Back to Journals » Clinical Ophthalmology » Volume 11
The use of Wavelight® Contoura to create a uniform cornea: the LYRA protocol. Part 3: the results of 50 treated eyes
Authors Motwani M
Received 3 February 2017
Accepted for publication 18 April 2017
Published 16 May 2017 Volume 2017:11 Pages 915—921
DOI https://doi.org/10.2147/OPTH.S133841
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Manoj Motwani
Motwani LASIK Institute, San Diego, CA, USA
Purpose: To demonstrate how using the Wavelight Contoura measured astigmatism and axis eliminates corneal astigmatism and creates uniformly shaped corneas.
Patients and methods: A retrospective analysis was conducted of the first 50 eyes to have bilateral full WaveLight® Contoura LASIK correction of measured astigmatism and axis (vs conventional manifest refraction), using the Layer Yolked Reduction of Astigmatism Protocol in all cases. All patients had astigmatism corrected, and had at least 1 week of follow-up. Accuracy to desired refractive goal was assessed by postoperative refraction, aberration reduction via calculation of polynomials, and postoperative visions were analyzed as a secondary goal.
Results: The average difference of astigmatic power from manifest to measured was 0.5462D (with a range of 0–1.69D), and the average difference of axis was 14.94° (with a range of 0°–89°). Forty-seven of 50 eyes had a goal of plano, 3 had a monovision goal. Astigmatism was fully eliminated from all but 2 eyes, and 1 eye had regression with astigmatism. Of the eyes with plano as the goal, 80.85% were 20/15 or better, and 100% were 20/20 or better. Polynomial analysis postoperatively showed that at 6.5 mm, the average C3 was reduced by 86.5% and the average C5 by 85.14%.
Conclusions: Using WaveLight® Contoura measured astigmatism and axis removes higher order aberrations and allows for the creation of a more uniform cornea with accurate removal of astigmatism, and reduction of aberration polynomials. WaveLight® Contoura successfully links the refractive correction layer and aberration repair layer using the Layer Yolked Reduction of Astigmatism Protocol to demonstrate how aberration removal can affect refractive correction.
Keywords: WaveLight Contoura, topographic guided ablation, LASIK, PRK, uniform cornea, Contoura with LYRA Protocol, measured astigmatism
Introduction
The use of topography-guided ablation with primary refractive correction (WaveLight® Contoura; WaveLight, Erlangen, Germany) (Contoura) is a relatively new concept (although it has been used for repair worldwide, primary correction is a new development), and performs two separate layers of correction: the first is the higher order aberration (HOA) removal layer to remove the natural biological aberrations found in the cornea. The second is the refractive correction layer, which treats sphere and astigmatism. Contoura has been performed thus far primarily using the manifest/cycloplegic manifest refraction (for this paper, we will consider them essentially the same – a clinician hand measured refraction), which has been our endpoint for refractive correction, no matter the modality of correction. The US Food and Drug Administration (FDA) study for Contoura approval used the manifest refraction. Topography does not provide spherical power, as eye length is not measured. Tan et al1 presented a large set of 2051 primary eyes, corrected with topography-guided ablation specifically only using the manifest refraction. In a US FDA study, Stulting et al2 also only used the manifest refraction, but the FDA approval did not specify whether manifest or Contoura measured refraction was to be used.
Building on this study, the author has theorized that there is a link (or yolk) between HOA removal and astigmatism correction, and that the Contoura processing software is able to accurately analyze this linkage. Using the manifest refraction with Contoura leaves out this critical link, that is, the removal of HOAs affects the astigmatism of the refractive correction layer.
The concept can be visualized if the cornea is imagined in three dimensions. The presence of coma, trefoil, or other aberrations on the cornea can cause astigmatism that can add to, or cancel out, the lower order astigmatism depending on the relationship to the pupil, as was demonstrated in Part 1 of this series.3 The result of these vectors can create varying astigmatic power and/or axis as measured across different pupil diameters. This can be shown in the Topolyzer Vario Fourier output, as the astigmatism graph will vary across the cornea from the central area to the periphery. The Contoura software calculates this linkage and provides a measured astigmatism and axis, which can be dramatically different from the manifest refraction.
