Back to Journals » International Journal of General Medicine » Volume 15
The Relationship Between Serum Folate Level and Residual Renal Function in CAPD Patients
Authors Yu J , Zhou Q, Xu Y , Wang T, Du J, Zhao L, Li J, Wang H, Xu Q, Lai X , Guo Z
Received 27 June 2022
Accepted for publication 23 August 2022
Published 2 September 2022 Volume 2022:15 Pages 6977—6984
DOI https://doi.org/10.2147/IJGM.S379594
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jianpeng Yu,1,* Qi Zhou,1,* Ying Xu,1,* Tieyun Wang,1 Jun Du,1 Lifang Zhao,1 Juan Li,1 Haiyan Wang,1 Qianqian Xu,2 Xueli Lai,1 Zhiyong Guo1
1Department of Nephrology, Shanghai Changhai Hospital, Shanghai, People’s Republic of China; 2Department of Rheumatology and Immunology, Shanghai Changhai Hospital, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xueli Lai; Zhiyong Guo, Email [email protected]; [email protected]
Objective: To investigate the relationship between serum folate (FA) levels and residual renal function (RRF) in continuous ambulatory peritoneal dialysis (CAPD) patients.
Methods: Clinical data were collected from 180 hospitalized patients who received CAPD regularly. Patients were divided into the FA deficiency group and the FA non-deficiency group according to serum FA level. Data on age, sex, PD vintage, hemoglobin, mean corpuscular volume, serum FA, total Kt/V, residual kidney Kt/V, peritoneum Kt/V, creatinine clearance (Ccr), ultrafiltration volume, cystatin C (cytC), serum creatinine (Scr), urea nitrogen, retinol-binding protein and the primary disease were gathered from 2 groups. Statistical methods were used to analyze the relationship between serum FA level and RRF.
Results: Peritoneal Kt/V, cytC, Scr were higher, and residual kidney Kt/V was lower in FA deficiency group than in non-deficiency group. Univariate correlation showed the peritoneal Kt/V, cytC, Scr negatively correlated with serum FA while residual kidney Kt/V positively correlated with serum FA, and there was a simple linear regression relationship between serum FA and residual kidney Kt/V. Differences were statistically significant (P< 0.05).
Conclusion: There is a relationship between serum FA and RRF in CAPD patients. Prospective studies or trials should be performed to clarify the importance of FA supplementation on RRF during peritoneal dialysis.
Keywords: folate, continuous ambulatory peritoneal dialysis, residual renal function
Introduction
Peritoneal dialysis (PD) is an important renal replacement therapy for patients with end-stage renal disease, however, concurrent cardiovascular disease (CVD) or PD-related peritonitis can not only affect the smoothness of the PD process but also be life-threatening in serious cases. Residual renal function (RRF) plays an important role in the quality of life and prognosis of PD patients. Studies have shown that a 5 L/1.73-m2 per-week increase in GFR and a 10 L/1.73-m2 per-week increase in Ccr reduce the mortality risk by 12% and 40%, respectively, in PD patients.1,2 Simultaneously, preservation of even a small amount of RRF also has significant positive effects during PD treatment.3 Furthermore, a decline in RRF can lead to malnutrition, infection, CVD and other serious adverse events during dialysis.4 Therefore, protecting RRF in PD patients as much as possible is important to prolonging the dialysis age and improving quality of life.
Folate (FA), also known as vitamin B9, is a water-soluble vitamin that plays important roles in the metabolism of genetic material and proteins, growth, development, and immunity enhancements that maintain normal life activities. FA deficiency can lead to anaemia, infertility and muscle weakness5–7 and is closely associated with hyperhomocysteinaemia,8 which correspondingly increases the risk of CVD.9 Previous research reported that approximately 40–60% of deaths among PD patients are related to CVD,10 while long-term FA supplementation significantly reduces all-cause mortality and cardiovascular mortality in continuous ambulatory peritoneal dialysis (CAPD) patients.11 FA cannot be synthesized by the human body, so its physiological level is entirely dependent on exogenous FA intake.12 The upper small intestine is the main FA absorption site; patients who have renal function damage up to uraemia often have concomitant gastrointestinal symptoms such as nausea, vomiting and loss of appetite, which decreases FA intake to a certain extent. Decreased of serum FA levels in PD patients have also been reported in the literature,13 FA supplementation has been shown to reduce Scr and increase GFR in subjects with atherosclerosis hazards.14 Therefore, we speculated that appropriate FA supplementation may play roles in maintaining RRF in PD patients. Although the relationship between serum FA and PD or serum FA and renal function has been reported in some studies, there are no direct analyses exploring the relationship between serum FA and RRF in PD patients. Therefore, we analysed the relationship between serum FA and RRF in CAPD patients, and preliminarily discuss the mechanism in this context.
