Back to Journals » Clinical Ophthalmology » Volume 14
The Role of Head Elevation in Treatment of Vitreous Haemorrhage
Authors Pongsachareonnont P , Rattana-aram N, Somkijrungroj T
Received 30 August 2019
Accepted for publication 19 November 2019
Published 7 January 2020 Volume 2020:14 Pages 7—13
DOI https://doi.org/10.2147/OPTH.S229109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Pear Pongsachareonnont, Nattadet Rattana-aram, Thanapong Somkijrungroj
Vitreoretinal Research Unit, Department of Ophthalmology, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, Thailand
Correspondence: Pear Pongsachareonnont
Department of Ophthalmology, King Chulalongkorn Memorial Hospital, 1873 RamaIV Road Payathai, Bangkok 10330, Thailand
Tel +66 2 256 4144 ext 0
Email [email protected]
Objective: To investigate the effect of head elevation on macular clearance of acute vitreous haemorrhage.
Design: Crossover, prospective, randomized clinical study.
Setting: University, tertiary care hospital.
Participants: 24 vitreous haemorrhage patients, average age 55 years.
Methods: Patients with acute vitreous haemorrhage who were randomly separated into 2 groups. In group A, the patients were assigned normal head position for the first week of sleep, then switched to head elevation for the second week (n=12). In group B, the patients were assigned the head position in reverse order (n=12). A washout period of 24 hrs was used between treatments. The carryover, sequence, and treatment effects were analysed by using various mixed models.
Outcomes: Best-corrected visual acuity (BCVA), vitreous haemorrhage grading, fundus photo colour intensity, and self-assessment scores.
Results: Although the mean BCVA (LogMAR) change following head elevation was higher than following normal head position, the difference was not statistically significant (−0.053 and 0.065 LogMAR, respectively, p = 0.2). Vitreous haemorrhage grading in the central region showed no statistical improvement in either group. Fundus photo colour intensity comparison in all fundus areas also showed no statistically significant differences in either group.
Conclusion: Although head elevation is recommended to patients with acute vitreous haemorrhage, this study showed no statistically significant improvement in BCVA, vitreous haemorrhage grading, or fundus photo colour intensity between head elevation and normal head position in the early observation period.
Trial registration: TCTR20150314001.
Keywords: vitreous haemorrhage, head elevation, visual acuity, fundus colour intensity
Synopsis
By sleeping with upright, a vitreous haemorrhage patient did not show higher improvement in the clearance of vitreous haemorrhage when compare to the sleep with normal head position.
Introduction
Vitreous haemorrhage (VH) is one of the most common causes of acute or subacute reduced vision worldwide. The incidence of spontaneous VH is 7 per 100,000.1 Visual disturbance from VH reduces patient quality of life.1 Importantly, VH can result from glaucoma,1 proliferative diabetic retinopathy, retinal tear without detachment, posterior vitreous detachment, rhegmatogenous retinal detachment, and proliferative retinopathy after retinal vein occlusion.2
The management of VH depends on its aetiology and visual prognosis. Treatment of the source of VH is required to prevent recurrent VH and long-term visual loss. VH itself can be treated conventionally by observation or surgical management.3 Notably, VH can spontaneously resolve and surgery is not necessary in some cases. Initial observation is preferred by some ophthalmologists if there is no urgent condition, such as retinal detachment or retinal breaks, or if the patient prefers conservative treatment. Vitrectomy surgery is also indicated in cases of non-clearing VH, neovascularization of the iris and/or angle, or ghost cell glaucoma.4 The timing of vitrectomy depends on its underlying aetiology. Blood in the vitreous cavity clears at a rate of approximately 1% per day, depending on a variety of factors, including haemolysis, liquefaction, phagocytosis, and fibrinosis.5 VH clears more rapidly in synergetic and vitrectomized eyes, whereas it clears slowly in younger eyes with well-formed vitreous.6 The natural history of VH depends on the underlying aetiology, with the worst prognoses for patients with diabetes and those with neovascular age-related macular degeneration.7 In the Diabetic Retinopathy Vitrectomy study (DRVS),8 there was no demonstrable benefit of early vitrectomy with respect to final visual acuity in patients with type 2 diabetes. The guidelines for vitrectomy indication in diabetic patients with VH comprise a lack of improvement after 4 weeks of observation. The majority (80%) of patients would then benefit from pars planar vitrectomy.
