Back to Journals » Integrated Pharmacy Research and Practice » Volume 6
The role of community pharmacists in patient counseling and health education: a survey of their knowledge and level of involvement in relation to type 2 diabetes mellitus
Authors Erku DA , Belachew SA, Mekuria AB , Haile KT, Gebresillassie BM, Tegegn HG , Ayele AA
Received 30 April 2017
Accepted for publication 7 June 2017
Published 19 July 2017 Volume 2017:6 Pages 137—143
DOI https://doi.org/10.2147/IPRP.S140777
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Jonathan Ling
Daniel Asfaw Erku,1,* Sewunet Admasu Belachew,1 Abebe Basazn Mekuria,2 Kaleab Taye Haile,3 Begashaw Melaku Gebresillassie,1 Henok Getachew Tegegn,1 Asnakew Achaw Ayele1,*
1Department of Clinical Pharmacy, 2Department of Pharmacology, 3Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, University of Gondar, Gondar, Ethiopia
*These authors contributed equally to this work
Purpose: The present study aimed at evaluating the knowledge and level of involvement of community pharmacists in the provision of patient counseling and health education services for patients with DM and perceived barriers that limit the delivery of such services.
Materials and methods: A self-administered questionnaire based-survey was undertaken from January to March, 2017 with 412 pharmacists working in community pharmacies in six cities of Amhara regional state of Ethiopia: Debre Markos, Gondar, Dessie, Bahir Dar, Woldya, and Debre Birhan. Descriptive statistics, ANOVA, and Student’s t-test were employed to examine different variables.
Results: Community pharmacists were found to have poor knowledge and low level of involvement, with an overall mean score of 11.54 and 2.06, respectively. A significant number of community pharmacists never practiced promoting smoking cessation (45.2%), counseling on good foot care techniques (33.7%), and counseling on the potential impact of over–the-counter and herbal drugs on DM management (34%). On the other hand, describing the right time to administer antidiabetic medications (46%) and counseling on suitable administration, handling, and storage of insulin (33.7%) were done more frequently. The main reported barriers to the delivery of these services were lack of knowledge or clinical skills, lack of access to additional training programs, and lack of personnel or resources.
Conclusion: The present study revealed a poor knowledge and low level of involvement in counseling and health education services for patients with DM. Lack of knowledge or clinical skills was the most commonly reported barrier for providing such services. In order to better integrate community pharmacies into future public health programs and optimize the contribution of pharmacists, interventions should focus on overcoming the identified barriers.
Keywords: community pharmacy, patient counseling, diabetes mellitus, Ethiopia
Introduction
DM is a chronic devastating disease that, regardless of recent advances in care and management, still precipitates substantial morbidity and long-term complications.1 It is a growing chronic disease with expected global prevalence of more than 552 million by the year 2030.2 In Ethiopia, the number of patients living with diabetes is increasing at an alarming rate, with a national prevalence close to 6.5%.3 The high prevalence and the chronic nature of this disease make it imperative the need of diabetes disease state management. Many approaches are known to improve diabetes disease control including effective screening, management, regular monitoring, and consistent follow-up.4 The patients’ medication adherence, lifestyle modifications, and regular monitoring of blood glucose are some of the factors which contribute to better health outcome and can be significantly affected by health education and counseling.5,6
One of the main goals of the agenda set by the WHO for the future of public health is to form accessible, multidisciplinary networks of public health professionals who actively engage within communities and provide key public health services, including screening and health promotion service for chronic diseases.1 Community pharmacies, being one of the most easily accessible and widely distributed health professionals among the community, could be an indispensable component of this agenda. Community pharmacies’ location in the heart of the community provides a platform for more proactive contribution in solving gaps in programs including health promotion and a variety of preventive services.7
The role of community pharmacists is expanding globally from merely dispensing medication to involving in different public health services and playing a key role in disease state management.8–12 Many studies conducted elsewhere in the globe demonstrate that pharmacist’s involvement in diabetes management resulted in reduced cost burden to the patient and improved overall treatment outcome and patient satisfaction.13–16 However, there are a number of barriers that have hindered the provision of public health services in community pharmacy settings. Lack of knowledge and skills, lack of confidence and adequate training, lack of policies, poor recognition within the health care system, patients’ reluctance to use pharmacy services, and presence of inadequate number of pharmacy staff are some of the factors that can contribute to the low level of pharmacy services uptake and public health initiatives.17
Unlike the developed countries, community pharmacists in Ethiopia are not yet legally included as health care professionals within the public health workforce, and their role in providing public health services is yet to be recognized and endorsed by public health and other health care professionals. Rather, they tend to focus more on their traditional role of dispensing medication. The aim of the present study was to document the knowledge and level of involvement of community pharmacists in the provision of screening and health promotion services for patients with T2DM and the perceived barriers that limit their involvement in the delivery of such services.
