Back to Journals » Psychology Research and Behavior Management » Volume 14
The Role of Clinical Activity, Loneliness, and Satisfaction with e-Health Services as Factors Affecting Quality of Life in Patients with Rheumatoid Arthritis During the SARS-CoV-2 Pandemic
Authors Tański W
Received 1 August 2021
Accepted for publication 13 September 2021
Published 5 October 2021 Volume 2021:14 Pages 1581—1590
DOI https://doi.org/10.2147/PRBM.S332141
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Wojciech Tański
Department of Internal Medicine, 4th Military Teaching Hospital, Wroclaw, Poland
Correspondence: Wojciech Tański
Department of Internal Medicine, 4th Military Teaching Hospital, Weigla 5, Wroclaw, 53-114, Poland
Email [email protected]
Introduction: During the SARS-CoV-2 pandemic, most primary and specialist care outpatient clinics have started to offer their patients teleconsultation appointments as well as electronic prescriptions and referrals. For many patients, it was the only available way to access medical care.
Purpose: The aim of the study was to assess the quality of life in rheumatoid arthritis (RA) patients and determine whether loneliness and satisfaction with telemedicine service can affect their perceived QoL during the SARS-CoV-2 pandemic.
Material and Methods: One hundred and forty-three RA patients (mean age 45.83± 13.5 years) were included in the study. The De Jong-Gierveld Loneliness Scale (DJGLS), The Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL) and the questionnaire of satisfaction with teleconsultations were used in the study. The following statistical tests were used in the study: Spearman correlation test, multivariate linear regression. A significance level of 0.05 was used in the analysis.
Results: The patients presented a moderate level of loneliness (DJGLS; 31.1 points). The mean ASQoL score was 11.49± 4.64. The correlation analysis showed a significant positive relationship between the level of loneliness and QoL – the higher the level of loneliness, the poorer the QoL (rho=0.283; p=0.001). An analysis of the relationship between satisfaction with teleconsultations and perceived QoL showed a statistically significant negative relationship – the higher the level of satisfaction with teleconsultations, the better the QoL (b=− 0.166; p=0.047). The linear multivariate regression analysis showed that the loneliness (rho=0.1; p=0.01) was significant (p< 0.05) independent predictor of QoL.
Conclusion: During the SARS-CoV-2 pandemic, RA patients experienced loneliness and their QoL was low. Teleconsultation visits proved to be unsatisfactory and negatively perceived by patients. Higher severity of RA symptoms (weakness, fatigue), being unemployed and loneliness during the blockade are independent determinants of reduced QoL in RA patients.
Keywords: e-health, loneliness, SARS-CoV-2, rheumatoid arthritis
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune connective tissue disease that leads to disability and premature death.1 The symptoms of the disease mainly affect the locomotor system. As they intensify, RA patients lose the ability to function on a day-to-day basis with regard to self-maintenance and performance of work activities.2 The limitations caused by the disease often lead to a loss of independence and result in dependency on outside help. The recurrent pain associated with inflammation and limited joint mobility as well as the loss of autonomy have a negative influence on other aspects of functioning (mental, physical, social and environmental), which affects the perceived quality of life in these patients.3
Modern medicine aims both to increase the lifespan of patients and to improve their quality of life to a level comparable to that before the onset of the disease. As for the latter, the most commonly used definition is health-related quality of life (HRQoL), which is an important complement to the evaluation of clinical parameters. However, HRQoL can only be assessed by patients themselves. The assessment consists in comparing one’s current health condition with the desired health status.4,5 A patient’s subjective assessment of their health status is a practical factor that allows for a better planning and improvement of the quality of care provided to the patient. A patient’s self-assessment of their health indicates their limitations in functioning caused by the disease or the treatment administered.4
With the onset of the SARS-CoV-2 pandemic, there have been concerns that patients with rheumatic conditions may be at higher risk of contracting the coronavirus and experiencing severe COVID-19 symptoms, especially during acute episodes of their condition.8 This is due, on the one hand, to reduced immunity during inflammation, and on the other hand to the changes caused by an intensive treatment with immunosuppressive drugs.9 The slogans“stay at home”, “quarantine” and “maintain social distance” during the SARS-CoV-2 pandemic have been of particular relevance for patients with rheumatic conditions. If a patient with a rheumatic condition contracts COVID-19, it is important that the treatment of their condition is discontinued and resumed after 2 weeks of symptom-free observation.9 The current ACR and EULAR recommendations for the management of inflammatory joint diseases state that treatment with disease-modifying drugs, including biologics, should be continued only in those patients who were not infected or exposed.7,9