Methods
Study Participants
Our study used a cross-sectional design. We collected the clinical data of 213 hospitalized patients who received CAPD regularly at Department of Nephrology, Shanghai Changhai Hospital between March 1, 2019, and March 19, 2021. The exclusion criteria were as follows:1 patients aged <18 years;2 patients who had acute kidney injury and received emergency haemodialysis;3 patients with concomitant malignant tumours; or4 patients who had received FA supplement treatments. Among those excluded, there were 16 patients who had received emergency haemodialysis and 17 patients who had received FA supplementation. Finally, 180 patients were enrolled in the study. The serum FA level was determined by radioimmunoassay, and a level <4 ng/mL was defined as FA deficiency.15 Then, patients were divided into 2 groups according to FA levels. There were 83 cases in the FA deficiency group and 97 cases in the non-deficiency group. Figure 1 shows the distribution of serum FA levels in this study.
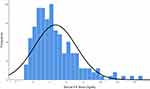 |
Figure 1 Frequency distribution histogram of serum FA levels. |
Data Collection
The information collected consisted of enumeration and measurement data. Enumeration data were collected for the sex and primary disease of the PD patients, which was categorized as male, female, diabetic nephropathy (DN) and non-diabetic nephropathy (NDN). Measurement data were collected for the age, PD vintage, hemoglobin (Hb), mean corpuscular volume (MCV), serum FA, total Kt/V, residual kidney Kt/V, peritoneum Kt/V, creatinine clearance (Ccr), ultrafiltration volume, cystatin C (cytC), serum creatinine (Scr), urea nitrogen (BUN) and retinol-binding protein (RBP).
Statistical Analyses
Statistical analysis was performed using SPSS, IBM (version 26) software. Measurement data with a normal distribution are shown as means ± standard deviations, and differences between 2 groups were evaluated by independent-sample t-tests. Measurement data without a normal distribution are expressed as the median (interquartile range) and were analysed by means of the Mann–Whitney U-test. Enumeration data are expressed as frequencies (percentages) and were analysed by means of the chi-square test. Spearman correlation analysis was used to determine the correlation between serum FA and all measurement data. Simple linear regression analysis was performed with residual kidney Kt/V and Ccr as the dependent variable and serum FA level as the independent variable. Adjustments were made for the influence of sex, age, brain natriuretic peptide (BNP), and Lipoprotein a (LP(a)) on serum FA in the model. P < 0.05 indicates significant differences. Figure 2 shows the flow chart of this research process.
 |
Figure 2 Flowchart of the study. |
Results
Comparison of Observation Indices Between 2 Groups
Table 1 shows the comparison of all observation indices between the 2 groups. The peritoneal Kt/V, cytC, and Scr in the FA deficiency group were higher than those in the non-deficiency group, and the residual kidney Kt/V was lower in the FA deficiency group than in non-deficiency group; the differences were statistically significant (P<0.05). There were no statistically significant differences in the age, sex, PD vintage, Hb, MCV, primary disease, total Kt/V, Ccr, ultrafiltration volume, BUN or RBP between the 2 groups (P≥0.05).
 |
Table 1 Comparison of Observation Indices Between the 2 Groups |
Univariate Correlations Between Serum FA Level and Other Factors
Table 2 shows the univariate correlation between serum FA and all measurement data. Peritoneal Kt/V, cytC, and Scr were negatively correlated with serum FA (peritoneal Kt/V: ρ=−0.181; P=0.014, cytC: ρ=−0.326; P=0.000, Scr: ρ=−0.287; P=0.000), while residual kidney Kt/V positively correlated with serum FA (ρ=0.251; P=0.001).
 |
Table 2 Univariate Correlations Between Serum FA Level and Other Factors |
Linear Regression Analysis Between Residual Kidney Kt/V, Ccr and Serum FA
Simple linear regression analysis was performed with serum FA as an independent variable and Kt/V and Ccr as dependent variables. Model 1 was adjusted for age and sex, and Model 2 comprised Model 1 in addition to adjustments for plus LP(a) and BNP levels. There was a linear relationship between serum FA levels and residual kidney Kt/V in both models after the adjustments (Model 1: P=0.035; Model 2: P=0.036), and no linear regression was performed between serum FA and Ccr levels in either model (Model 1: P=0.081; Model 2: P = 0.100) (Table 3).