Ophthalmologists are frequently taught that patients with VH must follow a regimen of bed rest and head elevation.9 The main goal is to facilitate settling of the blood, thereby improving visual function and view on fundus examination. In the current practice, ophthalmologists generally recommend head elevation during sleeping time for patients with VH.2 However, there are many disadvantages of elevated head position, such as inability to sleep due to uncomfortable position, neck discomfort, and daytime somnolence.10
To the best of our knowledge, there has been no experimental study showing the benefits of an elevated head position in clearance of VH. The results of previous studies regarding this issue remain controversial and insufficient.1–3 Thus, this experimental study was undertaken to assess the effect of head elevation on the clearance of central VH.
Materials and Methods
This prospective randomized crossover trial was approved by the institutional review board at King Chulalongkorn Memorial Hospital, Bangkok, Thailand (IRB No. 621/57). The study was performed in accordance with the ethical standards established in the Declaration of Helsinki and was registered in the Thai Clinical trials registry (TCTR20150314001).
Patient Selection and Randomization
This study enrolled 26 patients with acute onset of VH who visited the ophthalmology clinic at King Chulalongkorn Memorial Hospital from June 1, 2015 through June 1, 2016.
Inclusion criteria were: patient age >18 years old with evidence of acute onset of new VH within the prior 1 month, best-corrected visual acuity (BCVA) less than 20/50 or a reduction of more than 3 lines of the EDTRS chart from baseline, and an initial conservative treatment plan for VH.
Exclusion criteria were: history of recent eye injury within 3 months; previous treatment with intravitreal anti-VEGF agents or other intravitreal drugs by injection within 1 month before enrolment, or plan to undergo intravitreal drug injection within 1 month; retinal specialist preference for surgery within 1 month; VH with ultrasonographic evidence of retinal break or rhegmatogenous retinal detachment; advanced cataract affecting fundal examination (nuclear sclerosis grade >2+, cortical grade >1+, posterior subcapsular grade >1+ and posterior polar cataract); patients with limited ability to elevate head position at 45 degrees, such as patients with neck and C-spine abnormality; and patients with limited ability to lie in the supine position, such as patients with heart failure, end-stage renal disease, or pulmonary congestion.11
After obtaining consent from patients, treatment sequence was randomized via 1:1 allocation in blocks of four by using a computerized randomization generator with numbers sealed in envelopes for allocation concealment. The first group of patients were assigned to sleep with normal head position for the first week, then switch to head elevation for the second week (group A). The second group of patients were assigned to sleep with head elevation for the first week and switch to normal head position for the second week (group B). In the head elevation period, patients were asked by the investigation team to use a customized triangular pillow (45 degrees of head elevation) during sleep hours. Conversely, in the normal head position period, the patients were asked to use a control pillow (standard flat pillow). The washout period was set at 24 hrs between treatments. Patient pillow usage was checked by phone on the first day after each visit.
The primary endpoint was BCVA at the end of each treatment period. The secondary endpoint was VH grading by a retinal specialist, fundus photo pixel analysis, and vision self-questionnaire scores.
In case of incomplete follow up, the patient’s data were not included in this analysis.
Patient Examination
Complete ophthalmic examinations were performed before each pillow assignment and at 1-week follow-up visits. At each visit, patients underwent BCVA measurement via Snellen chart visual acuity examination. Measurements were performed by a trained technician who was blinded to the randomization. Clinical examinations were performed, including dilated funduscopic VH grading and fundus photography. There are few accepted standardized scales for grading VH;12,13 thus, it is largely subjective and tends to vary among clinicians. In this study, the quasi-quantitative approach for VH grading (by Ziemianski et al) was used with stages 0–4, where 0 exhibits no vitreous haze and 4 involves total vitreous haze.12
Fundus photography was performed by a trained ophthalmic technician, who was masked to the randomization, by using a TRC-50IX retina camera (Topcon© America Corporation, Oakland, NJ, USA) by flashing scale at 3 and 30 degrees at central fixation, upgaze, downgaze, medial gaze, and lateral gaze. Five funduscopic pictures were analysed in 6 areas: area 1 (macular area), area 2 (optic disc area), area 3 (2 disc-diameter distance superotemporal from macula), area 4 (2 disc-diameter distance inferotemporal from macula), area 5 (2 disc-diameter distance superonasal from optic disc), and area 6 (2 disc-diameter distance inferonasal from optic disc). Pixel colour analysis was performed in each area by Adobe Photoshop CS6 version 13.0 (Adobe Systems Incorporated, San Jose, CA, USA). We used a customized template for each individual patient. The template included all 6 areas, in which each area equated to 1 disc-diameter area of each patient and the distance between areas equated to 2 disc-diameters, as described above and shown in Figure 1. The template was placed on the fundus photo to ensure that the same area would be analysed in each visit, with the optic nerve as a reference. The measurement of colour intensity changes was performed at the centre of each area by pixel analysis (11*11 pixels within the Photoshop CS6 program). The VH colour were select to be white haemorrhage or dark haemorrhage categories before grading by a blind single examiner. In the baseline examination and at the end of each treatment, the patients were asked to grade their vision and effect on their lifestyle by 8 questions (Translated from Thai language, see Appendix 1 provided) including:
- Difficulty in distance vision.
