Back to Journals » Clinical Epidemiology » Volume 12
The Relationship Between Health-Related Quality of Life and Trust in Primary Care Physicians Among Patients with Diabetes
Authors AlRuthia Y , Sales I , Almalag H , Alwhaibi M , Almosabhi L , Albassam AA , Alharbi FA , Bashatah A , Asiri Y
Received 1 November 2019
Accepted for publication 20 January 2020
Published 5 February 2020 Volume 2020:12 Pages 143—151
DOI https://doi.org/10.2147/CLEP.S236952
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Vera Ehrenstein
Yazed AlRuthia,1,2 Ibrahim Sales,1 Haya Almalag,1 Monira Alwhaibi,1,3 Latifa Almosabhi,1 Ahmed A Albassam,4 Fawaz Abdullah Alharbi,5 Adel Bashatah,6 Yousif Asiri1
1Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 2Pharmacoeconomics Research Unit, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 3Medication Safety Research Chair, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia; 4Department of Clinical Pharmacy, College of Pharmacy, Prince Sattam Bin Abdulaziz University, Alkharj, Saudi Arabia; 5Drug Information and Poison Centre, Alansar Hospital, Medina, Saudi Arabia; 6Department of Nursing Education and Administration, College of Nursing, King Saud University, Riyadh, Saudi Arabia
Correspondence: Yazed AlRuthia
Department of Clinical Pharmacy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Tel +966 11 4677483
Fax +966 11 4677480
Email [email protected]
Background: Trust is pivotal for a productive relationship between patients and healthcare providers and is positively correlated with multiple clinical and humanistic outcomes. However, the impact of trust in healthcare providers on different domains of health-related quality of life (HRQoL) among diabetic patients has not been studied in detail.
Purpose: The aim of this study was to examine the association between the physical, mental or psychological, social, and environmental domains of HRQoL with the patients’ trust in their primary care physicians while controlling for several sociodemographic and clinical factors. The study was conducted among a sample of diabetic patients.
Patients and Methods: This study had a prospective questionnaire-based, multi-center, cross-sectional design. The patients were recruited from three public hospitals in Saudi Arabia. Patients’ experiences and trust in their primary care physicians were assessed using the Health Care Relationship Trust (HCR-Trust) scale. HRQoL was assessed using the Arabic version of the World Health Organization Quality of Life-BREF (WHOQOL-BREF). Multiple linear regression was conducted to assess the relationship between HCR-Trust and the WHOQOL-BREF physical, psychological, social, and environmental domains controlling for age, Charlson Comorbidity Index (CCI) score, health literacy, sex, education, annual income, nationality, and illness duration.
Results: Three hundred and sixty-four patients participated in the study. The scores in all four domains of WHOQOL-BREF were positively associated with HCR-Trust scores of the diabetic patients. Additionally, the scores in the physical (β = − 10.26; 95% CI: − 13.77 to − 6.74; P < 0.0001) and psychological (β = − 3.91; 95% CI: − 7.44 to − 0.38; P < 0.0001) domains were negatively associated with female gender. Furthermore, the physical domain score was negatively associated with the duration of illness (β = − 0.26; 95% CI: − 0.506 to − 0.02; P = 0.032). The environmental domain score was positively associated with annual income (β = 2.31; 95% CI: 1.05 to 3.56; P = 0.030). Other patient characteristics, such as age and education, were not associated with the scores of any of the WHOQOL-BREF domains.
Conclusion: Patient trust in healthcare providers is positively associated with different domains of HRQoL. Therefore, building and maintaining trust with patients is important to achieve favorable treatment outcomes.
