Back to Journals » Cancer Management and Research » Volume 10
The role of brigatinib in crizotinib-resistant non-small cell lung cancer
Authors Mezquita L, Planchard D
Received 28 October 2017
Accepted for publication 22 December 2017
Published 18 January 2018 Volume 2018:10 Pages 123—130
DOI https://doi.org/10.2147/CMAR.S129963
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Laura Mezquita, David Planchard
Medical Oncology Department, Gustave Roussy, Villejuif, France
Abstract: Despite the advances in new targeted therapies in ALK positive population, most patients progress under ALK inhibitors within first 2 years; being the brain the most frequent site of relapse. ALK mutations, in ~30% of patients, are the main known mechanism of resistance. Classically, second-generation ALK inhibitors have been the standard of care in the crizotinib-resistant population; however, each ALK inhibitor has a different spectrum of sensitivity to ALK mutations, complicating the optimal treatment strategy for the resistant population. Brigatinib (AP26113) is a novel highly selective and potent inhibitor of ALK and ROS1 with a high degree of selectivity. In vitro, brigatinib not only inhibited ALK with 12-fold higher potency compared to crizotinib, but also inhibited IGF-1R, FLT3 and EGFR mutants, with some activity against the EGFRT790M resistance mutation. In xenograft models, brigatinib overcomes resistance to ALK inhibitors, including the ALK G1202R mutation, which is resistant to first- and second-generation inhibitors. The efficacy of brigatinib in crizotinib-resistant, ALK-positive patients has been demonstrated in two early studies, which led to its approval in this setting, and it is currently being investigated as the first-line therapy versus crizotinib in tyrosine kinase inhibitor-naïve patients. Brigatinib demonstrates not only promising whole-body activity, but also an impressive improvement of intracranial outcomes in terms of both objective response rate and progression-free survival in the crizotinib-resistant population, with optimal efficacy at 180 mg (following a 90 mg run-in for 7 days) and good tolerance. These data confirm brigatinib as an excellent therapeutic strategy after crizotinib failure, particularly in the setting of central nervous system involvement. In this review, we summarize the two main clinical studies reported to date with brigatinib in ALK-positive advanced NSCLC patients, in particular, in the crizotinib-resistant population. We also address the mechanism of action for development of resistance and the challenging issues of optimal implementation for sequences of administration for ALK inhibitors.
Keywords: NSCLC, ALK, crizotinib resistant, brigatinib
Introduction
ALK rearrangements are present in ~5% of non-small cell lung cancer (NSCLC) patients, defining a specific molecular subgroup population.1 Over the last decade, the development of new and highly potent targeted therapies has enlarged the therapeutic strategy for advanced ALK-positive patients, achieving impressive improvements in survival.
Crizotinib was the first ALK inhibitor to be approved for the treatment of advanced NSCLC patients harboring an ALK rearrangement, first by the US Food and Drug Administration agency in August 2011 and subsequently by the European Medicines Agency in November 2012. In tyrosine kinase inhibitor (TKI)-naïve patients, crizotinib improves outcomes over platinum-based chemotherapy, the front-line standard of care until 2017, giving an objective response rate (ORR) of 74% and a median progression-free survival (PFS) of 10.9 months.2
In 2017, Peters et al reported the results of the Phase III ALEX trial in which alectinib, a second-generation ALK inhibitor, was compared to crizotinib in the front-line setting. This study demonstrated an ORR of 83% (versus 76% with crizotinib), including central nervous system (CNS) activity, and a remarkable survival benefit with a median PFS of 25.7 months (versus 10.4 with crizotinib), resulting in alectinib taking over as the new standard of care in the first-line setting in ALK-positive patients.3 Ceritinib is another second-generation ALK inhibitor approved for first-line treatment of ALK-positive patients, due to the results of the Phase III ASCEND-4 study, which demonstrated a survival improvement for ceritinib over platinum-based chemotherapy, with a median PFS of 16.6 versus 8.1 months.4
Despite these advances, most patients progress on ALK inhibitors within 2 years, with the brain being the most frequent site of relapse.5 ALK mutations, present in ~30% of patients treated with ALK inhibitors, are the main known mechanism of resistance.6 Classically, second-generation ALK inhibitors such as alectinib or ceritinib have been the standard of care in the crizotinib-resistant population;7,8 however, each ALK inhibitor has a different spectrum of sensitivity to ALK mutations, complicating the optimal treatment strategy for the resistant population.
