Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
The Role of the Nurse in the Management of Medicines During Transitional Care: A Systematic Review
Authors Mardani A , Griffiths P , Vaismoradi M
Received 7 August 2020
Accepted for publication 4 September 2020
Published 30 October 2020 Volume 2020:13 Pages 1347—1361
DOI https://doi.org/10.2147/JMDH.S276061
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abbas Mardani,1 Pauline Griffiths,2 Mojtaba Vaismoradi3
1Nursing Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran; 2Department of Nursing, College of Human and Health Sciences, Swansea University, Swansea, Wales, UK; 3Faculty of Nursing and Health Sciences, Nord University, Bodø, Norway
Correspondence: Mojtaba Vaismoradi
Faculty of Nursing and Health Sciences, Nord University, Bodø 8049, Norway
Tel + 47 75517813
Email [email protected]
Purpose: To synthesise knowledge and to explore the role of the nurse in medicines management during transitional care.
Methods: An integrative systematic review was conducted. Electronic databases such as PubMed [including Medline], Web of Knowledge, Scopus, and Cinahl from January 2010 to April 2020 were searched. Original qualitative and quantitative studies written in English that focused on the role of the nurse in medicines management during transitional care, which included movement between short-term, long-term, and community healthcare settings were included.
Results: The search process led to the retrieval of 10 studies, which were published in English from 2014 to 2020. They focused on the role of the nurse in patients’ medicines management during transitional care in various healthcare settings. Given variations in the aims and methods of selected studies, the review findings were presented narratively utilizing three categories developed by the authors. In the first category as ‘medication reconciliation process’ the nurse participated in obtaining medication history, performing medication review, identifying medication discrepancies, joint medication reconciliation and adjustment. The second category as ‘collaboration with other healthcare providers’ highlighted the nurses’ role in clarifying medicines’ concerns, interdisciplinary communication and consultation, discharge planning and monitoring. In the third category as ‘provision of support to healthcare recipients’, the nurse was responsible for interpersonal communication with patients, education about medicines, and simplification of medication regimens, and symptoms management during transitional care.
Conclusion: Nurses play a crucial role in the safety of medicines management during transitional care. Therefore, they should be empowered and more involved in medicines management initiatives in the healthcare system. Patient safety and avoidance of medication errors during transitional care require that medicines management becomes a multidisciplinary collaboration with effective communication between healthcare providers.
Keywords: continuity of care, multidisciplinary collaboration, medicines management, nurse, patient safety, systematic review, transitional care
Introduction
Transitional care has become an important aspect of patient care in the healthcare system due to shorter lengths of hospital stay and the increased requirements of post-discharge care.1 Given the association between patient handovers during transitional care and incidences of adverse events, transitional care has been identified as a high-risk stage of the patient care journey.2–4 Transitional care has been defined as a set of developed measures to ensure the continuity and coordination of health care when the patient is transferred between various levels of health care in the same or to other healthcare settings.5,6 The transfer of necessary information and the liability of patient care from one healthcare setting to another is the fundamental and essential element of quality and safety in healthcare facilities.7 Factors that can disrupt effective transitional care across healthcare settings include inadequate patient or caregiver training, inappropriate communication between healthcare providers, insufficient evaluation of access to medication, and low health literacy levels.8 Therefore, transitional care has become a concentrated area of research and practice in medical sciences.9
Transitional Care: Medicines Management and Patient Safety
Achieving optimal transitional care between healthcare settings is essential to ensure patient safety and prevent hospital readmissions.10 It has been suggested that effective transitional care can reduce by 50% the relative risk of readmission within 30 days of discharge and save $2 for every $1 spent in the healthcare system.11 In general, transitional care programmes work as the bridge between pre-discharge and post-discharge caring interventions at multiple points in time. Patient engagement, as well as collaboration and communication between healthcare staff,12 is encouraged from admission to the primary care setting to the return to the patient's own home.13
Medicines management is an essential component of the provision of high-quality care and patient safety in transitional care.14 One of the primary solutions for patient safety from the perspective of the World Health Organization (WHO) is to ensure medication safety in transitional care.15 Also, medication-related issues have been considered to be substantial components of high-quality care in transitional care,16 in particular, that the medication regimen be transferred as safely as possible.17 Transitional care programmes can help with reducing medication-related problems, improving access to medication therapy, providing comprehensive medication counselling, and bridging gaps in medication care following hospital discharge.10 However, patients in transitional care between healthcare settings are prone to medication errors due to the lack of appropriate communication between healthcare providers, insufficient education and training, inappropriate follow-up, inadequate medication reconciliation, and lack of engagement of patients and their family caregivers in medicines management.18 Preventable adverse drug events in transitional care account for 46%–56% of all medication errors.19 A systematic review reported that 11%-59% of the medication history errors at admission and discharge had the potential to harm the patient.20 Redmond et al21 in a Cochrane review on 20 studies reported that 559 out of 1000 patients were at the risk of one or more medication discrepancies during standard transitional care programmes. Points of care transition in the healthcare system where patients are at the danger of medication-related harm include hospital to home transition;22 admission to the hospital;23 hospital admission, transfer and discharge;24 discharge from the hospital and post-discharge;25 and admission to the emergency department.26
Effective medicines management is a complex undertaking in both short-term and long-term healthcare settings including hospitals and nursing homes and requires collaboration by healthcare providers such as nurses, physicians and pharmacists to maximize positive healthcare consequences and to minimize practice errors.14 Medicines management is one of the most complex interdependent clinical challenges in health care and each healthcare provider involved in transitional care has independent, joint and overlapping responsibilities.27,28 Nurses are considered to be key members of the transitional care team.29,30 Their crucial role encompasses evaluating the transitional care plan, recognizing potential problems and then resolving them in order to improve patient safety.31 Involvement of nurses in medicines management of transitional care helps with the provision of access to care for patients with fragmented care or those at high risk of readmission. Their role has been suggested to be an alternative to the use of emergency services because it improves the workflow for referring physicians and supports care navigation back to community healthcare providers through patient education and medication self-management.32
Despite the importance of nurse participation in the safety of medication practice and the success of transitional care, there is no integrated knowledge of the nurse role in medicines management of transitional care in the international literature. Therefore, this systematic review of the international literature aimed to find an answer to the following question: What is the role of the nurse in medicines management during transitional care?
