Back to Journals » International Journal of General Medicine » Volume 16
The Safety and Efficacy of Rituximab-Based Regimen in Atypical Membranous Nephropathy: A Single Center Retrospective Cohort Study
Authors Liu Y, Zhang S, Hu R, Li C , Chen G, Shi X, Liu Y, Zheng K, Li H, Wen Y, Li X, Li X, Xia P, Qin Y
Received 9 March 2023
Accepted for publication 16 May 2023
Published 23 May 2023 Volume 2023:16 Pages 1983—1993
DOI https://doi.org/10.2147/IJGM.S410169
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yanan Liu, Shuo Zhang, Rongrong Hu, Chao Li, Gang Chen, Xiaoxiao Shi, Yan Liu, Ke Zheng, Hang Li, Yubing Wen, Xuemei Li, Xuewang Li, Peng Xia, Yan Qin
Department of Nephrology, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China
Correspondence: Peng Xia; Yan Qin, Department of Nephrology, Peking Union Medical College Hospital, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, 100730, People’s Republic of China, Tel +86 01069155058, Email [email protected]; [email protected]
Purpose: There are increasing reports of atypical membranous nephropathy (AMN) cases with similar pathological characteristics to secondary membranous nephropathy (SMN) without definite underlying causes. Although rituximab has become a first-line option in treating idiopathic membranous nephropathy (IMN), the efficacy and safety of rituximab-based regimen for AMN is not clear.
Patients and Methods: This is a retrospective, single-center study. AMN patients who received rituximab-based therapy were included. IMN patients treated with rituximab during the same period were selected as the control group matched by gender, sex, baseline urinary protein and albumin levels. Baseline data and follow-up data were collected.
Results: A total of 20 AMN patients and 40 IMN patients were included. The baseline levels of urinary protein were comparable between the two groups [6.77 (IQR 3.34, 11.49) g/24 h vs 6.47 (IQR 3.4, 10.76) g/24 h, P=0.944]. The baseline levels of serum albumin were 26.15± 6.71 g/L and 26.8± 5.54 g/L (P=0.689) respectively. The cumulative remission rate for rituximab-based treatment at the 12th month was lower in AMN group than IMN group [13 (65%) vs 36 (90%), P=0.045]. In AMN group, non-responders showed a higher level of proteinuria and a worse renal function at baseline than those of responders. There was no significant difference in the overall adverse events or serious adverse events between the two groups.
Conclusion: In our study, AMN patients obtained proteinuria remission in a lower percentage compared with IMN patients. In general, rituximab-based therapy is effective in AMN patients with an acceptable safety profile.
Keywords: rituximab, atypical membranous nephropathy, idiopathic membranous nephropathy, efficacy
Introduction
Membranous nephropathy (MN) is a leading cause of nephrotic syndrome (NS) in adults.1 Approximately one-third of MN cases are classified as secondary MN (SMN) because they could be attributed to systemic autoimmune diseases, infections, malignancies, or medications.2 According to immunofluorescence (IF), light microscopy (LM), and electron microscopy (EM), SMN has its own unique pathological characteristics, including positive C1q deposition, mesangial and endothelial cell proliferation, and deposits of subendothelial and subepithelial electron dense materials.3
In recent years, there have been increasing reports of atypical MN (AMN) cases.4–6 This group of patients usually showed similarity of pathological characteristics to SMN but no definite underlying causes of MN could be identified. According to a Chinese single-center study,5 the main clinical manifestation in patients with AMN is nephrotic syndrome and hematuria is more common compared with idiopathic MN (IMN). Based on recent data, serum PLA2R antibody could not be used to differentiate AMN from IMN.5
There is no uniform treatment regimen for AMN patients with nephrotic syndrome. The most widely used immunosuppressive therapies (IST) included corticosteroids combined with alkylating agents and calcineurin inhibitors (CNIs) based regimen. It seemed that the renal outcomes were similar between IMN and AMN patients.6 Nonetheless, adverse effects such as severe infections and metabolic abnormalities still remained a matter of concern.7,8
In the past decade, rituximab has emerged as a promising new first-line therapeutic option with positive results in the treatment of IMN.9–14 The efficacy and safety of a rituximab-based regimen for nephrotic syndrome brought on by AMN, however, have not been described. In this study, we reported 20 AMN patients treated with Rituximab-based regimen. Comparisons were made between AMN and IMN patients in treatment response and side effects.
