Back to Journals » Journal of Asthma and Allergy » Volume 14
The Usefulness of FEF25–75 in Predicting Airway Hyperresponsiveness to Mannitol
Authors Kim Y , Lee H , Chung SJ, Yeo Y , Park TS , Park DW, Min KH , Kim SH , Kim TH , Sohn JW, Moon JY , Yoon HJ
Received 3 May 2021
Accepted for publication 20 September 2021
Published 28 October 2021 Volume 2021:14 Pages 1267—1275
DOI https://doi.org/10.2147/JAA.S318502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amrita Dosanjh
Youlim Kim,1,* Hyun Lee,2,* Sung Jun Chung,2,* Yoomi Yeo,2 Tai Sun Park,2 Dong Won Park,2 Kyung Hoon Min,3 Sang-Heon Kim,2 Tae-Hyung Kim,2 Jang Won Sohn,2 Ji-Yong Moon,2 Ho Joo Yoon2
1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Konkuk University Hospital, School of Medicine, Konkuk University, Seoul, Korea; 2Department of Internal Medicine, College of Medicine, Hanyang University, Seoul, Korea; 3Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Korea University Medical Center, Guro Hospital, Seoul, Korea
*These authors contributed equally to this work
Correspondence: Ji-Yong Moon
Department of Internal Medicine, Hanyang University Guri Hospital, Gyeongchun-ro 153, Guri-si, Gyeonggi-do, 11923, Korea
Tel +82-31-560-2224
Fax +82-31-553-7369
Email [email protected]
Ho Joo Yoon
Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, 222-1, Wangsimni-ro, Seongdong-gu, Seoul, 04763, Korea
Tel +82-2-2290-8336
Fax +82-2-2298-9183
Email [email protected]
Background and Objective: Despite the usefulness of airway hyperresponsiveness (AHR) testing in diagnosing and monitoring asthma, it is challenging to perform in a real-world setting. Forced expiratory flow between 25% and 75% of vital capacity (FEF25– 75), a pulmonary measurement that can be obtained easily during routine spirometry, represents the status of medium-sized and small airways. However, the performance of FEF25– 75 in predicting AHR has not been well elucidated. Therefore, we investigated whether FEF25– 75 can predict AHR to mannitol.
Methods: We performed a retrospective cohort study of 428 patients who visited a single clinic due to cough, wheezing, or dyspnea. All patients underwent spirometry with a mannitol provocation test. We compared the area under the curve (AUC) of the percentage of the predicted values of FEF25– 75 (FEF25– 75 %pred) with that of forced expiratory volume in 1 second (FEV1%pred), FEV1/forced vital capacity (FVC), and FEF25– 75/ FVC for predicting AHR.
Results: The rate of AHR to mannitol was 20.3%. In the overall study population, the AUC of FEF25– 75 %pred for predicting AHR (0.772; 95% confidence interval [CI], 0.729– 0.811) was significantly higher than that of FEV1%pred (0.666; 95% CI, 0.619– 0.710; p < 0.001), FEV1/FVC (0.741; 95% CI, 0.697– 0.782; p = 0.047), and FEF25– 75/FVC (0.741, 95% CI = 0.696– 0.782, p = 0.046). The sensitivity, specificity, positive predictive value, and negative predictive value of FEF25– 75 %pred < 81% for predicting AHR in the overall study population were 77.0% (95% CI = 66.8– 85.4%), 63.9% (95% CI = 58.6– 69.0), 35.3%, and 91.6%, respectively. When we restricted the study group to subjects with normal lung function, the results were similar.
Conclusion: Our results indicate that FEF25– 75 %pred can be used as a surrogate for predicting AHR in patients with respiratory symptoms.