Our hypothesis was that the Contoura measured astigmatism power and axis more accurately corrects astigmatic power and axis to create a more uniform, aberration-free cornea. We also theorized that the HOAs of the anterior cornea contribute to changing the astigmatic axis and power that a patient will subjectively accept to achieve an acceptable quality of vision. This would mean that the manifest refraction may not be the best refraction, but the best compromise resulting from the central ray of light, passing through the corneal vertex and central HOAs, that causes the least amount of visual confusion to the cerebral processing centers.
Novis4 reported a change in axis of astigmatism by 1° from the actual axis can cause a loss of 3.3% of the effect of the correction. What is not as well recognized is that when there is a discrepancy (large or small) between the “manifest” versus “measured” astigmatic power and axis, treatment of the incorrect axis and power will create a resultant new astigmatism power and axis, as is demonstrated in Part 2 of this series.5 As power and axis varies across different pupil diameters (or across the cornea), the physician is left with difficult choices on what to actually treat. This retrospective analysis demonstrates that Contoura measured astigmatism and axis treatment can fully and accurately correct corneas to make them more uniform.
Patients and methods
This was a retrospective analysis of the first 50 primary LASIK corrections of 26 patients performed by one surgeon (MM) at one center using Contoura measured astigmatism and axis (as per the Layer Yolked Reduction of Astigmatism [LYRA] Protocol) within the FDA indications of myopia up to −8.00D with astigmatism no >−3.00D. We included eyes with a myopic goal for monovision. We monitored all eyes for at least 3 months post LASIK via visual acuity, refraction, and Topolyzer Vario HOAs to determine if the eye was accurately treated and the LYRA Protocol was successful.
All surgeries were performed by one surgeon (MM) at one center in San Diego, CA, USA, using a WaveLight® EX500 with Contoura (WaveLight) and the Topolyzer Vario (WaveLight). All LASIK flaps were made with the Moria M2 Microkeratome (Moria Surgical, Antony, France) with 110 micron calibrated blades from Microspecialties, LLC, Middletown, CT, USA. All surgical planning was done using the Wavenet Server and the Contoura planning system using the LYRA Protocol, which is described below.
The measured Contoura astigmatism and axis were obtained from the surgical planning page in the Contoura planning software. This page is after the Topolyzer images are processed, and after the information is entered for the patient’s manifest refraction, pachymetry, and pupil size. On this page, the surgeon can enter their final input for sphere, astigmatism, and axis, and the effect on the ablation pattern will be shown as the values change. Zeroing out the sphere and astigmatism correction shows only the HOA removal, and the HOA pattern can be resolved. Entering the astigmatism and axis will create a pattern that can be compared with the anterior elevation of a Pentacam Scheimflug analyzer scan (Oculus, Wetzlar, Germany) (a Ziemer Gallelei [Ziemer Ophthalmic Systems, Port, Switzerland] will output similar scans). This demonstrates that using the measured Contoura astigmatism and axis creates an ablation pattern that closely matches the elimination of the anterior elevation on Pentacam, which results in a more uniform cornea.
This study included 50 eyes from 26 patients of which 10 were male and 16 were female. Patients’ ages ranged from 19 to 62 years, with an average age of 31.65 years. Preoperative evaluation included best corrected visual acuity, manifest/cycloplegic manifest refraction, anterior exam, posterior dilated exam, tonometry, pachymetry via Pentacam, autorefraction with the Nidek OPD (Nidek Co., Ltd, Gamagori, Japan), and topographic analysis with the Topolyzer Vario.
Specific attention was paid to obtaining high quality reproducible scans with the Topolyzer Vario. A patient would have 8–12 scans taken per eye, and at least 4 accurate similar scans with appropriate iris registration and complete data (as indicated by the Topolyzer Vario) were necessary to proceed with surgical planning. If the scans were too variable, or not enough scans with high quality information were taken, the scans were repeated until enough scans to create an accurate, reproducible, consistent picture were obtained. Great care was taken not to induce astigmatism when holding the eyelids open for scans, and blinks were allowed to prevent the corneal surface from desiccation.
Patients were not included if they had prior refractive surgery, could not achieve 20/20 vision preoperatively, were not within the FDA treatment parameters, had anterior segment abnormalities or findings that could affect the outcome such as keratoconus or corneal ectasia, recurring eye disease such as iritis or herpetic keratitis, severe dry eye, uncontrolled diabetes or hypertension, or were pregnant.
All patients provided written consent to have their data published in this paper.