Methods
Study Design and Participants
This is a single-center, retrospective study conducted in Peking Union Medical College Hospital (PUMCH). All IMN and AMN patients admitted to the Department of Nephrology from January 2017 to January 2022 were screened. The inclusion criteria for the AMN patients were as follows: 1) in addition to immune complex deposition under the epithelial and thickening GBM, renal biopsy showed at least one of the following characteristics: a) moderate or marked mesangial and/or endothelial proliferation; b) immune complex and electron dense deposits deposited in mesangial and/or subendothelial areas; c) “full house” in immunofluorescence, that is IgG, IgA, IgM, C3, C1q positive; 2) serum tests were negative for antinuclear antibodies, anti-neutrophil cytoplasmic antibody, hepatitis B surface antigen, e antigen, e antibody, core antibody, hepatitis C surface antibody and serum immunofixation electrophoresis; 3) no evidence of malignancy; 4) no history of suspicious medication intake prior to disease onset; 5) received rituximab-based therapy; 6) followed up for at least 6 months after rituximab treatment. IMN patients treated with rituximab during the same period were 1:2 matched by gender, sex, baseline urinary protein and albumin levels. The inclusion criteria for the IMN cohort were as follows: 1) renal biopsy showed immune complex deposition under the epithelial and thickening GBM without mesangial cells proliferation, mesangial matrix proliferation, or endothelial cell proliferation; 2) no immune complex or electron dense deposits deposited in mesangial and subendothelial; 3) no C1q positivity in IF; 4) serum tests were negative for antinuclear antibodies, anti-neutrophil cytoplasmic antibody, hepatitis B surface antigen, e antigen, e antibody, core antibody, hepatitis C surface antibody and serum immunofixation electrophoresis; 5) no evidence of malignancy; 6) no history of suspicious medication intake prior to disease onset; 7) received rituximab-based therapy; 8) followed up for at least 6 months after rituximab treatment. MN patients accompanied with possible IgA nephritis were excluded. This study protocol was performed in accordance with the Declaration of Helsinki. And the protocol was reviewed and approved by the Institution Review Board of Peking Union Medical Hospital (ZS-2816, I-23PJ636). Written informed consent were acquired from all participants.
Data Collection
The medical records of included patients were carefully reviewed to collect the data. Baseline data included age, gender, body mass index (BMI), comorbidity and complication, previous treatment and response, course of the disease, dosage of rituximab, concomitant immunosuppressive therapy, and comprehensive laboratory test results, such as 24 h urinary protein (24hUP), serum albumin (Alb), serum creatinine (sCr), uric acid (UA), serum complement, serum IgG and CD19+ B cell counts. The estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI formula.15 The results of anti-phospholipase A2 receptor (PLA2R) tests before rituximab treatment were also documented. The pathological characteristics were collected and the AMN diagnosis were checked by both clinicians and pathologists. Following the initial rituximab treatment, levels of 24hUP, Alb, sCr, anti-phospholipase A2 receptor (PLA2R) antibody, and CD19+ B cell counts were measured at 3rd, 6th, and 12th months.
Treatment Regimen
Patients received a single dose of 1g rituximab to achieve B-cell depletion. Repeated dosing of rituximab was recommended when B cell repopulation occurred during follow-up. The frequency and doses of rituximab administration were adjusted by the physicians in accordance with the underlying condition. The application of combined medications including corticosteroids, immunosuppressive drugs, ACE inhibitor and ARB were recorded.