Keywords: forced expiratory flow between 25% and 75% of vital capacity, mannitol, bronchial hyperresponsiveness
Introduction
Airway hyperresponsiveness (AHR), showing increased airway sensitivity to an inhaled airway constrictor, is a major characteristic of bronchial asthma.1 This is important not only when diagnosing asthma, but also in monitoring the current status of an asthma patient.2 Despite the usefulness of AHR testing, it is not easy to use in real-world clinics, especially in the primary care clinics in which most asthmatic patients are managed, due to the complexity of the test and clinician unfamiliarity with it.3 As a result, primary care providers need a cost-effective test that can serve as a substitute or screening test. Measuring patient lung function is very important in clinical practice because pulmonary function is regarded as a treatment outcome in asthma, and it is crucial to evaluate the current status of patients.4 Furthermore, because current asthma guidelines strongly recommend regular spirometry testing,4 many subjects with asthma or suspected asthma undergo spirometry during clinic visits. Thus, it would be useful in real practice if a surrogate biomarker of AHR could be found among the values already commonly measured during routine spirometry.
Among the various measurements collected during conventional spirometry, forced expiratory flow at 25% and 75% of the pulmonary volume (FEF25–75) measures the average flow rates of medium-to-small airways during the forced vital capacity (FVC) segment to testing and presents the status of those airways in patients, along with the normal forced expiratory volume in 1 second (FEV1) and FEV1/FVC.5,6 One study suggested that FEF25–75 is more appropriate than FEV1 for assessing AHR and that it can reveal small-airway impairment earlier than other tests in patients with bronchial asthma or allergic rhinitis.7 Another study showed that FEF25–75 is associated with AHR in allergic patients and bronchial asthma patients with respiratory symptoms,8,9 suggesting it could be a potential surrogate test for AHR.
The mannitol provocation test applies mannitol as an indirect stimulator to provoke AHR.10,11 Very few data are available about the value of the spirometric indices for predicting AHR to mannitol. In this study, we compare the predictive value of those common spirometric parameters as surrogate markers of airway responsiveness to mannitol.
Methods and Materials
Study Design and Study Population
We conducted a retrospective study at a single university hospital between December 2013 and July 2014 to determine whether spirometric parameters predict AHR, consecutively enrolling 428 patients. All patients had asthma-like symptoms of dyspnea, coughing, or wheezing and underwent both spirometry and a mannitol provocation test. None of the patients in this study had any medical history of airway diseases such as asthma or chronic obstructive pulmonary disease (COPD) at the time of study enrollment. Demographic data (age, sex, height, and weight), respiratory symptoms, spirometric results, and mannitol provocation test results were collected by chart review. This study was conducted in accordance with Declaration of Helsinki. Only first authors, corresponding authors, and co-authors have access to patients’ information, and patients’ information will be discarded after the study is completed. The Institutional Review Board of Hanyang University Guri Hospital approved the study protocol and waived the need for informed consent because of the retrospective study design (IRB number 2017-04-036-002).
Spirometry and Mannitol Provocation Test
Spirometry was conducted by well-trained technicians according to the American Thoracic Society and European Respiratory Society guidelines.12 The mannitol provocation test was carried out using Aridol™ (Pharmaxis Ltd., Sydney, Australia) according to the manufacturer’s protocol.13 AHR was defined as at least a 15% decrease in FEV1 after the provocation (compared with baseline FEV1). Patients were classified into two groups by the presence of AHR: the AHR group and the non-AHR group.
Statistical Analyses
Data were analyzed using SPSS software for Windows version 23.0 (IBM Corp., Armond, NY, USA). Continuous and categorical data are presented as the mean ± standard deviation and n (%), respectively. Differences in continuous data such as age, height, weight, and spirometric values were analyzed using the independent Student’s t-test or Mann–Whitney U-test. The chi-square test was performed to compare categorical variables such as sex and the presence of underlying diseases. The area under the receiver operating characteristic curve (AUC) was used to compare the predictive value of the spirometric parameters (percentages of the predicted values of FEV1 [FEV1%pred], FEF25–75 [FEF25–75 %pred], FEV1/FVC, and FEF25–75/FVC). To calculate and compare the AUC values, we used MedCalc (MedCalc Software, Ostend, Belgium) with the DeLong method. P-values less than 0.05 were considered statistically significant.