Materials and methods
Study design, setting, and sampling
A self-administered questionnaire was distributed to all community pharmacists and pharmacy technicians practicing in CDROs of six selected cities of Amhara regional state (Debre Markos, Gondar, Dessie, Bahir Dar, Woldya, and Debre Birhan), the second most populous region among the nine regional states of Ethiopia. The region covers an area of 154,709 km2, and the region is divided into 11 zones for administrative purpose.18 According to the recent report by Federal Ministry of Health’s Health Sector Development Program IV (2010–2015), there were a total of 661 active CDROs in the country at the end of 2010. As there is no available data on the proportion of pharmacists and pharmacy technicians currently practicing in each of the cities and regions, all of the consenting community pharmacists and pharmacy technicians working in the aforementioned cities were invited to participate in this survey. This study was approved by the ethical committee of University of Gondar, with a references number of SoP- UoG/0124/2017. Written informed consent from all participants was also gained before commencing the study. Participants’ information obtained was kept confidential.
The study tool
The questionnaire was created by modifying items in previously used instruments regarding the role of community pharmacists in management of diabetic status,17,19 and items were thoroughly reviewed for relevance by a team of experts including experienced pharmacists and public health experts. The final study tool included three main parts. Part one contained questions regarding the sociodemographic characteristics of respondents including age, sex, year of experience, and highest educational level attained. Part two included questions regarding the knowledge and level of involvement of community pharmacists toward screening and health promotion services for T2DM patients. Knowledge was assessed by a 20-item questionnaire adopted from the Michigan Diabetes Research Training Centre Diabetes Knowledge Test. The questions had only one “correct” answer, and 1 point was assigned for every correct answer. Using published literatures as a reference,20,21 the overall score was subclassified into good knowledge (17–20), moderate knowledge (13–16), and poor knowledge (0–12). The level of involvement of community pharmacy professionals were assessed by a series of nine diabetic care service questions, and their level of response was scored as never, rarely, often, and always. The “always” choice was considered as good practice, and other choices were considered as negative practice. One score was given to each “always” option, and the practice score was calculated by adding the points accordingly. Respondent-perceived barriers in the delivery of such services were then assessed using Likert scale questions (0= not at all problematic to 5= extremely problematic) and included data on lack of knowledge or clinical skills, lack of personnel or resources, lack of clinical tools, lack of coordination with other health care professionals, lack of access to additional training programs, and lack of time.
Data analysis
The responses from each study site were manually entered into SPSS Inc. (Cary, NC, USA) version 21.0 and were double-checked for accuracy. Descriptive statistics, ANOVA, and Student’s t-test were employed in order to examine different variables. A P-value of less than 0.05 was considered significant.
Result
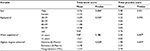
Among 472 community pharmacists approached, 412 completed the survey, leading to a response rate of 87.3%. Among the respondents, 284 (68.9) were males, with a mean (with SD) age of 28.7±8.4 years. The characteristics of respondents and CDROs are shown in Table 1.
Overall, community pharmacists were found to have poor knowledge and practice, with a mean knowledge score of 11.54 and mean practice score of 2.06. In fact, only 2.05% had good knowledge, 18% had fair knowledge, and 79.9% of them had poor knowledge as per the definition set in our study. Promoting smoking cessation and counseling on good foot care techniques was not at all practiced by 45.2% and 33.7% of community pharmacists, respectively. In addition, about 34% of pharmacists never practiced counseling on the potential impact of OTC and herbal drugs on diabetes management. Compared to other T2DM related counseling and health promotion services, describing the right time to administer antidiabetic medications and counseling about missed doses (46%) and regarding suitable administration, handling, and storage of insulin was done more frequently (33.7%) (Table 2).