The next-generation ALK inhibitors, such as brigatinib or lorlatinib, have a wider coverage of ALK resistance mutations, and sequential therapy with these ALK inhibitors is the preferred treatment approach in crizotinib-resistant and/or the second-generation–resistant populations, showing impressive responses and survival in pretreated crizotinib-resistant patients. Second- and third-generation ALK inhibitors have been evaluated versus crizotinib in the front-line setting to establish the optimal sequence of ALK inhibitors.
In this review, we summarize the two main clinical studies reported to date with brigatinib in ALK-positive advanced NSCLC patients and, in particular, in the crizotinib-resistant population. We also address the mechanism of action for development of resistance and the challenging issues of optimal implementation for sequences of administration for ALK inhibitors.
Mechanism of action
Brigatinib (AP26113; ARIAD Pharmaceuticals, Cambridge, MA, USA) is a 2,4-diarylaminopyrimidine, a novel highly-selective and potent inhibitor of ALK (IC50, 14 nmol/L) and ROS1 (IC50, 18 nmol/L), with a high degree of selectivity when compared to a panel of more than 250 kinases.9 In vitro, brigatinib inhibited ALK with a 12-fold higher potency compared to crizotinib, while it inhibited FLT3 and IGF-1R with an 11-fold lower potency than ALK (IC50, 148–158 nmol/L) and FLT3 and EGFR mutants with a 15-fold to 35-fold lower potency, respectively (IC50, 211–489 nmol/L), with some activity against the EGFRT790M resistance mutation (IC50, 489 nmol/L). In animal models, brigatinib has demonstrated overcoming resistance mechanism to ALK inhibitors, including the ALK G1202R mutation, which is resistant to first and second generation.10 Structurally, brigatinib has the unique feature of containing a phosphine oxide, a novel and little known hydrogen-bond acceptor that confers its highly selective potency and favorable pharmacokinetic and pharmacodynamic characteristics.
Clinical activity
Brigatinib was first assessed in a single-arm, open-label, Phase 1/2 trial designed to establish a recommended Phase II dose, characterize safety and perform a preliminary evaluation of efficacy. A total of 137 patients with advanced tumors were included in the USA and Spain, including 79 TKI-naïve and crizotinib-resistant ALK-positive NSCLC patients.11–13
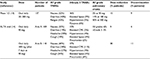
In the initial dose-escalation part, daily doses of oral brigatinib from 30 to 300 mg were evaluated. Two patients had dose-limiting toxicity, one grade 3 ALT elevation (at 240 mg) and the other one grade 4 dyspnea (at 300 mg), and the recommended Phase II dose was established as 180 mg daily. In the Phase II expansion part, three oral daily doses were assessed, 90, 180 and 180 mg, after a 7-day run-in at 90 mg. Five cohorts of patients were included – ALK inhibitor-naive NSCLC (cohort 1), crizotinib-resistant ALK-positive NSCLC (cohort 2), EGFRT790M-positive NSCLC resistant to one prior EGFR TKI (cohort 3), other non-NSCLC tumors with molecular alterations in brigatinib targets (cohort 4) and crizotinib-naive or crizotinib-resistant ALK-positive NSCLC with active, measurable CNS involvement (cohort 5). The Phase II primary endpoint was the assessment of ORR by Response Evaluation Criteria in Solid Tumors v1.1 (Table 1).
An efficacy analysis was performed in the 79 ALK-positive (58%) advanced NSCLC patients, 78 of whom were evaluable. The ORR was 62% (44/51) in crizotinib-resistant patients and 100% (8/8) in crizotinib-naïve patients. All four patients in cohort 1 had a response, giving a 100% ORR in this group (95% CI 40–100), and 31/42 (74% [95% CI 58–86]) in cohort 2, none (0/1) in cohort 3, 3/18 (17% [95% CI 4–41]) in cohort 4 and 5/6 (83% [95% CI 36–100]) in cohort 5 showed response (Table 2).
  | Table 2 Efficacy of brigatinib in the primary analysis in different populations of the expansion part of the Phase 1/2 trial in a crizotinib-resistant and crizotinib-naïve population Notes: +Measurable disease; *non-measurable disease. Data from Gettinger et al.13 Abbreviations: CNS, central nervous system; NA, not available; NR, not reached; ORR, objective response rate; OS, overall survival; PFS, progression-free survival. |
Median duration of response was 11.2 months (95% CI 7.6–29.7) in the 51 crizotinib-resistant patients and was not reached (NR) in the crizotinib-naive patients (95% CI 5.6 to NR). Median PFS (Phase II secondary outcome) was NR in the crizotinib-naïve cohort (95% CI 7·4 months to NR), 14.5 months (95% CI 9.2 to NR) in the crizotinib-resistant cohort and 1.8 months (95% CI 1.7–3.7) in the brigatinib-targeted alterations cohort; only one EGFRT790M-positive patient had an event (progression) at 7.4 months.