Aim
This review aimed to synthesise knowledge and explore the role of the nurse in medicines management during transitional care.
Methods
Protocol and Registration
This integrated systematic review of international literature involved both qualitative and quantitative studies.33–35 It allowed the authors to combine individuals' understandings obtained from statistical findings of quantitative research and narrative findings of qualitative studies in order to develop a comprehensive understanding of the study phenomenon.36 This systematic review was informed of the Preferred Reporting Items Systematic Reviews and Meta-analysis (PRISMA) Statement35 and has been registered on the PROSPERO under the code of CRD42020163046: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=163046.
Search Process and Eligibility Criteria
To identify appropriate keywords, the research team undertook discussions amongst themselves and also drew upon their experiences in the field of transitional care and medicines management. They also conducted a pilot search in general and specialized databases to find relevant keywords. To identify papers on the role of the nurse in medicines management during transitional care, the Boolean search method was applied using the following keywords: (nurs* AND (participation OR involvement OR engagement OR role) AND (“transitional care” OR “transition of care” OR “care transition” OR “healthcare transition” OR “continuity of patient care”) AND (“medicines management” OR medication OR medicines OR drug OR “pharmaceutical preparations” OR pharmaceuticals)). Guidance and support were received from an expert librarian during the search process. Accordingly, the online databases of PubMed [including Medline], Web of Knowledge, Scopus and Cinahl were searched to extract studies published in online peer-reviewed scientific journals from January 2010 to April 2020. Grey literature search encompassed policy documents, clinical guidelines and cross-references from bibliographies for improving the search coverage. Inclusion criteria for selecting relevant studies were: qualitative and quantitative studies, focus on the role of the nurse, medicines management of transitional care in short-term and long-term healthcare settings as well as community healthcare settings, and publication in peer-reviewed scientific journals. Articles without exact relevance to the nurse’s role or concentration on the role of other healthcare professionals involved in medicines management were excluded.
Study Selection
Each step of the systematic review process was performed independently by the authors (AM, PG and MV). They undertook online conversations to share the search results and decide on the next steps of the study. The studies' titles, abstracts and full-texts were obtained during the search process and were screened by the authors. The authors held discussions to resolve controversies and reach a consensus over the inclusion of selected studies.
Quality Appraisal
For the overall quality appraisal of selected studies in terms of the appropriateness of the research process and structure, the Enhancing the Quality and Transparency of Health Research (EQUATOR) was used.37 Tools for the appraisal of selected studies were as follows: the Standards for Reporting Qualitative Research (SRQR) for qualitative research; the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for observational, cross-sectional and cohort studies; the Good Reporting of A Mixed Methods Study (GRAMMS) for Mixed-methods designs; Consolidated Standards of Reporting Trials (CONSORT) for experimental and quasi-experimental studies. Also, the Hawker et al38 criteria regarding the research aim, scientific structure, quality of the research process and methodology, conclusion and references were specially considered for appraising the studies. In addition to the consideration of scores given by the appraisal tools for making a final decision on the inclusion or exclusion of studies, the authors discussed and made appropriate decisions on the significance and the methodological quality of each study for data analysis and synthesis.
Data Collection Process and Synthesis of Results
A data extraction table, containing the first author surname, publication year, the country where the study was conducted, design, sample size and setting, and data relating to the role of the nurse in medicines management of transitional care were developed and pilot-tested to ensure that it could collect required data on the characteristics of selected studies. The review findings were presented narratively due to variations within the selected studies in terms of aims and methods that hindered performing a meta-analysis. The results of the selected studies were then reviewed and appropriate categories were developed based on differences and similarities in their findings. The authors undertook frequent discussions to reach agreements on assigning the studies’ findings into the categories.
Results
Search Outcome and Selection of Studies
The results of our search in the databases have been presented in Table 1. The search process using the predetermined keywords led to retrieving 4037 articles. After deleting unrelated and duplicate titles, and performing abstract and full-text reading, ten studies were selected finally for data analysis and synthesis. The methodological quality of the selected studies was evaluated during the full-text appraisal phase. No study was excluded as it was judged that they had an acceptable level of quality in terms of presentation and research design, theoretical and conceptual framework, and their findings could inform our review. No more studies were discovered for inclusion during the grey literature search and from reviewing the reference lists of the selected studies.
 |
Table 1 Results of Different Phases of the Search Process |
The study flow diagram according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) has been presented in Figure 1.