Keywords: trust, health-related quality of life, diabetes
Introduction
Trust is one of the cornerstones of a productive and healthy patient–provider relationship. Trust is defined as “a belief held by a trustor that a trustee will act in the best interest of the trustor, even if such action may not be in the best interest of the trustee”.1 However, the power in the patient–provider relationship is ultimately held by the provider, and any misuse of power can be detrimental to the relationship and patient care.2 Patients actively search for providers they can trust, but building a firm and unwavering trust is a process that occurs over the course of the patient–provider relationship.3 LoCurto and Berg identified a number of qualities and behaviors associated with developing and maintaining trust, such as “honesty, confidentiality, dependability, communication, competency, fiduciary responsibility, fidelity, and agency”.4 Moreover, effective cordial and interpersonal communication strategies, such as reverence, esteem, and empathy, are highly important in several clinical settings, because these strategies enhance the trust between patients and their healthcare providers.5–8 The failure to build trust between patients and their healthcare providers can lead to mistrust and distrust. Distrust is the opposite of trust. Yan defined distrust as one’s negative expectations of the other person in a dyadic relationship, or a person’s belief that the other person in the relationship will definitely not act in the former’s best interests.9 Mistrust occurs when the trust in a patient–provider relationship becomes damaged by an incident, breaching the existing bond.9
Even though the conduct of healthcare providers is most commonly identified as the reason for a suboptimal patient–provider relationship, Topp and Chipukuma10 described a chain of mistrust originating at the top of healthcare organizations and making its way down in their structure, ultimately negatively affecting patient outcomes. Specifically, lack of adequate resources and poor leadership lead to weak trust among providers in their workplace, contributing to low-quality and/or delayed healthcare services and, eventually, degrading the level of trust between the patient and the healthcare provider. Regrettably, this dissatisfaction may encourage patients to seek treatment options outside of the healthcare system, either due to the ease of access or simply because of a desire for a higher quality of care.10 An example of structural problems within the healthcare system resulting in patients’ mistrust was identified in urban regions of China.11 The study revealed that administratively instituted financial incentives such as bonuses and commissions prompt physicians to request and perform unnecessary examinations and procedures. These practices, in turn, give rise to generalized mistrust towards healthcare providers within patients.11
However, there is a reciprocal sense of mistrust of patients by physicians, often resulting from sensationalist media coverage.12 Due to the fear of retaliation from patients, their families, or various organized patients’ rights advocates, Chinese physicians have become less assertive in providing services that might be considered risky or criticized if unsuccessful.13 Using data from the Fifth National Health Service Survey in China and in-person interviews with the patients, Shan and colleagues explored the relationship between the patient-provider trust and external factors present at institutional and systemic levels. The researchers concluded that patient satisfaction is driven by patient trust, and high levels of patient trust are associated with a high standard of provided services, genuine and empathic patient–provider interaction, and high-quality health insurance plans.14 Moreover, race and ethnicity influence both patients’ trust in their healthcare providers15 and the healthcare providers’ trust in their patients.16
Patient trust in healthcare providers has a positive impact on both clinical and patient-reported outcomes.17 The clinical significance of mutual trust has been documented in various settings.18 The self-management abilities of patients with chronic conditions correlate positively with the level of trust in their healthcare providers.19 Additionally, the health-related quality of life (HRQoL) is significantly higher among patients who have a high level of trust in their dentists.20 Moreover, patient trust in healthcare providers is associated with improved medication adherence.21–24 Improved trust in healthcare providers is also associated with higher rates of colorectal cancer screening.25
HRQoL is a broad and multifaceted concept. According to Wilson and Cleary, HRQoL represents the patient’s general perception of his/her health status that covers a wide range of patient outcomes, such as the biological and physiological variables that determine patient health, symptom status (emotional, cognitive, and physical), and functional status (physical, social, and psychological). Therefore, its importance stems from the fact that it addresses patient satisfaction with the treatment, which is one of the three most important objectives in any treatment plan.26 Assessing patient HRQoL is crucial when comparing the effectiveness of different treatments; however, the complexity of this concept makes measuring HRQoL and capturing its different domains considerably difficult.27 Therefore, multiple tools have been developed to assess HRQoL and have been validated across different patient populations, such as Short Form Health Survey (SF-36) and Health Profiles.26 However, these tools vary widely in their length, domains, and face and construct validity.27 Consequently, selecting the appropriate tool to assess patient HRQoL is important. Even though the association between trust in healthcare providers and HRQoL has been reported,28–30 the analyses performed were characterized by an upward bias and a lack of control for potential confounders, such as some sociodemographic and medical characteristics.31 Moreover, these studies focused mainly on the relationship between trust in healthcare providers and the physical and/or mental domains of HRQoL;28–30 however, other HRQoL domains, such as social and environmental domains, were not included in the analyses. Therefore, the aim of this study was to examine the association between the physical, mental or psychological, social, and environmental domains of HRQoL with the patients’ trust in their primary care physicians while controlling for sociodemographic and clinical factors among a sample of diabetic patients. This objective was established as a result of the high incidence and prevalence rates of diabetes in Saudi Arabia, which are estimated to be as high as 21 per 100,000/year and 25%, respectively.32 Furthermore, diabetes complications require a long-term and trusting relationship between patients and healthcare providers.32
Materials and Methods
This study had a prospective questionnaire-based, multi-center, and cross-sectional design. Eligible patients were adults (≥18 y) with a confirmed diagnosis of diabetes and no cognitive disabilities (e.g., dementia) who were Arabic-speaking and taking prescription medications for diabetes. Patients who had inactive electronic medical records, gestational diabetes, speech disorders, or cancer were excluded. The subjects were recruited from three public hospitals in Riyadh, Alkharj, and Almadina, Saudi Arabia, and were identified from their electronic medical records. These three hospitals were selected based on the high reported prevalence estimates of diabetes in the geographic areas where the hospitals are located in comparison to other regions in Saudi Arabia.32 The data collection started in May, 2016 and ended in November, 2018.