The second study evaluating brigatinib in crizotinib-resistant, ALK-positive NSCLC patients was the ALTA trial, a randomized, multicenter, Phase II trial assessing efficacy and safety.14 Two brigatinib regimens, initially assessed in the Phase II part of the initial Phase 1/2 trial, were evaluated. Patients were randomized (1:1) to receive oral brigatinib 90 mg once daily (arm A) or 180 mg once daily with a 7-day run-in at 90 mg (arm B), and were stratified by brain metastasis and prior response to crizotinib. The primary endpoint was investigator-assessed confirmed ORR. A total of 222 patients were enrolled (arm A: n=112, 109 treated; arm B: n=110, 110 treated), 154 (69%) of whom had baseline brain metastases. Results were reported after a median follow-up of 8 months, showing impressive outcomes, with an ORR of 45% (97.5% CI 34%–56%) and 54% (97.5% CI 43%–65%) in arms A and B, respectively, while median PFS was 9.2 months (95% CI 7.4–15.6) and 12.9 months (95% CI 11.1 to NR) in arms A and B, respectively, supporting better efficacy with the 180 mg dose.
Based on the findings from these two early studies, on April 28, 2017, the US Food and Drug Administration granted accelerated approval to brigatinib for the treatment of metastatic crizotinib-resistant, ALK-positive NSCLC patients. An update of the ALTA trial was presented at the 2017 International Association for the Study of Lung Cancer World Conference on Lung Cancer, supporting these results, notably for the 180 mg daily dose. With a median follow-up of 16.8 and 18.6 months in arms A and B respectively, the ORR was 46% (arm A) and 55% (arm B) by investigator assessment, with a median duration of response of 12 and 13.8 months, respectively. Median PFS was 9.2 months in arm A and 15.6 months in arm B. Median overall survival (OS) was NR in arm A and was 27.6 months in arm B.
Based on the promising results in crizotinib-naïve patients from the Phase 1/2 study, brigatinib is now being assessed in the front-line setting in the multicenter, randomized, Phase III ALTA 1L trial (NCT02737501). Approximately 270 advanced TKI-naïve, ALK-positive NSCLC patients with no more than one prior line of systemic treatment will be randomized (1:1) to receive brigatinib (1 week at 90 mg daily followed by 180 mg daily) or crizotinib (250 mg twice a day). Patients with asymptomatic or controlled brain and leptomeningeal metastasis are eligible. The primary endpoint is PFS as per Response Evaluation Criteria in Solid Tumors v1.1 assessed by a blinded independent review committee (BIRC); the secondary endpoints include ORR, duration of response, OS, safety/tolerability, patient-reported outcomes (PROs) and intracranial outcomes. Recruitment started in April 2016 and is ongoing.
In summary, the efficacy of brigatinib in crizotinib-resistant, ALK-positive patients has been demonstrated in two early studies leading to its approval in this setting, and it is currently being investigated as a first-line therapy versus crizotinib in TKI-naïve patients to establish the best sequence of ALK inhibitors in this population.
CNS activity
Brain is the primary site of failure with ALK inhibitors in ALK-positive patients, occurring in 20% of patients with no prior CNS involvement and in up to 70% of patients with CNS involvement at diagnosis.3,5,15 Consequently, CNS outcomes are a primary consideration in terms of the global efficacy of any ALK inhibitor.
In general, the second-generation ALK inhibitors show better diffusion across the brain–blood barrier, improving the CNS outcomes compared to crizotinib.3 It is hoped that the next-generation ALK inhibitors including brigatinib may further enhance this property.
CNS activity of brigatinib was evaluated in the Phase 1/2 trial in the 50 patients (63%) with CNS involvement. Forty-six (92%) of them had measurable CNS disease (with at least one follow-up scan), assessable for intracranial response, with a CNS ORR of 53%. Among the 31 patients with only non-measurable CNS disease, the CNS ORR was 35% (Table 1).
