Back to Journals » Journal of Inflammation Research » Volume 15
The Relationship Between Plasma Selenium, Antioxidant Status, Inflammatory Responses and Ischemic Cardiomyopathy: A Case-Control Study Based on Matched Propensity Scores
Authors Luo Y, He X, Hu L, Zhao J, Su K, Lei Y, Li Y
Received 27 July 2022
Accepted for publication 20 September 2022
Published 10 October 2022 Volume 2022:15 Pages 5757—5765
DOI https://doi.org/10.2147/JIR.S383476
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Yinhua Luo,1,* Xiaohong He,2,* Linbo Hu,3 Jinbo Zhao,1 Ke Su,1 Yuhua Lei,1 Yuanhong Li1
1Cardiovascular Disease Center, Central Hospital of Tujia and Miao Autonomous Prefecture, Hubei University of Medicine, Shiyan, People’s Republic of China; 2Centre for Disease Control and Prevention, Enshi Center for Disease Control and Prevention, Enshi Prefecture, People’s Republic of China; 3Health Management Centre, Central Hospital of Tujia and Miao Autonomous Prefecture, Enshi Prefecture, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuanhong Li, Cardiovascular Disease Center, Central Hospital of Tujia and Miao Autonomous Prefecture, Hubei University of Medicine, Shiyan, People’s Republic of China, Email [email protected]
Background: Ischemic cardiomyopathy (ICM) with high morbidity and mortality is closely associated with an abnormal equilibrium of circulation selenium levels. The oxidative stress theory is the most accepted theory of selenium causing ischemic cardiomyopathy. However, the role of inflammatory responses in ICM has received limited attention.
Methods: This study included 119 subjects, 43 of whom were patients with ICM, and 76 were healthy controls. Blood specimens were collected from subjects and serum levels of inflammatory and oxidative stress indicators and plasma levels of selenium were measured.
Results: When plasma selenium and indicators of inflammation and oxidative stress were compared between groups, plasma selenium levels were significantly lower in the ICM group than in the control group (68.83874 vs 104.39775, p=0.02032), while indicators of inflammation such as tumour necrosis factor-alpha (TNF-α) (79.09773 vs 46.15634, p< 0.001), interleukin-6 (IL-6) (49.41484 vs 38.46923, p< 0.01) and neutrophil/lymphocyte ratio (3.696574 vs 2.383658, p< 0.001) were significantly higher in the ICM group than in the control group (all of these results were statistically different). Additionally, malondialdehyde (MDA), a marker of oxidative stress, was considerably higher in the ICM group than in the control group (61.63078 vs 39.0609, p< 0.01). In contrast, there were no significant differences in superoxide dismutase (SOD) levels between groups (p> 0.05). The Poisson regression analysis revealed a significant association between selenium and high levels of MDA, IL-6 and TNF-α (p< 0.05). Additionally, selenium was negatively connected with SOD levels and the neutrophil/lymphocyte ratio, but this relationship was not statistically significant (p=0.96, 0.15, respectively).
Conclusion: Selenium deficiency is strongly associated with the development of ICM, and with levels of inflammation and oxidative stress in patients with ICM. Selenium can prevent the development and delay the progression of ICM by alleviating inflammatory responses.
Keywords: inflammatory responses, ischemic cardiomyopathy, oxidative stress, selenium
Background
Ischemic cardiomyopathy (ICM), characterised by high mobility and mortality, is one of the most prevalent aetiologies of congestive heart failure (HF). The mechanism by which ischemic heart disease causes HF is through the development of left ventricular (LV) systolic dysfunction, usually resulting from previous acute myocardial infarction(s), and, alternatively, from an insidious process of progressive decline in systolic function without recognisable episodes of acute coronary syndromes.1 Thus, the term ICM describes the syndrome of HF caused by chronic LV systolic dysfunction resulting from underlying coronary artery disease (CAD). ICM is believed to affect more than 125 million people worldwide, and an average of 720,000 people in the United States experience their first myocardial infarction every year, thus resulting in ICM.2–4 ICM ultimately has a significant impact on individuals and even society.