A convenience sampling technique was used by asking the patients to participate in the study during the waiting time before their scheduled appointments with primary care physicians. The objective of the study was verbally explained to the patients prior to asking them to sign a consent form, which also contained a written explanation of the objective of the study and information regarding the right of the patients to withdraw from the study at any time. Once the consent form was signed, the patient was invited to a private meeting room for a face-to-face interview. The interviews were performed by six pharmacy interns (three interns in Riyadh, two in Alkharj, and one in Almadina) who were trained by clinical faculty members on data collection and patient interviews using the role-playing technique.
Patients’ experiences and trust in their primary care physicians were assessed using the Health Care Relationship Trust (HCR-Trust) scale developed by Bova and colleagues.33 The scale, which consists of 13 items, is available in both English and Arabic and both versions have good internal consistency (Cronbach’s alpha coefficient ≥ 0.9).33,34 The HCR-Trust scale has good validity in assessing patient trust in healthcare providers.35 The HCR-Trust scale is scored from 0 to 4 leading to a maximum score of 52, with high scores indicating high trust levels in healthcare providers.33 The Arabic version of HCR-Trust scale was used in this study.34
The Arabic version of the World Health Organization Quality of Life-BREF (WHOQOL-BREF) was used to assess the HRQoL of the recruited patients. This tool was used because it has adequate reliability and validity within the Arabic-speaking population.36 The 26 items of WHOQOL-BREF assess the physical, psychological, social, and environmental domains of the HRQoL. Each item of WHOQOL-BREF is scored using a five-level Likert scale (1= never; 2 = rarely; 3 = sometimes, 4 = often, and 5 = always). The physical domain consists of seven items and assesses the activities of daily living, energy and fatigue, mobility, pain and discomfort, sleep and rest, and ability to work. The psychological domain consists of six items and assesses body image and appearance, negative and positive feelings, religious and personal beliefs, and cognitive ability. The social relationship domain consists of three items assessing sexual activity, social support, and personal relationships. The environmental domain consists of eight items assessing personal financial resources, physical safety and security, healthcare accessibility and quality, transportation quality and accessibility, and home and physical environment (e.g., pollution, noise, traffic, and climate).36 The four domains of WHOQOL-BREF are scored separately with each domain having a maximum transformed score of 100.36
Health literacy was evaluated using the Arabic version of the Single Item Literacy Screener (SILS), which includes a single question assessing whether the patient needs assistance in understanding the information contained in a prescription drug leaflet.37,38 The “never” or “rarely” response indicates good health literacy, while responses such as “sometimes,” “often,” or “always” indicate marginal/limited level of health literacy.37
The sociodemographic characteristics of the patients, such as age, gender, education level, nationality, and annual income, were collected during the interview and verified using their electronic health records. Medical characteristics, such as disease history, names and number of prescription medications, and duration of illness were obtained from the patient electronic health records and confirmed with the patients during the interview. The burden of illness was determined by Charlson Comorbidity Index (CCI), which assigns variable weights to 17 different health conditions depending on their severity (e.g., metastatic solid tumor vs diabetes without complications).39 These health conditions were identified through the electronic health records of the recruited participants.
