specifically noted in the radiologist impression section of the radiologist report, and presence of any other notable findings in the report.
Statistical Analysis
We calculated the sensitivity, specificity, and accuracy for ED physician TAUS review as compared to radiologist interpretation. These parameters were calculated using the Wilson procedure for 95% confidence interval for proportions via VassarStats statistical software. Additionally, an interrater reliability analysis using the Cohen linear weighted κ was performed to determine the level of consistency between the two ED physicians for their identification of key variables.
Results
One hundred and eight ultrasound studies met inclusion criteria and were enrolled into the study. Out of these 108, a total of 82 had a radiologist interpretation that included the presence of an intrauterine pregnancy. Table 1 provides details on the final radiologist interpretation of pregnancy location for these 108 studies.
 |
Table 1 Radiologist Interpretation of Pregnancy Location |
On transabdominal-only review of these 108 ultrasound studies, ED physician 1 identified 58 intrauterine pregnancies, while ED physician 2 identified 68 intrauterine pregnancies. The results on identification of IUP from both ED physicians are shown in Table 2. The studies where the ED physicians disagreed on presence of IUP are shown in Table 3. Figure 2 represents one such study where one ED physician noted an IUP on TAUS, while one did not. An anechoic sac is present on this image, but the yolk sac was only apparent on subsequent TVUS. The pooled sensitivity for ED physician transabdominal identification of IUP amongst the 108 included studies was 76.8% (95% CI of 69.6% to 83.1%) and the specificity was 98.1% (95% CI of 89.7% to 100%). Accuracy was 81.9% (95% CI of 76.2% to 86.8%). There was only one case wherein an ED physician recorded the presence of an IUP when the radiologist did not identify an IUP. In this case, the radiologist report noted no findings of pregnancy, advised pregnancy of unknown location, and recommended follow up imaging. At time of follow up imaging, this patient was found to have had a spontaneous miscarriage. On the standardized data sheet for this study, the reviewing ED physician commented that the findings were questionable but were judged to represent an IUP with a gestational sac and yolk sac visible.
 |
Table 2 Individual and Pooled Performance of Identification of Intrauterine Pregnancy from Both ED Physicians |
 |
Table 3 Studies in Which the Two ED Physicians Disagreed on the Presence or Absence of Intrauterine Pregnancy on Their Review of TAUS (Transabdominal Ultrasound) Images |
 |
Figure 2 Transabdominal and transvaginal image of one study wherein the two ED physicians disagreed about the presence or absence of an intrauterine pregnancy on transabdominal imaging. |
Out of the 69 cases where one, or both, ED physicians identified an IUP on their review of the transabdominal imaging, there were 5 cases of IUFD noted on the radiologist report. The two emergency physicians each accurately identified these five cases, with a pooled sensitivity of 100% (95% CI of 69% to 100%) and specificity of 100% (95% CI of 97% to 100%) as shown in Table 4. Additional findings that were included in the radiologist impression section from the 69 patients where one, or both, ED physicians noted an IUP on TAUS are shown in Table 5 and Table 6. Fifteen out of the 69 studies had a subchorionic hemorrhage noted and three had an ovarian cyst noted. On study 40, one ED physician recorded “no IUP”, while the other recorded “IUP” but then made a specific notation that these studies were suspicious for miscarriage.
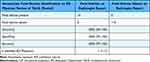 |
Table 4 Pooled Performance of Identification of Intrauterine Fetal Demise from the ED Physicians in Cases Where IUP Was Identified on TAUS |
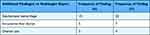 |
Table 5 Presence of Findings Noted in Radiologist Impression Section Amongst Those Studies Wherein One, or Both, ED Physicians Identified an IUP on TAUS |
 |
Table 6 Additional Findings Noted in Radiologist Impression Section of the Radiologist Report Amongst the 69 Patients Wherein One, or Both, ED Physicians Identified an IUP |
Out of the 108 total included patients, there were two ectopic pregnancies. In both of these cases, each of the emergency physicians noted the absence of an IUP. There were no cases of heterotopic pregnancy in this cohort. If the patients who had an identifiable IUP on TAUS had not received TVUS, it would have resulted in a theoretical reduction of TVUS performed on this patient cohort by 54% (EP 1) or 63% (EP 2). This is shown in Table 7.
