Back to Journals » Medical Devices: Evidence and Research » Volume 10
The use of Invos™ somatic oximetry to measure variations in placental tissue oxygenation in laboring healthy term parturients with epidural analgesia: an observational study
Authors Loubert C, Ouellette M, Zaphiratos V, Tanoubi I
Received 31 August 2017
Accepted for publication 19 September 2017
Published 25 October 2017 Volume 2017:10 Pages 253—256
DOI https://doi.org/10.2147/MDER.S150472
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Christian Loubert,1 Mélissa Ouellette,2 Valérie Zaphiratos,1 Issam Tanoubi1
1Department of Anesthesia, Maisonneuve-Rosemont Hospital, CIUSSS-de-l’Est de l’île de Montréal, University of Montreal, Montreal, 2Department of Anesthesia, Saint-Jerôme Hospital Center, CISSS des Laurentides, Saint-Jerôme, QC, Canada
Purpose: Near-infrared spectroscopy provides a non-invasive continuous real-time monitoring of tissue oxygen saturation. As uterine contractions during labor may be associated with a transient uteroplacental hypoperfusion, this prospective, observational study investigates the ability of near-infrared spectroscopy to detect variation in uteroplacental oximetry during uterine contractions.
Patients and methods: Four Invos™ oximetry probes (Medtronic®, Minneapolis, MN, USA) per subjects were applied on the placental surface (PLA), the abdomen (MYO), the forearm (ARM) and the leg (LEG), of twenty healthy laboring parturients with epidural analgesia. Measurements of mean tissue oxygen saturation and area under the curve (AUC) were made during 60 minutes. The primary outcome was the difference of the AUC measurements between the PLA probe and the MYO probe.
Results: The AUC values for the PLA and MYO probes were not different. The mean saturation values recorded by the PLA probe were not different from the other probes.
Conclusion: The Invos monitor was unable to detect variations in uteroplacental saturation during labor in healthy parturients.
Keywords: near-infrared spectroscopy, uteroplacental perfusion, Invos™ monitor, tissue oxygenation
Introduction
Obstetric decision-making algorithms to evaluate the fetus well-being and assess the indication for cesarean delivery could benefit from the near-infrared spectroscopy (NIRS), as a continuous, non-invasive, real-time monitoring of fetal oxygen delivery. The rationale behind its use follows the idea that the uterine contractions during labor cause a cyclic, transient reduction in myometrial and uteroplacental blood perfusion, and could therefore serve as an in vivo human clinical model of transient uteroplacental hypoperfusion which could be detected by variations in tissue oxygen saturation.1
The primary objective of this novel concept is to evaluate the feasibility and the usefulness of the NIRS to detect the variations in the uteroplacental oxygen saturation during the contraction.
Patients and methods
After approval by the Maisonneuve-Rosemont Hospital Research Ethics Committee (approval # 12117) and written informed consent received, a convenience sample of 20 laboring healthy (American Society of Anesthesiologists physical status II) term parturients were included, between April and July 2013, according to the following inclusion criteria: normal pregnancy, anterior placenta, planned vaginal birth, term pregnancy (≥37 weeks of gestation), and desire for epidural analgesia. Patients were excluded if they presented with exclusion criteria: contraindication to neuraxial analgesia, utero-placental insufficiency as diagnosed by the attending obstetrician, abruptio placentae, abnormal placentation, twin pregnancy, planned cesarean delivery or unplanned cesarean delivery, morbidly obese patient and refusal to participate. Demographic data such as age, height, weight, parity, color of the skin and position of the placenta were collected at the clinic.
In the labor ward, the attending anesthesiologist performed a standardized epidural at the L2–L3 or L3–L4 interspace upon maternal request. Maternal blood pressure, heart rate and pulse oximetry were collected every 5 minutes until the end of the study. The fetal heart rate as well as the frequency and length of uterine contractions were measured with a cardiotocographic device every 5 minutes. A control ultrasound was performed by an experiment investigator to delineate the location of the placenta and measure the distance between the skin and the uterine edge of the placenta.