The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of FEF25–75 %pred for AHR to mannitol were calculated using different cut-off values of FEF25–75 %pred (50%, 60%, 70%, 80%, and 90% and an optimal cut-off value determined using the Youden index). The most suitable AUC to predict AHR using FEF25–75 %pred was determined by plotting sensitivity versus 1–specificity using a receiver operating characteristic (ROC) curve. The best threshold of FEF25–75 %pred for predicting AHR was determined using the Youden index as the value that maximized sensitivity while minimizing the false-positive rate.14 Subsequently, we calculated PPV and NPV using MedCalc to determine the effectiveness of FEF25–75 %pred in predicting the results of the mannitol provocation test. To evaluate whether FEF25–75 ≤ optimal cut-off values were associated with AHR to mannitol in the overall study population and the subgroup with normal spirometry, we performed univariable and multivariable logistic binary regression analyses. In the multivariable analysis, age, sex, BMI, and smoking status were adjusted.
Results
Baseline Characteristics of the Study Population
The baseline characteristics of the study population are shown in Table 1. Of 428 patients, 87 (20.3%) had AHR, and 341 (79.7%) did not. The mean age was 52.4 ± 18.3 years, and 183 subjects (42.8%) were male. Patients with and without AHR did not differ significantly in age, sex, height, weight, BMI, or smoking status. Spirometric values, FEV1 %pred (p < 0.001), FVC %pred (p = 0.048), FEV1/FVC (p=0.001), and FEF25–75 %pred (p = 0.001), were all significantly higher in the non-AHR group than in the AHR group (Table 1). The baseline characteristics of subjects with normal spirometry are presented in Supplemental Table 1.
 |
Table 1 The Baseline Characteristics of Overall Study Population |
Final Clinical Diagnosis After Work-Up
After work-up, asthma was diagnosed by the attending physicians in 105 subjects; its prevalence was higher in the AHR group (94.3% vs 6.7%, p < 0.001) than in the non-AHR group. Among subjects with normal spirometry, the prevalence of asthma was also higher in the AHR group (70.3% vs 7.1%, p < 0.001). COPD was diagnosed in 15 subjects; the rate of COPD patients did not differ significantly between the AHR and non-AHR groups (p = 0.524).
AUC Values of Spirometric Parameters in the Overall Study Population
The ROC curves and AUC values of the spirometric parameters for predicting AHR in the overall study population are shown in Figure 1 and Table 2, respectively. The AUC value of FEF25–75 %pred (0.772, 95% CI = 0.729–0.811) was significantly higher than those of FEV1/FVC (AUC = 0.741, 95% CI = 0.697–0.782, p = 0.047), FEF25–75/FVC (AUC = 0.741, 95% CI = 0.696–0.782, p = 0.046), and FEV1 %pred (AUC = 0.666, 95% CI = 0.619–0.710, p < 0.001) (Table 2, Figure 2).
 |
Table 2 AUC Values of Typical Spirometric Indices Obtained Based on All Patients’ Spirometry |
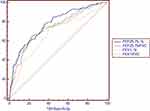 |
Figure 1 ROC curves for predicting AHR to mannitol (total study population). Abbreviations: ROC, receiver operating characteristic; AHR, airway hyperresponsiveness. |
 |
Figure 2 ROC curves for predicting AHR to mannitol (subjects with normal spirometry). Abbreviations: ROC, receiver operating characteristic; AHR, airway hyperresponsiveness. |
AUC Values of Spirometric Parameters in the Subgroup with Normal Spirometry
The ROC curves and AUC values of the spirometric parameters for predicting AHR in the subgroup with normal spirometry are shown in Figure 3 and Table 3, respectively. The AUC value of FEF25–75 %pred (AUC = 0.704, 95% CI = 0.646–0.757) was higher, though not always significantly, than those of FEV1/FVC (AUC = 0.644, 95% CI = 0.584–0.700, p = 0.047), FEF25–75/FVC (AUC = 0.665, 95% CI = 0.606–0.720, p = 0.231), and FEV1 %pred (AUC = 0.589, 95% CI = 0.529–0.648, p = 0.012) (Table 3, Figure 2).
