Back to Journals » Advances in Medical Education and Practice » Volume 13
The Status of Respiratory Care Education in Saudi Arabia: A National Survey of Program Directors
Authors Almeshari MA , Alshehri Z, Alqahtani JS , Alasmari AM , Alzahrani AA, Alahmadi FH , Alsulayyim AS , Alenezi FK , Alwadeai KS
Received 31 January 2022
Accepted for publication 24 May 2022
Published 10 June 2022 Volume 2022:13 Pages 619—628
DOI https://doi.org/10.2147/AMEP.S360658
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Mohammed A Almeshari,1,2 Ziyad Alshehri,3 Jaber S Alqahtani,4 Ali M Alasmari,3 Ahmed A Alzahrani,3 Fahad H Alahmadi,3 Abdullah S Alsulayyim,5 Faraj K Alenezi,6 Khalid S Alwadeai1
1Rehabilitation Health Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia; 2Institute of Inflammation and Ageing, University of Birmingham, Birmingham, UK; 3Department of Respiratory Therapy, College of Medical Rehabilitation Sciences, Taibah University, Madinah, Saudi Arabia; 4Department of Respiratory Care, Prince Sultan Military College of Health Sciences, Dammam, Saudi Arabia; 5Department of Respiratory Care, College of Applied Medical Sciences, Jazan University, Jazan, Saudi Arabia; 6College of Applied Medical Sciences, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Correspondence: Mohammed A Almeshari, Rehabilitation Health Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia, Tel +966 11 469 3593, Email [email protected]
Background: Respiratory Care Practitioner (RCP) is a vital healthcare professional in Saudi Arabia (SA). Many factors regarding the education of RCPs in SA are unknown, including the number of active institutions, levels of education and barriers to promoting the profession.
Methods: A cross sectional-based survey was conducted between June 1st, 2020 and September 20th, 2020 in SA to explore the status of RCPs education. Institutions that offered RCP programs were identified through the Ministry of Education and Ministry of Defense academic programs websites. The RCP program directors were invited to participate in an electronic survey.
Results: Among the 74 institutions searched, 23 indicated that they offered RC programs. Only 13 (56.52%) responded to the survey. Among all programs, four (17.39%) were inactive, 17 (73.91%) were governmental institutions, and only one (4.35%) obtained a national accreditation. From the 13 respondents, there were 1297 students enrolled and 123 full-time faculty members. None of the institutions reported offering postgraduate RC degrees. The respondents reported many barriers; however, shortage of staff (76.92%), lack of postgraduate programs (69.23%), lack of research activity (69.23%), and ineffective communications between institutions (61.54%) were the most reported barriers.
Conclusion: The RC education in SA is developing but not well distributed throughout the country. The shortage of staff and the limited number of postgraduate degree holders potentially contributed to the delay in establishing postgraduate RC degrees, obtaining accreditation, and implementing subspecialties to advance the profession in terms of research and quality of care.
Keywords: respiratory care, education, respiratory therapy, Saudi Arabia
Background
Respiratory care practitioners (RCPs) are professionals who provide essential and life-saving healthcare services that are related to the pulmonary system. Respiratory care (RC), sometimes referred to as respiratory therapy, is a profession that first started in the US and became a distinct specialty among different professions in the 1950s.1 Following this and over the years, the scope of the RC profession has expanded to manage patients with cardiorespiratory conditions using highly advanced respiratory care approaches, such as mechanical ventilation (MV), pulmonary rehabilitation, and pulmonary function diagnostic tests.2
The Ministry of Health (MoH) in SA was formed in the early 1950s, yet the first RC service started in SA within a tertiary hospital in Riyadh in 1975.3 The first RC service in SA was established by the Medical Services Directorate (MSD), a health service provider from the Ministry of Defense (MoD), which has also provided education and training for the RC workforce.4 Since then, several educational initiatives, including the establishment of new RC programs and scholarships, have been launched to develop qualified RCPs to meet the growing need for RC services in SA.4
In SA universities, RCPs educational programs are established after approval from the university’s council. Academic programs apply for accreditation through the National Center for Academic Accreditation and Evaluation (NCAAA). Graduates are then credentialed and registered through the Saudi Commission for Health Specialties (SCFHS).