During the SARS-CoV-2 pandemic, most primary and specialist care outpatient clinics have started to offer their patients teleconsultation appointments as well as electronic prescriptions and referrals. For many patients it was the only available way to access medical care. In the case of RA patients, this form of care may seem to be a perfect solution, as rheumatology specialists have access to the medical records of their patients and know most of them. The ability to monitor the health condition of patients and provide medical advice by telephone allows doctors to continuously provide their patients with treatment appropriate to their health status and allows patients to avoid unnecessary contacts.10 This model of care may in principle seem to be appropriate for patients with rheumatic conditions. However, the opinions voiced by patients suggest that they are not fully satisfied with this form of care and that they were more satisfied with face-to-face appointments with specialists, which they considered to have been more effective in their treatment.11 One major problem during the SARS-CoV-2 pandemic has been the lack of access to rehabilitation, which is as important as pharmacological treatment in the case of patients with rheumatic conditions. Rehabilitation plays an important role in improving the ability of young patients to perform work-related activities and allows older patients to maintain mobility. Both the treatment methods should be used to ensure that comprehensive treatment is provided.6
In light of the above, we carried out a study on patients with RA, whose aim was to assess the quality of life in these patients and determine the factors that may affect their perceived QoL. The study also included an assessment of satisfaction with telehealth services and its impact on QoL. Moreover, the study addressed the issue of loneliness, which in the last year has been experienced by many people confined to their homes because of the SARS-CoV-2 pandemic. The study took into account such factors as the severity of symptoms, loneliness, and satisfaction with remote consultations with specialists, including consultations carried out using electronic means only.
Materials and Methods
The study was conducted using electronic means. Patients were invited to take part in the study through online social forums for patients with RA. In order to complete our online survey, patients had to give their consent for voluntary and anonymous participation in the study. Only those patients who in the period from November to April agreed to take part in the study by confirming their choice (clicking the consent and GDPR checkboxes) on the invitation website were invited to participate in the study. A link to the online survey was sent to 250 registered patients. We received 174 completed surveys. Once the data received were checked for completeness and compliance with the criteria adopted, 143 RA patients were ultimately included in the study.
The following standardised research tools were used in the study:
- The De Jong-Gierveld Loneliness Scale (DJGLS), which is used to measure loneliness in respondents.12 The overall score ranges from 11 to 55, with a higher score denoting a higher level of loneliness. There are no standards as to what score on the scale indicates a high or a low level of loneliness. However, an average number of points per item can be calculated and interpreted using the scoring scale for a single item, with 1 – definitely not lonely, 2 – not lonely, 3 – a neutral response, 4 – lonely, and 5 –definitely lonely.
- The Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL), which is used to assess QoLin patients with ankylosing spondylitis.13 The total score in the questionnaire ranges from 0 to 18, with a higher score denotingworseQoL. There are no official standards as to what score denotes good or poor QoL. For the purpose of our study, ASQoLwasadministered to RA patients. The patients were asked to answer the questions with reference to their current health status related to RA.
- Questionnaire of satisfaction with teleconsultations and care provided by specialist outpatient clinics during the SARS-CoV-2 pandemic, which investigated the level of satisfaction with the quality of remote consultations and their comparison with face-to-face appointments, comprehensibility of the information provided during teleconsultation appointments, and the possibility of having a teleconsultation appointment when needed. Satisfaction with the prescriptions provided during teleconsultation appointments was also assessed. The questionnaire comprises four items, with one point scored for each answer starting with ‘Yes’. The total score in the questionnaire ranges from 0 to 4, with a higher score denoting a higher level of satisfaction with teleconsultations. The results of the questionnaire are presented as a percentage of points that can be scored in the questions answered by the respondent. Thus, the level of satisfaction with teleconsultations ranges from 0 to 100%. Based on their scores for satisfaction with teleconsultations, respondents were divided into two groups, with a ≤50% cut-off point denoting dissatisfaction with teleconsultations: group 1 – patients dissatisfied with teleconsultations (n=75; 52.45%), group 2 – patients satisfied with teleconsultations (n=68, 47.55%).