 |
Table 7 Estimate of Number of TVUS That Could Have Been Avoided if Not Pursuing TVUS Following Identification of IUP on TAUS |
Discussion
Our study sought to investigate the utility of TVUS in the setting of an identified intrauterine pregnancy on TAUS among ED patients presenting with early pregnancy-related complaints. We did this through an analysis of radiology performed early pregnancy ultrasounds in first trimester ED patients. We chose this strategy given that nearly all of the first trimester pregnancy ultrasounds in the Department of Radiology during this time period involved utilizing both TAUS and TVUS. We subdivided cases into those where an IUP was identified on the ED physician review of TAUS images versus those that did not have an IUP identified. Within the cohort of patients where an IUP was present on the TAUS images, we further analyzed the theoretical value of TVUS by comparing ED physician findings with the radiology interpretation, which was inclusive of both the TAUS and TVUS portions of the study.
It is often suggested that once an IUP is identified on TAUS, the pursuit of subsequent TVUS is not necessary.15,16 This is based on the logic that an ectopic pregnancy is almost entirely excluded once an IUP is identified. Therefore, the primary “question” or purpose of the ultrasound is complete once an IUP is visualized on TAUS. An exception is those patients on fertility treatments, where the risk of heterotopic pregnancy mandates an evaluation of the adnexal regions regardless of presence or absence of an IUP.13,14
However, formal evidence supporting this practice is lacking and specialty society guidelines provide mixed guidance on the question of whether TVUS is still needed after identification of IUP on TAUS. It is also not clear what percentage of ED patients nationwide with first trimester pregnancy complaints receive TVUS following a TAUS that demonstrates an IUP. Routine TVUS does have inherent drawbacks as noted above. TVUS can carry financial implications, as it is a separately billable exam from the TAUS, with a wRVU assignment in the United States of 0.75 (CPT 76817) in 2021.17
In our cohort of 119 patients, there were only 2 cases wherein a TVUS was not done following a TAUS (see Figure 1). In one case the radiologist specifically noted in the report that the patient declined the transvaginal portion of the exam. The remaining patients received both TAUS and TVUS, regardless of whether an IUP might have been readily present on the TAUS. If it were indeed safe and reasonable to forgo TVUS after identifying an IUP on TAUS, then this would have reduced the number of TVUS performed on this cohort by 54% (EP 1) or 63% (EP 2). Utilizing the 2023 United States Medicare national reimbursement average, each TVUS would carry a professional fee of $36.26 and facility fee of $106.88.18 This would lead to an estimated cost savings of $8302 (EP 1) and $9734 (EP 2) in our cohort of 108 patients.
In the current study, the two ED physicians demonstrated very high specificity for the identification of IUP (98.1%, 95% CI of 89.7% to 100%), with only one false positive case out of the both physicians’ review. This high specificity is important, as it supports the idea that the added diagnostic value of TVUS in ruling out ectopic pregnancy is low in situations where an IUP is already identified on TAUS.