- Difficulty in near vision.
- How vision affected their normal lifestyle.
- Severity of neck pain.
- Changes in sleeping time, compared with typical sleep.
- Difficulty in sleeping.
- Severity of dyspnoea during sleep.
- Severity of obstructive sleep apnoea.
Each question was graded with an ordinal score of 0–10, where 0 was lowest symptom/severity and 10 was maximum symptom/severity.
Statistical Analysis
Based on a pilot crossover randomized study and by using a web-based sample size calculator for a parallel study (Creative Research Systems, Sebastopol, CA, USA), assuming a rate of VH clearance at 1% per day,5 and an alpha of 0.05, a total of 24 patients were necessary to achieve a power of 80%. Power calculation required 12 patients in each studied group (total n=24) to ensure that changes in BCVA could be predicted with a 95% confidence interval (CI). BCVA in Snellen form was converted to LogMAR units to provide continuous variable data.14 All statistical analyses were conducted by using R i386 version 3.2.5 software package (R studio©, Boston, MA, USA). Comparisons of baseline characteristics between the 2 groups were performed by using a generalized linear mixed model to confirm successful randomization. For normally distributed values, a linear mixed model was used to analyse continuous data, including LogMAR visual acuity and colour intensity. An ordinal mixed effects model was used to analyse ordinal data, including VH grading and self-vision assessment scores. Carryover and sequence effects were analysed by various mixed effects models. P values less than 0.05 were considered statistically significant.
Results
Of all 26 patients, 24 patients completed the study. Two patients were lost to follow-up during the second week. Baseline characteristics of the patients are shown in Table 1. Demographic and comorbidity data did not differ between the 2 groups. Patients randomized to Group B had better BCVA and were younger by a mean of 3.2 years than those in Group A.
 |
Table 1 Baseline Patient Characteristics of Each Group and Overall (Combined Groups) |
Mean BCVA in the head elevation group was 1.436 LogMAR at baseline and 1.383 LogMAR after 1 week of head elevation. Mean BCVA in the non-head elevation was 1.368 LogMAR at baseline and 1.433 LogMAR after 1 week of normal head position. Changes in BCVA from baseline to the 1-week follow-up were −0.053 LogMAR in the head elevation group and 0.065 LogMAR in the non-head elevation group, as shown in Table 2. There were no significant differences in BCVA improvement between the head elevation and non-head elevation groups (mean difference = −0.11 LogMAR, 95% CI: −0.05, 0.15; p=0.2). The various mixed effects models showed no statistically significant carryover or sequence effects in BCVA, VH grading, or colour intensity analysis, with the exception of nasal VH grading (P<0.01); thus, these measurements were eliminated from the analysis.
 |
Table 2 Mean BCVA Changes in Each Group |
Median VH grades at central locations in the head elevation and non-head elevation groups were equal at baseline (2.5). Median VH grades improved to 2 for both groups at the end of the study. Differences between the 2 groups in VH grades at central locations showed no statistical significance (OR=0.41, 95% CI: 0.092, 1.845; p=0.24). There were also no statistically significant differences in the non-head elevation group in central, superior, inferior, and temporal location, as shown in Table 3.