 |
Table 3 Linear Regression Analysis Results |
Discussion
RRF is the endocrine and clearance function of the remnant nephrons after renal function damage. For PD patients, maintaining good RRF contributes to the improvement of nutritional level, water and electrolyte balance, assurance of dialysis adequacy and loss of morbidity and mortality of dialysis-related complications.16 FA is absorbed into the body through glomerular filtration and reabsorption of the proximal tubule, while FA transporters located in the proximal tubule contribute to FA reabsorption and maintain homeostasis. Studies have found a decrease in the expression of FA transporters and the serum FA level in an acute kidney injury rat model,17 which provides us with an important reference to explore the relationship between RRF and serum FA levels in patients undergoing PD due to chronic renal failure. In this study, we assessed Scr, BUN, cytC, Kt/V and other indicators to reflect RRF in CAPD patients directly or indirectly and then analysed their relationships with serum FA to provide a reasonable interpretation.
Kt/V is an important index used to evaluate PD adequacy, which reflects the ability to eliminate small molecule toxins during dialysis. It includes the Kt/V of the residual kidney and peritoneum function, which represents the urea removal capacity provided by the residual kidney and peritoneum function, respectively. The increase in residual kidney Kt/V improves the anaemia of CAPD patients, according to a study by Karel al.18 In addition, residual kidney Kt/V has the ability to improve the viability and serum albumin and nutritional level of CAPD patients.19,20 In our study, the relationship between the residual kidney Kt/V level and serum FA deficiency was significant, and we found an obviously positive correlation between the two parameters. On the one hand, deficiency of folate results in megaloblastic anemia, and there have been many reports on the use of folate supplements for anemia treatment. On the other hand, we also observed a decrease in the urea level after FA supplementation in DN mice,21 while linear regression analysis showed that the residual kidney Kt/V changed with the change in serum FA. This allowed us to consider that the elevated residual kidney Kt/V improves anemia in CAPD patients,18 during which serum FA likely plays an important role. Serum FA can improve the Kt/V level, which is reflected as an indicator of urea removal capacity. However, peritoneal Kt/V was significantly increased in the FA-deficient group and was negatively correlated with serum FA, which was related to the fact that the total Kt/V of PD inpatients in our center were stable caused by the nicely quality control of PD consistently. The increase in residual kidney Kt/V will inevitably lead to a corresponding decrease in peritoneal Kt/V when the total Kt/V value is stable, which consequently reaches the opposite conclusion of residual kidney Kt/V. Similarly, this conjecture has been made in previous studies, namely, that the peritoneal Kt/V has the function of keeping the total Kt/V level stable when the residual kidney Kt/V decreases.19,22
CytC is a non-glycosylated, low-molecular-weight basic protein (13 kDa) that is used as a marker for the glomerular filtration rate, and it has significant effects in the evaluation of RRF and predicting clinical outcomes in PD patients;23,24 moreover, it is characterized by a significant negative correlation with residual kidney Kt/V.25 In the present study, we found that the relationship between the cytC level and serum FA deficiency was significant, and both showed an obvious negative correlation. It is further speculated that some kind of correlation between them may exist.
Scr, always used as the indicator of renal function, has also been mentioned to be related to serum FA in a previous study. In addition to the study by Mierzecki et al that FA supplementation reduced Scr in subjects with atherosclerotic hazards,14 serum FA also decreased in AKI rats with the rise of Scr and showed a significantly negative correlation in another study by Yang et al.17 Moreover, M Achón et al found a reduction in Scr in rats fed high-dose FA after 4 weeks.26 Our statistical results were similar to those of previous studies, except that the subjects were CAPD patients, which was the main difference in our research.
Ccr, together with Kt/V, constitutes an index for small solute clearance during PD and plays an important role in improving dialysis adequacy. Clinically, a weekly total Kt/V > 1.7 and Ccr > 60 are considered adequate dialysis. Consequently, broadly similar trends for Kt/V and Ccr should be observed, but our study showed completely different results. There were no significant differences in Ccr levels between the FA deficiency group and the nondeficiency group. Univariate correlation analysis and simple linear regression analysis also revealed no relationship between Ccr and FA level, and we surmise that this finding is probably attributed to renal physiology. A previous retrospective study found that the results of Kt/V and Ccr dialysis were contradictory in nearly 23% of PD patients, and further analysis suggested that the reason may have been related to the role of renal filtration and reabsorption.27 The creatinine produced during human metabolism is excreted mainly through glomerular filtration and renal tubular secretion, while urea can be partially reabsorbed by renal tubules after glomerular filtration, which causes a discrepancy in the statistical analysis results between assessments of Kt/V and Ccr.