To further answer the question of what additional diagnostic value TVUS can add once an IUP is identified on TAUS, we evaluated the radiologist report impression section for additional findings beyond presence or absence of IUP. This would allow one to capture additional findings that might theoretically be missed by not pursuing TVUS after IUP identification on TAUS. The most common additional finding identified was subchorionic hemorrhage, followed by IUFD, and ovarian cysts. It would be anticipated that subchorionic hemorrhage (SCH) is better detected by TVUS given the additional resolution noted above. However, the significance of finding SCH is unclear and likely does not, in itself, justify the additional cost and resource expense of TVUS. While it has been thought that the presence of SCH may increase the risk of miscarriage and this may be dependent on the size of the SCH,19,20 newer evidence suggests that there may not be a strong association between SCH and subsequent miscarriage.21,22 Regardless, the management of an SCH is generally conservative, as therapies such as vaginal progesterone supplementation and bedrest have not been shown to increase live birth rates.23–25 Many practitioners will advocate for “pelvic rest” and reduced activity, though strong evidence is lacking for these recommendations as well. It is thus unlikely that a high accuracy of SCH identification is of high diagnostic value.
TAUS does not provide the level of detail as TVUS for the evaluation of ovarian cysts and adnexal lesions, and TVUS has been shown to be highly accurate in the evaluation of ovarian cysts.26,27 There were 3 patients that had an ovarian cyst or lesion noted in the radiologist impression section of the report in the cohort of patients with an IUP identified on ED physician TAUS review. One was a simple cyst (4 cm in largest dimension), one was a corpus luteal cyst (4 cm in largest dimension), and one was a case with two hemorrhagic cysts (each 5 cm in largest dimension). None of these patients required intervention for their cysts, though the patient with the hemorrhagic cysts did have a recommendation for repeat ultrasound in 7–10 days for reassessment. They followed up with their obstetrics physician and did not require an intervention. Given the drawbacks of routine TVUS, it may be prudent to only selectively pursue TVUS after IUP identification when a specific question or concern is present.
There are several important limitations inherent in our study design that should be taken into account. To evaluate our study question, we utilized pre-existing ultrasound studies that were performed on ED patients in the Department of Radiology. This has the potential for the introduction of selection bias, as our department also has an active point-of-care ultrasound program, with first trimester TAUS and TVUS sometimes being performed instead by the ED physician at the bedside. The reasons as to why an ED physician might order a Radiology ultrasound instead of performing a point-of-care ultrasound at the bedside could include provider comfort with the exam, time limitations, and un-identified patient specific factors. These were not evaluated in the present study, thus introducing the potential for selection bias to influence our results.
An additional limitation of note is that we utilized ED physicians as the interpreters of the TAUS images from the included radiology studies. The images were pre-saved and stored in PACS after being obtained by a sonographer. Our ED physicians simply viewed these images and did not do the scanning themselves, which is atypical for point of care ultrasound utilization in the ED. Fortunately, the overall agreement on the identification of IUP amongst our two ED physicians was high, speaking to their ability to reliably identify an IUP on TAUS images even though they were not the individuals performing the image acquisition.
The discrepancy that did exist between our two ED physicians may have been related to one of the ED physicians being more comfortable with calling an intrauterine pregnancy when there was a gestational sac without a clear and decisive yolk sac or fetal pole. Classic teaching is that one should be wary in identifying an IUP unless a yolk sac or fetal pole is present, so as to avoid mislabeling a pseudogestational sac as an IUP.1 However, there are additional sonographic features, such as the double decidual sign, that are generally seen only in true gestational sacs. This could account for the small additional number of IUPs that EP 2 identified.
An additional limitation to note is the size of the study. Arguably, the most important diagnosis to avoid missing with early pregnancy ultrasound is the ectopic pregnancy. Our cohort of patients had 2 ectopic pregnancies, or roughly 2% of our study cohort. While the ED physician review of TAUS would not have resulted in any ectopic pregnancy misses if one was forgoing TVUS after identification of TAUS IUP (eg - both physicians correctly noted “no IUP” on these two patients), it would have been helpful to have larger numbers to further validate this finding. This is also true for the identification of additional findings, such as ovarian cysts. In our study cohort, the three ovarian cysts noted in the impression portion of the radiologist report did not require any intervention, but a larger study may have identified an occasional ovarian cyst that does require intervention.
