Back to Journals » Clinical Ophthalmology » Volume 11
The use of WaveLight® Contoura to create a uniform cornea: the LYRA Protocol. Part 2: the consequences of treating astigmatism on an incorrect axis via excimer laser
Authors Motwani M
Received 3 February 2017
Accepted for publication 18 April 2017
Published 16 May 2017 Volume 2017:11 Pages 907—913
DOI https://doi.org/10.2147/OPTH.S133840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Manoj Motwani
Motwani LASIK Institute, San Diego, CA, USA
Purpose: To show how an incorrect manifest astigmatism axis can cause an abnormal induced astigmatism on a new axis.
Patients and methods: Four eyes of three patients were treated primarily with WaveLight® EX500 wavefront optimized (WFO) treatments for astigmatism. All four eyes needed enhancements and were analyzed retrospectively via WaveLight® Contoura to determine the reason for the incorrect astigmatism treatment. Two of the eyes were retreated with topographic-guided ablation, and two were treated with WFO correction.
Results: The eyes that had an incorrect manifest axis resulted in a new abnormal induced astigmatism on a wholly new axis. Treatment with topographic-guided ablation completely eliminated the newly induced astigmatism. Treatment with WFO of an abnormal induced astigmatism corrected the refraction but still left topographic evidence of the abnormal astigmatism behind. One eye was incorrectly treated for astigmatism due to coma affecting refraction when the patient was dilated. This eye had a normal induced astigmatism on a perpendicular axis and was corrected using WFO. The use of manifest refraction with WaveLight® Contoura topographic-guided ablation will lead to incorrect astigmatism correction when the manifest astigmatism and axis differ from the WaveLight® Contoura measured.
Conclusion: Correction of an incorrect manifest refraction astigmatic axis does not simply create undercorrection of the astigmatism but induces an entirely new abnormal astigmatism on a different axis. Manifest refraction is less accurate and can lead to abnormal astigmatism when laser ablation is performed.
Keywords: WaveLight Contoura, astigmatism treatment, asymmetric astigmatism, topographic guide ablation, higher order aberrations, Contoura with LYRA Protocol, LASIK, PRK
Introduction
The advent of topographic-guided ablation to treat primary corrections has the power to change how refractive surgeons view laser vision correction, and vision correction as a whole. Throughout our ophthalmic training, we have been taught to use our best manifest refraction (whether dilated or nondilated) to perform vision correction including with the excimer laser. With the US Food and Drug Administration approval of WaveLight® Contoura topographic-guided ablation (Contoura) (WaveLight, Erlangen, Germany), refractive surgeons now have a choice whether to use the manifest refraction or the Contoura measured astigmatic correction (the astigmatism/axis that Contoura calculates and displays on the Contoura surgical planning page) for topographic-guided laser correction. The Contoura-measured astigmatism correction is derived by systematic analysis of the cornea with a WaveLight® proprietary algorithm and may be markedly different from the manifest refraction, resulting in a dilemma for refractive surgeons. This confusion is now being alleviated that Alcon clinical staff are now actively teaching the use of measured Contoura correction with the LYRA (Layer Yolked Reduction of Astigmatism) Protocol.
In the first part of this LYRA Protocol Thematic Series, the interaction between higher order aberrations (HOAs) and lower order corneal astigmatism was explored. In the second part, we will now explore the consequences of correcting on the incorrect astigmatic axis. These have neither been completely understood nor demonstrated.
Bueeler et al1 have theorized that in cases where torsional misalignment is present, not only does the original astigmatism become improperly treated but also that a new abnormal astigmatism is created on a wholly new axis. Although the assumptions have been made for wavefront-guided treatment, the assumptions apply fully to all ablation profiles, since they are applied to the anterior surface of the cornea. This can best be envisioned as a force vector diagram with the laser acting on the cornea with deviation in relation to the true astigmatic axis. It has been estimated that there is up to 3.3% loss of cylinder power for every degree of off-axis correction.2 Most refractive surgeons are familiar with the loss of cylinder correction when treating on the wrong axis, but what is underappreciated is that an abnormal new astigmatism is created. It intuitively makes sense when we realize that the system must incorporate the new regular astigmatism pattern created, and the original astigmatism pattern, and this leads to the abnormal induced astigmatism on a whole new axis.
A departure from our traditional dependence on the manifest refraction is not an easy transition. The decision to fully trust the measured Contoura cylinder axis was an evolution from manifest refraction to 50/50 (difference between manifest and measured power and axis), and then to full measured readings. This paper will demonstrate our results when the initial treatment was done with manifest astigmatism and axis. The incorrect astigmatic axis or power was used, and induced astigmatism along a new axis was created. We present here four eyes from three patients who initially had primary LASIK on the WaveLight® EX500 using wavefront optimized (WFO) ablation.