For all 19 evaluable patients with complete response (for all measurable and non-measurable disease), the median duration of CNS response was 18.9 months (95% CI 5.5 to NR); however, with only seven events at the cut-off, more mature data are needed to more accurately evaluate this activity. Median CNS PFS in the 46 evaluable patients was 15.6 months (95% CI 13.0 to NR). The CNS ORR in the crizotinib-naïve patients was 50% (3/6) and no events were reported in the CNS+ crizotinib-naïve cohort (Table 1).
Twenty-three patients (46%) with CNS involvement had not received previous brain radiotherapy, of whom 21 were assessable. Of them, 56% with measurable CNS disease (n=9) and 58% with non-measurable CNS disease (n=12) achieved a confirmed CNS ORR. Median CNS PFS was 22.3 months (95% CI 8.0–22.3).
Of the 25 patients who had been previously treated with brain radiotherapy, 20 patients had received this therapy more than 4 months earlier. The CNS ORRs were 53% (n=8/15) and 35% (n=11/31) in CNS measurable and non-measurable disease, respectively.
In the Phase II ALTA trial, 153 patients (69%) of the 222 enrolled had baseline brain metastases. A total of 44 (29%) patients were assessable for intracranial response (n=26 arm A, n=18 arm B), giving a CNS ORR of 42% in arm A and 67% in arm B. The median duration of CNS activity in patients with CNS response was NR (95% CI 3.7 to NR in arm A; 95% CI 5.6 to NR in arm B). The median CNS PFS was 15.8 months (95% CI 7.3–15.7) and 12.8 months (95% CI 11.0 to NR) in arms A and B, respectively.
In the 2017 update of the ALTA trial reported at the 2017 IASLC World Conference on Lung Cancer, the BIRC-assessed CNS ORRs were 50% and 67% in arms A and B, respectively. The median duration of CNS response was NR in arm A and 16.6 months in arm B. Considering all patients with CNS involvement at baseline, the median CNS PFS as assessed by the BIRC was 12.8 months in arm A and 18.4 months in arm B.
Thus, brigatinib demonstrates not only promising whole-body activity, but also an impressive improvement of intracranial outcomes in terms of both ORR and PFS in the crizotinib-resistant population, with optimal efficacy at 180 mg (following a 90 mg run-in for 7 days). These data confirm brigatinib as an excellent therapeutic strategy after crizotinib failure, particularly in the setting of CNS involvement.
Safety profile and tolerance
ALK-positive patients are typically exposed to ALK inhibitors not only for long periods, but also sequentially, making safety and tolerability critical endpoints for therapeutic management.
The safety of brigatinib was first assessed in the Phase 1/2 trial in patients with advanced tumors.11–13 In the dose escalation part, two dose-limiting toxicities were observed, grade 3 ALT elevation (at 240 mg) and grade 4 dyspnea (at 300 mg), and 180 mg was selected as the Phase II recommended dose. Safety was assessed in all 137 treated patients (from both parts of the study). The most frequent adverse events were nausea (52%), fatigue (42%) and diarrhea (40%). Treatment-related adverse events of grade 3 or more included elevated lipase (9%), pneumonia (7%), dyspnea (6%), and hypoxia (5%). Sixteen (12%) patients died during treatment or within 31 days of the last dose of brigatinib, which was due to progression in 8 of 16 cases (Table 3).
  | Table 3 Safety profile of brigatinib from the Phase 1/2 trial and the Phase II ALTA trial Abbreviations: CPK, creatine phosphokinase; G, grade; TRAEs, treatment-related adverse events. |
The authors reported a subset of pulmonary events occurred within 7 days of treatment initiation (or after re-initiation following a dose interruption) at the dose of 180 mg once daily, usually as an early event (within 24–48 hours), with a median time to onset of 2 days (interquartile range 2–2). These events included dyspnea, hypoxia, cough, pneumonia and pneumonitis, often with chest imaging findings of linear or ground-glass pulmonary opacities, without any apparent alternative cause. Incidence was dose dependent, increasing from 2% to 14% at 90 and 180 mg once daily and to 50% at 300 mg once daily. Two of 11 patients (18%) rechallenged with brigatinib had recurrence of pulmonary event. No definitive discontinuations due to this event occurred.