- Questionnaire concerning clinical data, which was designed in such a way as to enable patients to rate the severity of their symptoms on a scale from 0 to 10 (the higher the score, the higher the severity of a given symptom).The DAS-28 - CRP scale recommended by ACR/EULAR was used to assess disease activity and the degree of joint damage.14
- Additionally, patients were asked about basic sociodemographic data.
Statistical Analysis
An analysis of quantitative variables (ie expressed in numbers) was carried out by calculating means, standard deviations, medians and quartiles. An analysis of qualitative variables (ie not expressed in numbers) was carried out by calculating the number and percentage of occurrences of each value. Correlations between quantitative variables were analysed using the Spearman correlation coefficient. A linear multivariate regression analysis of the impact of multiple variables on a quantitative variable was performed using linear regression. The results are presented as the parameter values in the regression model with a 95% confidence interval. A level of significance of 0.05 was used in the analysis. Thus, all p-values lower than 0.05 indicated significant relationships. The analysis was performed using the R software, version 4.0.5.15
Ethical Considerations
The study was carried out following approval from the Bioethics Committee of the Wroclaw Medical University (No. 52/2021). Participation was voluntary and anonymous, and all patients were informed about the study’s purpose and their right to decline or discontinue their participation. Data confidentiality was assured by using assigned code numbers in lieu of participants’ names. The study was performed in accordance with the Helsinki Declaration and the principles of good clinical practice, with respect for the rights and dignity of participants.
Results
Sociodemographic Characteristics
The mean age of the patients surveyed was 45.83±13.5 years. Over half of respondents had tertiary education (53.15%) and almost the same percentage were employed at the time of the study (56%). The vast majority of respondents were married or in a partnership (72.74%). The results are presented in Table 1.
 |
Table 1 Sociodemographic and Clinical Characteristics of the Group Studied |
The mean level of loneliness as measured using the DJGLS was 31.1 points, ie 2.83 points per question. The scores indicate that the respondents reported moderate levels of loneliness. The mean ASQoL score was 11.49 (SD = 4.64) out of a maximum of 18 points, with scores ranging from 1 to 18, which indicates a relatively sharp decrease in quality of life.
Severity of RA Symptoms
The respondents rated the severity of their RA symptoms on a scale from 1 to 10 (Table 2). The higher the rating, the higher the severity of the symptom. The symptoms rated as most severe were weakness, fatigue (7.07±2.32), hand and wrist joint pain (5.94±2.47), and large joint pain (5.91±2.7). The symptoms rated as least severe were swelling of hand and wrist joints (5.01±2.82), and foot joint pain (5.55±2.69).
 |
Table 2 Severity of Symptoms Characteristic of Rheumatoid Arthritis |
Satisfaction with Appointments During the Pandemic
All the respondents answered questions concerning satisfaction with teleconsultations (Figure 1). The overall level of satisfaction with teleconsultation appointments was 47.55%, which indicates low levels of satisfaction with this form of care. Thirty-one per cent of respondents were not satisfied with the way in which information related to the health problem for which they booked a teleconsultation appointment was provided to them during the appointment, 13.3% of respondents reported that their doctor did not provide them with any information and that they had to ask about all the details related to their treatment. Eighteen per cent of respondents reported that they had to ask for information about how to take their medication and about the causes of their medical problem. According to over 46% of respondents, the quality of the medical advice given during a teleconsultation appointment is not comparable to the quality of the advice provided during an in-person appointment. Sixteen per cent of respondents reported that their doctor only provided them with general information about medical recommendations during their teleconsultation appointment and that it was only through their own initiative that they obtained more precise information. Almost half of respondents reported that it is easier for them to establish a rapport with a doctor and obtain all the information necessary in relation to their treatment during in-person consultations.
