Back to Journals » Patient Preference and Adherence » Volume 17
The Relationship Between Social Capital and Hypertension Among Type 2 Diabetes Mellitus Patients: The Moderating Effect of Depressive Symptoms
Authors Yan N , Chen D, Pan R, Zhang L, Ma J, Zhang Z, Dang Y, Wang L, Ma X, Jia S
Received 17 November 2022
Accepted for publication 7 January 2023
Published 21 January 2023 Volume 2023:17 Pages 209—216
DOI https://doi.org/10.2147/PPA.S396383
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ning Yan,1,* Dapeng Chen,1,* Ruiping Pan,2 Li Zhang,3 Juan Ma,4 Zhengjun Zhang,1 Yuqi Dang,5 Liqun Wang,6 Xueping Ma,1,7 Shaobin Jia1,7
1Heart Centre & Department of Cardiovascular Diseases, General Hospital of Ningxia Medical University, Yinchuan, 750004, People’s Republic of China; 2Department of Chinese Medicine, The Second People’s Hospital of Shizuishan, Shizuishan, 753000, People’s Republic of China; 3Department of Endocrinology, General Hospital of Ningxia Medical University, Yinchuan, 750004, People’s Republic of China; 4Clinical Medical College, Ningxia Medical University, Yinchuan, 750004, People’s Republic of China; 5Department of Endocrinology, Yinchuan Hospital of Traditional Chinese Medicine, Yinchuan, 750001, People’s Republic of China; 6Department of Epidemiology and Statistics, School of Public Health and Management, Ningxia Medical University, Yinchuan, 750004, People’s Republic of China; 7Ningxia Key Laboratory of Vascular Injury and Repair Research, Ningxia Medical University, Yinchuan, 750004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xueping Ma; Shaobin Jia, Heart Centre & Department of Cardiovascular Diseases, General Hospital of Ningxia Medical University, Yinchuan, 750004, People’s Republic of China, Tel +8613519290991 ; +8613995078969, Email [email protected]; [email protected]
Purpose: This study aimed to evaluate the relationship between social capital (SC) and hypertension among type 2 diabetes mellitus (T2DM) patients, considering the moderation effects of depressive symptoms.
Patients and Methods: A total of 1761 Chinese T2DM patients completed measure scales of social capital and epidemiological survey depression scale (CES-D). The Bootstrap methods PROCESS program is employed to test the moderation model.
Results: The prevalence of hypertension among T2DM patients was 39.3%. The SC was negatively correlated with the CES-D score (r=− 0.18, P< 0.01); the SC was also negatively correlated with diastolic blood pressure (r=− 0.05, P< 0.05); and the CES-D score was positively correlated with systolic blood pressure (r=0.05, P< 0.05). Both logistic regression analysis and the Bootstrap method showed that depressive symptoms weakened the protective effect of SC on hypertension, there existed a moderating effect of depressive symptoms on the relationship between SC and hypertension among T2DM patients.
Conclusion: Depressive symptoms may be one crucial moderator of the relationship between SC and hypertension in a representative sample of Chinese diabetes patients. The findings indicate that improving SC and mental health may help manage hypertension among T2DM patients.
Keywords: social capital, depressive symptoms, hypertension, moderation, type 2 diabetes mellitus
A Letter to the Editor has been published for this article.
Introduction
With the development of the economy and acceleration of urbanization, combined with population aging, type 2 Diabetes Mellitus (T2DM) is a significant public health concern worldwide.1 Meanwhile, two-thirds of patients with T2DM have hypertension, and the coexistence of those two risk factors leads to a four-fold increased risk for cardiovascular disease (CVD) compared with normotensive non-diabetic controls.2 Therefore, it is essential to identify the potential influencing factors or mechanisms of hypertension among T2DM patients, to manage this condition and reduce the burden of CVD.