In the ALTA trial, the profile of common treatment-related adverse events was similar to that of the Phase 1/2 study, with nausea (arm A/B, 33%/40%), diarrhea (arm A/B, 19%/38%), headache (arm A/B, 28%/27%) and cough (arm A/B, 18%/34%), which were mainly grade 1 or 2. Early pulmonary events (within the first 48 hours) were also seen in 14 of the 219 patients (all grades, 6%, including ≥grade 3 in 3%), although in arm B, no cases were reported after the initial run-in dose was increased to 180 mg. Of these 14 patients, 7 (50%) were retreated, none of whom experienced repetition of the event.
In the ALTA trial update, the most common grade 3 or higher treatment-related adverse events in arms A and B included increased blood creatine phosphokinase (3% and 11%), hypertension (4% and 4%), increased lipase (4% and 4%), rash (1% and 4%) and pneumonitis (2% and 4%). Dose reduction due to adverse events was implemented in 9% and 30% of patients in arms A and B, respectively, and treatment discontinuation due to adverse events occurred in 4% and 11% in arms A and B, respectively.
The tolerability profile was also assessed from the patients’ perspective in the ALTA trial, according to PROs, as reported by Langer et al at the 2017 the American Society of Medical Oncology meeting.16 The European Organisation for Research and Treatment of Cancer Quality of life questionnaire-C30 (QLQ-C30) questionnaires were completed at baseline and on the first day of each cycle, and 208 (94%) of the 222 randomized patients were evaluated. No statistically significant differences were found in Global Health Status/Quality of Life score between arms, adjusted for baseline score, performance status (PS), and presence of liver/bone metastases. At Cycle 5, 80% of all patients reported an improvement or no change in Global Health Status/Quality of Life scores, with 50% reporting clinically meaningful improvement, and around 30% had clinically meaningful reduction in symptoms (i.e., 80% and 90% reported reduction or no change in pain and dyspnea, respectively). Less than 15% and 5% of patients reported clinically meaningful worsening of nausea/vomiting and diarrhea, respectively.
The relatively well-tolerated profile together with the above-described efficacy outcomes in the crizotinib-resistant population support a role for brigatinib as an optimal therapy in ALK-positive NSCLC patients.
Overcoming ALK resistance mechanisms
The development of resistance to ALK inhibitors remains a major challenge in the therapeutic decision-making process for ALK-rearranged NSCLC patients. Secondary ALK resistance mutations are the main known mechanism of resistance to ALK inhibitors, present in ~30% of advanced NSCLC patients.6 Most of these acquired ALK mutations generate conformational changes in the ALK protein, interfering with the binding of the inhibitors.
The development of ALK resistance mutations is more frequent in patients treated with second- or next-generation ALK inhibitors. Gainor et al reported a 20% rate of ALK mutations at progression under crizotinib (n=50) versus 53%–54% at progression under second-generation ALK inhibitors (n=41) and 71% under brigatinib (n=7).6 The ALKL1196M gatekeeper mutation is the most frequent mutation after progression following crizotinib exposure, and the ALK G1202R mutation is the most common mutation under second-generation inhibitors.
Additionally, the type of ALK inhibitor to which the patient has been exposed impacts the spectrum of ALK resistance mutations found, with broad analyses of mutational profiles in relation to ALK inhibitors showing that each inhibitor is associated with a distinct sensitivity profile to all ALK resistance mutations, with the optimal profile found with next-generation ALK inhibitors such as brigatinib. In vitro, brigatinib has demonstrated remarkable inhibition of cell growth in patient-derived cell lines harboring ALKC1156Y, ALKI1171N, ALKI1171S, ALKI1174C, ALKL1196M, ALKL1198F, ALKD1203N, and ALKE1210K mutations (IC50 <50 nM), whereas moderate inhibition (IC50 >50 nM <200 nM) was seen in cell lines harboring ALK G1202R and ALK G1202 deletions, or complex patterns of ALK mutations such as ALKD1203N+ALKF1174C and ALKD1203N+ALKE1210K.6 Although the identification of ALK resistance mutations is a strategic weapon when selecting subsequent lines of therapy, particularly interesting for the next-generation ALK inhibitors, the clinical impact of these findings remain unknown.