 |
Figure 1 Satisfaction of respondents with teleconsultations. |
Impact of Selected Variables on Perceived Quality of Life
In the next stage of the study, an analysis of the relationship between loneliness and both quality of life and satisfaction with teleconsultations was carried out (Table 3). The analysis showed a significant (p<0.05) positive relationship between the level of loneliness and QoL, which means that the higher the level of loneliness, the poorer the quality of life (the higher the ASQoL score). An inverse relationship was observed between the level of loneliness and satisfaction with teleconsultations. It was found that the higher the level of loneliness, the lower the satisfaction with teleconsultations. However, the relationship was not statistically significant.
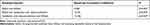 |
Table 3 Impact of the Level of Loneliness and Satisfaction with Teleconsultations on Perceived Quality of Life in RA Patients |
An analysis of the relationship between satisfaction with teleconsultations and perceived quality of life showed a statistically significant negative relationship. This means that the higher the level of satisfaction with teleconsultations, the better the quality of life (b=−0.166; p=0.047).
Analysis of the Impact of Symptom Severity on Quality of Life
An analysis of the impact of symptom severity on perceived quality of life showed a statistically significant positive relationship between each of the symptoms and perceived QoL. This means that the higher the severity of the symptoms, the poorer the quality of life (Table 4):
 |
Table 4 Analysis of the Correlation Between Symptoms and Perceived Quality of Life |
- the higher the severity of hand and wrist joint pain, the higher the ASQoL score (poorer QoL),
- the higher the severity of morning stiffness, the higher the ASQoL score (poorer QoL),
- the higher the severity of foot joint pain, the higher the ASQoL score (poorer QoL),
- the higher the severity of large joint pain, the higher the ASQoL score (poorer QoL),
- the higher the level of weakness and fatigue, the higher the ASQoL score (poorer QoL).
The Linear Multivariate Regression Analysis – Factors Affecting QoL
The linear multivariate regression analysis showed that the following variables are significant (p<0.05) independent predictors of quality of life (Table 5):
 |
Table 5 The Linear Multivariate Regression Analysis of the Impact of Selected Variables on Perceived Quality of Life |
- being unemployed - the regression parameter was 2.009, thus it increased the ASQoL score (decreased quality of life) by an average of 2.009 points as compared to being employed; and benefiting from a disability pension - the regression parameter was 3.178, thus it increased the ASQoL score (decreased quality of life) by an average of 3.178 points as compared to being employed.
- weakness, fatigue - the regression parameter was 0.593, thus these features increased the ASQoL score (decreased quality of life) by an average of 0.593 points.
- DJGLS - the regression parameter was 0.1, thus every “loneliness point” increased the ASQoL score (decreased quality of life) by an average of 0.1 point.
The R2 coefficient for this model was 54.35%, which means that 54.35% of variation in the quality of life variable is explained by the variables included in the model. The remaining 45.65% depends on variables that were not included in the model as well as random factors.
Discussion
Following the announcement of a state of epidemic from 20 March 2020 until further notice, and given that elderly people, the chronically ill, and patients with compromised immunity are at higher risk of experiencing severe COVID-19 symptoms, solutions have been introduced to enable patients to access health services remotely.This has significantly reduced their risk of infection due to limited contacts.16 Given that some patients were afraid of attending face-to-face appointments, teleconsultations have turned out to be an effective tool for ensuring the continuity of care.17 E-medicine involves the use of modern communication technologies to meet the needs of citizens, patients, medical experts, and persons responsible for the provision of medical services.18 One of the key aspects related to the functioning of medical facilities is patient satisfaction, which is an important element in the assessment of the quality of medical services provided. By meeting the expectations of patients, who play a vital role in healthcare facilities and other health entities, high quality services can be ensured.19 In our study, the patients surveyed were dissatisfied with teleconsultations, with less than half of respondents reporting satisfaction with this form of care. The majority of patients stated that the quality of teleconsultations is not comparable to the quality of in-person appointments. The insufficiently detailed information offered by doctors as well as difficulties getting through by phone and booking a teleconsultation appointment were major problems in relations between patients and healthcare professionals.