The development and progression of ICM are closely associated with an abnormal equilibrium of circulation molecules such as minerals and trace elements (for example, selenium, copper and zinc) in the patient’s blood. Selenium is an essential trace element in the body and sufficient concentrations are required for numerous biological functions. These include thyroid hormone metabolism, antioxidant defences and immunological responses. They have also been observed to be essential in certain types of cancer.5
The most widely accepted theory explaining how selenium causes ICM is the oxidative stress theory. An imbalance in generating and eliminating reactive oxygen species (ROS) and its intermediates causes oxidative stress. This is harmful and contributes to the pathogenesis of cardiac dysfunction and induces irreversible myocardial tissue damage or cell death. Selenium is a component of the glutathione peroxidase enzyme (Se-GSH-Px).6 Since Se-GSH-Px can reduce oxidative stress and platelet aggregation,7 it was believed that having a high selenium status would protect against cardiovascular disease.8 Additionally, a considerable number of evidence7,9 supports the abovementioned mechanism in the pathogenesis of ICM.
However, the role of inflammatory responses in ICM has received limited attention. It has been reported that selenium supplements can effectively alleviate inflammatory responses. Rancano, K.M. et al reported that in a cohort encompassing elderly women, selenium supplementation was observed to ameliorate obesity-induced inflammatory responses. There was an increase in insulin-like growth factor 1, a central biomarker in inflammation,10 following selenium supplementation.10,11 There are, however, limited studies that compare the selenium status, levels of inflammatory markers and oxidative stress between patients with ICM and healthy controls. The impact of selenium on inflammation in the population with ICM requires further study. This present case-control study specifically investigated the interrelationships between selenium status, oxidative stress and inflammatory responses in the population with ICM to aid future researchers in their investigation of the role of selenium on ICM and its relevant mechanism. This study confirmed that serum selenium levels are significantly lower in patients with ICM than in healthy controls and that low selenium levels are significantly correlated with increased levels of inflammatory response and oxidative stress in vivo.
Methods and Material
Study Population
This study was conducted in the Cardiovascular Disease Center, Central Hospital of Tujia and Miao Autonomous Prefecture, China (Research approval was obtained from the Ethical Committees of Central Hospital of Enshi Tujia and Miao Autonomous Prefecture). The study included 119 subjects, of whom 43 were patients with ICM and 76 were healthy controls. Additionally, both groups were homogeneous in terms of area of origin and long-term residence. Patients with ICM were recruited for the study by clinicians based on expert consensus on ICM 2020.2 ICM is defined as LV dysfunction caused by CAD, with or without clinical HF.2 The inclusion criteria for subjects selected as the control group were as follows. First, no coronary stenosis was confirmed by a coronary angiogram. Second, the patient has no family history of coronary heart disease. This study was conducted following the Helsinki declaration.
Plasma Selenium Determination
Early in the morning, we collected 2 mL of fasting venous blood from the elbow of each subject in two anticoagulation tubes. After centrifugation at 2000 rpm for 15 min, the upper serum was collected in freezing tubes and was then frozen at −80 °C for storage until biochemical examination. Subsequently, 1-mL aliquots of plasma were frozen at −20 °C for transportation and storage in the laboratory of Central Hospital of Enshi Tujia and Miao Autonomous Prefecture until analysis. Within a week of blood collection, the plasma samples were used to measure selenium using an atomic emission photoelectric optical emission spectrometer (AFS-930, Beijing).12,13
Serum Biomarkers Measurement
Interleukin-6 (IL-6), tumour necrosis factor-alpha (TNF-α), superoxide dismutase (SOD) and malondialdehyde (MDA) in serum were determined using an enzyme-linked immunosorbent assay kit (Cloud-clone corp, SEA079Hu, SEA133Hu, SES134Hu, CEA597Ge, respectively).
Quality Control
We employed a set of unified protocols for laboratory quality control and quality control in sample collecting, packing, coding and transportation. All technicians were trained prior to the start of the trial, and the same batch numbers were used to purchase all test reagents. Each sample batch contained blank samples, 10% parallel samples and quality control samples that met the requirements of the quality control standards.
Statistical Analysis
We conducted propensity score matching (PSM) to account for confounding biases and construct a scenario resembling a randomised experiment. PS were estimated using a logistic regression model in which patient characteristics were regarded as covariates. These included age and gender. Using a PS graph, we determined the degree of PS value and covariates overlap between the ICM and control groups. To avoid bias from distant matches, matching was performed using Coarsened Exact Matching with a calliper of 0.02. The balance between groups was defined as a p-value of ˃0.05.
The two groups of patients were matched based on age and sex using the PSM method, and the matched subgroups were compared. Quantitative variables were reported as mean ± standard deviation. For data before propensity matching, independent t-tests were used where chi-squared was satisfied; otherwise, Wilcox tests were used. The paired t-tests were used for group comparisons of data after propensity matching.