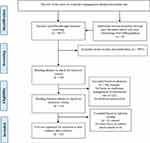 |
Figure 1 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Note: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. Available from: http://prisma-statement.org/PRISMAStatement/FlowDiagram.aspx. The PRISMA Statement distributed under the terms of the Creative Commons Attribution License.65 |
General Characteristics of the Selected Studies
An overview of the selected studies (n = 10) has been demonstrated in Table 2. They were all published in English from 2014 to 2020, seven studies were from the USA,39–45 one from Canada,46 one from Oman,47 and one from Australia.48
 |  |  |
Table 2 Characteristics of the Studies Selected for Data Analysis and Synthesis |
Regarding the studies' methodologies, two studies used a qualitative design,45,48 one was a secondary qualitative analysis,44 one was a survey,47 one used an experimental design,43 two used a prospective cohort,39,46 one was a retrospective cohort,41 one used a mixed-method study,42 and one was a retrospective review of medical records.40
Transitional Point of Care in the Selected Studies
The selected studies focused on medicines management during the transition of care in various settings as follows: from the emergency department to the medical ward,39 from the hospital to the long-term care facilities and home,42 from the hospital to home,40,41 between different wards in the hospital,46 from the skilled nursing facility to home,43 from the admission to discharge at the hospital,47 from the emergency department to discharge,48 to a home hospice,44 and to a nursing home.45
The Role of the Nurse in Medicines Management During Transition of Care
Since there were heterogeneities in the studies' methods, objectives and results, a meta-analysis could not be conducted and our review findings were presented narratively. Three categories concerning the role of the nurse in the safety of medicines management of transitional care were identified: “medication reconciliation process”, “collaboration with other healthcare providers”, and “provision of support to healthcare recipients”. These categories were identified after an analysis of the studies' findings (Figure 2).
 |
Figure 2 The nurse role in medicines management of transitional care. |
Medication Reconciliation Process
This category discusses the role of the nurse in the medicines' assessment process during transitional care at various healthcare levels. Nurses were noted to play a crucial role in medicines management through the reconciliation process, where an accurate list of a patient's current medicines was assessed and was compared with the current list in use. Accordingly, the nurses had three main responsibilities as “assessment of medication history”, “identification of medicines discrepancies”, and “joint role in medicines reconciliation” that were described as follows.
Assessment of Medication History
Nurses were involved in obtaining medication history from patients in the admission time to healthcare centres or at the transition between healthcare levels.39,46 Chhabra et al39 noted that clinical nurses were involved in the medication reconciliation process at admission. Accordingly, emergency nurses collected medication history, and admitting floor (ward) nurses collected additional medication history and sent the report about medication reconciliation to admitting physicians. The mean time spent by admitting floor nurses collecting medication history prior to (11 minutes) or after (16.6 minutes) placing the admission orders were not significantly different, but time spent per medication after placing admission orders (2 minutes) was higher than before it (0.94 minute). In the study by Chan et al46 the nurses' role in the medication reconciliation process was to obtain the best possible medication history and perform medication reconciliation for those patients who were admitted to the cardiology ward or the critical care unit or those who were transferred between wards.
Identification of Medicines Discrepancies
Reviewing medications overall,40,42 collecting information for identifying medication discrepancy,45 and medication support and deprescribing process44 were reported as roles of nurse. In the transitional care programme devised by Lovelace et al40 the case management nurse performed an initial assessment and extensive medication review during the first home visit or telephone follow-up after discharge from the hospital. The outpatient nurse practitioner then collaborated with the case management nurse during home visits. They reviewed medications according to the assessment provided by the case management nurse, made adjustments, and ordered medications renewals if the case management nurse faced difficulties in access to primary healthcare providers. Prusaczyk et al42 described transitional care measures being provided to older adults with and without dementia in the transition from the hospital to long-term care facilities and home, and noted that registered nurses and advanced practice registered nurses delivered medication safely to 99% and 37% of patients, respectively. Advanced practice registered nurses were described as being highly involved in medication review and medication reconciliation.
In the study by Tjia et al,44 nurses' perspectives on their role in family caregivers' medicines management and support in transition to home hospice were addressed. Nurses considered that medication review was a key component of medication support and the deprescribing process. The nurse was responsible for checking the medication list to find essential and nonessential medicines, describing them to the family caregiver and discussing with the physician to receive recommendations on discontinuing nonessential ones to prevent side effects, adverse drug reactions (ADRs), and polypharmacy. The nurse would also monitor the process of medication by the patient and the family caregiver before making any decision regarding changes to essential medicines.
Vogelsmeier45 reports that nurses in nursing homes had a primary role in performing medication reconciliations and they assessed medication history and identified medication order discrepancies during transition to nursing homes. Some nurses performed “active information seeking” through reviewing transfer documents and talked with residents and families in order to understand the medication history and reasons behind ordering medications. Others performed “passive information seeking” as they assumed that medication orders at transfer were correct and that time challenges and heavy workloads hindered deciphering clinical information to discover medication order discrepancies. Many nurses did engage in a cognitive process called “sense-making” where tried to identify medication discrepancies. In this respect, rules/regulations, specific medications and the experience of errors and adverse events were cues to consider potential discrepancies.