Over the last year, since the introduction of the modern forms of contact, measures have frequently been taken to assess the quality of the medical services provided in the new harsh reality of the SARS-CoV-2 pandemic.20 The results of the studies undertaken vary. In the survey of satisfaction with remote services conducted at the request of the Polish government, the services provided by primary care physicians were rated highly by patients.21 Some respondents in the survey stated that telephone/video consultations could be one of the main channels of contact between patients and primary care physicians, who would determine whether a face-to-face appointment is required. In the own study, according to approx. 30% of respondents, the quality of teleconsultation appointments is comparable to that of in-person appointments. The survey also found that as many as 80% of respondents had used the option to book a face-to-face appointment with their primary care physician following a teleconsultation appointment, which indicates that patients have a strong need for face-to-face contact with a doctor.21 The difference in the level of satisfaction with this form of care between our study and the survey referred to above may result from differences in the profile of the patients surveyed. In our study, the mean age of respondents was 45, whereas the largest proportion of patients using primary care services in the aforementioned survey were aged ≥ 60. The number of teleconsultation appointments also differed between the studies. In our study it was 3.3, whereas in the survey of patients using primary health care services, it was only 1.
Today, the expectations of patients continue to rise. Factors determining the quality of the medical services provided, and thus affecting patients’ level of satisfaction with these services, include: the way the patient is treated, the amount and quality of information provided, the time and attention given to patients by doctors and nurses, as well as the safety and accessibility of health services.22 The patients participating in our study rated the quality of teleconsultations negatively and complained that their doctor provided them only with general information about their treatment, rehabilitation and psychological problems. They also stressed that medical personnel showed no initiative during those interactions, which were perfunctory and limited to answering the questions asked. Once their main health-related problems have been attended to, patients may expect a different quality of care or have other needs, including those relating to the doctor-patient relationship.21 All aspects of care aimed at ensuring a holistic approach are extremely important for patients with chronic conditions.6 It is not only essential to treat the medical problems of patients, but also take care of their mind and spirit, especially in the light of the uncertainty, stress, limitation of social, professional and family interactions, as well as loneliness associated with the COVID-19 pandemic.23,24
Studies have shown that over 20% of RA patients are diagnosed with depression25 and that the higher the level of depression, the lower the self-care abilities and the higher the level of helplessness and loneliness in patients.26 It has been observed that widowed persons who do not have support from a loved one find it more difficult to cope with different aspects of life, including in particular the physical27 and social28 ones, as compared with people who are married or who are single by choice. Authors of studies on patients with chronic conditions indicate that loneliness has a significant negative impact on self-care ability,29 adherence30 and quality of life.31
Similarly to studies on patients with cardiac problems,32 our study found moderate levels of loneliness in the patients surveyed, which had a significant negative impact on the perceived quality of life and negatively influenced satisfaction with the medical services received. However, the latter relationship was not statistically significant. Studies have found a correlation between loneliness and an increased pro-inflammatory gene expression, which may initiate the development and progression of both acute and chronic conditions that contribute to comorbidities and mortality.33,34 It has also been reported that a lower level of loneliness results in improved immunity and reduced C-reactive protein levels.34 Loneliness and the pandemic situation are associated with high levels of stress. In her paper, Felsted notes that mindfulness is an effective treatment for a number of chronic conditions in older adults.35 It was found that mindfulness has an impact on both stress levels and disease activity in patients with RA. It was also demonstrated that mindfulness plays an important role in reducing psychological stress and the severity of joint stiffness, pain and tenderness.35
It is believed that there is a significant link between the mental status and QoL. According to Bai et al,36 there is a link between the medical measures of QoL and the mental status of patients, which suggests that it is necessary to ensure that treatment includes psychological interventions, especially in this difficult time of the SARS-CoV-2 pandemic. Researchers investigating health-related quality of life stress that for a patient-client higher quality of life does not mean a change in health parameters, but rather a perceived improvement in social and personal functioning. This clearly indicates that pharmacological treatment alone is not sufficient.37