 |
Table 3 AUC Values of Typical Spirometric Indices in Patients with Normal Spirometry (FEV1 ≥ 80% and FEV1/FVC ≥ 70) |
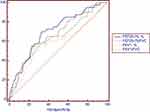 |
Figure 3 AUC distributions in the total study population and subjects with normal spirometry. Abbreviation: AUC, area under the curve. |
Performance of Spirometric Parameters in Predicting AHR
The optimal cut-off values of FEF25–75 %pred for predicting AHR were 81% (Supplemental Figure 1) and 87% (Supplemental Figure 2) in the overall population and the subgroup with normal spirometry, respectively. As shown in Table 4, the sensitivity, specificity, PPV, and NPV of FEF25–75%pred <81% for predicting AHR in the overall study population were 77.0% (95% CI = 66.8–85.4%), 63.9% (95% CI = 58.6–69.0), 35.3%, and 91.6%, respectively (Table 4, Supplementary Figure 1). The sensitivity, specificity, PPV, and NPV of FEF25–75 %pred <87% for predicting AHR in the subgroup with normal spirometry were 70.0% (95% CI = 53.5–83.4%), 66.8 (95% CI = 60.7–72.5%), 24.3%, and 93.6%, respectively (Table 4). The sensitivity, specificity, PPV, and NPV calculated using other cut-off values for FEF25–75 %pred are also provided in Table 4.
 |
Table 4 Criterion of FEF25–75 for Predicting AHR to Mannitol |
As shown in Table 5, FEF25–75 %pred <81% and FEF25–75 %pred <87% were associated with AHR in the overall study population (unadjusted odds ratio [OR] = 5.93, 95% CI = 3.43–10.25; adjusted OR = 9.57, 95% CI = 4.88–18.74) and in the subgroup with normal spirometry (unadjusted OR = 4.69, 95% CI = 2.27–9.67; adjusted OR = 6.86, 95% CI = 2.80–16.78), respectively.
 |
Table 5 Unadjusted or Adjusted or of FEF25–75 ≤Optimal Cut-Off Values for AHR to Mannitol |
Discussion
In this study, we investigated the diagnostic value of FEF25–75 %pred in predicting AHR during the mannitol provocation test. Our results show that FEF25–75 %pred had a significantly higher AUC value than the other spirometric parameters we evaluated. FEF25–75 %pred values with a cut-off of 81% (for the overall population) and 87% (for those with normal spirometry) performed relatively well in terms of sensitivity and NPV for predicting AHR in the mannitol provocation test.
AHR is an abnormal bronchial response to bronchoconstrictor stimuli and one of the typical features of bronchial asthma.1,15 To confirm AHR, direct and indirect provocation tests16 are used, both of which have limited clinical practicality due to their complexity.3,17 Thus, an easy-to-use biomarker that can predict AHR is needed for real practice in primary clinics.
From that perspective, FEF25–75 has the advantages of being routinely reported during simple spirometry and being easily assessable in primary clinics. FEF25–75 is more sensitive to the presence of small-airway diseases than FEV1.5,6,18 An asthma patient with a normal FEV1 might show a decreased FEF25–75 level by the time of the test.19 Asthma patients in primary care clinics can show mild respiratory symptoms and normal ranges of airflow limitation, allowing earlier diagnosis and under- or late diagnosis,20 respectively. Several previous attempts have been made to assess AHR using FEF25–75.21,22 In a study by Rao et al.21 FEF25–75 was used to identify a positive bronchodilator response in asthmatic patients, and it was able to predict the severity and acute exacerbation of asthma. Another study found that an abnormal FEF25–75 level was associated with AHR in patients with asthma-like symptoms and normal FEV1.22 However, those previous studies did not determine an ideal cut-off value for FEF25–75. The major advantage of our study is that we calculated cut-off values of FEF25–75 and evaluated their performance in predicting AHR to mannitol provocation. We further showed that it can be applied not only to subjects with abnormal lung function, but also to those with normal spirometry values.