Joint Role in Medicines Reconciliation
In the study by Otsuka et al41 nurses were the members of interprofessional post-acute care clinics and were involved in medicines management for those patients who were transferred from the hospital to their own homes. The process of medication reconciliation was started through assessing patients' capabilities to fill out their new prescriptions via telephone calls to the patient or the caregiver within two business days post discharge.
Al-Hashar et al47 reported that nurses had a supportive role working with pharmacists and physicians in medication reconciliation from hospital admission to discharge. Nurses considered themselves to be second only to physicians in medication reconciliation since they: obtain an accurate medication history on admission, verify and reconcile discrepancies between the medication history list, those ordered on admission and at transition, and send the discharge medication list to the next healthcare provider. Nurses considered that they were second only to the pharmacist in the provision of instructions and counselling for patients about medications upon discharge. From the pharmacists' perspective, the nurses' role in the process of medication reconciliation was of less importance than that of pharmacists and physicians as nurses were not involved in sending the patients' discharge medication list to the next healthcare provider. Physicians described the nurse playing a supportive role in the medication reconciliation process with key roles being played by themselves and the pharmacist in the medication reconciliation in transitional care.
Collaboration with Other Healthcare Providers
This category describes the role of the nurse in the medicines management of transitional care at various healthcare levels in collaboration with other healthcare providers. In the study by Manias et al48 regarding communication about medicines management during the transition point between emergency departments and medical wards, the nurses' proactive stance in medical wards was evident as nurses clarified concerns over medicines with doctors. Nurses in the medical ward evaluated the clinical parameters of transferred patients from the emergency department and alerted doctors about gathered information leading to rational medicine changes. When the patient was transferred to the nursing home, those nurses then organized medicines' changes via a phone call to the general practitioner.48
Various synchronous and asynchronous forms of interdisciplinary communication among healthcare professionals including nurses, physicians, and pharmacists influenced medicines management between the transition points of care.48 While nurses considered verbal communication essential so as to be equipped quickly to provide suitable care, asynchronous communication, such as discharge summaries and referral letters, was also valued. The accuracy and readability of the documented content of communication were significant requirements to avoid medication discrepancies at transitional points of care. Nurses acknowledged that written communication was essential to face the challenge of working in a quickly changing environment.48
In the study by Lovelace et al40 some patients were transferred to nursing homes for short-term rehabilitation following their hospitalizations based on the devised transitional care programme. The pharmacist contacted the nursing home to obtain a list of discharge medications and sent the list and information to the case management nurse who then contacted the patients or their caregiver to schedule a home visit. Following the home visit, case management nurses would then report medication discrepancies to the members of the transition care programme team and the patients' primary care provider and care manager. The case management nurse would also collaborate with a pharmacist to provide a precise discharge medication chart with print size adjustments for those patients suffering from impaired vision.
Vogelsmeier’s45 study found that nursing home physicians relied on information and recommendations provided by the nurse to know what medications the resident was supposed to be taking because they provided care to residents only in the nursing home. The physicians were unfamiliar with residents' medical care prior to transfer, rarely communicated with other healthcare providers and were not present at the time of transfer. Therefore, nurses were the prime source of information on medicines management and would request that the physician perform required assessments and review laboratory values. The nurse would then consult with the physician prior to medicines being prescribed.
Reidt et al43 focussed on a model for interprofessional collaboration that improved discharge from a skilled nursing facility to home. Nurses played the main role in discharge planning from the skilled nursing facility. The pharmacist a few days before discharge would review the electronic health record to evaluate dietary supplement prescriptions and over-the-counter medications in terms of indication, effectiveness and safety and would ensure that changes of medications made during the hospital and skilled nursing facility stays were still appropriate. The pharmacist resolved unexplained changes by consulting with the nurse practitioner and shared recommendations such as starting or ceasing medicines, adjusting doses, or ensuring that necessary laboratory work was ordered for the discharge medication regimen. In addition, the pharmacist and nurse determined collaboratively the discharge medication regimen. The nurse also monitored particular medicines' side effects and reminded patients about follow-up appointments.
Provision of Support to Healthcare Recipients
This category discusses the nurses' provision of support to healthcare recipients in the medicines management of transitional care at various healthcare levels. Tjia et al44 explored nurses' perspectives on their role in family caregivers' medicines management and support in the transition to home hospice. Nurses provided education and skill building for family caregivers, and emphasized increasing knowledge and education regarding symptoms. To enable skill-building, they focused on symptom management and less on medicines organization and administration. The medication regimen was simplified for patients' and family caregivers by eliminating as many medications as possible.44 Nurses also improved trust and communication through paying attention to patients and their family caregivers and understanding the concerns of the family caregiving when deprescribing medications.44
Prusaczyk et al42 evaluated transitional care interventions provided by various healthcare providers to older adults with and without dementia in transition from the hospital to long-term care facilities and home. Nurses were the primary providers of patient education regarding medication education and how to manage and monitor symptoms after discharge. Advanced practitioner registered nurses also helped with education about the management and monitoring of symptoms. In the Al-Hashar et al47 study, nurses described their key role in the provision of instructions and counselling to patients about medications upon discharge. Manias et al48 described interpersonal communication between health professionals, including nurses, and patients being the key ingredient of maintaining medication safety. Provision of medicines' instructions for patients when moved between their homes and the hospital meant patients could take a more active stance in managing their medicines.