Hand and wrist joint pain was the most severe symptom reported by the RA patients surveyed. In addition to medication, the treatment of pain should include non-pharmacological interventions, which are associated with a holistic approach and psychological measures aimed at teaching patients how to cope with pain and form positive attitudes.6 In her study, Felsted notes that there is a significant relationship between mindfulness and both reduction in pain intensity and improvement in sleep quality and quality of life.35 In light of the findings from our study, indicating that the patients surveyed were not satisfied with communication with their doctor during teleconsultation appointments, this may be difficult to achieve. This is because the patients complained that they did not receive sufficient information from their doctor during the appointments and that the doctor only focused on solving their physical health problem and issuing prescriptions. When confronted with the challenges associated with their condition, patients develop individual, subjective perception of their quality of life, which is not consistent with the assessment performed by a doctor based on external, objective determinants of QoL.37
It is worth stressing that wellbeing is a concept that encompasses two separate components: a balance between positive and negative emotions, and the cognitive evaluation of one’s life.38 In the case of patients with chronic conditions, negative emotions caused by pain, body deformities and restricted mobility may prevail, but this does not necessarily lead to a negative perception of one’s entire life.37 However, when the emotions experienced are coupled with loneliness and dissatisfaction with the medical services received, negative emotions can dominate and even an improvement and reduction in the symptoms associated with a given condition will not have the desired impact and will not result in an improvement in QoL.
Our study is the first to investigate the level of satisfaction with treatment and the perceived quality of life in RA patients during the pandemic. Our findings indicate that it is necessary to further study and expand on the issue concerned, as it is of vital importance for the care of patients with rheumatic conditions.
Conclusion
- During the SARS-CoV-2 pandemic, RA patients have experienced loneliness and their QoL has been poorer than before the pandemic.
- The proposed and implemented model of care in the form of teleconsultation appointments proves unsatisfactory and is negatively rated by patients.
- Both satisfaction with telehealth services and loneliness are factors that have a significant impact on perceived QoL.
- Higher severity of RA symptoms (weakness, fatigue), being unemployed, and loneliness during lockdown are independent determinants of reduced QoL in RA patients.
Study Limitation
Our study has several limitations. One of them is the lack of a control group of patients who had face-to-face appointments with a specialist. One additional problem is that the findings obtained during the pandemic were not compared to the results obtained before the pandemic. Another limitation of the study is the fact of using ASQoL questionnaire designed for patients with ankylosing spondylitis in patients with RA.The majority of patients were in a low clinical activity status, what may be important when examining QoL in RA patients. Another limitation of the study was the lack of assessment of depression, as a determinant of QoL and a common factor in RA patients. It is possible that feelings of loneliness and satisfaction with telemedicine may be more impaired in RA patients with depression. Additionally, according to the DAS-28 data, most patients had low disease activity, which made the results of the study more focused on patients responding to medication. Another limitation of our study is the fact of recruiting patients via the Internet on social networks, which may have an impact on the selection of the group. However, paying attention to the purpose of the study, it can be concluded that this group is the most frequently used telemedicine.
Practical Implications
It is important to systematically promote and improve the quality of teleconsultations, a modern form of contact between medical personnel and patients, to improve patient care and access to primary care physicians, and to enable the implementation of other modern telehealth solutions in primary care. The authors emphasise that when developing teleconsultation services, it is appropriate to focus on improving such aspects as the ability to get through to primary care outpatient clinics by telephone and the provision of full and comprehensive information about treatment and all the necessary documents to patients during teleconsultation appointments. What is also important is the possibility to book an in-person appointment whenever the teleconsultation appointment does not have the expected outcome.
Acknowledgments
The author declares no conflict of interest. The author received no specific funding for this work.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Guo Q, Wang Y, Xu D, et al. Rheumatoid arthritis: pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018;6:15. doi:10.1038/s41413-018-0016-9
2. Brekke M, Hjortdahl P, Thelle DS, Kvien TK. Disease activity and severity in patients with rheumatoid arthritis: relations to socioeconomic inequality. Soc Sci Med. 1999;48:1743–1750. doi:10.1016/S0277-9536(99)00075-1
3. Grimmer M, Riener R, Walsh CJ, Seyfarth A. Mobility related physical and functional losses due to aging and disease - a motivation for lower limb exoskeletons. J Neuroeng Rehabil. 2020;17(1):26. PMID: 30606194; PMCID: PMC6318939.