In addition, it is important to note that biopsy collection upon progression is not an option for all ALK-positive patients given that the first site of failure is commonly the CNS. Taking this into consideration, the development of new non-invasive alternative tools, such as the liquid biopsy in plasma, has been explored in this setting to assess resistance mutations. Bazhenova et al recently presented interesting data on the role of the liquid biopsy in detecting ALK fusions and mutations at baseline in plasma from patients in the Phase 1/2 ALTA trial.17 Out of 291 patients enrolled, 67 patients (23%) had baseline plasma samples or analysis (Resolution Bioscience ctDx Lung Panel v3.0). ALK fusions were detected in 45% (30/67), 33% of whom (10/30) had secondary ALK mutations. Complex patterns of mutations were observed, including between one and six ALK resistance mutations per patient, and secondary driver mutations such as BRAFV600E or KRASG12D were identified in combination with ALK resistance in one patient.
Gettinger et al also reported the efficacy of brigatinib according to the ALK resistance mutations detected in plasma at baseline or at progression under brigatinib from patients in the Phase 1/2 ALTA trial.12 Thirty of 301 patients (10%) had evaluable samples (FoundationOne next-generation sequencing platform). Nine patients (30%) presented ALK resistance mutations (three patients had ALKF1174L, and ALKL1196M, ALKS1206F, ALKG1269A, ALK G1202R, ALKL1196M and ALKF1245V were reported in one patient each). Taken together, these preliminary data support the feasibility of liquid biopsies for detecting ALK resistance mutations, which can be used when selecting subsequent anti-ALK therapy. However, large-scale studies are needed to optimize their application in the clinic.
In terms of ALK-independent mechanisms, a bypass mechanism via activation of EGFR-signaling pathways18 is reported in around 30% of cases of resistance; however, to date, anti-EGFR therapies have not been explored as a therapeutic strategy. Taking this into consideration, a double inhibitory approach using brigatinib as an anti-ALK and an anti-EGFR is an excellent candidate combination meriting assessment in a resistant population in which EGFR bypass signaling appears the predominant resistance mechanism. Brigatinib was recently proposed in combination with an anti-EGFR antibody as a means of overcoming resistance to osimertinib, a third-generation EGFR TKI, due to its structural characteristic of being able to fit into the ATP-binding pocket of the triple-mutant C797S/T790M/activating EGFR mutation.19 Further studies are warranted in both ALK-rearranged and EGFR mutant populations.
Future perspectives
The efficacy of brigatinib in crizotinib-resistant, ALK-positive patients has been established in two early development studies, and is currently being investigated in TKI-naïve patients in the Phase III ALTA 1L trial versus crizotinib to define the optimal sequence of ALK inhibitors in this population. The currently used sequence of therapy with a first-generation ALK inhibitor followed by second- or next-generation ALK inhibitor could be modified if brigatinib improves the benefit compared to crizotinib. A direct comparison of brigatinib versus a second-generation ALK inhibitor (alectinib or ceritinib) is not currently planned, although such a study would be valuable given that alectinib and ceritinib will become the standard of care in the front-line setting, with ALK resistance mutations found more frequently at progression compared to crizotinib. In this scenario, the next-generation ALK inhibitors such as brigatinib will have a predominant role, considering that they can address ALK resistance mutations.
However, today, the optimal sequence of ALK inhibitors remains to be defined with respect to second-generation ALK inhibitors and next-generation ALK inhibitors such as brigatinib that may replace the prior generation ALK inhibitors.
For now, the primary unanswered question is to define the optimal upfront inhibitor, with the secondary important issue to address being the best sequence of ALK inhibitors, maintaining the option of crizotinib in the front-line setting for certain patients. At ESMO 2017, Mok et al20 reported an update of OS from the Phase III PROFILE 1014 trial comparing crizotinib versus chemotherapy, with a median follow-up duration for OS of 46 months in both arms. Median OS was NR with front-line crizotinib (95% CI 45.8 to NR) versus 47.5 months (95% CI 32.2 to NR) with chemotherapy. Although these findings were not statistically significant, they showed impressive survival data for ALK-positive patients, with first-line crizotinib followed by second or third-generation ALK inhibitors, emphasizing the importance of the proper sequence of the available ALK inhibitors. The mature OS data of the ALEX and ASCEND 4 should help establish whether a second-generation ALK inhibitor upfront is a more successful approach.
Assessment of the molecular mechanisms of resistance could also have an impact in the decision-making process, on which the sequence of therapy with first- or second-generation followed by next-generation inhibitors according to ALK resistance mutations is also an appropriate strategy.