Finally, our study faces the inherent problem that we compared an ED physician review of TAUS images to a radiologist interpretation of the comprehensive study (TAUS and TVUS images). This adds an additional variable that confounds whether the differences in findings are due to the imaging modality used or due to type of reader. In other words, the differences in findings could be due to the different modality (TAUS versus TAUS and TVUS) or could be due to the different reader (radiologist versus ED physician). Given this, additional research would be needed by a single subtype of readers to explore this question further. Lastly, it would have been helpful to have separate radiologist reports for TAUS and TVUS available to compare these modalities directly, but these do not exist at our institution and thus we used the comprehensive report that was inclusive of both TAUS and TVUS.
Conclusion
The value of transvaginal ultrasound in first trimester pregnancy evaluations amongst ED patients may be low in cases where an intrauterine pregnancy can readily be identified on transabdominal ultrasound. While there is additional diagnostic information obtained, this must be weighed against the added cost, time, patient discomfort, ultrasound exposure, and high level disinfection requirements of transvaginal sonography. Therefore, selective use of transvaginal ultrasound should be encouraged in ED patients with early pregnancy complaints and an IUP apparent on transabdominal ultrasound.
Ethics and Consent Statements
The University of Virginia Institutional Review Board did not require patient consent for this study. This waiver was provided secondary to the retrospective nature of the study and the maintenance of all data on secure University of Virginia Health System servers. All patient data was kept confidential and in compliance with the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
1. American College of Obstetricians and Gynecologists. Committee on practice bulletins—obstetrics and the American Institute of Ultrasound in Medicine. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016;128(6):e241–e256. doi:10.1097/AOG.0000000000001815
2. Brown DL, Packard A, Maturen KE, et al.; Expert Panel on Women’s Imaging. ACR appropriateness criteria® first trimester vaginal bleeding. J Am Coll Radiol. 2018;15(5S):S69–S77. doi:10.1016/j.jacr.2018.03.018
3. Hahn SA, Promes SB, Brown MD, Brown MD; American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy [published correction appears in Ann Emerg Med. 2017;70(5):758]. Ann Emerg Med. 2017;69(2):241–250.e20. doi:10.1016/j.annemergmed.2016.11.002
4. Hendriks E, MacNaughton H, MacKenzie MC. First trimester bleeding: evaluation and management. Am Fam Physician. 2019;99(3):166–174.
5. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27–e54. doi:10.1016/j.annemergmed.2016.08.457
6. Jain KA, Hamper UM, Sanders RC. Comparison of transvaginal and transabdominal sonography in the detection of early pregnancy and its complications. AJR Am J Roentgenol. 1988;151(6):1139–1143. doi:10.2214/ajr.151.6.1139
7. Kaur A, Kaur A. Transvaginal ultrasonography in first trimester of pregnancy and its comparison with transabdominal ultrasonography. J Pharm Bioallied Sci. 2011;3(3):329–338. 16. doi:10.4103/0975-7406.84432
8. Gramith F, Sirr S, Hollerman J, et al. Transvaginal versus transabdominal sonography in patients suspected of having ectopic pregnancy. Minn Med. 1991;74(1):27–31.
9. Biggs WS, Marks ST. Diagnosis and management of adnexal masses. Am Fam Physician. 2016;93(8):676–681.
10. Rodgers SK, Chang C, DeBardeleben JT, et al. Normal and abnormal us findings in early first-trimester pregnancy: review of the Society of Radiologists in Ultrasound 2012 consensus panel recommendations. Radiographics. 2015;35(7):2135–2148. doi:10.1148/rg.2015150092
11. American Institute of Ultrasound in Medicine Official Statement. Guidelines for cleaning and preparing external- and internal-use ultrasound transducers and equipment between patients as well as safe handling and use of ultrasound coupling gel; 2017. Available from: https://www.aium.org/officialstatements/57.