4. Klocek M. Kliniczne znaczenie danych w badaniach jakości życia [The clinical significance of data in studies on quality of life] [in:] Jakość życia w chorobach układu sercowo-naczyniowego. In: Kawecka-Jaszcz K, Klocek M, Tobiasz-Adamczyk B, editors. Metody pomiaru i znaczenie kliniczne [The Quality of Life of Patients with Cardiovascular Diseases. Measurement Methods and Clinical Significance]. Poznań: Termedia; 2006:85–96.
5. Megari K. Quality of life in chronic disease patients. Health Psychol Res. 2013;1(3):e27. doi:10.4081/hpr.2013.e27
6. Vliet Vlieland TP. Multidisciplinary team care and outcomes in rheumatoid arthritis. Curr Opin Rheumatol. 2004;16(2):153–156. doi:10.1097/00002281-200403000-00015
7. Landewé RB, Machado PM, Kroon F, et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann Rheum Dis. 2020;79(7):851–858. doi:10.1136/annrheumdis-2020-217877
8. Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology (Oxford). 2012;52:53–61. doi:10.1093/rheumatology/kes305
9. Mikuls TR, Johnson SR, Fraenkel L, et al. American college of rheumatology guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: version 3. Arthrit Rheumatol. 2021;73(2):e1–e12. doi:10.1002/art.41596
10. Pare G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base. JAMIA. 2007;14:269–277. doi:10.1197/jamia.M2270
11. Orrange S, Patel A, Mack WJ, Cassetta J. Patient satisfaction and trust in telemedicine during the COVID-19 pandemic: retrospective observational study. JMIR Hum Factors. 2021;8(2):e28589. doi:10.2196/28589
12. De Jong Gierveld J, Van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing. 2010;7(2):121–130. doi:10.1007/s10433-010-0144-6
13. Reynolds S, Doward LC, Spoorenberg A, et al. The development of the Ankylosing Spondylitis Quality of Life Questionnaire (ASQoL). Qual Life Res. 1999;8:651.
14. van Riel PL, Renskers L. The Disease Activity Score (DAS) and the Disease Activity Score using 28 joint counts (DAS28) in the management of rheumatoid arthritis. Clin Exp Rheumatol. 2016;34(5 Suppl 101):S40–S44.
15. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2021. Available from: https://www.R-project.org/.
16. ROZPORZĄDZENIE MINISTRA ZDROWIA z dnia 20 Marca 2020 r. w sprawie ogłoszenia na obszarze Rzeczypospolitej Polskiej stanu epidemii [Regulation of the Minister of Health of 20 March 2020 on announcing a state of epidemic in the Republic of Poland]. Available from: https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20200000491. Accessed July 16, 2021.
17. Okruszek Ł, Aniszewska-Stańczuk A, Piejka A, Wiśniewska M, Żurek K. Safe but lonely? Loneliness, mental health symptoms and COVID-19. Available from: https://psyarxiv.com/9njps/.
18. Fundacja Telemedyczna Grupa Robocza. Podstawowe zasady udzielania świadczeń telemedycznych [Foundation Telemedicine Working Group. Basic principles of telemedicine services.]. Available from: https://www.gov.pl/attachment/707c1949-9939-49d2-ab98-ec3fc1f2d297.
19. Lynn M, McMillen B, Sidani S. Understanding and measuring patients’ assessment of the quality of nursing care. Nurs Res. 2007;56(3):159–166. doi:10.1097/01.NNR.0000270025.52242.70
20. Rzecznik Praw Pacjenta [Eng. Patients’ Rights Ombudsman]. Problemy pacjentów w obliczu epidemii choroby COVID-19 [Problems faced by patients during the COVID-19 pandemic]. Available from: https://www.gov.pl/attachment/94b4e6ee-7cf0-4e47-932c-22a90b26d06a. Accessed July 16, 2021.