The baseline characteristics of the patients were described using mean, standard deviation, frequency, and percentage. The relationships between the HCR-Trust scores and the four domains of WHOQOL-BREF were examined using multiple linear regression analyses. Variables that might influence both HRQoL and trust in healthcare providers, such as patients’ age, sex, education level, health literacy, annual income, nationality, CCI score, duration of illness, and number of prescription medications, were controlled for in all regression analyses.31 The minimum sample size required to conduct multiple linear regression analyses was estimated to be 359 patients for an effect size of f2 = 0.02, power of 0.8, and α of 0.05.40 However, a sample size of 400 patients was planned to ensure adequate statistical power. SAS statistical software (version 9.2, SAS Institute Inc., Cary, NC, USA) was used in all statistical analyses.
The study was approved by Institutional Review Boards of King Saud University College of Medicine, Riyadh, Prince Sattam bin Abdulaziz University College of Medicine, AlKharj, and Al Ansaar General Hospital, Almadina, Saudi Arabia. Furthermore, the study adhered to the ethical guidelines of the Declaration of Helsinki for medical research.41
Results
A total of 472 diabetic patients met the inclusion criteria in the three medical centers (Figure 1). One hundred and eight patients withdrew from the study, leaving a total of 364 patients who completed the interviews. The mean age of the patients was approximately 54 y, and the majority of them were female (62%) and Saudi nationals (93%). The percentage of patients who did not receive a formal education or completed elementary, middle, high school, or some college degree ranged from 15% to 26%. Based on the SILS value, 188 patients (51.65%) were considered to have marginal/limited health literacy, while the remaining 176 (48.35%) were considered to have good health literacy. The distribution of annual incomes was very wide, with 87 (23.9%) of patients earning less than $9600 and eight (2.2%) earning more than $79,992 annually (Table 1).
 |
Table 1 Baseline Characteristics of the Diabetic Patients |
 |
Figure 1 Patient recruitment scheme. |
The majority of the patients took two or more prescription medications (70.34%), and more than one third of them (38.19%) had a Charlson Comorbidity Index (CCI) score > 2. Most of the patients suffered from the disease for more than 10 y (63.19%), and almost half of them had a HCR-Trust score ≥ 40 (47.80%; Table 1). The patients’ mean scores of the WHOQOL-BREF physical, psychological, social, and environmental domains were 53.64, 66.43, 66.18, and 69.96, respectively (Table 2). Patients with a high level of trust in their primary care physicians were more likely to have high physical HRQoL in comparison to their counterparts with a low level of trust in their primary care physicians (β = 0.64; 95% confidence interval: 0.50 to 0.79; P < 0.0001). On the other hand, female patients were less likely to have high physical HRQoL compared to their male counterparts (β = −10.26; 95% confidence interval: −13.77 to −6.74; P < 0.0001). Moreover, patients with a long duration of diabetes were less likely to have high physical HRQoL compared to their counterparts with short duration of diabetes (β = −0.26; 95% confidence interval: −0.506 to −0.02; P = 0.032). Age, CCI, health literacy, education, annual income, and nationality had no impact on the physical HRQoL (Table 3).
 |
Table 2 The World Health Organization Quality of Life-BREF (WHOQOL-BREF) Domain’s Scores |
 |
Table 3 Multiple Linear Regression Analysis of the Association Between the World Health Organization Quality of Life-BREF Physical Health Domain and Health Care Relationship (HCR) Trust Scores |
Similar analyses were performed to examine the association between HCR-Trust scores and the psychological (Table 4), social (Table 5), and environmental (Table 6) domains of WHOQOL-BREF. The results revealed that patients with high level of trust in their primary care physicians were more likely to have high psychological (β = 0.69; 95% confidence interval: 0.54 to 0.84; P < 0.0001), social (β = 0.68; 95% confidence interval: 0.48 to 0.88; P < 0.0001), and environmental (β = 0.74; 95% confidence interval: 0.59 to 0.88; P < 0.0001) HRQoL compared to their counterparts with low level of trust in their primary care physicians. Similar to the negative association between female gender and the physical domain of the HRQoL, female patients were less likely to have higher psychological HRQoL than their male counterparts (β = −3.91; 95% confidence interval: −7.44 to −0.38; P < 0.0001). On the other hand, patients with higher annual incomes were more likely to have higher environmental HRQoL than their counterparts with lower annual incomes (β = 2.31; 95% confidence interval: 1.05 to 3.56; P = 0.030). The other characteristics of the patients were not associated with the psychological, social, or environmental domains of the HRQoL.