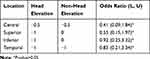 |
Table 3 Median Changes in Vitreous Haemorrhage Grade |
Fundus pixel colour intensity in 6 areas was compared between treatment groups. We found that newer VH appeared darker in fundus photos, whereas older VH appeared whiter. VH status was analysed by a single-trained ophthalmologist. Total net changes were evaluated and adjusted according to white or dark types of VH. Colour changes were used to clarify the improvement of VH of both forms. Data were analysed by using an ordinal mixed effects model which showed no statistically significant improvement in the head elevation group, compared with the non-head elevation group, in all areas. The mean colour intensity in the macular area of the head elevation group was 250.13 at baseline and 243.00 at the 1-week follow-up. The mean colour intensity in the macular area of the non-head elevation group was 236.30 at baseline and 251.12 at the 1-week follow-up. The difference in macular area between both groups was not statistically significant (mean difference= −11.75, 95% CI: −33.21, 9.71; p=0.14). There were no significant sequence or carryover effects in any areas (p>0.05). Table 4 shows changes in colour intensity.
 |
Table 4 Mean Absolute Fundus Pixel Colour Intensity Change |
In the self-assessment of 8 questionnaires, severity grading questions number 1 and 3 (distance vision and effect of lifestyle) had significant carryover effects (P<0.01 and 0.02, respectively); thus, they were not included in the analysis. There was no statistically significant improvement of severity grading question number 2 (near vision) between the head elevation and non-head elevation groups (median severity grading reduction of 1 in head elevation group and no change in non-head elevation group, OR=0.04, 95% CI: −0.38, 0.46, p=0.42). Severity grading question numbers 4 to 8 were not normally distributed. Scores of 0 in each question were 12 (50%), 15 (62.5%), 16 (66.7%), 22 (91.7), and 17 (70.8%), respectively, for severity grading question numbers 4 to 8. However, neck pain score and sleep time worsened in the head elevation group. Median severity grading in question number 4 (neck pain) increased from 2 to 3 in the head elevation group and decreased from 2 to 1 in the non-head elevation group. Median severity grading in question number 5 (sleeping quality) increased from 0 to 1 in the head elevation group and did not change from 0 in the non-head elevation group. Median severity grading in question numbers 6, 7, and 8 did not change from 0 in both the head elevation and non-head elevation groups.
Discussion
The recommendation for patients with VH to perform head elevation may permit intrahyaloid and retrohyaloid blood to settle, allowing improved visual outcome and better views for posterior segment examination.2 Clearance of haemorrhage occurs through erythrocyte exit through the trabecular meshwork, or can persist within the vitreous for many months.15 Our study found no significant difference between head elevation and non-head elevation with respect to visual outcome. Improvement of VH in the head elevation group in our study might have occurred as a result of the natural degradation of blood in the vitreous cavity and precipitation of blood at the inferior portion, due to gravitational force. In contrast, in the non-head elevation group, blood may have precipitated at the posterior pole and macular area, resulting in slight deterioration of visual outcome, as noted in our results above. There was an insufficient number of patients to perform subgroup analysis, which was necessary to clarify the effect on vitrectomized eyes with respect to the clearance of VH.
In fundus photography of acute VH, fresh blood appears dark red in colour; however, in chronic VH, red blood cells undergo haemolysis and the haemorrhage appears whiter in colour.5 Although we enrolled patients with acute onset of VH, in fundus analysis we found the appearance of chronic forms in 6 patients (25%). The white colour of old haemorrhage increases in colour intensity and becomes darker due to the normal orange colour of the normal fundus. Conversely, the dark colour of new haemorrhage decreases in colour intensity over time. Consequently, we analysed absolute colour change to measure the improvement of VH.
Kobayashi et al suggested that elevating head position produces substantial reductions in upper airway collapsibility and maintains upper airway patency during sleep.16 Pillow height elevation significantly increases the average and peak pressures of the cranial and cervical regions, and increases the extension and lordosis of the cervical spine; these are believed to reflect the quality of sleep.10 In our results, there was no improvement of dyspnoea and apnoea; however, neck pain score, sleep time, and sleep comfort worsened in the head elevation group, as a result of normal sleep ergonomics.
The strength of this study is its randomized design and the placement of all patients in both groups by crossover design, thus reducing confounding effects. The limitations of this study are its sequence and carryover effects in specific portions of VH grading, possibly due to measurement bias. There were also a limited number of samples and a relatively short follow-up period. Larger sample size and long-term follow-up are needed to determine the final BCVA and overall recovery rate of patients with VH.