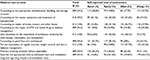  | Table 2 Levels of involvement of community pharmacists in counseling and health promotion services, Ethiopia, N=412 Abbreviation: OTC, over the counter. |
Our analysis showed that there was a significant mean difference in knowledge of community pharmacists among different age groups, with pharmacists between 30 and 39 years old (mean =12.44) having higher knowledge than those between 18 and 29 years old (mean =10.89) (P=0.025). Similarly, females had higher mean knowledge (mean =12.32) than males (P=0.046) toward DM management. Regarding the level of involvement of community pharmacists, those with more than 5 years of work experience (mean =3.02, P=0.007) and with a postgraduate qualification (mean =3.78, P=0.007) had higher mean practice score than those with less than 5 years of work experience (mean =2.45) and with a diploma qualification (mean =1.98) (Table 3).
Perceived barriers to the provision of counseling and health promotion services
As shown in Table 4, lack of knowledge or clinical skills was the most commonly reported barrier for delivering counseling and health promotion services in the pharmacy, followed by lack of access to additional training programs. Two items, lack of personnel or resources and lack of access to additional training program, were more commonly perceived as serious problems in drug stores than in pharmacies (P-value<0.05).
Discussion
Community pharmacists can play a crucial role in diabetes management through regular screening, evaluation, health education, and referral.21 Since chronically ill patients visit pharmacies more frequently for their medicine refill, this is an ideal opportunity for the pharmacists to counsel and educate the patient regarding his/her condition more efficiently. In order to perform this, the community pharmacists need to have adequate knowledge about DM and its management as it is an important prerequisite for the provision of correct and adequate information for patients. To the best of our knowledge, this is the first survey to explore the knowledge and level of involvement of community pharmacists in counseling and health promotion services for T2DM patients in Ethiopia.
The majority of the respondents (79.9%) in our study had poor knowledge on diabetes management, which corroborates with the findings of similar studies conducted in Nepal (76.5%),22 Libya (69.6%),23 and Qatar (60%).24 The reasons of poor level of knowledge could be due to absence of enduring training and education for community pharmacists regarding chronic disease management, including DM, which has been shown to improve the pharmacist’s knowledge and practice.25 Overall, community pharmacists in our study were less intensely engaged in the provision of counseling and health promotion services for T2DM patients. Although the beneficial effect of involving community pharmacists in DM and other chronic conditions has been confirmed in different clinical trials,26 it is apparent from our study that community pharmacists’ involvement in Ethiopia is severely limited. Many other studies conducted elsewhere also showed that community pharmacists are mostly involved in activities pertaining to the dispensing of medications and have less intense involvement in public health activities.27 This is due to the narrow scope of Ethiopian community pharmacists as they are largely restricted to the dispensing of medications and seldom provide screening and counseling services on chronic diseases. While some community pharmacies are offering pharmaceutical care to chronically ill patients, the role is still in its infant stage. Their responsibilities in chronic disease state management and health promotion should be further developed to successfully tap their invaluable contribution to patient care. In Ethiopia, there are no appropriate counseling guidelines available for community pharmacists about diabetes disease management. Interestingly, a higher rate of counseling was reported on the appropriate administration, handling, and storage of insulin, and this was reflected in our study results. In contrast, studies done elsewhere reported a very low counseling rate.28,29 The ANOVA and post hoc tests indicated that respondents between the age of 30 and 39 years old had higher knowledge than those between 18 and 29 years old. Similarly, respondents with more than 5 years of work experience and with a postgraduate qualification had higher mean practice score than those with less than 5 years of work experience and with a diploma qualification. This is expected as community pharmacists become more experienced through years of practice, and so they will acquire a comparably good knowledge and ultimately a higher level of involvement toward counseling and health promotion services.