Discussion
This systematic review integrated the findings of qualitative and quantitative studies and synthesised knowledge regarding the role of the nurse in the safety of medicines management of transitional care. Findings from this review indicate that the nurse's role in medicines management of transitional encompasses: medication reconciliation, collaboration with other healthcare providers, and provision of support to healthcare recipients. According to the international literature, all healthcare professionals should collaborate together to ensure patient safety. Moreover, nurses should take more responsibility and become more involved in patient safety initiatives and act proactively in order to protect and maintain the safety of medicines' management through disclosing and reporting errors.49 In addition, nurses are able to be involved in the reduction of medicines' side effects and ADRs through monitoring medicines and providing informational support to doctors, pharmacists, patients and their families as well as applying fundamental nursing interventions to relieve potentially negative consequences on patient wellbeing.50,51
This review discovered that nurses actively played various roles in the medication reconciliation process such as collecting medication history, reviewing medications, collecting information to identify medication discrepancies, coordinating medication support, and supporting the deprescribing process. They started the medication reconciliation process by assessing patients' capabilities to comply with their new prescriptions and engaging in their joint role with pharmacists and physicians in medicines management from admission to the hospital until discharge. The nurse was the key health professional in performing medication reconciliation in nursing homes. Nurses raised concerns over medicines prescribed by doctors, provided medication consultation to the pharmacist, assisted in collaboratively determined discharge medication regimes, and had interdisciplinary communication with physicians and pharmacists to ensure medication safety. They provided medication education, consultation and symptoms management associated with medications, helped with simplifying the medication regimen, and established interpersonal communication to ensure medication safety and support to healthcare recipients. The nurses' integral role in the medication reconciliation process in various transitional points of care has been supported by current international literature.1,52,53 Medication reconciliation is defined as an official process in which healthcare providers work with patients to ensure the exact and complete transfer of medication information at the interfaces of care.54 Several international patient safety organizations including the Institute for Health Improvement (IHI), the Joint Commission (TJC), and the World Health Organization (WHO) have acknowledged that medication reconciliation is pivotal to achieve medication safety through identifying medication discrepancies, particularly at transition care points.55 Achieving optimal medication reconciliation requires the recognition of responsibilities and roles, interdisciplinary teamwork, proper communication, and better tracking and reporting of information to successfully incorporate the stages of medication reconciliation and ensure patient safety.54,56 On the other hand, healthcare professionals' insufficient knowledge of medicines management is one of the important barriers to achieving optimal medication reconciliation.57 Sufficient education and training are not provided to nursing students to practice medication reconciliation. Therefore, there is an evident need for training on the full medication reconciliation process and policy in clinical settings and the medication reconciliation process should be covered in the degree education curriculum of nurses.58
As highlighted in the findings of this review, two of the main roles of the nurse in medicines management during transitional care are communication and collaboration with other healthcare providers. As a part of an interdisciplinary team, nurses along with physicians and pharmacists can play a crucial role in medicines management during transitions from one setting to another. The findings of Albert's59 systematic review on transition-of-care models in patients with heart failure suggested that multi-professional teamwork, communication, and collaboration had key roles in ensuring patient safety. Another recent systematic review by Bethishou et al60 investigating the effectiveness of pharmacy-led continuity of care programmes indicated that the collaboration of the pharmacist with nurses in undertaking phone calls to patients after discharge improved the quality and safety of care. Ensing et al's52 suggested that in the transition point of care and post-discharge, pharmacists were most likely to collaborate closely with nurses to improve patient care outcomes. Lack of communication and collaboration between healthcare providers, including nurses, is an important barrier to medicines management at the transitional point of care.57 Therefore, nurses should develop communication skills and effectively be invited to collaborate with the interprofessional team in order to improve the continuity and coordination of care.61,62
Our review findings indicate that the nurses' role in the provision of education and support about medications and symptoms management to patients and their family caregivers requires optimal communication to ensure medication safety. Provision of patient support and education at the transition points of care can reduce the risk of adverse medication-related events.16 Ozavci et al63 showed that medication discrepancies at transitional care of older patients were associated with nurses' communication with patients. A systematic review by Tobiano et al64 on how patients engaged in medication communication during admission and discharge demonstrated that nurses performed counselling and education about medication, instructed patients about the medication discharge plan, and conducted telephone calls for post-hospital discharge follow-ups about medications.