To explore the correlation between inflammatory and oxidative stress indicators and selenium, we used Poisson distribution. Results were considered significant if p≤0.05. Data were analysed using R version 4.0 software.
Results
Prior to PSM, the ICM and control groups included 43 and 76 patients, respectively. The baseline characteristics of the ICM and control groups before data propensity matching are presented in Table 1. Sex, platelet distribution width, white blood cell count, alanine transferase (ALT) concentration, total triglycerides, height, weight, fasting blood glucose and systolic blood pressure (SBP) were similar between groups.
 |
Table 1 The Baseline Characteristics of the Subjects |
When comparing the basic characteristics of the ICM and control groups before PSM, as presented in Table 1, it was observed that the age range of the case and control groups was 60–74 and 49–67.75 years, respectively. Statistical differences in indicators such as age, red cell distribution width, haemoglobin concentration, platelet count, SBP and creatinine were observed between groups. The remaining baseline indicators were balanced.
Figure 1 reveals that the age and sex of the two groups tended to be balanced after matching, ie, the matching effect was satisfied, and it was verified by regression analysis to achieve the desired outcome. As presented in Table 2, when the matched data for plasma selenium and indicators of inflammation and oxidative stress were compared between groups, plasma selenium levels were significantly lower in the ICM group than in the control group, and indicators of inflammation such as TNF-α, IL-6 and neutrophil/lymphocyte ratio were significantly higher in the ICM group than in the control group (all of these results were statistically different). Furthermore, MDA, an indicator of antioxidant stress, was significantly higher in the ICM group than that in the control group. While SOD did not differ significantly in the comparison between groups (p>0.05).
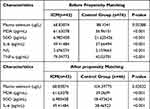 |
Table 2 Plasma Selenium Levels and Biomarker Index Levels Between Groups |
 |
Figure 1 The age and gender of the two groups tended to be balanced after matching, the matching effect was satisfied. |
The Poisson regression analysis in Table 3 revealed a significant correlation between selenium and elevated levels of MDA, IL-6 and TNF-α (p<0.05).
 |
Table 3 Pearson Correlation Coefficient Between Plasma Selenium Level and Other Variables |
Discussion
It is confirmed that the neutrophil/lymphocyte ratio, an index associated with inflammatory response and neointimal proliferation, is a potent inflammatory indicator.14 In this study, 43 patients with ICM who had undergone angiographical confirmation were assessed for plasma levels of selenium, oxidative stress status (SOD and MDA) and inflammatory responses status (IL-6, TNF-α and neutrophil/lymphocyte ratio), and the results were compared to those from healthy controls. Our findings revealed that plasma selenium levels were significantly correlated with the risk of ICM and serum levels of IL-6, MDA, TNF-α and neutrophil/lymphocyte ratio were significantly higher in patients with ICM than in controls. In addition, correlation analysis suggested that selenium deficiency was significantly associated with serum levels of IL-6, MDA and TNF-α.
Selenium, an essential micronutrient and an important component of selenoproteins, has been reported to prevent the development of ICM and delay its progression by combating oxidative stress. The influence of selenium on cardiomyopathy came to light in 1935 when reports of Keshan disease15 were made in Keshan County, China. Among these, selenium is involved in combating oxidative stress and delaying the formation of cardiomyopathy. It has been reported that selenium is an essential micronutrient that can ameliorate ROS formation,16 increase antioxidant defence and thus acts as an antioxidant stress agent.17,18 We previously explored the association of plasma selenium with coronary heart disease and cardiomyopathy in rat models and demonstrated that selenium deficiency is closely related to the severity and progression of coronary heart disease, by disrupting the natural structure of erythrocytes and thereby decreasing erythrocyte deformability.19 Furthermore, this study indicated that the patients with ICM had significantly lower mean plasma selenium levels and the biomarkers that can reflect the oxidative stress status (MDA) than healthy controls (P<0.001), which is consistent with the findings of Miguel Navarro-Alarco´n et al.20 Selenium prevents the reaction of MDA, a metabolite of lipid peroxidation, with deoxyribonucleic acid (DNA) in tissues and prevents DNA degeneration, inhibits tumours and related inflammation-related diseases, increases the activity of GSH-Px and interrupts the process of lipid peroxidation in the body. Thus, effectively protects cell and organelle membranes from damage, prevents various biochemical disorders and maintains normal physiological functions of the organism. Regretfully, SOD did not significantly differ between groups and there was no correlation observed between selenium and SOD levels. This is perhaps understandable given that glutathione peroxidase and SOD are two different antioxidant systems.