One of the significant milestones that promoted the profession was when the Central Board for Accreditation of Healthcare Institutions (CBAHI), the national accreditation body of healthcare providers in SA, recognized the importance of the profession and established that having an RC department with qualified RCPs as a standard in the hospital accreditation process.5 Moreover, SCFHS, the national credentialing and registry of health care professionals in SA, has recognized the profession and established 12 subspecialties (respiratory adult critical care, respiratory pediatrics critical care, respiratory neonatal care, respiratory general care, emergency room and trauma, respiratory cardiac, respiratory laboratory, respiratory sleep, respiratory education and discharge planning, respiratory assistant, respiratory home care, and pulmonary rehabilitation).6 Indeed, the demand for RC services is increasing since acute and chronic respiratory-related diseases are leading causes of disability and mortality worldwide, increasing health and economic burden.7 According to a national survey published in 2015, there were 1477 active RCPs in SA, and only 25% of them were Saudi nationals.8 Additionally, the study found that among the 411 hospitals surveyed, only 88 provided RC services by RCPs, showing a considerable gap in the profession for optimal care. In those hospitals, RCPs mostly worked in critical care areas. The typical ratio for ventilated patients to RCP was previously reported to be 5:1.9 As stated by the most recent MoH data published in 2018, there were 494 hospitals across SA in which there were 8532 intensive care unit (ICU) beds in all healthcare sectors. That number increased during the coronavirus disease 2019 (COVID-19) pandemic. Therefore, the need for RCPs is high due to their critical role in managing patients with respiratory-related diseases.
However, the status of RCPs education in SA has not been studied to provide insight into the current situation and plans following the Saudi Vision 2030, of which to “ensure alignment of educational outputs with labor market needs” is an objective. Therefore, this study aims to explore and evaluate the status of RCPs educational programs, teaching and training characteristics, and potential barriers.
Methods
A cross sectional-based descriptive survey was conducted in SA between June 1st and September 20th of 2020. The electronic survey was developed by MAA, ZDA, JSA, and FHA to investigate RCP educational programs’ status in SA. The first version of the survey was pretested and piloted for face and content validity, flow, and clarity by four of the research group (AMA, AAZ, ASA, and KSA). The feedback on the form was used to improve the content of the survey’s questions before data collection. Institutions were searched through the Ministry of Education (MoE) official website, and each institution was searched for an RC department or program. Additionally, the academic programs of the MoD were searched for possible institutions.
To explore geographic outreach, if an institute has multiple campuses, each campus was considered a separate institution. The survey was sent via email to the department chairpersons or program directors. The survey included items regarding the current level of education offered; current faculty members employed (full time and part time); barriers to enrolling more students; characteristics of faculty members in terms of gender, level of education, work allocation, and scholarship status. For research purposes, those who contributed to the educational process, such as giving lectures, laboratory based teaching, or clinical training, were considered faculty members. Additionally, the survey contained items regarding the accreditation status of institutions, teaching techniques, and clinical competencies based on the SCFHS subspecialties. Finally, the survey included questions regarding barriers and possible solutions to advancing the RC profession in SA. The study was approved by the Research Ethical Committee (REC) at the College of Medical Rehabilitation Sciences of Taibah University (#CMR-RT-2020-06).
Data Collection and Analysis
The data collection was done using Microsoft Forms, and the data was exported and compiled by MAA using Microsoft Excel (Office 365) software. Due to the nature of the survey, descriptive statistics were assessed using frequencies and percentages. No statistical analysis was performed due to the aggregate nature of the data.