Limitations
The heterogeneity of the selected studies' methods and variations in their focus including being conducted in short-term and long-term healthcare settings might have impacted the synthesis and integration of the review findings. Also, studies were limited to English language. However, performing our search using multidimensional keywords and in international databases provided a comprehensive overview of the current international knowledge about the role of the nurse in medicines management safety during transitional care. Also, bias in the process of data collection and synthesis was reduced as much as possible through close cooperation and discussion between the authors. The role of nurses in medicines management during transitional care is closely related to the type of healthcare settings and type of transitional point of care. Given the limited number of studies that met the inclusion criteria for this review prevented the full exploration of the role of the nurse in medicines management at different transitional points of care including transition within the hospital, from hospital to home and other healthcare facilities, which needs consideration in future studies.
Conclusion
This systematic review focused on the role of the nurse in medicines management during transitional care and identified how it impacted on patient safety. Both qualitative and quantitative research findings through an integrative review design were included in order to provide a comprehensive image of the study phenomenon.
Considering the critical role of nurses in medicines management during the transitional care process requires adequate attention to degree level education and in-service training for nurses. Successful medicines management and reducing medication errors require the recognition of responsibilities and roles, a multidisciplinary collaboration and communication between various healthcare professions including nurses, doctors and pharmacists. Healthcare professionals through interdisciplinary collaboration and communication share objectives, display shared responsibility and power, make decisions collectively, and work together to improve medication safety during transitional care. Also, health professionals should be aware of the role of the nurse in medicines management to ensure medication safety during transitional care. Future studies using qualitative and quantitative research methods should explore how nurses can be more actively involved in medicines management of transitional care affecting on patient care outcomes including adherence to medication regimens, visits to the emergency department, and reduction of the readmission rate to long-term healthcare settings.
Data Sharing Statement
All data pertinent to this study are contained in the article.
Acknowledgments
Nord University, Bodø, Norway has supported the publication of this manuscript through coverage of publication charges.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. It should be mentioned that this article has been written in British English.
Funding
This research received no external funding.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Donald F, Kilpatrick K, Reid K, et al. Hospital to community transitional care by nurse practitioners: a systematic review of cost-effectiveness. Int J Nurs Stud. 2015;52(1):436–451. doi:10.1016/j.ijnurstu.2014.07.011
2. Kapoor A, Field T, Handler S, et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019;179(9):1254–1261. doi:10.1001/jamainternmed.2019.2005
3. Tsilimingras D, Bates DW. Addressing postdischarge adverse events: a neglected area. Jt Comm J Qual Patient Saf. 2008;34(2):85–97.
4. Tsilimingras D, Schnipper J, Duke A, et al. Post-discharge adverse events among urban and rural patients of an urban community hospital: a prospective cohort study. J Gen Intern Med. 2015;30(8):1164–1171. doi:10.1007/s11606-015-3260-3
5. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. Health Aff (Millwood). 2011;30(4):746–754. doi:10.1377/hlthaff.2011.0041
6. World Health Organization (WHO). Transitions of Care: Technical Series on Safer Primary Care. Geneva: WHO; 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/252272/9789241511599-eng.pdf;jsessionid=08FCC79EDB6223987AEFA4611AD59B0E?sequence=1.
7. Aase K, Laugaland KA, Dyrstad DN, Storm M. Quality and safety in transitional care of the elderly: the study protocol of a case study research design (phase 1). BMJ Open. 2013;3:8. doi:10.1136/bmjopen-2013-003506
8. Dempsey J, Gillis C, Sibicky S, et al. Evaluation of a transitional care pharmacist intervention in a high-risk cardiovascular patient population. Am J Health Syst Pharm. 2018;75(17Supplement 3):S63–s71. doi:10.2146/ajhp170099
9. Storm M, Schulz J, Aase K. Patient safety in transitional care of the elderly: effects of a quasi-experimental interorganisational educational intervention. BMJ Open. 2018;8(1):e017852. doi:10.1136/bmjopen-2017-017852
10. Cole J, Wilkins N, Moss M, Fu D, Carson P, Xiong L. Impact of pharmacist involvement on Telehealth Transitional Care Management (TCM) for high medication risk patients. Pharmacy (Basel). 2019;7:4.
11. Polinski JM, Moore JM, Kyrychenko P, et al. An insurer’s care transition program emphasizes medication reconciliation, reduces readmissions and costs. Health Aff (Millwood). 2016;35(7):1222–1229. doi:10.1377/hlthaff.2015.0648
12. Rennke S, Ranji SR. Transitional care strategies from hospital to home: a review for the neurohospitalist. Neurohospitalist. 2015;5(1):35–42. doi:10.1177/1941874414540683
13. Lee KH, Low LL, Allen J, et al. Transitional care for the highest risk patients: findings of a randomised control study. Int J Integr Care. 2015;15:e039. doi:10.5334/ijic.2003
14. Vogelsmeier A, Pepper GA, Oderda L, Weir C. Medication reconciliation: a qualitative analysis of clinicians’ perceptions. Res Social Adm Pharm. 2013;9(4):419–430. doi:10.1016/j.sapharm.2012.08.002
15. World Health Organization (WHO). Patient safety solutions preamble. WHO Collaborating Centre for Patient Safety Solutions. 2007. Available from: https://www.who.int/patientsafety/solutions/patientsafety/Preamble.pdf?ua=1.