To the best of our knowledge, this is the first investigation to directly analyse the correlation between serum FA and RRF in CAPD patients. Although this is only a cross-sectional study that cannot investigate the causal relationship, it certainly indicates the significance of the serum FA level in CAPD patients. A series of prospective studies will be carried out on this basis to further explore the influence of FA supplementation on the quality of life of PD patients.
In conclusion, there is a relationship between serum FA and RRF in CAPD patients. Prospective studies or trials should be performed to clarify the importance of FA supplementation on RRF during peritoneal dialysis.
Confidentiality Statement
Patients’ clinical data were stored in our professional medical database, the process of data collection was supervised of the experts for the full time, which ensured the clinical data cannot be compromised. All attempts to access these data for private purposes are not allowed. The datasets generated and analyzed during this study are not publicly available because of professional discretion, as they were part of patients’ records, but are available as a de-identified data sheet from the corresponding author on reasonable request.
Abbreviations
PD, peritoneal dialysis; FA, folate; CAPD, continuous ambulatory peritoneal dialysis; RRF, residual renal function; Hb, hemoglobin; MCV, mean corpuscular volume; Ccr, creatinine clearance; cytC; cystatin C; Scr, serum creatinine; CVD, cardiovascular disease; DN, diabetic nephropathy; NDN, non-diabetic nephropathy; BUN, urea nitrogen; RBP, retinol-binding protein; BNP, brain natriuretic peptide; LP(a), lipoprotein a.
Data Sharing Statement
The datasets analysed during the current study available from the corresponding author on reasonable request.
Ethics Statement
The study was conducted in accordance with the principles of the Declaration of Helsinki, and the study protocol was approved by the ethics committee of The First Affiliated Hospital of Naval Medical University. Because of the retrospective nature of the study, patient consent for inclusion was waived.
Acknowledgments
The authors thank all staffs in Department of Nephrology, Shanghai Changhai Hospital (Shanghai, China) for their technical support.
Funding
This work was supported by National Natural Science Foundation of China (No.81800678, No.81770763), The Science and Technology Commission of Shanghai Municipality (21ZR1478700), Discipline Construction Climbing 234 Plan of Changhai Hospital of Naval Medical University (No.2020YXK041).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bargman JM, Thorpe KE, Churchill DN. Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol. 2001;12(10):2158–2162. doi:10.1681/ASN.V12102158
2. Rocco M, Soucie JM, Pastan S, McClellan WM. Peritoneal dialysis adequacy and risk of death. Kidney Int. 2000;58(1):446–457. doi:10.1046/j.1523-1755.2000.00184.x
3. Carvalho MJ, Rodrigues A. Importance of residual renal function and peritoneal dialysis in anuric patients. Contrib Nephrol. 2009;163:155–160.
4. Wang AY, Lai KN. The importance of residual renal function in dialysis patients. Kidney Int. 2006;69(10):1726–1732. doi:10.1038/sj.ki.5000382
5. Nejatinamini S, Debenham BJ, Clugston RD, et al. Poor vitamin status is associated with skeletal muscle loss and mucositis in head and neck cancer patients. Nutrients. 2018;10(9):1236. doi:10.3390/nu10091236
6. Yadav MK, Manoli NM, Madhunapantula SV. Comparative assessment of vitamin-B12, folic acid and homocysteine levels in relation to p53 expression in megaloblastic anemia. PLoS One. 2016;11(10):e0164559. doi:10.1371/journal.pone.0164559
7. Hwang SY, Kang YJ, Sung B, et al. Folic acid is necessary for proliferation and differentiation of C2C12 myoblasts. J Cell Physiol. 2018;233(2):736–747. doi:10.1002/jcp.25989
8. Levy J, Rodriguez-Guéant RM, Oussalah A, et al. Cardiovascular manifestations of intermediate and major hyperhomocysteinemia due to vitamin B12 and folate deficiency and/or inherited disorders of one-carbon metabolism: a 3.5-year retrospective cross-sectional study of consecutive patients. Am J Clin Nutr. 2021;113(5):1157–1167. doi:10.1093/ajcn/nqaa432