In recent decades, social capital (SC) has been a research hotspot related to human health. SC, existing when healthy social networks between people, neighborhoods, and organizations offer benefits and resources such as coordination, reciprocity, and cooperation, has been associated with improved health and management of chronic disease.3,4 Several studies also described an inverse relationship between SC and hypertension.5–8 It has been suggested that SC may lower the risk of developing hypertension.3,9
More and more psychologists have recognized depression or depressive symptoms are closely associated with hypertension.10,11 Hypertension patients are prone to depression, and a meta-analysis reported that the prevalence of depression among hypertensive patients is 26.8%.12 In addition, mental health is influenced by individual-level factors such as socioeconomic status and social capital.13 Previous epidemiological studies suggested an inverse association between SC and depression among migrant hypertensive patients.14,15
To our knowledge, the potential mechanism of depressive symptoms on the association between SC and hypertension among T2DM patients has not been reported in the literature. The current study assumes depressive symptoms as a significant mental disease among hypertension patients, which may moderate the SC of individuals and further affect the blood pressure of patients. Hence, according to the above description and hypothesis, in this study, we examined the moderate effect of depressive symptoms on the relationship between SC and hypertension among T2DM patients.
Methods
Participants
The participants included N=1761 T2DM patients collected from August 2019 to November 2020 in Ningxia province, China. A probability proportionate to size (PPS) sampling method was developed to recruit the subjects. A similar sampling procedure was described previously.16 Eligibility criteria were aged ≥18 years old and living at the present address for at least six months. Excluded following: a) with severe mental disorders; b) a severe illness that prevents communication; c) deafness, aphasia, or other language barriers; d) pregnancy or lactation; e) diabetic ketoacidosis in the past month; f) with malignant tumor; and g) refuse to sign the informed consent. The Institutional Review Board of the Yinchuan Hospital of Traditional Chinese Medicine approved the study, and the study adhered to the 1964 Helsinki declaration and the later amendments or similar ethical standards. All the participants provided a written consent form at the beginning of the survey.
Measures
Hypertension
Hypertension was considered with systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or reported use of antihypertensive medication.17 BP was measured three times by nurses in subjects seated for at least 5 minutes using a mercury sphygmomanometer on the right arm (Baumanometer; Baum, Copiague, NY, USA). The mean value of three separate BPreadings was used for data analysis.
Social Capital
Based on the social capital scale, two dimensions of social capital developed by Mujahid18 were included in the current study: social cohesion and social interaction. A total of 9 commonly used and easily understandable items were applied to measure social capital and adapted to the Chinese context. In the present study, the five-point Likert social cohesion scale was adopted in the social capital questionnaire, and respondents were asked to rate their agreement ranged from 1 to 5 (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree). Cronbach’s alpha was 0.88 among the Chinese sample,19 and among this sample was 0.95. The social interaction scale consists of five items, and each item scored from 1 to 4 in response to a 4-point Likert scale (from never to often). The Cronbach’s alpha in this sample was 0.92. The measurement of social capital has also been described elsewhere.16
Depressive Symptoms
Depressive symptoms were assessed by using a 20-item Center for Epidemiological Studies Depression Scale (CES-D) Chinese edition, the Chinese version of the CES-D scale shows good reliability and validity.20 This scale consists of 16 negative affect and 4 positive affect items. The items reflect the following six aspects of depression: depressive mood, guilt and value lessness, helplessness and hopelessness, psychomotor retardation, loss of appetite, and sleep disorder. The total score ranged from 0 to 60, with higher scores indicating higher levels of depression. The Cronbach α in this study was 0.702.
Covariates
This study selected the following as potential confounders. Information on the demographic and health-related variables was collected. These variables included age, gender (male, female), marital status (unmarried, married, and widowed or divorced), educational attainment, residence (urban, rural), and family average individual income per month (<2000RMB, ≥2000 RMB). Information on smoking and drinking status, body mass index (BMI, kg/m2), physical activity (perform at least 30 minutes of physical activity at work and/or leisure time more than 4 days a week?”, with a yes/no response.), salt intake (moderate, salt, mild), sleep quality (The measure of self-reported sleep quality was dichotomized into poor, moderate, good), blood glucose level and dyslipidemia. According to 2016 Chinese guidelines for the management in adults,21 participants were defined as having dyslipidemia if they had one or more of the following conditions: TC ≥6.22 mmol/L, LDL-C ≥ 4.14 mmol/L, HDL-C ≤ 1.04 mmol/L, TG ≥2.26 mmol/L. Family history of T2DM (yes vs no), T2DM complications (yes vs no), drug uses (yes vs no).