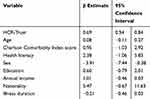 |
Table 4 Multiple Linear Regression Analysis of the Association Between the World Health Organization Quality of Life-BREF Psychological Domain and Health Care Relationship (HCR) Trust Scores |
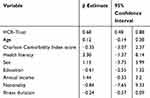 |
Table 5 Multiple Linear Regression Analysis of the Association Between the World Health Organization Quality of Life-BREF Social Domain and Health Care Relationship (HCR) Trust Scores |
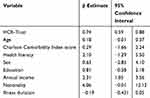 |
Table 6 Multiple Linear Regression Analysis of the Association Between the World Health Organization Quality of Life Environment Domain and Health Care Relationship (HCR) Trust Scores |
Discussion
Our study findings show a positive association between patient trust in healthcare providers and different domains of HRQoL. This strong and positive association unequivocally shows the importance of trust in the relationship between patients and their healthcare providers. Additionally, the physical and psychosocial domains of HRQoL were negatively associated with female gender, which is consistent with previously published research.42 Female gender is associated with worse HRQoL despite controlling for potential confounding factors, such as sociodemographic variables (e.g., age, income, and education, among others).42 Illness duration was negatively associated with the physical domain, consistent with previously published studies that found a negative association between the duration of chronic health conditions and HRQoL scores.43 Chronic health conditions, such as diabetes and arthritis, result in loss of HRQoL as time progresses.43 However, patients’ annual income was positively associated with the environmental domain of the HRQoL, which has been examined before.44 Other confounding factors, including age, comorbidities, health literacy, education, and nationality of the patient were not associated with any of the WHOQOL-BREF domain scores.
The number of studies focusing on trust and health-related quality of life among patients with diabetes is limited. A 2011 study reported that the impact of patient trust in primary care providers was associated with improved physical and psychological HRQoL scores among a cohort of Taiwanese patients with type 2 diabetes.28 Our study examined the impact of patient trust on the social and environmental domains of the HRQoL in addition to the physical and psychological domains of the HRQoL. Therefore, this study is in agreement with previous investigations and provides a detailed analysis of the potential impact of confounding factors.
The presence of an association does not indicate a cause-and-effect relationship. Therefore, the collected data do not answer the question whether it is the patient’s trust in the physician that leads to an improved HRQoL through better adherence to medications as an example or whether the perception of improved quality of life by the patient is promoted by his or her trust in the healthcare provider. Moreover, it remains to be determined whether trust in healthcare providers is merely a reflection of the level of interpersonal trust that the patient has towards other individuals, or is an independent characteristic, specific to the relationship with his or her physician. In this regard, a high level of general interpersonal trust has been demonstrated to be associated with lower mortality,45 emotional and physical health,46 and clinical outcomes.47 However, it has been suggested that some patients with naïve trust in healthcare providers may not appreciate the value of their own active participation in making health-related decisions, which could result in decreased health-related quality of life.28,48 The positive association between trust and HRQoL identified in our analysis does not support the notion that any degree of trust would undermine the health outcomes. However, more studies addressing specifically this point should be conducted to obtain a definitive answer.