Results
Institutions Across SA and Response Rate
In the 74 institutions searched through the MoE and MoD, 23 RC programs were identified, of which five were private institutions. Table 1 presents a list of the identified public and private institutions and their current enrollment status. All departments chairperson or program directors were contacted, and only 13 (56.52%) completed the survey. Table 2 lists the overall characteristics. Among the institutions that did not respond to the survey, three (13.04%) have indicated that the departments were inactive on their institution websites. Of the 13 regions in SA, six (46.15%) did not have an institution offering RC educational programs. Figure 1 shows a map with the number of institutions across SA cities and regions.
 |
Table 1 Respiratory Care Public and Private Institutions Across Saudi Arabia |
 |
Table 2 Characteristics of the Institutions |
Degrees Offered and Student Characteristics
Only one institution offered a diploma degree (referred to as an associate degree in some countries). One offered a Bachelor’s (BSc) degree bridging program, where diploma degree holders can continue their education to get a BSc degree. Twelve institutes offered a BSc degree, and none of the respondents offered postgraduate degrees such as Master’s (MSc) or Doctor of Philosophy (PhD) degrees. In the previous five years, the 13 institutions had stated graduating a total of 1206 students. At the time of the survey, 1297 students were enrolled in RC programs. Respondents have stated that 1873 students are expected to graduate in five years. Compared to female students, the present study showed that more male students have graduated in the past five years (56.22%), are currently enrolled (62.07%), and are expected to graduate in five years (57.34%).
Faculty Members
Institutions stated that there were 123 faculty members with different degree levels and 39 part-time faculty members. Fifty-seven faculty members are currently on scholarship, of which 13 (22.81%) were studying MSc degrees, and 44 (77.19%) were studying PhD degrees. Similar to students, male faculty members were found to constitute most faculty members, accounting for 77 (62.60%) compared to female faculty members accounting for 46 (37.40%). Regarding the faculty members’ level of education, 37 (30.08%) were BSc degree holders, 51 (41.46%) were MSc degree holders, and 35 (28.46%) were PhD degree holders.
Quality Assurance
Only one (7.69%) institution reported being accredited by the NCAAA and another one (7.69%) by the SCFHS (the accreditation body for diploma programs). Seven (53.85%) institutions reported that accreditation by the NCAAA was ongoing, whereas the remaining three (23.08%) institutions reported that no accreditation was pursued at the time of completing the survey. Internationally, only one (7.69%) institution reported being recognized by the International Council for Respiratory Care, although it was not accredited by NCAAA.
Educational Characteristics
Twelve (92.31%) institutions reported having a research course as part of the curriculum. Problem-based learning is implemented in seven (53.85%) institutes. Ten (76.92%) institutions implemented clinical simulations in teaching. Only two (15.38%) institutions reported not having any laboratory when the survey was completed, of which one was inactive; however, that institution reported that a laboratory was being developed. The following laboratories were used in teaching as reported by the remaining institutes: 11 (84.61%) patient assessment laboratories, 10 (76.92%) simulation laboratories, 10 (76.92%) MV laboratories, seven (53.85%) pulmonary function testing (PFT) laboratories, six (46.15%) sleep disorders laboratories, four (30.77%) pulmonary rehabilitation laboratories, and one (7.69%) cardiopulmonary laboratory. Figure 2 shows the number of laboratories used by the institutions.
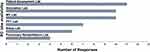 |
Figure 2 Respiratory care-specific laboratories that institutions are utilizing in teaching and training. |
Faculty Member to Student Ratio and Expected Growth
At the time of the survey, the overall faculty to student ratio ranged from 1:6 to 1:37, with a median ratio of 1:11. The male faculty member–male student ratio was slightly lower (1:10) than female faculty members–female students (1:11). The programs’ directors stated that in the following five years of completing the survey, there was an expected growth of 44.41% in enrollment. Nevertheless, faculty members currently on scholarship are expected to join the workforce in the following five years, increasing the current workforce by 46.34%. With the expected growth in faculty members and students, the overall faculty member–student ratio will be reduced to 1:10.