Four Invos (In-Vivo Optical Spectroscopy) cerebral/somatic oximetry adult SomaSensor™ probes (Medtronic®, Minneapolis, MN, USA) were applied on each patient to measure tissue oxygen saturation. The first probe (PLA) was placed on the maternal abdomen in a position that was directly above the ultrasound delineated uterine placenta. A second probe (MYO) was applied on the right side of the abdomen on the anterior axillary line outside the delineated placental surface. A third probe (ARM) was applied on the anterior right forearm on the mid-radial line. This probe served as a control for tissue oxygen saturation in a zone devoid of epidural-induced sympathetic alteration. A last probe (LEG) was placed on the anterior surface of the right thigh on the mid-femoral line. This probe served as a control for tissue saturation in a zone potentially affected by an epidural-induced sympathetic alteration. During 60 minutes, tissue oxygen saturation readings were recorded for all 4 probes while the subjects were breathing room air (30 minutes) and 100% oxygen through a Ventimask® (30 minutes).
The Invos monitor is allowed to measure the oxygen saturation of tissues in a 1.5 cm3 sample located ~1.7 cm under the skin’s surface.2 Extensive reviews of the mechanisms underlying Invos NIRS technology are provided in several articles.3–5 The Invos monitor provides cumulative tissue oxygen saturation every 5 seconds below a baseline threshold – the area under the curve (AUC) measure (mm%) – for 3 of the 4 probes (PLA, MYO, ARM). The rationale for using the AUC measure in this study is that during uterine contractions the transiently reduced oxygen delivery-to-extraction ratios could be detected as an increase in the AUC values for these organs in comparison with non-myometrial or non-uteroplacental tissue, such as skeletal muscle.
The primary outcome for this feasibility study is the difference of the AUC measurements between the PLA probe and the MYO probe. Secondary outcomes are the difference in mean tissue saturation values for each probe, and associations between clinical factors (color of skin, skin-to-placental distance, oxytocin administration) and AUC measurements.
An analysis of variance for repeated measures test with Bonferroni’s multiple comparison test was applied,when data were normally distributed. Clinical trial registry: Clinicaltrial.gov (NCT01834599).
Results
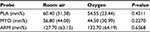
Subject characteristics are shown in Table 1. Table 2 reports AUC results for each probe. There was no difference between the AUC values for the PLA and MYO probes at room air, nor on 100% oxygen.
  | Table 1 Subjects characteristics Notes: aMean (standard deviation), bMedian (interquartile range), cN (%). Abbreviation: S-P, skin-to-placenta. |
Breathing 100% oxygen did increase the mean tissue oxygen saturation values from breathing room air as measured by all of the probes. The lowest mean tissue oxygen saturation value was recorded by the LEG probe. The mean oxygen saturation value (%) from the MYO and PLA probes did not differ, without oxygen (79.22 [9.81] vs 82.86 [9.10], P=0.1143) or with oxygen (83.07 [9.29] vs 85.67 [9.27], P=0.4226). The mean tissue saturation value for the LEG probe was lower than the MYO probe, without oxygen (70.86 [7.68] vs 82.86 [9.10], P=0.0003) and with oxygen (73.05 [8.09] vs 85.67 [9.27], P<0.0001).
In 12 subjects, the ARM probe showed increased oxygen saturation values with each uterine contraction. The contraction had no effect on oxygen saturation values for the other probes. The skin-to-placental distance, the skin color and the administration of oxytocin did not influence the AUC measurements for any probe.
Discussion
Our study found lack of variation in tissue saturation with uterine contractions for the placenta and the myometrium.
Our hypothesis was that the PLA probe would measure placental blood flow in the intervillous space, where feto-maternal gas exchange takes place. We suggested that this would have proven more likely in subjects where the distance between the skin and the myometrial-placental edge, as measured by the ultrasound examination, was <1.7 cm.