In our study, lack of knowledge or clinical skills was the most commonly reported barrier to expanding public health service delivery in the pharmacy; this was followed by lack of access to additional training programs. Studies conducted elsewhere in the globe have also documented important barriers including lack of time and personnel, lack of clinical skills, and lack of tools.17 Providing specific trainings that will fill the knowledge and skill gap required for the provision of such services is recommended both in academia and practice settings as it will result in the delivery of such services in a better and more skillful way than ever before. In order to better integrate community drug retail outlets into future disease state management programs and optimize the contribution of community pharmacy professionals, interventions should focus on overcoming the identified barriers, which starts from restructuring the health care system in order to integrate community pharmacists into the provision of a variety of diabetic care services that will ultimately improve the patients’ overall health outcome. Follow-up studies seeking their extent of involvement in diabetic care services on a national scale may also be needed to identify more barriers.
Limitations
This survey highlights an area of pharmacy practice where there is lack of literature. Yet, the survey has some limitations that should be taken into account while interpreting the results. As the study was a descriptive cross-sectional survey conducted in only six cities of Amhara regional state, caution should be exercised when generalizing to other cities and regions in Ethiopia. Moreover, our use of a self-administered questionnaire, which depends on honesty and faith of the respondents, could affect the responses as it may be subjected to social desirability bias. Even with the above limitations, this survey has significant implications for improving the involvement of community pharmacies in disease state management for patients with T2DM.
Conclusion
Community pharmacy professionals in our study had a poor knowledge and demonstrated a lower level of involvement in counseling and health promotion services for patients with T2DM patients Provision of advanced training and continuous education for community pharmacists, including regarding management of diabetes disease status, is recommended. Standard guidelines about diabetes care, counseling, and management also need to be distributed and implemented throughout the community pharmacies. Furthermore, continuous supervision and assessments with regard to the implementation of such guidelines are crucial in order to improve the level of involvement and optimize the contribution of community pharmacists.
List of abbreviations
ANOVA, analysis of variance; CDROs, community drug retail outlets; DM, diabetes mellitus; OTC, over the counter; SD, standard deviation; SPSS, Statistical Package for the Social Sciences; T2D, type 2 diabetes mellitus; WHO, World Health Organization.
Acknowledgments
The authors acknowledge the support of the School of Pharmacy, University of Gondar, in facilitating the data collection process. The authors are also thankful for the data collectors from all cities and for those pharmacists who took part in this study.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Global Strategy on Diet, Physical Activity and Health. Geneva: World Health Organization; 2004. | ||
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–321. | ||
Nshisso LD, Reese A, Gelaye B, Lemma S, Berhane Y, Williams MA. Prevalence of hypertension and diabetes among Ethiopian adults. Diabetes Metab Syndr. 2012;6:36–41. | ||
Venkartesan R, Devi AS, Parasuraman S, Sriram S. Role of community pharmacist in improving knowledge and glycemic control of type 2 diabetes. Perspect Clin Res. 2012;3(1):26–31. | ||
O’Loughlin J, Masson P, Déry V, Fagnan D. The role of community pharmacists in health education and disease prevention: a survey of their interests and needs in relation to cardiovascular disease. Prev Med. 1999;28(3):324–333. | ||
Paes AH, Bakker A, Soe-Agnie CJ. Impact of dosage frequency in patient compliance. Diabetes Care. 1997;20:1512–1517. | ||
Chua SS, Ramachandran CD, Paraidathathu TT. Response of community pharmacists to the presentation of back pain: a simulated patient study. Int J Pharm Pract. 2006;14:171–178. | ||