The clinical relevance of our study is reflected in the relatively good sensitivity and high NPV of FEF25–75 %pred for predicting AHR. The relatively good sensitivity of FEF25–75 %pred indicates that it might be used as a sensitive indicator to screen for AHR in patients with asthma-like respiratory symptoms in primary clinics, even when they have normal lung function. This measure can help in diagnosing asthma or deciding whether to transfer patients to secondary or tertiary hospitals for AHR testing. Notably, the NPV of FEF25–75 %pred is greater than 90%, which indicates that an FEF25–75 > 81% can be used to exclude the presence of AHR in patients with respiratory symptoms. However, considering the limitations of our retrospective study, well-designed prospective studies are needed.
Our study has several limitations. First, this was a retrospective study performed in a single referral hospital. Second, although we provide the useful information that FEF25–75 predicts AHR better than other pulmonary measurements (FEF25–75/FVC, FEV1 %pred, and FEV1/FVC), we could not compare FEF25–75 with other measurements that reflect small-airway diseases (eg, V50 or V25) because we did not measure those values during spirometry. Additionally, our study did not compare the performance of FEF25–75 %pred with tests such as fractional exhaled nitric oxide or blood eosinophil count. However, those tests are not commonly performed in primary clinics, putting those comparisons beyond the scope of our study. Lastly, we did not evaluate the association between treatment (eg, medication), airway reversibility, and subjective symptoms in patients presenting asthma-like symptoms. Because our study was retrospective, we could not evaluate treatment outcome measurements (eg, asthma control test for asthma, modified Medical Research Council scale for dyspnea, or visual analogue scale for cough). In general, the objective assessment of treatment response in respiratory diseases is very limited. Nonetheless, because we did not evaluate the clinical implications of our results in terms of treatment outcomes, we accept this as a limitation of our study. A well-designed prospective study for this issue is needed.
Conclusion
We found that FEF25–75 %pred had a significantly higher AUC value than other spirometric parameters for predicting AHR in the mannitol provocation test. With a cut-off of 81%, the FEF25–75 %pred showed good sensitivity and NPV in predicting AHR in the mannitol provocation test.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, agreed to the submitted journal, and agree to be accountable for all aspects of the work.
Funding
This work was supported by National Research Foundation of Korea (NRF) grants funded by the Ministry of Science, Information and Communications Technologies (MSIT) (NRF-2020R1F1A1070468 and NRF-2021M3E5D1A01015176) and by a Korea Medical Device Development Fund grant funded by the Korean government (Ministry of Science and ICT, Ministry of Trade, Industry and Energy, Ministry of Health & Welfare, and Ministry of Food and Drug Safety) (Project Number: 1711138447, KMDF_PR_20200901_0214).
Disclosure
Youlim Kim, Hyun Lee and Sung Jun Chung are co-first authors for this study. Ji-Yong Moon and Ho Joo Yoon are co-correspondence authors for this study. The authors have no conflicts of interests to declare.
References
1. Sposato B, Scalese M, Migliorini MG, Di Tomassi M, Scala R. Small airway impairment and bronchial hyperresponsiveness in asthma onset. Allergy Asthma Immunol Res. 2014;6(3):242–251. doi:10.4168/aair.2014.6.3.242
2. Cho EY, Oh KJ, Rhee CK, et al. Comparison of clinical characteristics and management of asthma by types of health care in South Korea. J Thorac Dis. 2018;10(6):3269–3276. doi:10.21037/jtd.2018.05.95
3. Choi JY, Yoon HK, Lee JH, et al. Current status of asthma care in South Korea: nationwide the health insurance review and assessment service database. J Thorac Dis. 2017;9(9):3208–3214. doi:10.21037/jtd.2017.08.109
4. 2020 GINA Report. Global Strategy for Asthma Management and Prevention; 2020.