Definitions
Nephrotic Syndrome (NS) was defined as urinary protein ≥3.5 g/24 h and serum albumin <30 g/L. Complete remission (CR) was defined as reduction of urinary protein from baseline to a value ≤0.3 g/24 h with normalization of serum albumin levels (≥35g/L). Partial remission (PR) was defined as reduction of urinary protein >50% from baseline and a value less than 3.5 g/24 h with the improvement of serum albumin concentration from baseline to≥30g/L. None remission (NR) was defined as a urinary protein reduction <50% from baseline values. B-cell depletion was defined as <5 CD19+ B cells/mm3 in the circulation. B cell repopulation was defined as ≥5 circulating B cells/mm3 after B cell depletion. The anti-PLA2R antibody was defined as positive when the titers were >14 RU/mL as measured with the standardized commercial ELISA (Euroimmun, Lubeck, Germany). Patients who achieved PR or CR were defined as responders. Accordingly, non-responders are those who did not achieve remission during follow-up. Relapse was defined as recurrence of proteinuria ≥3.5 g/day after partial or complete response.
Statistical Methods
Categoric variables were expressed as frequency and percentage and continuous variables were expressed by mean ± SD (for data that were normally distributed), or median and inter-quartile range (IQR) (for data that were not normally distributed). When the data were normally distributed, independent t-tests were used to compare the means of continuous variables. Otherwise, the Mann–Whitney test was used. The Chi-square test and Fisher exact tests were used to compare the variations of categorical variables. Cumulative incidences and time to remission were performed with Kaplan–Meier curves and Log rank test. Cox proportional hazards models were used to analyze the factors related to remission. All statistical analyses were performed using SPSS version 22.0 software. A P value of 0.05 is statistically significant.
Results
Baseline Characteristics
A total of 20 AMN patients were included in this study. In renal pathology, all of them showed at least one characteristic of mesangial and/or endothelial proliferation (18 patients), immune complex and electron dense deposits deposited in multisite (16 patients), and “full house” in immunofluorescence (14 patients). Forty IMN patients matched with age, gender, baseline urinary protein and serum albumin levels, were selected as control group. Baseline characteristics are summarized in Table 1. The male to female ratio group was 13:7 in both groups. The mean age of AMN patients and IMN patients was 36.05±12.87 years old and 40.63±12.08 years old, respectively (P=0.181). The levels of urinary protein were comparable between AMN and IMN patients at baseline [6.77 (IQR 3.34, 11.49) g/24 h vs 6.47 (IQR 3.40, 10.76) g/24 h, P=0.944]. And the levels of serum albumin were 26.15±6.71 g/L and 26.8±5.54 g/L (P=0.689) respectively. In AMN group, the median eGFR was 102.80 (IQR 72.73, 124.01) mL/min/1.73 m2. Correspondingly, the median eGFR was 100.26 (IQR 76.77, 115.66) mL/min/1.73 m2 in IMN group. 75% of the AMN patients and 80% of the IMN patients received prior immunosuppressive treatments (P=0.912). All patients received anti-PLA2R autoantibodies test before rituximab treatment. Twelve (60%) AMN patients and twenty-five (62.5%) IMN patients were anti-PLA2R autoantibodies positive (P=0.851) (Table 1).
 |
Table 1 Baseline Characteristics of Patients with AMN and IMN Treated with RTX-Based Regimen |
Treatment Responses
The median follow-up period after rituximab infusion was 13.5 (IQR 12.0, 30.5) months in AMN group and 23.5 (IQR 14.25, 34.5) months in IMN group (P=0.107). In AMN group, 16 (80%) patients received repeated rituximab treatment during follow-up with 2 doses in 9 cases, 3 doses in 4 cases and 4 doses in 3 cases. In IMN group, 33 (82.5%) patients received repeated rituximab treatment during follow-up with 2 doses in 20 cases, 3 doses in 7 cases, 4 doses in 3 cases and 5 doses in 3 cases. The cumulative doses of rituximab did not differ between the two groups (2.30±0.98g vs 2.38±1.10g, P=0.707). All patients achieved complete B-cell depletion in the two groups. During follow-up, 10 of 12 AMN patients and 25 of 25 IMN patients presented serum anti-PLA2R antibodies negative conversion after rituximab infusion. In AMN group, CR was achieved in 4 (20%) patients and PR was achieved in 9 (45%) patients. In IMN group, CR was achieved in 14 (35%) patients and PR was achieved in 22 (55%) patients. The cumulative remission rate at 12th month was lower in AMN group than IMN group [13 (65%) vs 36 (90%), P=0.045] (Figure 1 and Table 2). The clinical outcome expressed by Kaplan–Meier analysis is shown in Figure 2. No significant difference was observed between two groups in the median levels of urinary protein and serum albumin at 3rd, 6th, 9th, 12th months (shown in Figure 3 and Table 2).