21. Narodowy Fundusz Zdrowia [Eng. The National Health Fund]. RAPORT Z BADANIA SATYSFAKCJI PACJENTÓW KORZYSTAJĄCYCH Z TELEPORAD U LEKARZA PODSTAWOWEJ OPIEKI ZDROWOTNEJ W OKRESIE EPIDEMII COVID-19 [Report on the survey of patient satisfaction with teleconsultation appointments with primary care physicians during the COVID-19 pandemic]. Available from: https://www.nfz.gov.pl/download/gfx/nfz/pl/defaultaktualnosci/370/7788/1/raport_-_teleporady_u_lekarza_poz.pdf. Accessed July 16, 2021.
22. Yellen E, Davis G, Ricard R. The measuring of patient satisfaction. J Nurs Care Qual. 2002;16(4):23–29. doi:10.1097/00001786-200207000-00005
23. Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32(10):1217–1220. doi:10.1017/S1041610220000988
24. Pietrabissa G, Simpson SG. Psychological consequences of social isolation during COVID-19 outbreak. Front Psychol. 2020;11:2201. doi:10.3389/fpsyg.2020.02201
25. Sheehy C, Murphy E, Barry M. Depression in rheumatoid arthritis—underscoring the problem. Rheumatology. 2006;45(11):1325. doi:10.1093/rheumatology/kel231
26. Katz PP, Yelin EH. Activity loss and the onset of depressive symptoms: do some activities matter more than others? Arthritis Rheum. 2001;44:1194–1202. doi:10.1002/1529-0131(200105)44:5<1194::AID-ANR203>3.0.CO;2-6
27. Mili F, Helmick CG, Zack MM, et al. Health reality quality of life adults reporting arthritis: analysis of data from the Behavioral Risk Factor Surveillance System, US, 1996–1999. J Rheumatol. 2003;30:160–166.
28. Lapsley HM, March LM, Tribe KL, et al. Living with rheumatoid arthritis: expenditures, health status, and social impact on patients. Ann Rheum Dis. 2002;61:818–821. doi:10.1136/ard.61.9.818
29. Shamlou R, Nikpeyma N, Pashaeipour S, Sahebi L, Mehrgou Z. Relationship of loneliness and social isolation with self-care ability among older adults. J Psychosoc Nurs Ment Health Serv. 2021;59(1):15–20. doi:10.3928/02793695-20201210-04
30. Öksüz E, Cinar FI, Cinar M, Tekgoz E, Yilmaz S. Assessment of the effects of loneliness, perceived social support, and depression on medication adherence in patients with ankylosing spondylitis. Perspect Psychiatr Care. 2021;57(2):517–523. doi:10.1111/ppc.12570
31. Akkaya F, Kiyak E. Evaluation of the loneliness, social support and quality of life in patients with rheumatoid arthritis. Int J Caring Sci. 2018;11(1):457.
32. Musich S, Wang SS, Hawkins K, Yeh CS. The impact of loneliness on quality of life and patient satisfaction among older, sicker adults. Gerontol Geriatr Med. 2015;1:2333721415582119. doi:10.1177/2333721415582119
33. Hackett RA, Hamer M, Endrighi R, et al. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37(11):1801–1809. doi:10.1016/j.psyneuen.2012.03.016
34. Creswell JD, Irwin MR, Burklund LJ, et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26(7):1095–1101. doi:10.1016/j.bbi.2012.07.006
35. Felsted KF. Mindfulness, stress, and aging. Clin Geriatr Med. 2020;36(4):685–696. doi:10.1016/j.cger.2020.06.010
36. Bai M, Tomenson B, Creed F, et al. The role of psychological distress and personality variables in the disablement process in rheumatoid arthritis. Scand J Rheumatol. 2009;38:419–430. doi:10.3109/03009740903015135
37. Kulikowski K. Psychologiczny i medyczny kontekst jakości życia osób z chorobami reumatycznymi [The psychological and medical contexts of quality of life in patients with rheumatic conditions]. Reumatologia [Rheumatology]. 2014;3(3):200–206. doi:10.5114/reum.2014.44091
38. Gorbatkow AA. On the dependence of emotional well-being on a level of performance: proposed model. Przeglad Psychologiczny [Eng Psychological Review]. 2002;45(4):431–451.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