Although the ability of selenium to delay the development of ICM by reducing oxidative stress is the focus of attention, researchers seem to have overlooked the ability of selenium to alleviate inflammatory response. Subsequently, there is not sufficient evidence to conclude whether selenium can prevent the development of ICM and delay its progression by alleviating inflammatory responses. We conduct such a study for this reason.
Selenium has been reported to be associated with various inflammatory diseases21–28 such as inflammatory bowel disease,26 experimental colitis,24 chronic lymphocytic thyroiditis and hypothyroidism.25 Federico Galusso et al29 reported that low plasma selenium status and Development or risk of severe active inflammatory disease, such as systemic inflammatory response syndrome and multiple organ dysfunction syndromes, are closely linked. In addition, individuals with asthma, a chronic inflammatory disease, have been reported to have lower selenium status and decreased activity of glutathione peroxidase.30–33 Selenium deficiency is associated with both active inflammation and chronic inflammatory diseases. Selenium is currently believed to reduce the inflammatory response mainly through the following mechanisms: The nuclear factor kappa-B (NF-κB) activation process may be inhibited by selenium by regulating the expression of selenoprotein genes. In addition, the NF-κB signalling pathway and the generation of IL-6 and TNF have also been associated with elevated inflammatory responses. In summary, selenium deficiency is associated with the development and progression of many inflammatory diseases by inducing an inflammatory response and causing an exacerbation of the inflammatory response.
Furthermore, to our best knowledge, inflammatory responses and ICM are closely correlated. ICM is divided into three stages: Acute inflammation, reparative inflammation (days 4–14 after myocardial infarction) and chronic inflammation (>14 days after MI).34 It is well known that inflammatory response permeates all stages of the ICM disease progress. The early inflammatory response contributes to cardiac remodelling; however, studies on animals and patients with HF have reported that sustained inflammation is a cornerstone of adverse cardiac remodelling.34,35 The relationship between selenium and the inflammatory response and between ICM and the inflammatory response have all been the subject of numerous research, but there are none on the relationship between selenium, the inflammatory response and ICM. In our study, we demonstrated that compared with healthy controls, patients with ICM have a significantly low selenium status, significantly high inflammation levels and a significant correlation between selenium and inflammatory response. Despite its limitations, this study indicated that patients with ICM had significantly lower serum selenium levels and significantly higher levels of inflammatory and oxidative stress indicators than the healthy controls, and there was a significant correlation between selenium levels and both inflammatory and oxidative stress indicators.
Furthermore, this article offered a theoretical and experimental analysis of the ICM formation process and the pathogenesis of ICM by examining the relationship between selenium status, oxidative stress and inflammatory responses in patients with ICM. Our findings will provide useful feedback information for preventing the emergence of ICM and enhancing the prognoses of pertinent patients. In addition, our study may help patients, clinicians and policymakers make better evidence-based decisions for the initial treatment of these conditions.
Limitation
Even though we made every effort to improve our studies, there are still certain limitations. First, we did not examine further how oxidative stress and inflammatory responses to selenium can influence ICM. Nonetheless, this will be our next project. Second, although our study complied with the 0.9 minimum sample size criteria, the accuracy of our experiments was constrained by the small sample size. Last, this was a single-centre study with a relatively small population.
Conclusion
In our study, we have found that compared to healthy subjects, patients with ICM have a significantly lower selenium status, while inflammation levels were significantly higher and there was a significant correlation between selenium and inflammatory response. No withstanding its limitation, this study does suggest that selenium may prevent the development and delay the progression of ICM by alleviating the inflammatory responses.
Data Sharing Statement
All relevant data supporting the conclusions of this article are included within the article.
Ethical Approval
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethical Committees of Central Hospital of Enshi Tujia and Miao Autonomous Prefecture. Written informed consent was obtained from all patients to use their clinical data in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the corresponding author. The corresponding author agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
Yinhua Luo and Xiaohong He are co-first authors for this study. The authors declare that they have no conflict of interest.