The LYRA Protocol
This is a recognition of the fact that the aberration removal layer is yolked/linked to the refraction correction layer. Contoura calculates the results of that linkage. The protocol is as follows:
- Enter the manifest/cycloplegic refraction into Contoura during presurgical planning.
- Zero out the astigmatism and sphere to see ablation pattern for the aberration correction layer.
- Enter Contoura measured astigmatism and axis for the final correction. The ablation map at this point should be similar to the Pentacam anterior elevation map. This will assist understanding the ablation when there is a significant discrepancy between manifest versus measured astigmatic power and axis.
- The sphere is now entered after adjustment for the spherical equivalent of the change in astigmatism.
For all 50 eyes in this study, this protocol was followed exactly for treatment, with the only variation from Contoura measured astigmatism being rounding off of numbers.
During Contoura planning, excellent topographic image captured with the Topolyzer Vario was paramount. We set a requirement of having at least 4 high quality images, and preferably as many as 8 for processing by Contoura. Mean average deviation (MAD) of the astigmatic axis of ≤1° was required in the scan group sent to Contoura for processing. The Q value was left unchanged. Although the change in Q value from the ablation would theoretically induce some spherical aberration, experience has demonstrated that this is small enough in primary Contoura corrections to be ignored for the LYRA Protocol. Change in spherical aberration by the Q change must be addressed in retreatments of any kind, through the equalization of the C4 and C12 Zernicke polynomials that can be accessed on the Contoura surgical planning page. As this manuscript is mainly concerned with proving that the utilizing measured astigmatism and axis is effective, we will not address retreatments here. C4/C12 equalization is more difficult in the US with FDA approved Contoura as hyperopic Contoura is not yet approved, making equalizing C4/C12 difficult when C12 is less than C4. This equalization step has not been included in the LYRA Protocol as it increases the complexity, especially in the US, but mainly because for primary corrections the equalization is so small as to be negligible.
Results
Results for each eye were evaluated at 3 months for visual result, refractive result, and analyzed with Zernicke polynomials to quantify aberration reduction, and results were obtained for all patients except one (with 2 eyes in the study) who was away for medical school. This patient had 1 week results. The goal of this paper was to show accuracy of correction and elimination of astigmatism, and although we examined visual results, it is recognized that they would improve over time as the epithelium re-compensated and became more uniform.
Every eye of the 25 patients (50 eyes) received astigmatism treatment. The average of the absolute value of the deviation of astigmatic power from manifest to measured was 0.5462 D (range =0–1.69 D). Average amount of deviation of axis from manifest to measured was 14.94° (range =0–89). Eleven eyes had no astigmatism on manifest refraction, but had astigmatism on Contoura measured.
Forty-seven eyes were targeted for plano, 3 for monovision (−1.25, −1.25, −1.50). Of the 47 eyes targeted for plano, 44 (93.6%) were plano and 1 (3.68%) was −0.50 D. The remaining 2 had residual refractive errors of:
- Plano, −1.00×93 (Sph. Equiv =0.50)
- +0.50, −1.00×105 (Sph. Equiv =plano).
In the 47 eyes with a target of plano, all (100%) were within a spherical equivalent of ±0.50. In the 3 eyes that were corrected for monovision, one eye overcorrected and underwent enhancement of +0.75 D, and one eye with a goal of −1.25 regressed to −1.50, −0.75×150, and the final one had a goal of −1.25 and was corrected without any regression. Therefore, 49 of 50 (96%) eyes were corrected within a spherical equivalent of ±0.50 D, and one eye by 0.75 D of sphere. Only 2 eyes had residual astigmatism, thus 48 out of 50 eyes (96%) had full astigmatic correction. One eye had regression with an astigmatic component.
One patient had 2 eyes with significant residual error: plano, −1.00×93 oculus dexter (OD) and +0.50, −1.00×105 OD. This patient had an auto-refraction and manifest astigmatism of −0.75D OD, no astigmatism on auto-refraction or manifest refraction oculus sinister (OS), and no astigmatism correction in her glasses oculus utro. Her preoperative Contoura measured astigmatism was 2.55D OD, and −1.09D OS. Postoperative Contoura analysis demonstrated 0.47 D of astigmatism at 1 week, and 0.88 D at 3 weeks in OD. We determined that preoperative epithelial compensation of the aberration was responsible for the residual astigmatism, resulting in incomplete measurement of the preoperative aberration (which was trefoil).