Barriers and Solutions for Developing the RC Profession
Many barriers were reported by the respondents (n=13) as major barriers to the development of the RC profession in SA, including shortage of faculty members (n=10) 76.92%, lack of postgraduate programs (n=9) 69.23%, lack of research activity (n=9) 69.23%, ineffective communication between institutions (n=8) 61.54%, and inactive roles of subspecialties (n=8) 61.54%. Figure 3 shows the numbers of responses regarding barriers to the development of the RC profession as reported by the program directors. Additionally, the respondents have reported the following as possible solutions to the barriers to the development of the RC profession: establishing RC departments in all government and private hospitals (n=12) 92.31% and expanding the scope of the RC practice (n=10) 76.92%. Figure 4 shows the number of responses regarding solutions to the barriers reported by the programs’ directors.
 |
Figure 3 The number of responses on barriers or limitations of advancing the respiratory care profession. |
 |
Figure 4 The number of responses on proposed solutions for expanding the respiratory care profession. |
Discussion
To the best of the authors’ knowledge, the present study is the first to explore the status of RCPs education in SA. RCPs education in SA is developing but not well distributed throughout the country. Most institutions are governmental, and only one obtained national accreditation from the NCAAA. At the time of the survey, the highest academic degree offered is a BSc degree. Male faculty members and male students are greater in numbers than their female counterparts. Shortage of staff, lack of postgraduate programs, and lack of research activity were identified as the major barriers to the development of the RC profession.
Among the 13 regions of SA, the Northern regions (Hail, Aljouf, Tabuk, and Northern Border), and southern regions (Najran and Albaha), do not have an institution that offers RC degrees. The lack of RC institutions in those regions resulted in a small number of hospitals providing RC services by respiratory therapists.8 Therefore, establishing RC institutions in those regions offers several benefits, such as creating new opportunities for recruiting local RCPs that cover the hospitals’ demands and provide high-quality RC services.
Although RCPs are mostly needed at the bedside, there is an increasing demand for other practice areas, such as managers, researchers, and academics with postgraduate degrees, to participate as leaders and educators for the growing workforce. Postgraduate degrees may help develop leadership and advanced research skills that may not be possible in undergraduate education. It was previously reported that postgraduate degree holders are more successful in publishing, presenting, and teaching than undergraduates.10 Moreover, a recent report on the competencies needed by RC graduates included the ability to review and critique scientific literature and apply evidence-based medicine into practice.11 To the best of our knowledge, no academic graduate degrees in RC are offered in SA. However, efforts have been made to develop a professional postgradute RC diploma program that the SCFHS has recently approved. The program requires RCPs to perform clinical rotations for two years in specific RC practice areas, such as adult, neonatal, or pediatric ICUs and then get credentialed as senior practitioner after additional two years of experience.
In the presented study, the overall faculty member–student ratio may seem low (1:11), but this was found to be higher than what was reported in the US (1:5).12 There was also a wide disparity between responding institutes, with the ones that are not in the major cities of SA (Riyadh, Dammam, Jeddah) having a higher faculty member–student ratio. A decrease in the faculty member–students ratio is advised, especially in clinical and medical teaching. A previous report suggested a significant correlation between the reduction of the faculty member–student ratio with the passing rates in the clinical simulation exams.13 This confirms the programs’ directors report on the shortage of faculty members as a barrier to advancing the RC profession in SA. Therefore, increasing students’ enrollment in existing programs is warranted given that the faculty member–student ratio is kept low.
Another main area of concern in the status of RCPs education is the lack of external accreditation for most RCPs programs. Accreditation is a critical part of health professions’ education.14,15 The lack of accreditation may impact the graduates’ competencies and variation in graduates’ skills and patient care. Indeed, this may also be influenced by the discrepancies in educational styles. Therefore, benchmarks should be developed and implemented by institutions, NCAAA and the SCFHS to continually evaluate output quality. Nevertheless, the SCFHS have recently developed a standardized test for credentialing degrees instead of the previous credentialing method (interview-style evaluations), which should help advise institutions on how well their graduates performed.
The lack of accreditation may have contributed to the significant discrepancies in laboratories utilizations, which is essential in developing the students’ psychomotor and clinical skills. Several institutions lack essential laboratories, such as MV and PFT laboratories. Furthermore, some institutions do not have any laboratory, which may impose a considerable lack of confidence or clinical competencies, posing a significant barrier for students during clinical training.