References
1. Panza JA, Chrzanowski L, Bonow RO. Myocardial Viability Assessment Before Surgical Revascularization in Ischemic Cardiomyopathy: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;78(10):1068–1077. doi:10.1016/j.jacc.2021.07.004
2. Bakaeen FG, Gaudino M, Whitman G, et al. 2021: the American Association for Thoracic Surgery Expert Consensus Document: coronary artery bypass grafting in patients with ischemic cardiomyopathy and heart failure. J Thorac Cardiovasc Surg. 2021;162(3):829–850.e1. doi:10.1016/j.jtcvs.2021.04.052
3. Khan MA, Hashim MJ, Mustafa H, et al. Global epidemiology of ischemic heart disease: results from the global burden of disease study. Cureus. 2020;12(7):e9349. doi:10.7759/cureus.9349
4. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American heart association. Circulation. 2021;143(8):e254–e743. doi:10.1161/CIR.0000000000000950
5. Bomer N, Grote Beverborg N, Hoes MF, et al. Selenium and outcome in heart failure. Eur J Heart Fail. 2020;22(8):1415–1423. doi:10.1002/ejhf.1644
6. Rotruck JT, Pope AL, Ganther HE, Swanson AB, Hafeman DG, Hoekstra WG. Selenium: biochemical role as a component of glutathione peroxidase. Science. 1973;179(4073):588–590. doi:10.1126/science.179.4073.588
7. Salonen JT, Salonen R, Seppänen K, et al. Relationship of serum selenium and antioxidants to plasma lipoproteins, platelet aggregability and prevalent ischaemic heart disease in Eastern Finnish men. Atherosclerosis. 1988;70(1–2):155–160. doi:10.1016/0021-9150(88)
8. Boucher FR, Jouan MG, Moro C, Rakotovao AN, Tanguy S, de Leiris J. Does selenium exert cardioprotective effects against oxidative stress in myocardial ischemia? Acta Physiol Hung. 2008;95(2):187–194. doi:10.1556/APhysiol.95.2008.2.3
9. Salonen JT, Alfthan G, Huttunen JK, Pikkarainen J, Puska P. Association between cardiovascular death and myocardial infarction and serum selenium in a matched-pair longitudinal study. Lancet. 1982;2(8291):175–179. doi:10.1016/s0140-6736(82)
10. Rancaño KM, Ralston PA, Lemacks JL, Young-Clark I, Ilich JZ. Antioxidant intake in relation to serum C-reactive protein in mid-life and older African Americans. Ethn Health. 2020;25(8):1132–1144. doi:10.1080/13557858.2018.1492707
11. Alehagen U, Johansson P, Aaseth J, Alexander J, Brismar K. Increase in insulin-like growth factor 1 (IGF-1) and insulin-like growth factor binding protein 1 after supplementation with selenium and coenzyme Q10. A prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. PLoS One. 2017;12(6):e0178614. doi:10.1371/journal.pone.0178614
12. Navarro M, López H, Ruiz ML, González S, Pérez V, López MC. Determination of selenium in serum by hydride generation atomic absorption spectrometry for calculation of daily dietary intake. Sci Total Environ. 1995;175(3):245–252. doi:10.1016/0048-9697(95)
13. Navarro M, Lopez H, Lopez MC, Perez V. Determination of selenium in urine by hydride generation atomic absorption spectrometry. J AOAC Int. 1996;79(3):773–776. doi:10.1093/jaoac/79.3.773
14. Luo Y, Tan N, Zhao J, Li Y. A nomogram for predicting in-stent restenosis risk in patients undergoing percutaneous coronary intervention: a population-based analysis. Int J Gen Med. 2022;15:2451–2461. doi:10.2147/IJGM.S357250
15. Wang S, Yan R, Wang B, Meng P, Tan W, Guo X. The functional analysis of selenium-related genes and magnesium-related genes in the gene expression profile microarray in the peripheral blood mononuclear cells of keshan disease. Biol Trace Elem Res. 2019;192(1):3–9. doi:10.1007/s12011-019-01750-2
16. Hart WE, Marczak SP, Kneller AR, French RA, Morris DL. The abilities of selenium dioxide and selenite ion to coordinate DNA-bound metal ions and decrease oxidative DNA damage. J Inorg Biochem. 2013;125:1–8. doi:10.1016/j.jinorgbio.2013.03.016
17. Farrokhian A, Bahmani F, Taghizadeh M, et al. Selenium Supplementation Affects Insulin Resistance and Serum hs-CRP in Patients with Type 2 Diabetes and Coronary Heart Disease. Horm Metab Res. 2016;48(4):263–268. doi:10.1055/s-0035-1569276
18. Bahmani F, Kia M, Soleimani A, Asemi Z, Esmaillzadeh A. Effect of selenium supplementation on glycemic control and lipid profiles in patients with diabetic nephropathy. Biol Trace Elem Res. 2016;172(2):282–289. doi:10.1007/s12011-015-0600-4
19. Zhang C, Deng Y, Lei Y, Zhao J, Wei W, Li Y. The relationship between plasma selenium concentration and erythrocyte deformability in rat models of coronary heart disease. Minerva Cardioangiol. 2018;66(4):518–520. doi:10.23736/S0026-4725.18.04599-1
20. Navarro-Alarcón M, López-Garcia de la Serrana H, Pérez-Valero V, López-Martínez C. Serum and urine selenium concentrations in patients with cardiovascular diseases and relationship to other nutritional indexes. Ann Nutr Metab. 1999;43(1):30–36. doi:10.1159/000012764
21. Ayoglu H, Sezer U, Akin M, et al. Selenium, copper, zinc, iron levels and mortality in patients with sepsis and systemic inflammatory response syndrome in Western Black Sea Region, Turkey. J Pak Med Assoc. 2016;66(4):447–452.