 |
Table 2 Outcome of Patients with IMN and AMN Treated with RTX-Based Immunosuppressive Regimen |
 |
Figure 1 The percentage of patients in remission state (dark green bar), non-remission state (orange bar) and lost follow-up status (light green bar) in the AMN group and MN group during follow-up. |
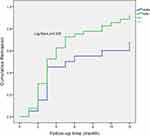 |
Figure 2 Kaplan–Meier curves for the percentages of participants achieving complete remission and partial remission. |
In AMN group, the baseline urinary protein level of responders was lower than non-responders [4.36 (IQR 2.34, 8.71) vs 12.58 (IQR 6.9, 17.4) g/24h, P= 0.008)]. Responders had a higher eGFR at baseline of 106.74 (IQR 96.07, 125.73) mL/min/1.73 m2 than non-responders [72.62 (IQR 65.83, 91.74) mL/min/1.73m2, P=0.036]. Moreover, the level of the serum IgG was higher in responders when compared with non-responders [5.83±1.87 vs 2.89±0.52 g/L, P=0.001]. (Table 3). Univariate COX proportional hazards models showed that urinary protein and serum IgG levels at baseline (grouped by quartile) were associated with response in AMN group (Table S1).
 |
Table 3 Baseline Characteristics of Responders and Non-Responders of Patients with AMN Treated with RTX-Based Regimen |
Kidney Function Stabilization
At 12th after rituximab treatment, the median eGFR of the two groups both maintained stable with 108.59 (IQR 73.50, 118.94) in AMN group and 104.24 (IQR 92.18, 117.96) mL/min/1.73 m2 and IMN group, respectively. But there were 2 patients in AMN group who showed kidney function deterioration with eGFR decreased >30%. One patient suffered acute kidney injury after a strike of pneumocystis Carinii pneumonia (PCP) at 6th month and received temporary continuous renal replacement therapy (CRRT). And the eGFR decreased from 91.74 mL/min/1.73 m2 at baseline to 24.22 mL/min/1.73 m2 at 12th month. Another patient had a gradually progressed renal function from 72.13 mL/min/1.73 m2 to 45.91 mL/min/1.73 m2.
Relapse
In AMN group, 1 patient relapsed after complete remission and the remission state was maintained for one and a half year. In IMN group, 2 patients relapsed during follow-up. One patient achieved partial remission at 2nd month and relapsed after 12 months. Another patient achieved partial remission at 6th month and sustained remission state for 2 years.
Association Between Anti-PLA2R Antibody and Treatment Response
In AMN group, 7/12 (58.3%) of the patients with positive anti-PLA2R antibodies achieved remission while 6/8 (75%) of the patients with negative anti-PLA2R antibodies achieved remission (P=0.439). In IMN group, 24/25 (96%) patients with positive anti-PLA2R antibodies achieved remission, while 12/15 (80%) in the negative group achieved remission (P=0.107). The levels of serum albumin and urinary protein did not differ significantly among subgroups divided by anti-PLA2R antibodies and regimens during follow-up (Table S2).