To describe the characteristics of the existing RC programs in SA, the respondents were asked about the barriers and solutions to their current role as RC program directors. Staff shortages and lack of postgraduate programs followed by lack of research activities were the most frequently identified barriers. Other supervisors of foreign RC programs have reported these barriers.16 The shortage of faculty staff was selected by most participants as a distinguishing barrier in advancing the profession. This may be explained by the already established low numbers of RCPs in SA.8 This issue may be addressed as faculty members currently abroad are expected to graduate and join the workforce, which will help increase the student enrollment capacity and the establishment of postgraduate programs. As critical solutions, participants were more likely to recognize the establishment of more RC jobs in most government hospitals, followed by an expansion of the existing RC scope of practice as critical solutions. Nevertheless, these solutions require an increase in the RCPs workforce as ageing and comorbidities increase, and the prevalence of lung diseases such as chronic obstructive pulmonary disease is of concern.17
There are no RC postgraduate degrees in SA, and this finding has important implications for developing the RC profession nationally by establishing postgraduate RC programs with different subspecialties. This would increase the advancement of the RC practice to reach regional and global excellence in research and, eventually, patient care. This, of course, will be achieved only by providing high-quality education and conducting high-quality research at universities across SA. Additionally, educational stakeholders, including universities, research institutions, medical and pharmaceutical companies should promote and fund students’ research and innovation activities to have more research engagement. Furthermore, forming an association for educators in SA is recommended to facilitate collaboration and close the gap between academic staff, clinical educators and clinicians. This is important as evidence suggests that increased clinical research activities were associated with better patient experience and lower mortality outcomes.18,19
Further work is required to establish RC programs in the regions where RCPs are hardly found, especially in the Northern and Southern regions. This should conform to the strategic objectives stated in Saudi Vision 2030 to have a thriving economy and vibrant society by improving the equity of access to education, especially in rural areas, and improving healthcare services. Finally, the RC profession is a fundamental part of clinical practice in SA. It should be empowered by promoting and implementing RC subspecialties into clinical practice to improve patient care and service provision.
This research is the first step toward a more profound understanding of the status of RCPs education in SA. Despite the collaboration of several institutions in completing the survey, noteworthy limitations were encountered: information from non-respondents is unknown, there is no information on current students studying RC abroad, the lack of input from leaders of the healthcare industry, and curricula differences were not evaluated. Furthermore, data on where previous graduates are currently working to assess geographical relocation was not evaluated.
Conclusion
RC education in SA has come a long way; however, many areas have opportunities for improvement. Regions of SA, such as the Northern and Southern regions, are underrepresented, and offering RC programs may help healthcare facilities in those regions provide RC services. Quality assurance was a significant area of concern as most institutions do not have national accreditation. Effective communication is required between institutions and other stakeholders, such as healthcare facilities, to ensure the demand and quality of graduates. Although the SCFHS offers a new professional RC postgraduate diploma program, well-established institutions have the opportunity to develop and offer postgraduate programs and subspecialties to help advance the RC profession in SA.
Abbreviations
RC, Respiratory Care; SA, Saudi Arabia; MV, Mechanical Ventilation; MoH, Ministry of Health; MoD, Ministry of Defense; RCP, Respiratory Care Practitioner; CBAHI, Central Board for Accreditation of Healthcare Institutions; SCFHS, Saudi Commission for Health Specialties; ICU, Intensive Care Unit; COVID-19, Coronavirus Disease 2019; MoE, Ministry of Education; BSc, Bachelor’s of Science degree; MSc, Master’s of Science degree; PhD, Doctor of Philosophy degree; NCAAA, National Center for Academic Accreditation and Evaluation; PFT, Pulmonary Function Testing.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The study was approved by the Taibah University, College of Medical Rehabilitation Sciences Research Ethics Committee (TUCMRS- REC) (CMR-RT-2020-06). All methods were carried out per relevant guidelines and regulations. All participants were provided with full information about the study before completing the questionnaire and were informed that no personal information would be used or disclosed and informed consent to participate was obtained. Participants were also informed of their right to decline to participate.