22. Duntas LH. Selenium and inflammation: underlying anti-inflammatory mechanisms. Horm Metab Res. 2009;41(6):443–447. doi:10.1055/s-0029-1220724
23. Parnham MJ, Winkelmann J, Leyck S. Macrophage, lymphocyte and chronic inflammatory responses in selenium deficient rodents. Association with decreased glutathione peroxidase activity. Int J Immunopharmacol. 1983;5(5):455–461. doi:10.1016/0192-0561(83)90022-x
24. Speckmann B, Steinbrenner H. Selenium and selenoproteins in inflammatory bowel diseases and experimental colitis. Inflamm Bowel Dis. 2014;20(6):1110–1119. doi:10.1097/MIB.0000000000000020
25. Sun C, Zhu M, Li L, Fan H, Lv F, Zhu D. Clinical Observation of Levothyroxine Sodium Combined with Selenium in the Treatment of Patients with Chronic Lymphocytic Thyroiditis and Hypothyroidism and the Effects on Thyroid Function, Mood, and Inflammatory Factors. Evid Based Complement Alternat Med. 2021;2021:5471281. doi:10.1155/2021/5471281
26. Vaghari-Tabari M, Jafari-Gharabaghlou D, Sadeghsoltani F, et al. Zinc and selenium in inflammatory bowel disease: trace elements with key roles? Biol Trace Elem Res. 2021;199(9):3190–3204. doi:10.1007/s12011-020-02444-w
27. Angstwurm MW, Engelmann L, Zimmermann T, et al. Selenium in Intensive Care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Crit Care Med. 2007;35(1):118–126. doi:10.1097/01.CCM.0000251124.83436.0E
28. Sakr Y, Reinhart K, Bloos F, et al. Time course and relationship between plasma selenium concentrations, systemic inflammatory response, sepsis, and multiorgan failure. Br J Anaesth. 2007;98(6):775–784. doi:10.1093/bja/aem091
29. Manzanares W, Biestro A, Galusso F, et al. Serum selenium and glutathione peroxidase-3 activity: biomarkers of systemic inflammation in the critically ill? Intensive Care Med. 2009;35(5):882–889. doi:10.1007/s00134-008-1356-5
30. Miller AL. The etiologies, pathophysiology, and alternative/complementary treatment of asthma. Altern Med Rev. 2001;6(1):20–47.
31. Misso NL, Powers KA, Gillon RL, Stewart GA, Thompson PJ. Reduced platelet glutathione peroxidase activity and serum selenium concentration in atopic asthmatic patients. Clin Exp Allergy. 1996;26(7):838–847. doi:10.1111/j.1365-2222.1996.tb00616.x
32. Kadrabová J, Madaric A, Kovaciková Z, Podivínsky F, Ginter E, Gazdík F. Selenium status is decreased in patients with intrinsic asthma. Biol Trace Elem Res. 1996;52(3):241–248. doi:10.1007/BF02789165
33. Flatt A, Pearce N, Thomson CD, Sears MR, Robinson MF, Beasley R. Reduced selenium in asthmatic subjects in New Zealand. Thorax. 1990;45(2):95–99. doi:10.1136/thx.45.2.95
34. Michels da Silva D, Langer H, Graf T. Inflammatory and Molecular Pathways in Heart Failure-Ischemia, HFpEF and Transthyretin Cardiac Amyloidosis. Int J Mol Sci. 2019;20(9):2322. doi:10.3390/ijms20092322
35. Inflammatory AT. Mechanisms of Cardiovascular Remodeling. Circ J. 2018;82(3):629–635. doi:10.1253/circj.CJ-18-0063
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