Patients and methods
This is an analysis of four eyes of three patients that had WFO myopia/myopic astigmatism correction on the WaveLight® EX500 and had outcomes with residual astigmatism that needed to be retreated. All three patients had refraction and surgery by the same surgeon (MM) using the same WaveLight® EX500 laser in the same center. All three patients had their primary correction performed before Contoura was available, but all three had Topolyzer Vario scans prior to their primary laser correction. The preoperative scans were retrospectively analyzed using the Contoura system to show the measured astigmatic axis and astigmatic power, and comparison was made to the manifest refraction and the postoperative outcome. All four eyes were subsequently enhanced, two via topographic-guided ablation using measured Contoura astigmatism and axis (the LYRA Protocol as described in another paper3) and two via WFO.
All three patients had well-centered flaps, no significant dry eye or epithelial abnormalities, and had no other pathology noted that could affect their laser vision correction outcomes. On two of the patients, the fellow eye was corrected properly with plano refraction and 20/20 or better vision.
All patients provided written consent to have their data published in this paper.
Results
Case 1
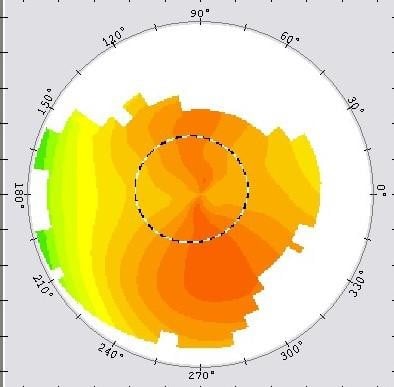
Patient 1 was a 29-year-old male who had WFO LASIK on the EX500 with an incorrect manifest refraction astigmatism axis. Figure 1 shows the preoperative Topolyzer topography.
- Manifest refraction: −4.00, −2.00×175
- Postoperator WFO: 0.50, −1.75×35 with an uncorrected visual acuity of 20/40
- Retrospective Contoura analysis of astigmatism: −1.99×6.
  | Figure 1 Patient 1: preoperative OD. |
This patient had a correction that was 11 degrees off axis and ended up with an entirely new astigmatism on the 35-degree axis. The 11-degree difference would result in a 33% loss of effectiveness, and we could calculate that we should have 0.66 D decrease in correction, with a new abnormal astigmatism of about 0.66 D.
- Contoura-measured treatment for enhancement −0.50, −1.50×39.
There seems to be a disparity between the calculated amount, and the actual amount necessary to be treated.
The postoperative topography (Figure 2) shows this astigmatism at the 35-degree axis, and it is not a normal, regular “bowtie” astigmatism shape, but an abnormal asymmetric shape. This patient was subsequently treated with topographic-guided ablation, which resulted in elimination of the abnormal astigmatism on topography (Figure 3), plano refraction, and 20/15 vision.
  | Figure 2 Patient 1: postoperative WFO OD. |
  | Figure 3 Patient 1: postoperative T-CAT (WaveLight, Erlangen, Germany) OD. |
Case 2
Patient 2 was a 30-year-old man who had WFO LASIK on the EX500 using an incorrect manifest axis.
- Preoperative refraction: −0.75, −4.00×20
- Postoperative refraction: +0.50, −1.25×133 with 20/25 vision
- Retrospective Contoura analysis of astigmatism: −4.27×13.
This patient had a correction that was 7 degrees off the correct axis. Due to the extent of correction, he ended up with a significant 1.25 D of astigmatism at a new axis of 13 (Figure 4). The deviation of 7 degrees multiplied by 3% results in a loss of effectiveness of ~21%, which would equal 0.88 D. This estimate is reasonably similar to the amount of astigmatism measured postoperatively, and the deviation from the axis resulted in astigmatism along a new axis of 133 degrees.
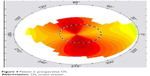  | Figure 4 Patient 2: preoperative OS. |
Figure 5 shows the new abnormal astigmatism. As this case preceded topographic-guided ablation availability, his correction was done using WFO on the EX500. He ended up with a correction of plano and 20/15 vision, but his postenhancement topography still shows remnants of the abnormal astigmatism (Figure 6). This WFO astigmatism laser ablation pattern is regular, but the induced astigmatism from the initial correction is not regular, and the end result is a residual abnormal astigmatism pattern.
  | Figure 5 Patient 2: postoperative WFO OS. |
  | Figure 6 Patient 2: postoperative WFO OS. |
Case 3
This female patient had bilateral primary WFO LASIK on the EX500. She had correction using an incorrect manifest refraction axis in the oculus dexter (OD) eye (Figure 7), and correction of astigmatism in the oculus sinister (OS) eye that was not actually present.