Adverse Events
As shown in Table 4, in AMN group, there were 7 adverse events observed including 1 PCP, 2 upper respiratory tract infections, 2 urinary tract infections, 1 intestinal infection and 1 skin infection. In IMN group, there were 11 adverse events including 1 PCP, 2 upper respiratory tract infections, 2 urinary tract infections, 2 intestinal infections, 2 skin infections, 1 suppurative tonsillitis and 1 esophagitis. The two cases of PCP infections both recovered after treatment. The incidences of adverse events showed no significant difference between AMN and IMN group (P=0.550).
 |
Table 4 Adverse Events of AMN Patients and IMN Patients Treated with RTX-Based Regimen |
Discussion
Our study was the first to report the efficiency and safety of rituximab-based regimen in AMN. In recent years, there has been an increasing number of AMN cases reported. However, clinical research on AMN is relatively scarce. In clinical practice, AMN is considered as a pathological variant of IMN and treated based on therapies of IMN. For patients with IMN, rituximab has become a promising first-line treatment option with a favorable efficacy and safety profile.16–20 MENTOR trial demonstrated the non-inferiority of rituximab to cyclosporine in inducing proteinuria remission.11 And the competition between cyclophosphamide and rituximab in patients with IMN remains open after the RICYCLO21 study and STARMAN study.10 However, the efficiency and safety of rituximab on AMN are not very clear. In our study, rituximab appears to be effective in reducing proteinuria in AMN patients with an apparent lower response rate when compared to IMN patients.
The comparisons between AMN and IMN in the treatment responses to conventional therapies have been made by previous research but the results are disputed. According to Jiang’s cohort study,6 there was no significant difference in the overall proteinuria remission rate at 6th month (59.1% vs 52.0%, P = 0.334) between the AMN and IMN patients who received glucocorticoid combined with cyclophosphamide or CNIs. In contrast, Sam et al22 found a significant difference in the average proteinuria of IMN and “lupus-like” MN patients after 3.5 years of follow-up [5.7 vs 3.1 g/d] with treatment of renin–angiotensin system inhibitor (RASi), prednisone, cyclosporine, and cyclophosphamide. These contradictory findings imply that more research is required to explore appropriate treatment options for AMN.
The reason for the less efficiency of rituximab in AMN group than IMN is unclear. Behind the differences in the pathological manifestation of renal biopsy, there may exist distinction in pathogenesis mechanism. From the perspective of mesangial proliferation, it is indicated that mesangial cells play a crucial role in the regulation of inflammation and immunity through their cross-talk with other intrinsic renal cells according to a single-cell profiling in MN.23 Thus, AMN patients might suffer more serious immunological and inflammatory disorders than IMN patients. Different complement deposition patterns also suggest different mechanisms. Complement activation evidently exists in patients with MN.24–26 As the initiation factor of classical complement pathway, C1q showed a low frequency in the immune deposits in IMN,27,28 which is consistent with the fact that IgG4, the IgG subclass that predominates in IMN, is unable to activate the classical pathway. It has been proposed that IMN may involve alternate or lectin pathway rather than the conventional pathway. In contrast, AMN tends to have a higher prevalence of C1q positive. Although the exact impact of complement activation on MN pathophysiology is not fully understood, different pathways may correspond to different pathogenic processes. Differences in immune mechanism behind their pathological manifestations may be the possible reason to explain the discrepancy in treatment response.
Our study demonstrated that the proteinuria remission of AMN patients was associated with baseline levels of urine protein. And the baseline renal function of non-responders was worse than that of responders. This finding was also consistent with previous studies. Giuseppe Remuzzi et al29 identified baseline proteinuria as an independent predictor of the decline of proteinuria and observed an increased GFR among those who achieved complete remission. What’s more, we found that the level of baseline serum IgG was significantly higher in responders.