An important area that has yet to be investigated is the active role of the physician in building this mutual relationship. This includes not only the personal attributes of the provider but also his professional ability to enable patients to better contend with their problems by understanding the diagnosis, symptoms, treatment options, and side effects.29,49,50 Another related question that should be addressed in future studies is whether the quality of life of patients may be affected by their trust in healthcare institutions and organizations, separately from their trust in individuals providing the care.51
Even though our findings highlight the importance of building a close and trustful patient–physician relationship, our study had some limitations. While the care for diabetic patients is inherently longitudinal, this was a cross-sectional study, which limits its ability to examine the impact of change in patient’s trust in primary care physicians on their HRQoL over time. It is well documented that both the extent of the patient’s trust in the healthcare provider and patient’s quality of life can vary over time.52,53 Therefore, longitudinal studies could provide more precise and generally applicable conclusions. Moreover, even though the study findings were positive after controlling for multiple confounding factors, the relationship between the two variables needs to be examined using a more robust design with better external validity, e.g., a prospective cohort study with cluster analysis. Additionally, the convenience sampling technique was used, which may have introduced sampling error and increased the risk of selection bias. The face-to-face interview method, which was used in the current investigation, may have introduced acquiescence bias, social desirability bias, and interviewer bias. However, this method was selected because it was deemed preferable by the respondents based on previously published research. Additionally, the method results in a fewer number of non-responders and a lower risk of recall bias.54 The reliance on self-reported measures may represent an additional form of bias.55
Conclusion
The present study underscores the value of a trustful relationship between the patient and healthcare providers. The developed trust benefits multiple aspects of health-related quality of life, which are of great value to patients with chronic health conditions such as diabetes. Future studies should examine the impact of patient trust in healthcare providers on their HRQoL in prospective and more robust study designs.
Abbreviations
HRQol, Health-Related Quality of Life; CCI, Charlson Comorbidity Index; WHO, World Health Organization; HCR-Trust, Health Care Relationship Trust; SILS, Single Item Literacy Screener; WHOQOL-BREF, World Health Organization Quality of Life-BREF (WHOQOL-BREF).
Data Sharing Statement
Study data are available from the authors upon request.
Acknowledgments
The authors are grateful to Nouf Alquait, Albandari Alnasser, Aliah Aldahash, and Majed Almuhaya for their data collection efforts. The authors acknowledge the financial support received from the Researchers Supporting Project number (RSP-2019/16), King Saud University, Riyadh, Saudi Arabia.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval for the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Marsh S, Dibben MR. Trust, untrust, distrust and mistrust – an exploration of the dark(er) side. In: Herrmann P, Issarny V, Shiu S, editors. Trust Management. Berlin, Heidelberg: Springer; 2005:17–33.
2. Delmar C. The excesses of care: a matter of understanding the asymmetry of power. Nurs Philos. 2012;13(4):236–243. doi:10.1111/j.1466-769X.2012.00537.x
3. Dawson-Rose C, Cuca YP, Webel AR, et al. Building trust and relationships between patients and providers: an essential complement to health literacy in HIV care. J Assoc Nurses AIDS Care. 2016;27(5):574–584. doi:10.1016/j.jana.2016.03.001
4. LoCurto J, Berg GM. Trust in healthcare settings: scale development, methods, and preliminary determinants. SAGE Open Med. 2016;4:2050312116664224. doi:10.1177/2050312116664224
5. Safran DG, Kosinski M, Tarlov AR, et al. The primary care assessment survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–739. doi:10.1097/00005650-199805000-00012
6. Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13(10):681–686. doi:10.1046/j.1525-1497.1998.00204.x
7. Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the trust in physician scale. The Stanford Trust Study Physicians. Med Care. 1999;37(5):510–517. doi:10.1097/00005650-199905000-00010
8. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi:10.1177/1077558702059003004
9. Yan Y. The ethics and politics of patient-physician mistrust in contemporary China. Dev World Bioeth. 2018;18(1):7–15. doi:10.1111/dewb.12155
10. Topp SM, Chipukuma JM. A qualitative study of the role of workplace and interpersonal trust in shaping service quality and responsiveness in Zambian primary health centres. Health Policy Plan. 2016;31(2):192–204. doi:10.1093/heapol/czv041
11. Chan CS. Mistrust of physicians in China: society, institution, and interaction as root causes. Dev World Bioeth. 2018;18(1):16–25. doi:10.1111/dewb.12162
12. Collier R. Professionalism: the importance of trust. CMAJ. 2012;184(13):1455–1456. doi:10.1503/cmaj.109-4264
13. Nie JB, Cheng Y, Zou X, et al. The vicious circle of patient-physician mistrust in China: health professionals’ perspectives, institutional conflict of interest, and building trust through medical professionalism. Dev World Bioeth. 2018;18(1):26–36. doi:10.1111/dewb.12170
14. Shan L, Li Y, Ding D, et al. Patient satisfaction with hospital inpatient care: effects of trust, medical insurance and perceived quality of care. PLoS One. 2016;11(10):e0164366. doi:10.1371/journal.pone.0164366
15. Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–365. doi:10.1016/S0033-3549(04)50262-5
16. Moskowitz D, Thom DH, Guzman D, et al. Is primary care providers’ trust in socially marginalized patients affected by race? J Gen Intern Med. 2011;26(8):846–851. doi:10.1007/s11606-011-1672-2
17. Eton DT, Ridgeway JL, Linzer M, et al. Healthcare provider relational quality is associated with better self-management and less treatment burden in people with multiple chronic conditions. Patient Prefer Adherence. 2017;11:1635–1646.