Statistical Analysis
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 26.0 (SPSS Inc., Chicago, Illinois). Firstly, descriptive analyses were carried out on all variables, the quantitative variables were described as means and standard deviations. Categorical variables were described as counts and proportions. Student’s t-test or analysis of variance for quantitative variables and the chi-square test for categorical variables were used to examine group differences by hypertension. The associations between variables were evaluated by bivariate correlations. A logistic regression model was used to explore the association of SC with depressive symptoms and hypertension after controlling the covariates. The PROCESS program was used to test the moderate model. To pursue the testing for the moderating effect, the following relationships have to be significant: (1) effect of predictor (SC) on hypertension, (2) effect of moderator (depressive symptoms) on hypertension, and (3) interaction effect (SC × depressive symptoms) on hypertension. According to the Hayes statistical principle,22 model 1 was used to test the moderation effect. Bootstrap repeatedly sampled 5000 times for correction to obtain parameter estimation and a 95% confidence interval. The bootstrap confidence interval does not contain 0 indicating that the moderation effect is statistically significant.23 To interpret the moderating effects, simple slope analysis was then employed for significant interactions for the relationship between the independent variable (SC) and the dependent variable (hypertension) when the levels of the moderator variable (depressive symptoms) was one standard deviation above and below the mean.
Results
Characteristics of Participants
In Table 1, a descriptive analysis of hypertension and the related variables was shown. A total of 1761 (965 men and 796 women) were included in our study. The average age was 58.6 (standard deviation (SD) =12.2) years. Slightly one-fifth was illiterate, and about 93.2% were married. The mean score of SC was 27.7 (SD=6.5). The mean score of CES-D was 11.1 (SD=7.3). And the prevalence of hypertension among T2DM patients was 39.3%.
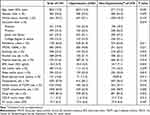 |
Table 1 Demographic Characteristics of Participant |
Correlations Analysis
The correlation matrix was showed in Table 2. the SC (r=−0.18, P<0.01) was negatively correlated with the CES-D score; the SC was also negatively correlated with DBP (r=−0.05, P<0.01); and the CES-D score was positively correlated with SBP (r=0.05, P<0.05).
 |
Table 2 Correlation Matrix (n=1761) |
Logistic Regression Analysis
The logistic regression model is presented in Table 3. After controlling for covariates (age, gender, marital status, education, economic condition, residency, smoking, alcohol use, physical exercise, BMI, salt intake, sleep quality, blood glucose level, dyslipidemia, family history of T2DM, T2DM complications and drug uses), the depressive symptoms were positively associated with hypertension (OR=1.11; 95% CI: 1.01–1.22; P<0.05). No significant association was found between SC and hypertension. There was, however, in model 3, the interaction between SC and depressive symptoms had statistical significance, indicating that there existed a moderating effect of depressive symptoms on the relationship between SC and hypertension among T2DM patients.
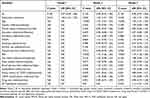 |
Table 3 Logistic Regression Model for Association Between SC, Depressive Symptoms and Hypertension (n=1761) |
Moderate Effect of Depression Symptoms on the Relationship of SC and Hypertension Among T2DM Patients
As shown in Table 4, the main effect of depressive symptoms on hypertension in T2DM patients was significant, while the negative main effect of SC on blood pressure was not significantly predicted, but the interaction effect between SC and depressive symptoms on predicting hypertension was significant, depressive symptoms weakened the protective effect of SC on hypertension. Further simple slope analysis showed that when depressive symptoms were at a low level (mean - 1 standard deviation), SC had a negative prediction of hypertension, while depressive symptoms were at medium and high levels, SC had no negative prediction of hypertension.