Acknowledgments
The abstract of this paper was presented at the 2021 AARC Congress (online) as an abstract poster with interim findings. The poster’s abstract was published in the Respiratory Care journal (http://rc.rcjournal.com/content/66/Suppl_10/3610526).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Mathews P, Drumheller L, Carlow JJ. Respiratory care manpower issues. Crit Care Med. 2006;34(3):S32–S45. doi:10.1097/01.CCM.0000203103.11863.BC
2. Kacmarek RM, Walsh BK. The respiratory therapy profession is at a crossroads. Respir Care. 2017;62(3):384–386. doi:10.4187/respcare.05484
3. DeBakey M, Beall JA, Feteih N, Mardini M, Guinn G, Mattox K. King Faisal Specialist Hospital and Research Centre cardiovascular surgery unit: first year. Cardiovasc Res Cent Bull. 1979;18(2):41–44.
4. Al-Otaibi HM, AlAhmari MD. The respiratory care profession in Saudi Arabia: past and present. Ann Thorac Med. 2016;11(4):237–242. doi:10.4103/1817-1737.191872
5. Central Board for Accreditation of Healthcare Institutions (CBAHI). National standards 2021; 2021. Available from: https://portal.cbahi.gov.sa/english/cbahi-standards.
6. Saudi Commission for Health Specialties. Professional accreditation and registration guide for health practitioners: SCFHS; 2014. Available from: https://www.scfhs.org.sa/en/registration/ClassAndRegister/Reregister/Documents/Professional%20Classification%20manual%20for%20Health%20Practitioners.pdf.
7. Iheanacho I, Zhang S, King D, Rizzo M, Ismaila AS. Economic burden of chronic obstructive pulmonary disease (COPD): a systematic literature review. Int J Chron Obstruct Pulmon Dis. 2020;15:439–460. doi:10.2147/COPD.S234942
8. Alotaibi G. Status of respiratory care profession in Saudi Arabia: a national survey. Ann Thorac Med. 2015;10(1):55–60. doi:10.4103/1817-1737.146878
9. West AJ, Nickerson J, Breau G, Mai P, Dolgowicz C. Staffing patterns of respiratory therapists in critical care units of Canadian teaching hospitals. Can J Respir Ther. 2016;52(3):75–80.
10. Baker RC, Lewis KO. Online master’s degree in education for healthcare professionals: early outcomes of a new program. Med Teach. 2007;29(9):987–989. doi:10.1080/01421590701551722
11. Barnes TA, Gale DD, Kacmarek RM, Kageler WV. Competencies needed by graduate respiratory therapists in 2015 and beyond. Respir Care. 2010;55(5):601–616.
12. Patrick L, Johnson J. The extent to which factors relevant to program function influence effectiveness of respiratory care education. Respir Care Educ Annu. 2001;10:15–32.
13. DC Shelledy, TH Dehm, Padilla J. An analysis of outcomes data for accredited respiratory therapist educational programs. Respir Care Educ Annu. 2001;10:55–66.
14. World Health Organization. Transforming and Scaling Up Health Professionals’ Education and Training. World Health Organization Guidelines; 2013.
15. Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi:10.1016/S0140-6736(10)61854-5
16. Barnes TA, Kacmarek RM, Durbin CG
17. Abla Mehio Sibai AS, Tabbara J, Rizk A. Ageing and health in the Arab region: challenges, opportunities and the way forward. Popul Horiz. 2017;14(2):73–84.
18. Jonker L, Fisher SJ, Dagnan D. Patients admitted to more research-active hospitals have more confidence in staff and are better informed about their condition and medication: results from a retrospective cross-sectional study. J Eval Clin Pract. 2020;26(1):203–208. doi:10.1111/jep.13118
19. Ozdemir BA, Karthikesalingam A, Sinha S, et al. Research activity and the association with mortality. PLoS One. 2015;10(2):e0118253. doi:10.1371/journal.pone.0118253
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