Consistent with previous evidence,5 anti- PLA2R antibodies could not distinguish IMN from SMN cases in our research. And there was no significant difference between antibodies positive subgroup and antibodies negative subgroup in baseline clinical characteristics and treatment responses in our study. Franck Pourcine30 did not detect a difference between PLA2R-related and PLA2R-unrelated MN in clinical characteristics and remission rates. A Chinese cohort31 found that patients with detectable PLA2R-Ab had a worse prognosis than those with undetectable PLA2R-Ab at onset. A meta-analysis of 21 studies32 did not identify a significant relationship between anti-PLA2R antibody status and the efficacy of rituximab in MN. It was already been described that high initial PLA2R-Ab titer was correlated with larger amount of proteinuria and worse outcome.33–41 In the AMN group, the anti- PLA2R antibody level of non-responders appeared to be higher than those of responders, but the difference was not significant. The sample size might not be sufficient to detect a meaningful difference.
The safety profile of rituximab-based therapy in AMN patients and IMN patients was comparable. Previous studies have reported an acceptable safety profile of rituximab9,20,42,43 or rituximab-based therapy44 in IMN patients. The total adverse events as well as serious adverse events did not differ significantly between AMN group and IMN group, suggesting an acceptable safety profile of rituximab-based regimen in patients with AMN.
We acknowledge limitations due to the retrospective nature and the small samples sizes. Our observations will need to be validated in larger cohorts of patients or RCT. Further enrollments are underway.
Conclusion
In our study, AMN patients obtained remission of proteinuria in a lower percentage in comparison to IMN patients at one year. In general, rituximab-based therapy is effective in AMN patients with an acceptable safety profile.
Data Sharing Statement
All data generated or analyzed during this study are included in this article and its Supplementary Material Files. Further enquiries can be directed to the corresponding author.
Funding
This work was supported by the National High Level Hospital Clinical Research Fund-ings (2022-PUMCH-B-20 to Dr Yan Qin), the National Natural Sciences Foundation of China (Grant 81970621 to Dr Yan Qin), Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS 2021-I2M-C&T-B-011 to Dr Peng Xia), National High Level Hospital Clinical Research Funding (2022-PUMCH-A-169 to Dr Peng Xia).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Austin HA
2. Glassock RJ. Secondary membranous glomerulonephritis. Nephrol Dial Transplant. 1992;7(Suppl 1):64–71.
3. Moroni G, Ponticelli C. Secondary membranous nephropathy. A narrative review. Front Med. 2020;7:611317. doi:10.3389/fmed.2020.611317
4. Wang WX, Hu CY. Value of immunofluorescence-mediated detection of Ig, C1q, C3, and FRA for the identification and diagnosis of atypical membranous nephropathy. Eur Rev Med Pharmacol Sci. 2017;21(23):5415–5419. doi:10.26355/eurrev_201712_13929
5. Jiang Z, Cai M, Dong B, et al. Clinicopathological features of atypical membranous nephropathy with unknown etiology in adult Chinese patients. Medicine. 2018;97(32):e11608. doi:10.1097/MD.0000000000011608
6. Jiang Z, Cai M, Dong B, et al. Renal outcomes of idiopathic and atypical membranous nephropathy in adult Chinese patients: a single center retrospective cohort study. BMC Nephrol. 2021;22(1):148. doi:10.1186/s12882-021-02348-4
7. van den Brand JA, van Dijk PR, Hofstra JM, Wetzels JF. Long-term outcomes in idiopathic membranous nephropathy using a restrictive treatment strategy. J Am Soc Nephrol. 2014;25(1):150–158. doi:10.1681/ASN.2013020185
8. Jha V, Ganguli A, Saha TK, et al. A randomized, controlled trial of steroids and cyclophosphamide in adults with nephrotic syndrome caused by idiopathic membranous nephropathy. J Am Soc Nephrol. 2007;18(6):1899–1904. doi:10.1681/ASN.2007020166
9. Dahan K, Debiec H, Plaisier E, et al. Rituximab for severe membranous nephropathy: a 6-month trial with extended follow-up. J Am Soc Nephrol. 2017;28(1):348–358. doi:10.1681/ASN.2016040449
10. Fernandez-Juarez G, Rojas-Rivera J, Logt AV, et al. The STARMEN trial indicates that alternating treatment with corticosteroids and cyclophosphamide is superior to sequential treatment with tacrolimus and rituximab in primary membranous nephropathy. Kidney Int. 2021;99(4):986–998. doi:10.1016/j.kint.2020.10.014
11. Fervenza FC, Canetta PA, Barbour SJ, et al. A multicenter randomized controlled trial of rituximab versus cyclosporine in the treatment of idiopathic membranous nephropathy (MENTOR). Nephron. 2015;130(3):159–168. doi:10.1159/000430849
12. Lu W, Gong S, Li J, Luo H, Wang Y. Efficacy and safety of rituximab in the treatment of membranous nephropathy: a systematic review and meta-analysis. Medicine. 2020;99(16):e19804. doi:10.1097/MD.0000000000019804
13. Scolari F, Dallera N, Gesualdo L, et al. Rituximab versus steroids and cyclophosphamide for the treatment of primary membranous nephropathy: protocol of a pilot randomised controlled trial. BMJ Open. 2019;9(12):e029232. doi:10.1136/bmjopen-2019-029232