Anderson C, Blenkinsopp A, Armstrong M. The contribution of community pharmacy to improving the public’s health: summary report of the literature review 1990–2007. Available from: http://eprints.nottingham.ac.uk/1576/. Accessed in December 01, 2016. | ||
Dent LA, Harris KJ, Noonan CW. Randomized trial assessing the effectiveness of a pharmacist-delivered program for smoking cessation. Ann Pharmacother. 2009;43:194–201. | ||
Mangum SA, Kraenow KR, Narducci WA. Identifying at-risk patients through community pharmacy-based hypertension and stroke prevention screening projects. J Am Pharm Assoc (Wash). 2003;43:50–55. | ||
Hess KM, Dai CW, Garner B, Law AV. Measuring outcomes of a pharmacist-run travel health clinic located in an independent community pharmacy. J Am Pharm Assoc. 2010;50:174–180. | ||
Mehuys E, Van Bortel L, De Bolle L, et al. Effectiveness of a community pharmacist intervention in diabetes care: a randomized control trial. J Clin Pharm Ther. 2011;36(5):602–613. | ||
Gerber RA, Liu G, Mccombs JS. Impact of pharmacist consultations provided to patients with diabetes on healthcare costs in a health maintenance organization. Am J Manag Care. 1998;4(7):991–1000. | ||
The R, Chen T, Krass I. Consumer perspectives of pharmacist delivered health promotion and screening services. Int J Pharm Pract. 2001;9:261–267. | ||
Armour CL, Taylor SJ, Hourihan F, Smith C, Krass I. Implementation and evaluation of Australian pharmacists’ diabetes care services. Medscape. 2004. Available from: http://www.medscape.com/viewarticle/487477. Accessed in December 01, 2016. | ||
Reddy PV, Kapoor KV. Impact of patient counseling on knowledge of diabetes mellitus and its management. Ind J Hospital Pharm. 2005;42:96–99. | ||
Dhippayom T, Fuangchan A, Tunpichart S, Chaiyakunapruk N. Opportunistic screening and health promotion for type 2 diabetes: an expanding public health role for the community pharmacist. J Public Health. 2013;35:262–269. | ||
Central Statistical Agency (CSA) of Ethiopia. Summary and Statistical Report of the 2007 Population and Housing Census. Addis Ababa, Ethiopia: CSA; 2008. | ||
Michigan Diabetes Research Training Centre Diabetes Knowledge Test. Available from: http://diabetesresearch.med.umich.edu/Tools_SurveyInstruments.php#dkt. Accessed in December 01, 2016. | ||
Al-Maskari F, El-Sadig M, Al-Kaabi JM, Afandi B, Nagelkerke N, Yeatts KB. Knowledge, attitude and practices of diabetic patients in the United Arab Emirates. PLoS One. 2013;8(1):e52857. | ||
Shrestha M, Maharjan R, Prajapati A, Ghimire S, Shrestha N, Banstola A. Assessment of knowledge and practice of community pharmacy personnel on diabetes mellitus management in Kathmandu district: a cross sectional descriptive study. J Diabetes Metab Disord. 2015;14:71. | ||
Eades CE, Ferguson JS, O’Carroll RE. Public health in community pharmacy: a systematic review of pharmacist and consumer views. BMC Public Health. 2011;11:582. | ||
Bisheya AF, El-Mijbri SB, Beshyah SA, Sherif I. Community pharmacists’ knowledge, attitude and practice towards diabetes care in Tripoli, Libya. Ibnosina J Med Biomed Sci. 2011;3(3):89–95. | ||
Basri MA, Yousef SE, ElHajj M. Diabetes Mellitus Care in the State of Qatar: A Survey of Pharmacists’ Activities, Attitudes and Knowledge. Qatar: Qatar University; 2013. | ||
Chen HY, Lee TY, Huang WT, Chang CJ, Chen CM. The short-term impact of a continuing education program on pharmacists’ knowledge and attitudes toward diabetes. Am J Pharm Educ. 2004;68(5):1–5. | ||
Snella KA, Canales AE, Irons BK, et al. Pharmacy- and community based screenings for diabetes and cardiovascular conditions in high-risk individuals. J Am Pharm Assoc. 2006;46:370–377. | ||
Laliberté MC, Perreault S, Damestoy N, Lalonde L. Ideal and actual involvement of community pharmacists in health promotion and prevention: a cross-sectional study in Quebec, Canada. BMC Public Health. 2012;12:192. | ||
Abduelkarem AR, Sackville MA, Morgan RM, Sackville MP, Hildreth AJ. Views and practices of community pharmacists regarding services for people with type 2 diabetes Int J Pharm Pract. 2003;11:161–168. | ||
Kotecki JE, Elanjian SI, Torabi MR. Health promotion beliefs and practices among pharmacists. J Am Pharm Assoc (Wash). 2000;40(6):773–779. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.