In conclusion, despite the advice for patient head elevation that has been taught for many years in ophthalmology training, we found that the head elevation recommendation for patients with acute VH might not help to increase central VH clearance and may cause greater discomfort and neck pain during sleep. Bed rest and sleep with a normal pillow can thus be advised for conservative treatment of VH to improve BCVA and allow patients to maintain a good quality of sleep.
Article Summary
Strengths
- First to compare the elevation of head and lie flat during sleep in vitreous haemorrhage patient.
- Crossover-randomized study.
- Using imaging technique for outcomes evaluation.
Limitations
- Small number of participants but reaching the planned sample size estimation.
- Longer follow-up period is required for final visual outcomes.
Ethical Approval and Patient Consent
The study protocol was approved by the institutional review board at King Chulalongkorn Memorial Hospital, Bangkok, Thailand (IRB No. 621/57). Written informed consent was obtained from all patients who participated in the study.
Data Sharing Statement
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Acknowledgments
We thank Assoc. Prof Cameron Paul Hurst for statistical analysis.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lindgren G, Sjodell L, Lindblom B. A prospective study of dense spontaneous vitreous hemorrhage. Am J Ophthalmol. 1995;119(4):458–465. doi:10.1016/S0002-9394(14)71232-2
2. Sarrafizadeh R, Hassan TS, Ruby AJ, et al. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundus-obscuring vitreous hemorrhage. Ophthalmology. 2001;108(12):2273–2278. doi:10.1016/S0161-6420(01)00822-3
3. El Annan J, Carvounis PE. Current management of vitreous hemorrhage due to proliferative diabetic retinopathy. Int Ophthalmol Clin. 2014;54(2):141–153. doi:10.1097/iio.0000000000000027
4. Brucker AJ, Michels RG, Green WR. Pars plana vitrectomy in the management of blood-induced glaucoma with vitreous hemorrhage. Ann Ophthalmol. 1978;10(10):1427–1437.
5. Spraul CW, Grossniklaus HE. Vitreous hemorrhage. Surv Ophthalmol. 1997;42(1):3–39. doi:10.1016/S0039-6257(97)84041-6
6. Dana MR, Werner MS, Viana MA, et al. Spontaneous and traumatic vitreous hemorrhage. Ophthalmology. 1993;100(9):1377–1383. doi:10.1016/S0161-6420(93)31472-7
7. El Baba F, Jarrett WH
8. Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Four-year results of a randomized trial: diabetic retinopathy vitrectomy study report 5. Arch Ophthalmol. 1990;108(7):958–964. doi:10.1001/archopht.1990.01070090060040
9. Ophthalmology Aao. Vitreous hemorrhage: diagnosis and treatment. Secondary Vitreous Hemorrhage. 2007. Available from: https://www.aao.org/eyenet/article/vitreous-hemorrhage-diagnosis-treatment-2.
10. Ren S, Wong DW, Yang H, et al. Effect of pillow height on the biomechanics of the head-neck complex: investigation of the cranio-cervical pressure and cervical spine alignment. PeerJ. 2016;4:e2397. doi:10.7717/peerj.2397
11. Chylack LT
12. Ziemianski MC, McMeel JW, Franks EP. Natural history of vitreous hemorrhage in diabetic retinopathy. Ophthalmology. 1980;87(4):306–312. doi:10.1016/S0161-6420(80)35232-9
13. Bhavsar AR. Vitrase for the treatment of vitreous hemorrhage. Retinal Physician. 2005;2(5):42–44.
14. Chen FK, Agelis LE, Peh KK, et al. Factors contributing to discrepancy between visual acuity fractions derived from a Snellen chart and letter scores on the early treatment diabetic retinopathy study chart. Asia-Pac j Ophthalmol. 2014;3(5):277–285. doi:10.1097/apo.0000000000000007
15. Spaide RF, Fisher YL. Intravitreal bevacizumab (Avastin) treatment of proliferative diabetic retinopathy complicated by vitreous hemorrhage. Retina. 2006;26(3):275–278. doi:10.1097/00006982-200603000-00004
16. Kobayashi M, Ayuse T, Hoshino Y, et al. Effect of head elevation on passive upper airway collapsibility in normal subjects during propofol anesthesia. Anesthesiology. 2011;115(2):273–281. doi:10.1097/ALN.0b013e318223ba6d
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.