16. Spinewine A, Claeys C, Foulon V, Chevalier P. Approaches for improving continuity of care in medication management: a systematic review. Int J Qual Health Care. 2013;25(4):403–417. doi:10.1093/intqhc/mzt032
17. Setter SM, Corbett CF, Neumiller JJ. Transitional care: exploring the home healthcare nurse’s role in medication management. Home Healthc Nurse. 2012;30(1):19–26. doi:10.1097/NHH.0b013e31823aa8c8
18. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi:10.1056/NEJMsa0803563
19. Chhabra PT, Rattinger GB, Dutcher SK, Hare ME, Parsons KL, Zuckerman IH. Medication reconciliation during the transition to and from long-term care settings: a systematic review. Res Soc Admin Pharm. 2012;8(1):60–75. doi:10.1016/j.sapharm.2010.12.002
20. Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. Cmaj. 2005;173(5):510–515. doi:10.1503/cmaj.045311
21. Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, Fahey T. Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev. 2018;8(8):Cd010791.
22. Corbett CF, Setter SM, Daratha KB, Neumiller JJ, Wood LD. Nurse identified hospital to home medication discrepancies: implications for improving transitional care. Geriatr Nurs. 2010;31(3):188–196. doi:10.1016/j.gerinurse.2010.03.006
23. Hellström LM, Bondesson Å, Höglund P, Eriksson T. Errors in medication history at hospital admission: prevalence and predicting factors. BMC Clin Pharmacol. 2012;12:9. doi:10.1186/1472-6904-12-9
24. Huynh C, Wong IC, Tomlin S, et al. Medication discrepancies at transitions in pediatrics: a review of the literature. Paediatr Drugs. 2013;15(3):203–215. doi:10.1007/s40272-013-0030-8
25. Riordan CO, Delaney T, Grimes T. Exploring discharge prescribing errors and their propagation post-discharge: an observational study. Int J Clin Pharm. 2016;38(5):1172–1181. doi:10.1007/s11096-016-0349-7
26. Zarif-Yeganeh M, Rastegarpanah M, Garmaroudi G, Hadjibabaie M, Sheikh Motahar Vahedi H. Incidence of medication discrepancies and its predicting factors in emergency department. Iran J Public Health. 2017;46(8):1086–1094.
27. Choo J, Hutchinson A, Bucknall T. Nurses’ role in medication safety. J Nurs Manag. 2010;18(7):853–861. doi:10.1111/j.1365-2834.2010.01164.x
28. Gunadi S, Upfield S, Pham N-D, Yea J, Schmiedeberg MB, Stahmer GD. Development of a collaborative transitions-of-care program for heart failure patients. Am J Health Syst Pharm. 2015;72(13):1147–1152. doi:10.2146/ajhp140563
29. Camicia M, Lutz BJ. Nursing’s role in successful transitions across settings. Stroke. 2016;47(11):e246–e249. doi:10.1161/STROKEAHA.116.012095
30. Fox MT, Butler JI, Sidani S, et al. Collaborating with healthcare providers to understand their perspectives on a hospital-to-home warning signs intervention for rural transitional care: protocol of a multimethod descriptive study. BMJ Open. 2020;10(4):e034698. doi:10.1136/bmjopen-2019-034698
31. Vaughn S, Mauk KL, Jacelon CS, et al. The competency model for professional rehabilitation nursing. Rehabil Nurs. 2016;41(1):33–44. doi:10.1002/rnj.225
32. Smith M. Transitional care clinics: an innovative approach to reducing readmissions, optimizing outcomes and improving the patient’s experience of discharge care-conducting a feasibility study. J Nurs Educ Pract. 2016;6(6):34. doi:10.5430/jnep.v6n6p34
33. Aromataris E, Pearson A. The systematic review: an overview. Am J Nurs. 2014;114(3):53–58. doi:10.1097/01.NAJ.0000444496.24228.2c
34. Deeks JJ, Higgins J, Altman DG, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0 (updated March 2011). The Cochrane Collaboration. 2011;2.
35. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100–e1000100.
36. Thomas J, Harden A, Oakley A, et al. Integrating qualitative research with trials in systematic reviews. BMJ. 2004;328(7446):1010–1012. doi:10.1136/bmj.328.7446.1010
37. EQUATOR Network. Enhancing the quality and transparency of health research. 2019. Available from: http://www.equator-network.org/.
38. Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. 2002;12(9):1284–1299. doi:10.1177/1049732302238251
39. Chhabra A, Quinn A, Ries A. Evaluation of time spent by pharmacists and nurses based on the location of pharmacist involvement in medication history collection. J Pharm Pract. 2019;32(4):394–398. doi:10.1177/0897190017753783
40. Lovelace D, Hancock D, Hughes SS, et al. Care Case management program: taking case management to the streets and beyond. Prof Case Manag. 2016;21(6):277–290. doi:10.1097/NCM.0000000000000158
41. Otsuka S, Smith JN, Pontiggia L, Patel RV, Day SC, Grande DT. Impact of an interprofessional transition of care service on 30-day hospital reutilizations. J Interprof Care. 2019;33(1):32–37. doi:10.1080/13561820.2018.1513466
42. Prusaczyk B, Fabbre V, Morrow-Howell N, Proctor E. Understanding transitional care provided to older adults with and without dementia: a mixed methods study. Int J Care Coord. 2020;23(1):14–23. doi:10.1177/2053434520908122
43. Reidt SL, Holtan HS, Larson TA, et al. Interprofessional collaboration to improve discharge from skilled nursing facility to home: preliminary data on postdischarge hospitalizations and emergency department visits. J Am Geriatr Soc. 2016;64(9):1895–1899. doi:10.1111/jgs.14258
44. Tjia J, DeSanto-Madeya S, Mazor KM, et al. Nurses’ perspectives on family caregiver medication management support and deprescribing. J Hosp Palliat Nurs. 2019;21(4):312–318. doi:10.1097/NJH.0000000000000574
45. Vogelsmeier A. Identifying medication order discrepancies during medication reconciliation: perceptions of nursing home leaders and staff. J Nurs Manag. 2014;22(3):362–372. doi:10.1111/jonm.12165
46. Chan C, Woo R, Seto W, Pong S, Gilhooly T, Russell J. Medication reconciliation in pediatric cardiology performed by a pharmacy technician: a prospective cohort comparison study. Can J Hosp Pharm. 2015;68(1):8–15.