Although visual acuity was not a primary goal, we present it here for completeness. Of the 47 eyes that had a goal of plano:
- 20/10: 3 eyes (6.38%)
- 20/15: 38 eyes (80.85%)
- 20/20: 47 eyes (100%).
Of the other 3 monovision eyes, distance vision was 20/30, 20/40, 20/70 and reading was J2 or J1.
Put simply, just about 81% of the eyes with plano correction were already at 20/15 in this limited study, and 100% of the eyes were 20/20 or better. Table 1 provides data from 10 eyes selected from the cohort of 50. Two eyes required re-treatment for incomplete correction due to high amounts of higher order aberrations, one reading eye over-corrected, and one reading eye regressed.
Astigmatism polynomials, C3 and C5 were also analyzed pre- and postoperatively at the 5.0 mm optical zone. The preoperative average at 5.0 mm for C3 was 0.1924 (range +0.6421 to −1.0966), and for C5 was 0.6889 (range +0.2854 to −2.54). This also demonstrates the well known tendency of human corneas to have with-the-rule-astigmatism. The preoperative average at 6.5 mm for C3 was 0.3190 (range 1.0017 to −1.5992), and for C5 was 1.1894 (range 1.1894 to −3.1859).
C3 and C5 values were measured preoperatively and at 3 months at the 5.0 and 6.5 mm zones, as epithelium grows from the limbus toward the center.
The postoperative average C3 at 3 months at 5.0 mm was 0.1254 (range +0.2865 to −0.5060), and the average C5 at 5.0 mm was 0.1980 (range of +0.6145 to −0.2353). The 3-month postoperative average C3 at 6.5 mm was 0.2184 (range of 0.5017 to −1.0982), and the average C5 was 0.3334 (range of 1.2317 to −0.5410).
At 5.0 mm, the average C3 was reduced by 74.33%, and the average C5 by 51.84%. At 6.5 mm, the average C3 was reduced by 86.5% and the average C5 by 85.14%.
Three patients did not have postoperative topographies of high enough quality to include their values within these calculations.
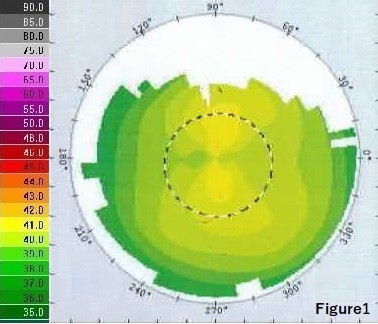
Sample case 1
- Preoperative manifest: −3.00 (Figure 1)
- Contoura measured treatment: −2.50, −1.00×179
- Postoperative 1 week: plano with 20/15 vision (Figure 2).
  | Figure 1 Case 1: preoperative topography. |
  | Figure 2 Case 1: postoperative topography. |
In this case, the patient’s aberrations were masking and offsetting the patient’s astigmatism.
Sample case 2
- Preoperative manifest: −6.50, −0.50×180 (Figure 3)
- Contoura measured treatment: −6.25, −1.00×8
- Postoperative 1 month: plano with 20/15 vision (Figure 4).
  | Figure 3 Case 2: preoperative topography. |
  | Figure 4 Case 2: postoperative topography. |
In this case, we can see the striking uniformity of the postoperative corneal topography.
Discussion
Correction via Contoura measured refraction can lead to large amounts of difference in terms of the manifest refraction. Correcting the measured refraction takes a “leap of faith” in Contoura and the linkage in between the HOA correction and the refractive correction that goes against our very training, but the effectiveness in our early experience is indisputable. The progression from manifest to measured took some time and thought. It began with the experience of one of the contributors (SL) treating irregular and ectatic corneas with manifest refraction. The result was unpredictable, so the treatment for some time was conservative, treating only the HOAs and disregarding the refractive correction. The experience postoperatively was that the residual astigmatism was often similar to that calculated by the topography-guided software preoperatively. In an effort to interpret these observations, MM followed up with carefully planned treatments on selected patients having particular suitable manifest and measured refractions, where part of the difference between measured and manifest astigmatism was treated, and the measured axis was used. The results were quite good, and upon analyzing the results, it was determined that full measured correction should be used.