- Preoperative refraction:
- OD: −5.25, −1.00×115
- OS: −5.00, −0.75×88
  | Figure 7 Patient 3: preoperative OD. |
Postoperative refraction:
- OD: plano, −0.75×145
- OS: plano, −0.50×170
Retrospective Contoura analysis of preoperative Topolyzer scans:
- Measured astigmatism OD: −0.70×137
- Measured astigmatism OS: −0.09×132.
In the OD eye, the measured axis was 22 degrees different resulting in a 66% loss of effectiveness, and an induced astigmatism ~66% of the original amount along an entirely new axis. Figure 8 also shows the abnormal shape of the new astigmatism.
  | Figure 8 Patient 3: postoperative WFO OD. |
OS Contoura analysis shows that there was virtually no astigmatism present. Looking at her preoperative Contoura laser ablation pattern shows removal of coma just below her pupil. We theorized that performing her refraction in a partially lit room would have shrunk her pupil out of the area of the coma resulting in no astigmatism being present. In a dark room, or with a dilated refraction, the coma had induced the 0.50D of astigmatism, and the resulting postoperative astigmatism (Figure 9) on the perpendicular axis, and more or less regular in shape.
  | Figure 9 Patient 4: postoperative WFO OS. |
This patient was treated with topographic-guided ablation OD because of the abnormal shape of the induced astigmatism and with WFO OS as the eye had induced relatively symmetrical astigmatism. The patient had resultant 20/15 vision oculus utro with elimination of her night halo symptoms, which was her main complaint after the primary procedure.
Discussion
These cases demonstrate how new technology can advance patient care. Previously, we have had patients who had suboptimal results on seemingly simple cases. Manifest refraction has inherent technical and subjective limitations when determining the precise value for cylinder power and axis. As HOAs have become better understood, we have appreciated the difficulty in determining the correct power and axis of an irregular cornea across various pupil diameters.
Manifest refraction requires subjective input by the patient and is based on the point of least confusion in the patient’s vision. By definition, it is subject to technical and subjective errors. Furthermore, topographic-guided ablation using manifest refraction correction does not take into account the effect on astigmatism/astigmatism axis when HOAs are removed. This makes the situation even more complex, as not only can there be a new abnormal induced astigmatism when correction is done without HOA removal on the wrong manifest axis, but the lower order astigmatism axis can change when the effect of the HOAs are removed. This builds on the new understanding of the interaction of HOAs on refractive astigmatism described in Part 1 of this series.4 In fact, as mentioned in Part 1, removal of the HOAs overwhelmingly resulted in refractive astigmatism that was within 15 degrees of the 90- and 180-degree axis showing that most eyes simply do not have oblique lower order astigmatism. In other words, removal of the HOA often resulted in a different lower order astigmatism and axis, and unless the Manifest Astigmatism and Axis coincide with the Contoura Measured Astigmatism and Axis (an uncommon occurrence in our experience), correction with the Manifest Refraction will not only be incorrect but will also induce a new abnormal astigmatism, which can be visualized on topography.
Case 1 demonstrates the results of a significant amount of astigmatism treated on an incorrect axis. As shown in Figure 2, a new vector resulting in an abnormal induced astigmatism is created on an entirely different axis, and new aberrations of higher order are induced. This abnormal shape of this new astigmatism cannot be fully corrected via normal laser ablation such as WFO and would likely not be corrected with wavefront-guided ablation either, as it cannot detect and treat such topographic asymmetry.
There is a disparity in between the amount of residual astigmatism by calculation versus the amount actually present on Contoura for the enhancement. This may have to do with an inaccurate original Topolyzer scan, as only one scan was taken originally, or the fact that the residual HOAs from prior to WFO interacted with the new HOAs created and resulted in a higher correction. Since we do not have a full array of Topolyzer scans, we cannot truly know. The data are limited, but the only reason we have it is because we obtained a Topolyzer Vario over a year before receiving the ability to perform Contoura corrections. We believe we were one of the few sites to have a Vario prior to performing Contoura, and although that gives a database of treatments performed with WFO that we can retrospectively analyze, we are limited by the fact that we only took single scans as at that time we were not trained as to the need for multiple scans, or even the technique for taking scans.