This study had specific technological limitations, such as the skin-to-placenta distance of 1.7 cm or less in 65% of the subjects, the presence of bony structures, which is not taken into consideration in the calculation algorithms included in the Invos monitor, and the fact that the Invos was originally created to function on tissues where the blood network is predominantly venous, which contrasts with the unique anatomy of the placenta as a large arterio-venous shunt. The findings of our study were negative and it is thus difficult to know whether it is because there is truly no change in uteroplacental blood flow, or whether the Invos technology is simply unable to accurately determine the uteroplacental blood oxygen saturation.
Yet, assuming the accuracy of the Invos, other explanations for our negative results could be proposed. First, reduced tissue vascular resistance, induced by the epidural sympathetic blockade, leading to an increase in regional blood flow would result in an increase in tissue saturation.5 Second, Brar et al suggested that fetoplacental blood flow is uninterrupted during uterine contractions,6 this is supported by Fairlie et al who showed that there was no change in the fetal umbilical artery pulsatility index as labor progressed in healthy parturients with a normal fetal heart rate,7 and despite a reduction in uteroplacental blood flow with uterine systole, placental oxygen delivery exceeds fetal oxygen extraction.8 So, under such excessive blood flow, it is possible that small variations in the oxygen delivery-to-extraction ratio may cause negligible shifts in placental pO2 and tissue saturation.9,10
Our study should be repeated in laboring pre-eclamptic women, especially when intrauterine growth restriction is present or when labor is complicated by fetal bradycardia. In these parturients, uteroplacental blood flow may be significantly impaired and the oxygen delivery-to-extraction ratio may be pathological, translating into wider shifts in placental pO2 between uterine contractions. These patients may constitute a better model for transient uteroplacental hypoperfusion, which may be detected by the Invos monitor.
Acknowledgment
None of the authors received funding for this study. Medtronic (Minneapolis, MN, USA) provided 20 sets of Invos for this trial but was not further involved in the elaboration of the protocol, conduct of the study or collection and analysis of the data.
Disclosure
The authors report no conflicts of interest in this work.
References
Sato M, Noguchi J, Mashima M, Tanaka H, Hata T. 3D power Doppler ultrasound assessment of placental perfusion during uterine contraction in labor. Placenta. 2016;45:32–36. | ||
Ohmae E, Ouchi Y, Oda M, et al. Cerebral hemodynamics evaluation by near-infrared time-resolved spectroscopy: correlation with simultaneous positron emission tomography measurements. Neuroimage. 2006;29(3):697–705. | ||
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103(Suppl 1):i3–13. | ||
Ward KR, Ivatury RR, Barbee RW, et al. Near infrared spectroscopy for evaluation of the trauma patient: a technology review. Resuscitation. 2006;68(1):27–44. | ||
Denault A, Deschamps A, Murkin JM. Le monitorage par oxymétrie cérébrale en anesthésiologie. Anesthésiologie Conférences Scientifiques. 2008;7(2). | ||
Brar HS, Platt LD, DeVore GR, Horenstein J, Medearis AL. Qualitative assessment of maternal uterine and fetal umbilical artery blood flow and resistance in laboring patients by Doppler velocimetry. Am J Obstet Gynecol. 1988;158(4):952–956. | ||
Fairlie FM, Lang GD, Sheldon CD. Umbilical artery flow velocity waveforms in labor. Br J Obstet Gynaecol. 1989;96(2):151–157. | ||
Wilkening RB, Meschia G. Fetal oxygen uptake, oxygenation, and acid-base balance as a function of uterine blood flow. Am J Physiol. 1983;244(6):H749–H755. | ||
Lee W, Rokey R, Miller J, Cotton DB. Maternal hemodynamic effects of uterine contractions by M-mode and pulsed-Doppler echocardiography. Am J Obstet Gynecol, 1989; 161(4):974–977. | ||
Anim-Nyame N, Sooranna SR, Johnson MR, Gamble J, Steer PJ. A longitudinal study of resting peripheral blood flow in normal pregnancy and pregnancies complicated by chronic hypertension and pre-eclampsia. Cardiovasc Res. 2001;50(3):603–609. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.