47. Al-Hashar A, Al-Zakwani I, Eriksson T, Al Za’abi M. Whose responsibility is medication reconciliation: physicians, pharmacists or nurses? A survey in an academic tertiary care hospital. Saudi Pharm J. 2017;25(1):52–58. doi:10.1016/j.jsps.2015.06.012
48. Manias E, Gerdtz M, Williams A, Dooley M. Complexities of medicines safety: communicating about managing medicines at transition points of care across emergency departments and medical wards. J Clin Nurs. 2015;24(1–2):69–80. doi:10.1111/jocn.12685
49. Vaismoradi M, Vizcaya-Moreno F, Jordan S, Gåre Kymre I, Kangasniemi M. Disclosing and reporting practice errors by nurses in residential long-term care settings: a systematic review. Sustainability. 2020;12:7. doi:10.3390/su12072630
50. Amaniyan S, Ghobadi A, Vaismoradi M. Cold application on bruising at the subcutaneous heparin injection site: a systematic review and meta-analysis. SAGE Open Nursing. 2020;6:2377960820901370. doi:10.1177/2377960820901370
51. Jordan S, Logan PA, Panes G, Vaismoradi M, Hughes D. Adverse drug reactions, power, harm reduction, regulation and the ADRe profiles. Pharmacy (Basel). 2018;6:3.
52. Ensing HT, Stuijt CC, van den Bemt BJ, et al. Identifying the optimal role for pharmacists in care transitions: a systematic review. J Manag Care Spec Pharm. 2015;21(8):614–636.
53. Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):397–403. doi:10.7326/0003-4819-158-5-201303051-00006
54. World Health Organization (WHO). Medication Safety in Transitions of Care: Technical Report. World Health Organization; 2019. Available from: https://www.who.int/patientsafety/medication-safety/TransitionOfCare.pdf?ua=1.
55. Almanasreh E, Moles R, Chen TF. The medication reconciliation process and classification of discrepancies: a systematic review. Br J Clin Pharmacol. 2016;82(3):645–658. doi:10.1111/bcp.13017
56. Lee KP, Hartridge C, Corbett K, Vittinghoff E, Auerbach AD. “Whose job is it, really?” Physicians’, nurses’, and pharmacists’ perspectives on completing inpatient medication reconciliation. J Hosp Med. 2015;10(3):184–186. doi:10.1002/jhm.2289
57. van Sluisveld N, Zegers M, Natsch S, Wollersheim H. Medication reconciliation at hospital admission and discharge: insufficient knowledge, unclear task reallocation and lack of collaboration as major barriers to medication safety. BMC Health Serv Res. 2012;12:170. doi:10.1186/1472-6963-12-170
58. Krivanek MJ, Dolansky MA, Kukla A, et al. Perspectives from academic and practice leaders on nursing student’s education and role in medication reconciliation. J Prof Nurs. 2019;35(2):75–80. doi:10.1016/j.profnurs.2018.07.005
59. Albert NM. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung. 2016;45(2):100–113. doi:10.1016/j.hrtlng.2015.12.001
60. Bethishou L, Herzik K, Fang N, Abdo C, Tomaszewski DM. The impact of the pharmacist on continuity of care during transitions of care: a systematic review. J Am Pharm Assoc (2003). 2020;60(1):163–177.e162. doi:10.1016/j.japh.2019.06.020
61. Dusek B, Pearce N, Harripaul A, Lloyd M. Care transitions: a systematic review of best practices. J Nurs Care Qual. 2015;30(3):233–239. doi:10.1097/NCQ.0000000000000097
62. Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009;(3):Cd000072.
63. Ozavci G, Bucknall T, Woodward-Kron R, et al. A systematic review of older patients’ experiences and perceptions of communication about managing medication across transitions of care. Res Social Adm Pharm. 2020. doi:10.1016/j.sapharm.2020.03.023
64. Tobiano G, Chaboyer W, Teasdale T, Raleigh R, Manias E. Patient engagement in admission and discharge medication communication: a systematic mixed studies review. Int J Nurs Stud. 2019;95:87–102. doi:10.1016/j.ijnurstu.2019.04.009
65. Moher D, Liberati A, Tetzlaff J, Altman DC, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