 |
Table 4 The Moderating Effect of Depressive Symptoms on the Relationship Between SC and Hypertension Among T2DM Patients* |
Discussion
To date, this was the first study to investigate the relationship between SC, depressive symptoms, and hypertension among type 2 diabetes patients in China. As hypothesized, we found: (1) hypertension was prevalent among T2DM patients in northwest China; (2) SC was negatively related to depressive symptoms and positively associated with hypertension; depressive symptoms were positively related to hypertension; (3) there existed a positive interaction effect of SC and depressive symptoms on hypertension, namely, in the relationship between SC and hypertension, depressive symptoms moderate the association.
In our study, we found that 39.3% of T2DM patients with hypertension is lower than the prevalence of hypertension among Sudan (47.6%)24 and Korean (54.6%) T2DM patients25 and also lower than Chinese T2DM patients reported by previous study (57.7%).26 The possible reasons may be due to different subjects, regions, and measurement instruments.27 Depression is the most frequent mental health and is considered a significant risk factor for the development of hypertension and T2DM.28,29 In view of this, more attention should be given to T2DM patients combined with hypertension concerning depression intervention. The relationship between depression and hypertension may be based on physiological mechanisms that involve the effects of the sympathetic nervous system, as it has been reported that norepinephrine is elevated in both patients with hypertension and depression.30
Correlation analysis showed a negative correlation between SC and hypertension among T2DM samples. The previous study reported that the prevalence of hypertension was high in patients with a lower social capital index.31 Social capital serves as a protective factor against chronic illness.32 It also reported South Asian women living in neighborhoods with high social cohesion had 46% reduced odds of having hypertension than those living in neighborhoods with low social cohesion.33 The possible mechanisms were the participants with higher SC were more likely to establish trustful and respectful relationships, engage with their partners and share experiences and practices, and further help to buffer the adverse health.34 Hence, patients with chronic diseases need more care, trust, and social support. Our results also showed that SC was negatively associated with CED-S score among hypertension and T2DM patients. Previous studies have also shown an inverse association between SC and depression among hypertensive patients.14
Further moderate effect results displayed SC has no direct effect on blood pressure of T2DM patients. Still, it can indirectly affect blood pressure through the moderate of depressive symptoms, which is especially shown when depressive symptoms were at a low level, SC had a negative prediction of hypertension, while depressive symptoms were at medium and high levels, SC had no negative prediction of hypertension. Depressive symptoms weakened the protective effect of SC on hypertension.
The present study has several limitations. First, because of the cross-sectional design, we cannot conclude that the relationship found between SC, depressive symptoms, and hypertension is causal. Second, the information regarding SC and depressive symptoms were self-reported by patients, which may have introduced recall bias. However, we carefully defined our survey questions, and the interviews were conducted by well-trained interviewers. Third, the study population was limited in hospitals in Ningxia, which limits the generalizability of the findings.