18. Anhang Price R, Elliott MN, Zaslavsky AM, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–554. doi:10.1177/1077558714541480
19. Cramm JM, Nieboer AP. Chronically ill patients’ self-management abilities to maintain overall well-being: what is needed to take the next step in the primary care setting? BMC Fam Pract. 2015;16:123. doi:10.1186/s12875-015-0340-8
20. Muirhead VE, Marcenes W, Wright D. Do health provider-patient relationships matter? Exploring dentist-patient relationships and oral health-related quality of life in older people. Age Ageing. 2014;43(3):399–405. doi:10.1093/ageing/aft183
21. Zolnierek KBH, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi:10.1097/MLR.0b013e31819a5acc
22. Nguyen GC, LaVeist TA, Harris ML, et al. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(8):1233–1239. doi:10.1002/ibd.20883
23. Young HN, Len-Rios ME, Brown R, Moreno MM, Cox E. How does patient-provider communication influence adherence to asthma medications? Patient Educ Couns. 2017;100(4):696–702. doi:10.1016/j.pec.2016.11.022
24. Linetzky B, Jiang D, Funnell MM, Curtis BH, Polonsky WH. Exploring the role of the patient–physician relationship on insulin adherence and clinical outcomes in type 2 diabetes: insights from the MOSAIc study. J Diabetes. 2017;9(6):596–605. doi:10.1111/1753-0407.12443
25. Carcaise-Edinboro P, Bradley CJ. Influence of patient-provider communication on colorectal cancer screening. Med Care. 2008;46(7):738–745. doi:10.1097/MLR.0b013e318178935a
26. Guyatt GH, Ferrans CE, Halyard MY, et al. Exploration of the value of health-related quality-of-life information from clinical research and into clinical practice. Mayo Clinic Proc. 2007;82(10):1229–1239. doi:10.4065/82.10.1229
27. Hays RD, Revicki DA. Reliability and validity, including responsiveness. In: Fayers P, Hays RD, editors. Assessing Quality of Life in Clinical Trials.
28. Lee YY, Lin JL. How much does trust really matter? A study of the longitudinal effects of trust and decision-making preferences on diabetic patient outcomes. Patient Educ Couns. 2011;85(3):406–412. doi:10.1016/j.pec.2010.12.005
29. Ernstmann N, Wirtz M, Nitzsche A, et al. Patients’ trust in physician, patient enablement, and health-related quality of life during colon cancer treatment. J Cancer Educ. 2017;32(3):571–579. doi:10.1007/s13187-017-1166-y
30. Jneid S, Jabbour H, Hajj A, et al. Quality of life and its association with treatment satisfaction, adherence to medication, and trust in physician among patients with hypertension: a cross-sectional designed study. J Cardiovasc Pharmacol Ther. 2018;23(6):532–542. doi:10.1177/1074248418784292
31. Birkhäuer J, Gaab J, Kossowsky J, et al. Trust in the health care professional and health outcome: a meta-analysis. PLoS One. 2017;12(2):e0170988. doi:10.1371/journal.pone.0170988
32. Alotaibi A, Perry L, Gholizadeh L, Al-Ganmi A. Incidence and prevalence rates of diabetes mellitus in Saudi Arabia: an overview. J Epidemiol Glob Health. 2017;7(4):211–218. doi:10.1016/j.jegh.2017.10.001
33. Bova C, Route PS, Fennie K, et al. Measuring patient–provider trust in a primary care population: refinement of the health care relationship trust scale. Res Nurs Health. 2012;35:397–408. doi:10.1002/nur.21484
34. AlRuthia Y, Almalag H, Sales I, et al. The relationship between trust in primary care physicians and medication knowledge among diabetic patients. Res Social Adm Pharm. 2019;15(6):656–661. doi:10.1016/j.sapharm.2018.08.004
