Back to Journals » Nature and Science of Sleep » Volume 14
The Relationship Between Circadian Typology and Dry Eye Symptoms in Chinese College Students
Authors Yan C, Li A , Hao Y, Zhang X, Guo Y, Gu Y , Wang Y , Wen Y, Tian L, Jie Y
Received 15 June 2022
Accepted for publication 2 October 2022
Published 26 October 2022 Volume 2022:14 Pages 1919—1925
DOI https://doi.org/10.2147/NSS.S378612
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ahmed BaHammam
Chao Yan,* Ao Li,* Yiran Hao, Xiaozhao Zhang, Yihan Guo, Yixuan Gu, Yinghui Wang, Ya Wen, Lei Tian, Ying Jie
Beijing Institute of Ophthalmology, Beijing Tongren Hospital, Capital Medical University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ying Jie; Lei Tian, Tel +86-13693572296 ; +86-18600166885, Fax +861058265900, Email [email protected]; [email protected]
Purpose: To explore the relationship between symptomatic dry eye and circadian typology in college students.
Methods: This study included 269 students from 3 Chinese universities. All participants completed the ocular surface disease index (OSDI) questionnaire, the morningness-eveningness questionnaire (MEQ), and the Pittsburgh sleep quality index (PSQI) questionnaire. Participants were grouped into 3 types by the reduced MEQ (rMEQ) score:E-Type, N-Type, and M-Type. All these parameters were then analyzed for the effect on the severity of dry eye.
Results: The occurrence rates of poor sleep quality (PSQI> 5) and symptomatic dry eye (OSDI > 13) in the college students were 53.2% and 40.2%, respectively. The distribution of the circadian typology differed significantly among the college students with different dry eye severities (χ2 = 59.44, P = 0. 000), and E-type was associated with the most severe dry eye symptoms. The OSDI and PSQI scores were both significantly different among college students with different chronotypes (F = 22.14, P = 0.000; F = 15.21, P = 0.000; respectively). For both scores, the E-type scored the highest, followed by N-type, and M-type was the lowest. The circadian typology was an independent factor for dry eye. The risk of E-Type was 6.99 times higher than that of M-Type (P = 0.000), and the risk of N-types was 3.23 times higher than that of M-Type (P = 0.000). Sleep quality was also an independent risk factor for dry eye (P = 0.000). Gender and awareness of dry eye were not risk factors for dry eye.
Conclusion: The severity of dry eye symptoms and sleep quality were associated with different circadian typologies. The more the circadian preference tended to be E-type, the worse the sleep quality and the more serious dry eye symptoms would appear.
Keywords: circadian typology, college students, dry eye, sleep disorder
Introduction
Dry eye is a multifactorial disease that affects the ocular surface and tear film. Patients can present with symptoms including dryness, itching, coarseness, pain, light sensitivity, and blurred vision, which may significantly affect their daily life.1 In 2019, a nationwide clinical multicenter dry eye epidemiology survey conducted in China revealed that the prevalence of dry eye was as high as 57.6% among the 31,124 volunteers.2 Thus, dry eye is recognized as a substantial global public health and financial burden.1
The prevalence of dry eye is also high in the college student population. Asiedu et al reported that the prevalence of symptomatic dry eye was as high as 44.3% among the 650 college students.3 In addition, more and more evidence shows that lifestyle is an important risk factor for dry eye development.4 Both poor sleep quality and psychological distress can contribute to symptomatic dry eye, which can, in turn, exacerbate the original psychological distress as well as sleep disorders.5 Moreover, these risk factors are related to the circadian rhythms. Circadian rhythms play important roles in the regulation of biological functions, including sleep/wake preference, body temperature, hormone secretion, etc. Disturbances in circadian rhythms can lead to chronic diseases and sleep disorders.6
Circadian rhythms in humans manifest as a complex phenotype with many physiological processes, of which the most prominent circadian rhythms in mammals are sleeping and waking.7 Circadian phase preference shows large differences in both biological and behavioral parameters, and different circadian rhythms lead to different sleep and activity times. This characteristic is reflected by the Circadian Typology (CT).8 CT is generally considered as an individual trait with a genetic basis. It is also influenced by external factors and varies across the lifespan, which reflects the different chronobiological phenotypes due to individual variation in circadian rhythms.9 Based on the circadian preferences, there are three distinct chronotypes: the morning type (M-Type), the evening type (E-Type) and neither type (N-Type).10 M-Type is more efficient and active during the first half of the day, while the E-Type has difficulty getting up in the morning and requires more time to reach optimal levels of mental and physical efficiency. N-Type exhibits intermediate features with no apparent circadian preference.10 This interindividual variation affects our biological and psychological functioning, not only in health but also in disease.8 Studies have found that biological rhythms vary among students, such as when they get up, when they sleep, or when they feel the best.9
However, whether different types of CT are related to dry eye in college students has not been studied. It is of prospective significance to study the relationship between CT and dry eye in the student population. This cross-sectional study aims to investigate the association between dry eye and the chronotype, so that preventive interventions can be taken in the future to reduce the prevalence of dry eye in the student population.