Conclusion
Brigatinib has shown efficacy including impressive intracranial activity and a good safety profile in a crizotinib-resistant, ALK-positive population. More data are needed to clearly establish the optimal place for brigatinib in sequential therapy, as first-line therapy according to the ALTA 1L trial or after second-generation ALK inhibitors. The selection of an ALK inhibitor by ALK resistance mutations could tip the balance in favor of brigatinib, considering its broad coverage of resistance mutations, which is of particular value in the context of post-second-generation ALK inhibitors.
Acknowledgment
The authors thank Sarah McKenzie, PhD for English language editing.
Disclosure
The authors report no conflicts of interest in this work.
References
Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009;27(26):4247–4253. | ||
Solomon BJ, Mok T, Kim DW, et al; PROFILE 1014 Investigators. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(23):2167–2177. | ||
Peters S, Camidge DR, Shaw AT et al; ALEX Trial Investigators. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–838. | ||
Soria JC, Tan DSW, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017;389(10072):917–929. | ||
Costa DB, Shaw AT, Ou SH, et al. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol. 2015;33(17):1881–1888. | ||
Gainor JF, Dardaei L, Yoda S, et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 2016;6(10):1118–1133. | ||
Shaw AT, Gandhi L, Gadgeel S, et al; study investigators. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol. 2016;17(2):234–242. | ||
Crinò L, Ahn MJ, De Marinis F, et al. Multicenter Phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non-small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2. J Clin Oncol. 2016;34(24):2866–2873. | ||
Huang WS, Liu S, Zou D, et al. Discovery of brigatinib (AP26113), a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. J Med Chem. 2016;59(10):4948–4964. | ||
Zhang S, Anjum R, Squillace R, et al. The potent ALK inhibitor brigatinib (AP26113) overcomes mechanisms of resistance to first- and second-generation ALK inhibitors in preclinical models. Clin Cancer Res. 2016;22(22):5527–5538. | ||
Camidge DR, Bazhenova L, Salgia R, et al. Safety and efficacy of brigatinib (AP26113) in advanced malignancies, including ALK+ non–small cell lung cancer (NSCLC). J Clin Oncol. 2015;33(suppl; abstr 8062). | ||
Rosell R, Gettinger SN, Bazhenova LA, et al. 1330: Brigatinib efficacy and safety in patients (Pts) with anaplastic lymphoma kinase (ALK)-positive (ALK+) non-small cell lung cancer (NSCLC) in a phase 1/2 trial. J Thorac Oncol. 2016;11(4 Suppl):S114. | ||
Gettinger SN, Bazhenova LA, Langer CJ, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 201617(12):1683–1696. | ||
Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non-small-cell lung cancer: a randomized, multicenter Phase II trial. J Clin Oncol. 2017;35(22):2490–2498. | ||
Solomon BJ, Cappuzzo F, Felip E, et al. Intracranial efficacy of crizotinib versus chemotherapy in patients with advanced ALK-positive non-small-cell lung cancer: results from PROFILE 1014. J Clin Oncol. 2016;34(24):2858–2865. | ||
Langer CJ, Huang H, Huang J, et al. Patient-reported outcomes and quality of life in ALTA: The randomized phase 2 study of brigatinib (BRG) in advanced ALK+ non–small cell lung cancer (NSCLC). [Internet]. [cited August 20, 2017]. Available from: http://meetinglibrary.asco.org/record/145768/abstract. Accessed August 20, 2017. | ||
Bazhenova L, Hodgson JG, Langer CJ, et al. Activity of brigatinib (BRG) in crizotinib (CRZ)-resistant ALK+ NSCLC patients (pts) according to ALK plasma mutation status. [Internet]. [cited August 13, 2017]. Available from: http://meetinglibrary.asco.org/record/145774/abstract. Accessed August 13, 2017. | ||
Camidge DR, Pao W, Sequist LV. Acquired resistance to TKIs in solid tumours: learning from lung cancer. Nat Rev Clin Oncol. 2014;11(8):473–481. | ||
Uchibori K, Inase N, Araki M, et al. Brigatinib combined with anti-EGFR antibody overcomes osimertinib resistance in EGFR-mutated non-small-cell lung cancer. Nat Commun. 2017;8:14768. | ||
Mok TS, Kim D, Wu Y, Nakagawa K, Mekhail T, Felip E, et al. Overall Survival (OS) for First-Line Crizotinib Versus Chemotherapy in ALK+ Lung Cancer: Updated Results from PROFILE 1014. Annals of Oncology (2017) 28 (suppl_5): v605-v649. 10.1093/annonc/mdx440. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