5. Lipworth BJ, Clark DJ. Effects of airway calibre on lung delivery of nebulised salbutamol. Thorax. 1997;52(12):1036–1039. doi:10.1136/thx.52.12.1036
6. Malerba M, Radaeli A, Olivini A, et al. Association of FEF25–75% impairment with bronchial hyperresponsiveness and airway inflammation in subjects with asthma-like symptoms. Respiration. 2016;91(3):206–214. doi:10.1159/000443797
7. Munoz-Lopez F, Rios-Alcolea M. The interest of FEF(25s–75) in evaluating bronchial hyperresponsiveness with the methacholine test. Allergol Immunopathol. 2012;40(6):352–356. doi:10.1016/j.aller.2011.07.003
8. Ciprandi G, Cirillo I. Forced expiratory flow between 25% and 75% of vital capacity may be a marker of bronchial impairment in allergic rhinitis. J Allergy Clin Immunol. 2011;127(2):
9. Alberts WM, Ferris MC, Brooks SM, Goldman AL. The FEF25–75% and the clinical diagnosis of asthma. Ann Allergy. 1994;73(3):221–225.
10. Anderson SD. Indirect challenge tests: airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest. 2010;138(2Suppl):25S–30S. doi:10.1378/chest.10-0116
11. Lee J, Song JU. Diagnostic comparison of methacholine and mannitol bronchial challenge tests for identifying bronchial hyperresponsiveness in asthma: a systematic review and meta-analysis. J Asthma. 2020;1–9. doi:10.1080/02770903.2020.1739704
12. Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. doi:10.7326/0003-4819-155-3-201108020-00008
13. Anderson SD, Brannan J, Spring J, et al. A new method for bronchial-provocation testing in asthmatic subjects using a dry powder of mannitol. Am J Respir Crit Care Med. 1997;156(3 Pt 1):758–765. doi:10.1164/ajrccm.156.3.9701113
14. Schisterman EF, Faraggi D, Reiser B, Hu J. Youden index and the optimal threshold for markers with mass at zero. Stat Med. 2008;27(2):297–315. doi:10.1002/sim.2993
15. Grootendorst DC, Rabe KF. Mechanisms of bronchial hyperreactivity in asthma and chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2004;1(2):77–87. doi:10.1513/pats.2306025
16. Kim MH, Song WJ, Kim TW, et al. Diagnostic properties of the methacholine and mannitol bronchial challenge tests: a comparison study. Respirology. 2014;19(6):852–856. doi:10.1111/resp.12334
17. Lim SY, Jo YJ, Chun EM. The correlation between the bronchial hyperresponsiveness to methacholine and asthma like symptoms by GINA questionnaires for the diagnosis of asthma. Validation studies. BMC Pulm Med. 2014;14(161):161. doi:10.1186/1471-2466-14-161
18. Quanjer PH, Weiner DJ, Pretto JJ, Brazzale DJ, Boros PW. Measurement of FEF25–75% and FEF75% does not contribute to clinical decision making. Eur Respir J. 2014;43(4):1051–1058. doi:10.1183/09031936.00128113
19. Strunk RC, Szefler SJ, Phillips BR, et al. Relationship of exhaled nitric oxide to clinical and inflammatory markers of persistent asthma in children. J Allergy Clin Immunol. 2003;112(5):883–892. doi:10.1016/j.jaci.2003.08.014
20. Lusuardi M, De Benedetto F, Paggiaro P, et al. A randomized controlled trial on office spirometry in asthma and COPD in standard general practice: data from spirometry in Asthma and COPD: a comparative evaluation Italian study. Chest. 2006;129(4):844–852. doi:10.1378/chest.129.4.844
21. Rao DR, Gaffin JM, Baxi SN, Sheehan WJ, Hoffman EB, Phipatanakul W. The utility of forced expiratory flow between 25% and 75% of vital capacity in predicting childhood asthma morbidity and severity. J Asthma. 2012;49(6):586–592. doi:10.3109/02770903.2012.690481
22. Raji H, Haddadzadeh Shoushtari M, Idani E, et al. Forced expiratory flow at 25–75% as a marker for airway hyper responsiveness in adult patients with asthma-like symptoms. Tanaffos. 2018;17(2):90–95.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