Patients and Methods
Survey Procedure and Data Collection
This study was a cross-sectional questionnaire-based survey conducted among students from 3 Chinese universities. Data collection started in September and ended in December 2021 (4 months). Inclusion criterion was college students who were willing to participate in this study. Exclusion criteria included: (1) any active external ocular diseases, (2) history of ocular surgery, (3) history of ocular trauma, (4) other eye diseases, (5) long term or frequent use of contact lens, (6) cognitive dysfunction. In total, 352 students were randomly selected and requested to complete the questionnaire. The study assistants contacted the students and conducted a survey including demographic data, dry eye symptoms, potential risk factors for dry eye disease, sleep quality, CT, and awareness of dry eye (Ever heard of dry eye). The final dataset included a total of 269 subjects. The gender of the students was determined due to random sampling. The age range ranged from 19–25 years (Table 1).
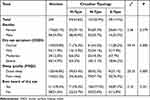 |
Table 1 Characteristics of the Study Population (n=269) |
This study was conducted in accordance with the tenets of the Declaration of Helsinki and approved by the Ethical Committee of Beijing Tongren Hospital. Informed consent was obtained from all participants.
CT
The morningness-eveningness questionnaire (MEQ) is one of the most widely used questionnaires for determining the type of CT.10 Reduced MEQ (rMEQ) is the shortened 5-item version of the standard 19-item MEQ, including sleeping and waking hours, peak time, morning alertness, and self-assessment of chronotype (Figure 1). rMEQ accounts for 83% of the total variance of the original MEQ and has advantages of simplicity and stability, and thus was used to assess the chronotype in the current study.11 The first four questions were scored 1–5, and question 5 was scored 0–6. The total score ranged from 4 to 26. Participants were grouped into 3 types by the rMEQ score:E-Type (<12 points), N-Type (12–17 points), and M-Type (>17 points).
 |
Figure 1 Questionnaire of rMEQ in this study. Abbreviation: rMEQ, reduced morningness-eveningness questionnaire. |
Sleep Quality
The Pittsburgh sleep quality index (PSQI) questionnaire is a scale for assessing sleep quality. It examines 7 components of sleep quality over the past month: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleeping pill use, and disorders in daily activities. The 7 components were derived from 19 self-rated questions in the questionnaire, and each component was scored 0–3. The total score ranged from 0–21. Participants were grouped into 2 types by the PSQI score:good sleepers (0–4 points) and poor sleepers (>4 points).12
Dry Eye Symptoms
The ocular surface disease index (OSDI) questionnaire is a validated dry eye questionnaire, which measures the severity, symptoms, functional problems, and environmental triggers of dry eye in the past week. It provides a rapid assessment of the discomfort symptoms, which are consistent with dry eye severity and their effect on the visual function. The OSDI contains 12 items, with each item scored 0 to 4. The final score of the OSDI is the sum of the scores of all questions answered multiplied by 25, and then divided by the total number of questions answered. Participants were grouped into 4 categories by the OSDI score: normal (0–12 points), mild dry eye symptoms (13–22 points), moderate dry eye symptoms (23–32 points), and severe dry eye symptoms (33–100 points).13
Statistical Analysis
All statistical analyses were performed using SPSS V.25.0 (SPSS, Chicago, IL) statistical package. The proportion of subjects with different severities of dry eye, different sleep quality and different circadian typology in the study population was expressed by N (%), and the comparison among groups was conducted by Chi-squared test. The total scores of OSDI and PSQI in M-Type, N-Type and E-Type were described as means ± standard deviation (SD). The comparison of the severity of dry eye symptoms among the three groups was conducted by one-way ANOVA, and the pairwise comparison between groups was analyzed by LSD-t or Tamhane’s T2 test. Multiple-ordinal logistic regression was used to analyze the effect of different factors on the severity of dry eye. A p-value lower than 0.05 was considered statistically significant in all analyses above.