35. Muller E, Zill J, Dirmaier J, Härter M, Scholl I. Assessment of trust in physician: a systematic review of measures. PLoS One. 2014;9:e106844. doi:10.1371/journal.pone.0106844
36. Ohaeri JU, Awadalla AW. The reliability and validity of the short version of the WHO quality of life instrument in an Arab general population. Ann Saudi Med. 2009;29(2):98–104. doi:10.4103/0256-4947.51790
37. Morris NS, MacLean CD, Chew LD, Littenberg B. The single item literacy screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006;7:21. doi:10.1186/1471-2296-7-21
38. Al-Jumaili AA, Al-Rekabi MD, Sorofman B. Evaluation of instruments to assess health literacy in Arabic language among Iraqis. Res Soc Adm Pharm. 2015;11:803–813. doi:10.1016/j.sapharm.2015.02.002
39. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
40. Pituch KA, Stevens JP. Applied Multivariate Statistics for the Social Sciences. New York: Routledge; 2016:793.
41. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
42. Hajian-Tilaki K, Heidari B, Hajian-Tilaki A. Are gender differences in health-related quality of life attributable to sociodemographic characteristics and chronic disease conditions in elderly people? Int J Prev Med. 2017;8:95. doi:10.4103/ijpvm.IJPVM_324_16
43. Busija L, Tan J, Sanders KM. Associations between illness duration and health-related quality of life in specified mental and physical chronic health conditions: results from a population-based survey. Qual Life Res. 2017;26(10):2671–2681. doi:10.1007/s11136-017-1592-7
44. Zhang Y, Ou F, Gao S, Gao Q, Hu L, Liu Y. Effect of low income on health-related quality of life: a cross-sectional study in northeast China. Asia Pac J Public Health. 2015;27(2):NP1013–1025. doi:10.1177/1010539513496839
45. Skrabski A, Kopp M, Kawachi I. Social capital in a changing society: cross sectional associations with middle aged female and male mortality rates. J Epidemiol Community Health. 2003;57(2):114–119. doi:10.1136/jech.57.2.114
46. Rose R. How much does social capital add to individual health? A survey study of Russians. Soc Sci Med. 2000;51(9):1421–1435. doi:10.1016/S0277-9536(00)00106-4
47. Poortinga W. Social capital: an individual or collective resource for health? Soc Sci Med. 2006;62(2):292–302. doi:10.1016/j.socscimed.2005.06.008
48. Kraetschmer N, Sharpe N, Urowitz S, Deber RB. How does trust affect patient preferences for participation in decision-making? Health Expect. 2004;7(4):317–326. doi:10.1111/hex.2004.7.issue-4
49. Thorne SE, Robinson CA. Reciprocal trust in health care relationships. J Adv Nurs. 1988;13:782–789. doi:10.1111/jan.1988.13.issue-6
50. Squier RW. A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships. Soc Sci Med. 1990;30:325–339. doi:10.1016/0277-9536(90)90188-X
51. Dinç L, Gastmans C. Trust in nurse-patient relationships: a literature review. Nurs Ethics. 2013;20:501–516. doi:10.1177/0969733012468463
52. Mainous AG, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001;33:22–27.
53. Williams J. Potential benefits of relationship continuity in patient care. Br J Nurs. 2014;23:S22–S25. doi:10.12968/bjon.2014.23.Sup5.S22
54. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health. 2005;27:281–291. doi:10.1093/pubmed/fdi031
55. Murphy G, Snetselaar L, Myers E, et al. Self-reported health parameters compared with clinician measurements: methods in practice-based research. J Public Health Manag Pract. 2014;20(5):513–522. doi:10.1097/PHH.0b013e3182a998fd
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