14. Rovin BH, Adler SG, Barratt J, et al. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(4):S1–S276.
15. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
16. Rojas-Rivera JE, Carriazo S, Ortiz A. Treatment of idiopathic membranous nephropathy in adults: KDIGO 2012, cyclophosphamide and cyclosporine A are out, rituximab is the new normal. Clin Kidney J. 2019;12(5):629–638. doi:10.1093/ckj/sfz127
17. Ponticelli C, Patrizia P, Del VL, Locatelli F. The evolution of the therapeutic approach to membranous nephropathy. Nephrol Dial Transplant. 2020;36(5):768–773.
18. Nikolopoulou A, Griffith M. MENTOR heralds a new era of therapy for membranous nephropathy. Nat Rev Nephrol. 2019;15(11):664–666. doi:10.1038/s41581-019-0200-1
19. Fiorentino M, Tondolo F, Bruno F, et al. Treatment with rituximab in idiopathic membranous nephropathy. Clin Kidney J. 2016;9(6):788–793. doi:10.1093/ckj/sfw091
20. van den Brand J, Ruggenenti P, Chianca A, et al. Safety of rituximab compared with steroids and cyclophosphamide for idiopathic membranous nephropathy. J Am Soc Nephrol. 2017;28(9):2729–2737. doi:10.1681/ASN.2016091022
21. Scolari F, Delbarba E, Santoro D, et al. Rituximab or Cyclophosphamide in the treatment of membranous nephropathy: the RI-CYCLO Randomized Trial. J Am Soc Nephrol. 2021;32:972–982. doi:10.1681/ASN.2020071091
22. Sam R, Joshi A, James S, et al. Lupus-like membranous nephropathy: is it lupus or not? Clin Exp Nephrol. 2015;19(3):395–402. doi:10.1007/s10157-014-1002-1
23. Xu J, Shen C, Lin W, et al. Single-cell profiling reveals transcriptional signatures and cell-cell crosstalk in Anti-PLA2R positive idiopathic membranous nephropathy patients. Front Immunol. 2021;12:683330. doi:10.3389/fimmu.2021.683330
24. Cravedi P. Complement in membranous nephropathy: what we thought we knew and what we really know. Kidney Int. 2021;100(3):499–501. doi:10.1016/j.kint.2021.03.010
25. Reinhard L, Stahl RAK, Hoxha E. Is primary membranous nephropathy a complement mediated disease? Mol Immunol. 2020;128:195–204. doi:10.1016/j.molimm.2020.10.017
26. Ma H, Sandor DG, Beck LH
27. Segawa Y, Hisano S, Matsushita M, et al. IgG subclasses and complement pathway in segmental and global membranous nephropathy. Pediatr Nephrol. 2010;25(6):1091–1099. doi:10.1007/s00467-009-1439-8
28. Jennette JC, Hipp CG. Immunohistopathologic evaluation of C1q in 800 renal biopsy specimens. Am J Clin Pathol. 1985;83(4):415–420. doi:10.1093/ajcp/83.4.415
29. Ruggenenti P, Chiurchiu C, Brusegan V, et al. Rituximab in idiopathic membranous nephropathy: a one-year prospective study. J Am Soc Nephrol. 2003;14(7):1851–1857. doi:10.1097/01.ASN.0000071511.35221.B3
30. Pourcine F, Dahan K, Mihout F, et al. Prognostic value of PLA2R autoimmunity detected by measurement of anti-PLA2R antibodies combined with detection of PLA2R antigen in membranous nephropathy: a single-centre study over 14 years. PLoS One. 2017;12(3):e0173201. doi:10.1371/journal.pone.0173201