Conclusion
In conclusion, we found an inverse association between social capital and depressive symptoms, social capital and hypertension, and a positive association between depressive symptoms and hypertension. Furthermore, this study also provides new evidence indicating that depressive symptoms moderate the relationship between social capital and hypertension. Our finding suggests that strategies to address hypertension should be used to improve the management of hypertension. For example, social capital as a component of health systems reform or social interventions should be designed and implemented to improve mental health and further manage hypertension.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82204955), the Ningxia Natural Science Foundation (2022AAC05058).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2014;2(1):56–64. PMID: 24622669. doi:10.1016/s2213-8587(13)70112-8
2. Pavlou DI, Paschou SA, Anagnostis P, et al. Hypertension in patients with type 2 diabetes mellitus: targets and management. Maturitas. 2018;112:71–77. PMID: 29704920. doi:10.1016/j.maturitas.2018.03.013
3. Story WT. Social capital and health in the least developed countries: a critical review of the literature and implications for a future research agenda. Glob Public Health. 2013;8(9):983–999. PMID: 24172027. doi:10.1080/17441692.2013.842259
4. Hu F, Hu B, Chen R, et al. A systematic review of social capital and chronic non-communicable diseases. Biosci Trends. 2014;8(6):290–296. PMID: 25639224. doi:10.5582/bst.2014.01138
5. Malino C, Kershaw T, Angley M, Frederic R, Small M. Social capital and hypertension in rural Haitian women. Matern Child Health J. 2014;18(10):2253–2260. PMID: 24057989. doi:10.1007/s10995-013-1351-5
6. Kamimura A, Tabler J, Nourian MM, Assasnik N, Wright L, Ashby J. Prevention and management of hypertension and diabetes using social capital and physical activity among socioeconomically disadvantaged populations. Fam Community Health. 2017;40(3):205–211. PMID: 28525440. doi:10.1097/fch.0000000000000156
7. Nakagomi A, Tsuji T, Hanazato M, Kobayashi Y, Kondo K. Association between community-level social participation and self-reported hypertension in older Japanese: a JAGES multilevel cross-sectional study. Am J Hypertens. 2019;32(5):503–514. PMID: 30793745. doi:10.1093/ajh/hpz028
8. Renta V, Walker RJ, Nagavally S, Dawson AZ, Campbell JA, Egede LE. Differences in the relationship between social capital and hypertension in emerging vs. established economies in Sub-Saharan Africa. BMC Public Health. 2022. 22(1):1038. PMID: 35610591. doi:10.1186/s12889-022-13471-8
9. Palafox B, Goryakin Y, Stuckler D, et al. Does greater individual social capital improve the management of hypertension? Cross-national analysis of 61 229 individuals in 21 countries. BMJ Glob Health. 2017;2(4):e000443. PMID: 29333284. doi:10.1136/bmjgh-2017-000443
10. Rantanen AT, Korkeila JJA, Löyttyniemi ES, Ukm S, Korhonen PE. Awareness of hypertension and depressive symptoms: a cross-sectional study in a primary care population. Scand J Prim Health Care. 2018;36(3):323–328. PMID: 30139283. doi:10.1080/02813432.2018.1499588
11. Takita Y, Takeda Y, Fujisawa D, Kataoka M, Kawakami T, Doorenbos AZ. Depression, anxiety and psychological distress in patients with pulmonary hypertension: a mixed-methods study. BMJ Open Respir Res. 2021;8(1):e000876. PMID: 33926959. doi:10.1136/bmjresp-2021-000876
12. Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of depression in patients with hypertension: a systematic review and meta-analysis. Medicine. 2015;94(31):e1317. PMID: 26252317. doi:10.1097/md.0000000000001317
13. De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–627. PMID: 16020636. doi:10.1136/jech.2004.029678
14. Zhu W, Li H, Wang X, Mao C. Social capital and depression among migrant hypertensive patients in primary care. J Am Soc Hypertens. 2018;12(8):621–626. PMID: 29941387. doi:10.1016/j.jash.2018.06.006
15. Li H, Xia H, Yi S, Rao L. Social capital, depressive symptoms, and perceived quality of care among hypertensive patients in primary care. Health Qual Life Outcomes. 2020;18(1):378. PMID: 33261641. doi:10.1186/s12955-020-01630-7