9. Moat SJ, Lang D, McDowell IF, et al. Folate, homocysteine, endothelial function and cardiovascular disease. J Nutr Biochem. 2004;15(2):64–79. doi:10.1016/j.jnutbio.2003.08.010
10. Johnson DW, Dent H, Hawley CM, et al. Association of dialysis modality and cardiovascular mortality in incident dialysis patients. Clin J Am Soc Nephrol. 2009;4(10):1620–1628. doi:10.2215/CJN.01750309
11. Rong R, Zhou Q, Lin J, et al. Maintained folic acid supplementation reduces the risk of mortality in continuous ambulatory peritoneal dialysis patients. Blood Purif. 2018;45(1–3):28–35. doi:10.1159/000480222
12. Hou H, Zhao H. Epigenetic factors in atherosclerosis: DNA methylation, folic acid metabolism, and intestinal microbiota. Clinica Chimica Acta. 2021;512:7–11. doi:10.1016/j.cca.2020.11.013
13. Sevitt LH, Hoffbrand AV. Serum folate and vitamin B12 levels in acute and chronic renal disease. Effect of peritoneal dialysis. Br Med J. 1969;2(5648):18–21. doi:10.1136/bmj.2.5648.18
14. Mierzecki A, Makarewicz-Wujec M, Kłoda K, Kozłowska-Wojciechowska M, Pieńkowski P, Naruszewicz M. Influence of folic acid supplementation on coagulation, inflammatory, lipid, and kidney function parameters in subjects with low and moderate content of folic acid in the diet. Kardiol Pol. 2015;73(4):280–286. doi:10.5603/KP.a2014.0209
15. de Benoist B. Conclusions of a WHO Technical Consultation on folate and vitamin B12 deficiencies. Food Nutr Bull. 2008;29(2 Suppl):S238–44. doi:10.1177/15648265080292S129
16. Chandna SM, Farrington K. Residual renal function: considerations on its importance and preservation in dialysis patients. Semin Dial. 2004;17(3):196–201. doi:10.1111/j.0894-0959.2004.17306.x
17. Yang C, Wijerathne CUB, Tu GW, et al. Ischemia-reperfusion injury reduces kidney folate transporter expression and plasma folate levels. Front Immunol. 2021;12:678914. doi:10.3389/fimmu.2021.678914
18. Opatrny Jr. K
19. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol. 1996;7(2):198–207. doi:10.1681/ASN.V72198
20. Misra M, Nolph KD, Khanna R, Prowant BF, Moore HL. Retrospective evaluation of renal kt/V(urea) at the initiation of long-term peritoneal dialysis at the University of Missouri: relationships to longitudinal nutritional status on peritoneal dialysis. ASAIO J. 2003;49(1):91–102. doi:10.1097/00002480-200301000-00015
21. Ebaid H, Bashandy SAE, Abdel-Mageed AM, Al-Tamimi J, Hassan I, Alhazza IM. Folic acid and melatonin mitigate diabetic nephropathy in rats via inhibition of oxidative stress. Nutr Metab. 2020;17:6. doi:10.1186/s12986-019-0419-7
22. Davies SJ, Phillips L, Griffiths AM, Naish PF, Russell GI. Analysis of the effects of increasing delivered dialysis treatment to malnourished peritoneal dialysis patients. Kidney Int. 2000;57(4):1743–1754. doi:10.1038/sj.ki.4495463
23. Yang Q, Li R, Zhong Z, et al. Is cystatin C a better marker than creatinine for evaluating residual renal function in patients on continuous ambulatory peritoneal dialysis? Nephrol Dial Transplant. 2011;26(10):3358–3365. doi:10.1093/ndt/gfr045
24. Li DY, Yin WJ, Zhou LY, et al. Utility of cystatin C-based equations in patients undergoing dialysis. Clinica Chimica Acta. 2018;485:282–287. doi:10.1016/j.cca.2018.07.010
25. Delaney MP, Stevens PE, Al Hasani M, Stowe HJ, Judge C, Lamb EJ. Relationship of serum cystatin C to peritoneal and renal clearance measures in peritoneal dialysis: a cross-sectional study. Am J Kidney Dis. 2008;51(2):278–284. doi:10.1053/j.ajkd.2007.08.018
26. Achón M, Alonso-Aperte E, Ubeda N, Varela-Moreiras G. Supranormal dietary folic acid supplementation: effects on methionine metabolism in weanling rats. Br J Nutr. 2007;98(3):490–496. doi:10.1017/S0007114507721499
27. Satko SG, Burkart JM, Bleyer AJ, Jordan JR, Manning T. Frequency and causes of discrepancy between Kt/V and creatinine clearance. Perit Dial Int. 1999;19(1):31–37. doi:10.1177/089686089901900106
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