A pattern emerged where coma and other aberrations such as trefoil would shift a patient’s subjective cylinder and axis because the HOA can cause an increase or decrease in astigmatism depending on the interaction with the astigmatism. Historically, if the corneal astigmatism did not match the refractive astigmatism, it was deemed to be by “exclusion” lenticular astigmatism. The effect of the LYRA Protocol led to the new understanding of higher order aberrations as demonstrated in the first two parts of this series.3,5
The goal of this article was to show the accuracy of the results in eliminating astigmatism, which the results demonstrate was very effective. Even though there was a significant amount of deviation between measured and manifest astigmatic power (over 0.5 D) and axis (14.94°), astigmatism was completely treated in 48 of 50 eyes, with one of those 48 eyes later showing regression with an astigmatic component. Furthermore, 11 eyes had no astigmatism on manifest refraction, but had astigmatism on measured Contoura analysis. If the LYRA Protocol had not been correct, we simply would not have seen the accurate results obtained.
The visual results are dramatic, with 80.85% of distance eyes achieving 20/15 vision, 100% achieving 20/20 vision, and 6.4% achieving 20/10 vision. The patient who had under-correction of her aberrations and refractive astigmatism immediately postoperatively still achieved 20/20 vision even with astigmatism present in both eyes. This confirms what we experience clinically, that achieving 20/20 vision does not mean a patient is fully corrected. The results of this study thus far may indicate that if the cornea is freed of aberrations, most retinal neuroreceptor density may achieve 20/15 vision, and with the LYRA Protocol, 20/15 will be the new normal rather than 20/20.
It is notable that only 3 eyes have achieved 20/10 thus far. Although with further healing time and epithelial uniformity, we expect that 20/10 rate to improve; it is notable that clinically in San Diego, we saw one of the worst allergy seasons this summer and fall, and during certain periods 2 of 3 patients walking into the office had irritation of their eyelids. This is notable as we began to see a pattern where untreated allergic conjunctivitis would cause a patient to measure at least a line worse on the Snellen chart than when treated. To avoid this limitation in future studies, it may be wise to place a punctal plug in each eye to obtain environmentally untainted results, as this effect may have delayed more patients from achieving 20/10, or even 20/15.
Examination of the astigmatism polynomials yielded some interesting results. The preoperative C3 and C5 numbers at both 5.0 and 6.5 mm showed lower amounts of astigmatism at C3 than C5, which demonstrates the tendency of human corneas to have with-the-rule-astigmatism. At 3 months, at 5.0 mm, we see an average of 74% of aberrations on the C3 axis, and about 52% on the C5 axis. The reduction at 6.5 mm at 3 months is significantly higher, at 86.5% on the C3 and 85.14% on the C5 axis. This seems to correspond with the tendency of human corneas to heal from the periphery to the center, and we expect 6-month values to be better in the 5.0 mm optical zone. We will be re-examining the data for these patients at 6 months and at 1 year, and should be able to determine how long it takes for the corneal epithelium to become its most uniform, and then determine the maximum aberration removal. We know some masking of aberrations by the epithelium will be occurring, and only time and examination of the polynomial data will tell us if we need to incorporate any corrective measures to increase aberration removal. A further limitation of the process was that my staff generally has been used to taking multiple preoperative Topolyzer scans, but not postoperatively, and this limited some of the data we were able to gather. We plan to increase the number of scans when we report back on follow-up longer-term data to ensure good data acquisition.
The aberration data support a higher average aberration removal at C3 and C5 at the 6.5 mm optical zone than the 5.0 mm OZ. As new epithelium grows from the limbus to the center, we expect this number to improve over time as the central area becomes more uniform and smoother, and this may be why our 20/15 rate is so much higher than our 20/10 rate also, or it may be that most humans do not have the retinal neuroreceptor density to achieve 20/10. Nevertheless, we may see the 20/10 rate go up with 6-month or 1-year long data, and the 20/15 rate continues to improve over time as the epithelium becomes more uniform.
The most striking parts of Contoura correction were the almost perfect uniform topographies that many of these patients had. They are so featureless, that it appears as if the topography was taken by an artificial lens rather than a human cornea. Of those patients that did not have these almost perfect corneas, it was not difficult to see how much smoother the overall contours of the cornea were. Only time will tell if uniformity will increase due to epithelial re-compensation over time on those corneas, and how much residual uniformity will remain from small amounts of epithelial masked aberrations. We have seen small amounts of residual astigmatism on the Contoura analysis of 3-month topographies, but we may also find that epithelial re-compensation actually will mask these residual aberrations. We estimate that 6-month topographies should be much more consistently uniform.