16. Wang L, Li J, Dang Y, Ma H, Niu Y. Relationship between social capital and depressive symptoms among type 2 diabetes mellitus patients in northwest china: a mediating role of sleep quality. Front Psychiatry. 2021;12:725197. PMID: 34616319. doi:10.3389/fpsyt.2021.725197
17. Liu LS, Wu ZS, Wang JG, et al. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. 2019;16(3):182–241. PMID: 31080465. doi:10.11909/j.issn.1671-5411.2019.03.014
18. Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165(8):858–867. PMID: 17329713. doi:10.1093/aje/kwm040
19. Gao J, Fu H, Li J, Jia Y. Association between social and built environments and leisure-time physical activity among Chinese older adults--a multilevel analysis. BMC Public Health. 2015;15:1317. PMID: 26715531. doi:10.1186/s12889-015-2684-3
20. Zhang B, Fokkema M, Cuijpers P, Li J, Smits N, Beekman A. Measurement invariance of the Center for Epidemiological Studies Depression Scale (CES-D) among Chinese and Dutch elderly. BMC Med Res Methodol. 2011;11:74. doi:10.1186/1471-2288-11-74
21. Jun-Ren ZH, Run-Lin GA, Shui-Ping ZH, Guo-Ping LU, Dong ZH, Jian-Jun LI. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15(1):1–29. PMID: 29434622. doi:10.11909/j.issn.1671-5411.2018.01.011
22. Jonas E, Fischer P. Terror management and religion: evidence that intrinsic religiousness mitigates worldview defense following mortality salience. J Pers Soc Psychol. 2006;91(3):553–567. PMID: 16938037. doi:10.1037/0022-3514.91.3.553
23. Zhou X, Lei Q, Marley SC, Chen J. Existential function of babies: babies as a buffer of death‐related anxiety. Asian J Socil Psychol. 2009;12(1):40–46. doi:10.1111/j.1467-839X.2008.01268.x
24. Abdelbagi O, Musa IR, Musa SM, ALtigani SA, Adam I. Prevalence and associated factors of hypertension among adults with diabetes mellitus in northern Sudan: a cross-sectional study. BMC Cardiovasc Disord. 2021;21(1):168. doi:10.1186/s12872-021-01983-x
25. Ko SH, Kwon HS, Kim DJ, et al. Taskforce team of diabetes fact sheet of the Korean Diabetes Association. Higher prevalence and awareness, but lower control rate of hypertension in patients with diabetes than general population: the fifth Korean national health and nutrition examination survey in 2011. Diabetes Metab J. 2014;38(1):51–57. doi:10.4093/dmj.2014.38.1
26. Gan S, Yongsheng L, Fangxu S, Ning D. The risk factors of type 2 diabetes with hypertension and the construction of its nomogram prediction model. Chongqing Med J. 2022;51(13):2189–2193+2198.Chinese.
27. Li J, Qiu X, Yang X, et al. Relationship between Illness perception and depressive symptoms among type 2 diabetes mellitus patients in China: a mediating role of coping style. J Diabetes Res. 2020;2020:3142495. PMID: 33123596. doi:10.1155/2020/3142495
28. Patten SB, Williams JV, Lavorato DH, Campbell NR, Eliasziw M, Campbell TS. Major depression as a risk factor for high blood pressure: epidemiologic evidence from a national longitudinal study. Psychosom Med. 2009;71(3):273–279. PMID: 19196807. doi:10.1097/PSY.0b013e3181988e5f
29. Rotella F, Mannucci E. Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry. 2013;74(1):31–37. PMID: 23419223. doi:10.4088/JCP.12r07922
30. Scalco AZ, Scalco MZ, Azul JB, Lotufo Neto F. Hypertension and depression. Clinics. 2005;60(3):241–250. PMID: 15962086. doi:10.1590/s1807-59322005000300010
31. Gupta R, Kaur M, Islam S, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. 2017;30(4):373–381. PMID: 28096145. doi:10.1093/ajh/hpw169
32. Ahern MM, Hendryx MS. Social capital and risk for chronic illnesses. Chronic Illn. 2005;1(3):183–190. PMID: 17152181. doi:10.1177/17423953050010030201
33. Lagisetty PA, Wen M, Choi H, Heisler M, Kanaya AM, Kandula NR. Neighborhood social cohesion and prevalence of hypertension and diabetes in a South Asian population. J Immigr Minor Health. 2016;18(6):1309–1316. PMID: 26527589; PMCID: PMCPMC4853276. doi:10.1007/s10903-015-0308-8
34. Szreter S, Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. Int J Epidemiol. 2004;33(4):650–667. PMID: 15282219. doi:10.1093/ije/dyh013
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