Results
The occurrence rate of poor sleep quality (PSQI>5) and symptomatic dry eye (OSDI > 13) in college students were 53.2% and 40.2%, respectively. The dominant CT type in college students was N-Type (50.9%), followed by M-Type (34.6%), and E-Type were the least (14.5%). The distribution of the CT differed significantly among the college students with different dry eye severities (χ2 = 59.44, P = 0. 000), and E-type was associated with the most severe dry eye symptoms. In addition, the distribution of the CT also differed significantly among the college students with different sleep quality (χ2 = 20.25, P = 0. 000), and the college students with poor sleep quality was more likely to be E-type. There was no significant difference in CT distribution between different gender (χ2 = 2.56, P = 0.279) or different degrees of dry eye awareness (χ2 = 2.10, P = 0.351) (Table 1).
The mean OSDI and PSQI scores of college students with different chronotypes were significantly different (F = 22.14, P = 0.000; F = 15.21, P = 0.000; respectively). E-type scored the highest, followed by N-type, and M-type was the lowest for both scores (Table 2).
 |
Table 2 Differences in PSQI and OSDI Scores of Different Circadian Typology |
The CT was an independent risk factor for the development of dry eye. The risk of E-Type was 6.99 times higher than that of M-Type (P = 0.000), and the risk of N-types was 3.23 times higher than that of M-Type (P = 0.000). Sleep quality was also an independent risk factor for dry eye (P = 0.000). Gender and awareness of dry eye were not risk factors for dry eye (Table 3).
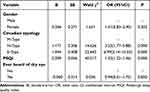 |
Table 3 Multivariate Logistic Regression of Potential Predictive Factors of Dry Eye Symptom |
Discussion
The study on circadian rhythm has made rapid progress in the past 20 years, and the difference between M-Type and E-Type in the CT can be reflected by personality characteristics, habits and lifestyle.8 Adolescence is the critical period when CT shifts from M-Type to a more pronounced E-Type.14,15 Compared with pre-adolescence children, adolescents tend to stay up late, get up later in the morning and sleep longer on weekends.16 Delayed sleep-wake phase disorder caused by circadian rhythm disorder accounts for 10% of patients with chronic insomnia, and is especially common in adolescents, with an incidence of 7%-16%.17 Therefore, it is particularly important to pay attention to adolescents with E-type. A cross-sectional study involving 79,866 subjects showed that dry eye was particularly common among people aged 20–30 with mental illness, sleep apnea, depression and other risk factors for dry eye.18 Our study showed that the occurrence rate of symptomatic dry eye (OSDI > 13) was 40.2% in college students. Most students were N-Type (50.9%), followed by M-Type (34.6%) and then E-Type (14.5%). The severity of dry eye symptoms (OSDI score) and sleep quality (PSQI score) were associated with different chronotypes. The more the circadian preference tended to be E-type, the worse the sleep quality and the more serious dry eye symptoms would appear.