31. Qin HZ, Zhang MC, Le WB, et al. Combined assessment of phospholipase A2 receptor autoantibodies and glomerular deposits in membranous nephropathy. J Am Soc Nephrol. 2016;27(10):3195–3203. doi:10.1681/ASN.2015080953
32. Huang L, Dong QR, Zhao YJ, Hu GC. Rituximab for the management of idiopathic membranous nephropathy: a meta-analysis. Int Urol Nephrol. 2021;53(1):111–119. doi:10.1007/s11255-020-02633-5
33. Hofstra JM, Debiec H, Short CD, et al. Antiphospholipase A2 receptor antibody titer and subclass in idiopathic membranous nephropathy. J Am Soc Nephrol. 2012;23(10):1735–1743. doi:10.1681/ASN.2012030242
34. Hoxha E, Thiele I, Zahner G, Panzer U, Harendza S, Stahl RA. Phospholipase A2 receptor autoantibodies and clinical outcome in patients with primary membranous nephropathy. J Am Soc Nephrol. 2014;25(6):1357–1366. doi:10.1681/ASN.2013040430
35. Hoxha E, Harendza S, Pinnschmidt H, Panzer U, Stahl RA. PLA2R antibody levels and clinical outcome in patients with membranous nephropathy and non-nephrotic range proteinuria under treatment with inhibitors of the renin-angiotensin system. PLoS One. 2014;9(10):e110681. doi:10.1371/journal.pone.0110681
36. Kanigicherla D, Gummadova J, McKenzie EA, et al. Anti-PLA2R antibodies measured by ELISA predict long-term outcome in a prevalent population of patients with idiopathic membranous nephropathy. Kidney Int. 2013;83(5):940–948.
37. Hoxha E, Harendza S, Pinnschmidt H, Panzer U, Stahl RA. M-type phospholipase A2 receptor autoantibodies and renal function in patients with primary membranous nephropathy. Clin J Am Soc Nephrol. 2014;9(11):1883–1890. doi:10.2215/CJN.03850414
38. Hofstra JM, Beck LH
39. Beck LH
40. Bech AP, Hofstra JM, Brenchley PE, Wetzels JF. Association of anti-PLA2R antibodies with outcomes after immunosuppressive therapy in idiopathic membranous nephropathy. Clin J Am Soc Nephrol. 2014;9(8):1386–1392.
41. Ruggenenti P, Debiec H, Ruggiero B, et al. Anti-phospholipase A2 Receptor antibody titer predicts post-rituximab outcome of membranous nephropathy. J Am Soc Nephrol. 2015;26(10):2545–2558. doi:10.1681/ASN.2014070640
42. Gao S, Cui Z, Wang X, et al. Rituximab therapy for primary membranous nephropathy in a Chinese cohort. Front Med. 2021;8:663680. doi:10.3389/fmed.2021.663680
43. Cravedi P, Sghirlanzoni MC, Marasa M, Salerno A, Remuzzi G, Ruggenenti P. Efficacy and safety of rituximab second-line therapy for membranous nephropathy: a prospective, matched-cohort study. Am J Nephrol. 2011;33(5):461–468. doi:10.1159/000327611
44. Zonozi R, Laliberte K, Huizenga NR, et al. Combination of rituximab, low-dose cyclophosphamide, and prednisone for primary membranous nephropathy: a case series with extended follow Up. Am J Kidney Dis. 2021;78(6):793–803. doi:10.1053/j.ajkd.2021.04.014
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