Case 2 demonstrates what happens when an abnormal induced astigmatism is treated with WFO enhancement (Figure 5). Although the refraction achieved is plano and the patient’s vision is good, topographic evidence of the abnormal astigmatism remains. The abnormal astigmatism cannot be fully corrected with a normal, regular astigmatism ablation pattern. It is unknown what these topographic abnormalities cause in the way of vision, but likely there will still be some asymmetric refraction of light rays entering the cornea, causing subtle distortion, especially at night as the pupil opens further on the abnormal topography.
Topographic-guided ablation does remove the abnormal astigmatism especially if the measured Contoura astigmatism and axis are used, and as shown in Figures 3 and 10 it results in a much more uniform corneal bed in comparison to Figure 6, which shows WFO correction of an abnormal induced astigmatism.
  | Figure 10 Patient 3: post T-CAT (WaveLight, Erlangen, Germany) OD. |
Case 3 is an interesting patient who had a manifest refraction WFO correction on the wrong axis in the OD eye (Figures 8 and 10) and topographic-guided correction of the abnormal induced astigmatism (Figure 11), which led to much more uniform topography (Figure 11). The OS eye, when retrospectively analyzed with Contoura, had coma adjacent to her central cornea, and with dilation she had astigmatism measured. Retrospective Contoura analysis showed no astigmatism present, only coma, so this patient actually had astigmatism created by the coma in a dark room (or with pupils dilated) and thus ended up with an induced symmetric astigmatism on the perpendicular axis. This was successfully corrected with a WFO correction, eliminating the astigmatism (Figure 12).
  | Figure 11 Patient 4: preoperative OS. |
  | Figure 12 Patient 4: postoperative WFO OS. |
The consequences of treating astigmatism on the wrong axis have not been well documented, and the repercussions of treating on the wrong axis are important to consider for not only laser vision correction but also for all other forms of vision correction including glasses, contacts, toric intra-ocular lenses, etc.
A pair of glasses that corrects the astigmatism on the wrong axis would then have not only a decrease in the astigmatic correction of the cornea but would also induce a new irregular astigmatism every time those glasses are worn. The same with toric soft contact lenses, which have the added problem of only being commercially available with astigmatism corrected on select axes. That means that every toric soft contact lenses wearer whose astigmatism is not on the available axis would have a new induced, irregular astigmatism on a different axis while having the original axis astigmatism correction decreased. This creates very complex optical aberrations that are likely present in many patients’ vision correction.
Furthermore, manifest refractions are inherently fraught with error. The maintenance of the phoropter is typically an afterthought in many practices. It is not difficult to surmise that there may be many people walking around in corrective lenses with multiple astigmatic aberrations in their vision, and this may be another reason why so many patients with significant astigmatism have such difficulty with their correction. Conceivably, the best correction for significant astigmatism can only come from properly measured topographic-guided ablation.
The understanding of corneal astigmatism is potentially on the precipice of a new age. As diagnostic technology advances, we have better ways of imaging and eventually understanding how to best image, measure, and eventually treat not only in laser vision correction but also in vision correction in general.
Conclusion
Finally, the data in Part 3 of this series3 strongly demonstrate that removal of the astigmatism is successful using the Measured Contoura correction and the LYRA Protocol, supporting that removal of HOAs does affect the lower order astigmatism treated. If the Manifest correction is used with Contoura, and the Manifest astigmatism and axis are different than the Measured Contoura correction, significantly incorrect astigmatic correction will be performed resulting in removal of the original HOAs, inducing new HOAs, abnormal new induced astigmatism, and a less than optimal result.
Acknowledgments
The author thanks Sissimos Lemonis for inspiration and collaboration and Ron Pei, OD, for editing.
Author’s contributions
Dr Motwani was involved in the conception, design, data collection, analysis, and interpretation, as well as writing and critical revision of the paper.
Disclosure
Dr Motwani has received a grant from Alcon for a previous unrelated study. The Contoura system using the LYRA Protocol was developed by Dr Motwani in conjunction with Sissimos Lemonis of WaveLight® Lasers. The author reports no other conflicts of interest in this work.
References
Bueeler M, Mrochen M, Seiler T. Maximum permissible torsional misalignment in aberration-sensing and wavefront-guided corneal ablation. J Cataract Refract Surg. 2004;30(1):17–25. | ||
Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11(1):47–50. | ||
Motwani M. The use of WaveLight® Contoura-measured astigmatism to create a uniform cornea: the LYRA Protocol part 3: results from 50 eyes. Clin Ophthalmol. In press 2017. | ||
Motwani M. The use of WaveLight® Contoura to create a uniform cornea: the LYRAProtocol. Part 1: the effect of higher-order corneal aberrations on refractive astigmatism. Clin Ophthalmol. In press 2017. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