12. American College of Emergency Physicians. Guideline for ultrasound transducer cleaning and disinfection. Ann Emerg Med. 2018;72(4):e45–e47. doi:10.1016/j.annemergmed.2018.07.035
13. Ciebiera M, Słabuszewska-Jóźwiak A, Zaręba K, Jakiel G. Heterotopic pregnancy - how easily you can go wrong in diagnosing? A case study. J Ultrason. 2018;18(75):355–358. doi:10.15557/JoU.2018.0052
14. Noor N, Bano I, Parveen S. Heterotopic pregnancy with successful pregnancy outcome. J Hum Reprod Sci. 2012;5(2):213–214. doi:10.4103/0974-1208.101024
15. Panebianco NL, Shofer F, Fields JM, et al. The utility of transvaginal ultrasound in the ED evaluation of complications of first trimester pregnancy. Am J Emerg Med. 2015;33(6):743–748. 17. doi:10.1016/j.ajem.2015.02.023
16. O’Connor TP, Garton N, Jones C, Estephan M, Lu M, Adler D. Emergency physician utilization of transvaginal ultrasound after initiation of revised sterilization protocol. Am J Emerg Med. 2019;37(4):789–791. doi:10.1016/j.ajem.2018.08.077
17. American College of Emergency Physicians Emergency Ultrasound Section. Emergency ultrasound coding guide; 2020. Available from: https://www.acep.org/globalassets/uploads/uploadedfiles/acep/by-medicalfocus/ultrasound/acep-us-cpt-update-2020.pdf.
18. Fujifilm SonoSite. Ultrasound reimbursement information, emergency medicine; 2020. Available from: https://www.sonosite.com/sites/default/files/2020%20SonoSite%20-%20Emed%20Guide%20022020.pdf.
19. Tuuli MG, Norman SM, Odibo AO, Macones GA, Cahill AG. Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis. Obstet Gynecol. 2011;117(5):1205–1212. doi:10.1097/AOG.0b013e31821568de
20. Bennett GL, Bromley B, Lieberman E, Benacerraf BR. Subchorionic hemorrhage in firsttrimester pregnancies: prediction of pregnancy outcome with sonography. Radiology. 1996;200(3):803–806. doi:10.1148/radiology.200.3.8756935
21. Naert MN, Khadraoui H, Muniz Rodriguez A, Naqvi M, Fox NS. Association between firsttrimester subchorionic hematomas and pregnancy loss in singleton pregnancies. Obstet Gynecol. 2019;134(2):276–281. doi:10.1097/AOG.0000000000003360
22. Inman ER, Miranian DC, Stevenson MJ, Kobernik EK, Moravek MB, Schon SB. Outcomes of subchorionic hematoma-affected pregnancies in the infertile population. Int J Gynaecol Obstet. 2022;159(3):743–750. doi:10.1002/ijgo.14162
23. Coomarasamy A, Devall AJ, Cheed V, et al. A randomized trial of progesterone in women with bleeding in early pregnancy. N Engl J Med. 2019;380(19):1815–1824. 18. doi:10.1056/NEJMoa1813730
24. McCall CA, Grimes DA, Lyerly AD. “Therapeutic” bed rest in pregnancy: unethical and unsupported by data. Obstet Gynecol. 2013;121(6):1305–1308. doi:10.1097/AOG.0b013e318293f12f
25. Ben-Haroush A, Yogev Y, Mashiach R, Meizner I. Pregnancy outcome of threatened abortion with subchorionic hematoma: possible benefit of bed-rest? Isr Med Assoc J. 2003;5(6):422–424.
26. Sahdev A. Ovary and adnexa: imaging techniques, anatomy and normal findings. In: Hamm B, Ros PR, editors. Abdominal Imaging. Berlin, Heidelberg: Springer; 2013.
27. Forstner R. Early detection of ovarian cancer. Eur Radiol. 2020;30(10):5370–5373. doi:10.1007/s00330-020-06937-z
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