The effect of aberration removal is essentially removal of the anterior elevations shown on a Pentacam analysis of the anterior surface. This is akin to a rigid gas permeable lens, which creates a uniform surface via a rigid anterior surface and a tear sandwich layer underneath masking the corneal aberrations. With Contoura measured correction, we are removing those aberrations, essentially correcting the inverse of the tear sandwich layer. This has the impact of providing not only excellent, detailed day vision, but we have noticed a striking absence of halos/night glare in the majority of these patients in as little as a few days postoperatively. The subjective improvement in quality of vision is what I have noticed most in my practice. Many patients describe headlights and light sources as pinpoint. Some patients had trouble answering if they have any halos or night glare, responding either that they had not noticed any at all, or even at times asking what a halo was. Creating a uniform cornea virtually eliminates the main focusing part of the eye as a limiting factor, thereby making retinal photoreceptor density the main limiting factor for resolution of vision, along with the smaller factors of posterior corneal astigmatism, lens flaws, and retinal astigmatism.
Critical to all of this is excellent Topolyzer Vario image capture. If there was too great a disparity in images, we obtained more images. Proper uniformity of the cornea can only come from at least 4 high quality Topolyzer Vario images with very small degrees of MAD of axis (1°) and dioptric variation (0.50 D). Good technician training resulted in very little dioptric difference between scans, and careful elimination of aberrant quality images almost always resulted in at least 4 images with a MAD of only 1° of axis. We would normally take at least 8–12 images, and perform comparisons for similarity and to eliminate those that were not consistent. Great care must be taken to not artificially induce astigmatism on Topolyzer Scans by pressing on the globe while opening the eyelids.
Uniform human corneas are uncommon to find naturally. The LYRA Protocol creates more uniform corneas, and it also allows better vision. No other vision correction modality (save a properly fitting RGP lens), whether glasses, contacts, normal or wavefront-guided LASIK, small incision lenticule extraction, implantable contact lenses, or intraocular lenses are able to correct vision this way. This would be the first vision correction modality, again save perhaps RGP lens, that is not an equivalent, but potentially better. This, in itself, would be a revolution in laser correction, as for the first time, we would have a procedure that could allow the full potential of the eye to be reached, and actually allow the refractive surgeon to tell the patient that Contoura excimer laser ablation with the LYRA Protocol has the potential to achieve better vision than virtually any other modality of vision correction. Although lens flaws and posterior corneal astigmatism may be present, we believe that they may play a smaller role than originally thought. If these latter factors do not affect the vision significantly, then the major limitation on vision clarity, acuity, and resolution would be retinal neuroreceptor density. Again, further study will show where the limitations of the power of this procedure and protocol reside.
We have not attempted to compare the outcomes of this to the FDA study2 nor to a similar group of wavefront optimized outcomes. That can be compared in later studies, as this manuscript was designed to show proof that the seemingly disparate Contoura measured astigmatism and axis (as opposed to manifest refraction) can be utilized to create laser corrections that are safe, effective, eliminate astigmatism effectively, and result in excellent vision. We consider this series of articles just the first chapter in a paradigm shift in laser vision correction.
Acknowledgments
Acknowledgments go to Sissimos Lemonis (SL) for inspiration and collaboration; and to Ron Pei, OD, for editing.
Author contribution
MM was involved in the conception, design, data collection, analysis and interpretation, as well as writing and critical revision of the manuscript.
Disclosure
Dr Motwani has received a grant from Alcon for a previous unrelated study. The Contoura system using the LYRA Protocol was developed by Dr Motwani in conjunction with Sissimos Lemonis of Wavelight Lasers. The author reports no other conflicts of interest in this work.
References
Tan J, Simon D, Mrochen M, Por YM. Clinical results of topography-based customized ablations for myopia and myopic astigmatism. J Refract Surg. 2012;28(11 Suppl):S829–S836. | ||
Stulting RD, Fant BS; Group TCS. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42(1):11–18. | ||
Motwani M. The use of WaveLight® Contoura to create a uniform cornea: the LYRAProtocol. Part 1: the effect of higher-order corneal aberrations on refractive astigmatism. Clin Ophthalmol. In press 2017. | ||
Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000;11(1):47–50. | ||
Motwani M. The use of Wavelight Contoura-measured astigmatism to create a uniform cornea: the LYRA Protocol part 2: the consequences of treating astigmatism on an incorrect axis via excimer laser. Clin Ophthalmol. In press 2017. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