Impaired light hygiene may be a relevant factor in the development of dry eye and sleep disturbance. Compromised light hygiene, as due to decreased time outdoors, and increased screen time in the evening, drives circadian phase delay and later sleep, decreasing sleep quality.19,20 Ishizawa et al21 have found that the proportion of deep sleep was significantly reduced in the blue light exposure group (P < 0.01), suggesting that blue light exposure affects sleep quality by decreasing the proportion of deep sleep. Saxvig et al22 conducted a large cross-sectional study in 3920 high school students between 16 and 17 years old and found that E-type individuals used electronic media more in bed compared with other chronotypes. A long-time video terminal use will shorten the tear film breakup time, resulting in or aggravating the dry eye.23 The similar circadian changes can also be linked with the decreased light perception due to certain eye disease that can be facilitated in individuals with the certain gene polymorphisms, eg, melatonin receptor, MTNR1B.24–26 In addition, poor light hygiene can be linked with unhealthy diet patterns and vitamin D deficiency that are also linked with dry eye risks.27
Circadian rhythm and sleep homeostasis interact precisely with each other to determine the sleep/wake times. And the mismatch of them can lead to sleep deprivation and sleep disorders, which may be a risk factor for dry eye. Previous studies have shown that compared with M-type, E-type is more likely to have difficulty falling asleep, have reduced sleep time and sleep efficiency, and have nightmares, insomnia and other sleep quality deterioration,28–30 which is consistent with our results. E-type shows more severe dry eye symptoms, which may be related to sleep deprivation. Hakki Onen et al31 found that rapid eye movement sleep deprivation induced a significant increase in rats’ responses to harmful mechanical, thermal and electrical stimuli. In a cross-sectional study, it was proposed that shortened sleep time could be an independent risk factor for dry eye with water deficiency, and a long-time use of video terminals and excessive pressure were risk factors for dry eye with excessive evaporation.4 A study conducted by Vitale et al32 in college students showed that the sleep quality of E-type was lower than that of M-type on weekdays, while the sleep quality and quantity of E-type reached the same level with other chronotypes on weekends. Their result might be related to the fact that the fixed study schedule of school is not synchronized with the students’ individual chronotype.33 E-type individuals may accumulate sleep deprivation during the weekdays and then recover from it during their “free days” on weekends. This “social jet lag” is common in our current society and has been confirmed to be linked to depression.34
Previous studies have shown that compared with M-type college students, E-type was not only characterized by poor sleep quality, but also by excessive anxiety and higher susceptibility to mental diseases. In addition, depression, mood disorders, and anxiety symptoms are also correlated with the severity of dry eye symptoms.35–37 Serotonin level affects the regulation of circadian preference,38 and is also associated with depression caused by abnormal rhythm, which means that it may play a role in the association between dry eye and chronotypes. Serotonin is a neurotransmitter known to be involved in nociceptor sensitization and is present in human tears.39 Elevated serotonin level is reported to be associated with signs and symptoms of dry eye disease, and the concentration of serotonin level is higher in tears of patients with dry eye symptoms and reduced tear secretion.39
Our study has several limitations. First, we investigated the relationship between dry eye symptom scores and the chronotypes in the population of college students. These participants may have different characteristics, such as specific family background, economic level and control over their daily work and rest time. Second, the signs of dry eyes in the students were not examined, and these variables will be further evaluated in our future studies.
Despite these limitations, the current results are instructive, and they indicate that optimization of students’ schedules and adherence to personal circadian preference can avoid sleep deprivation and emotional disorders caused by disturbed circadian preference and reduce the impact of dry eye on college students. Schools should consider aligning class hours with the students’ individual chronotypes when possible. Students should also learn about their chronotype as early as possible so that they can better arrange their classes and consider taking jobs that can synchronize with their chronotype in the future to reduce the occurrence of disease. In addition, it is suggested that supportive treatment for sleep disorders as well as emotional and mental disorders may be an important means for the prevention and treatment of dry eye.
Ethics Approval and Informed Consent
The Ethical Committee of Beijing Tongren Hospital approved the study procedures. The study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; have drafted or written, or substantially revised or critically reviewed the article; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by “The Youth Beijing Scholars program”, Natural Science Foundation of China (821704052 and 8217040515).
Disclosure
The authors declare that they have no competing interests.
References
1. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.003
2. Zhang S, Hong J. Risk factors for dry eye in Mainland China: a multi-center cross-sectional hospital-based study. Ophthalmic Epidemiol. 2019;26(6):393–399. doi:10.1080/09286586.2019.1632905
3. Asiedu K, Kyei S, Boampong F. Ocansey S: symptomatic dry eye and its associated factors: a Study of University undergraduate students in Ghana. Eye Contact Lens. 2017;43(4):262–266.
4. Wolffsohn JS, Wang MTM, Vidal-Rohr M, et al. Demographic and lifestyle risk factors of dry eye disease subtypes: a cross-sectional study. Ocul Surf. 2021;21:58–63.
5. Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–19.
6. Montaruli A, Castelli L, Mulè A. Biological rhythm and chronotype: new perspectives in health. Biomolecules. 2021;11(4):487.
7. Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23(7):571–585.
8. Adan A, Archer SN, Hidalgo MP, Milia LD, Natale V, Randler C. Circadian typology: a comprehensive review. Chronobiol Int. 2012;29(9):1153–1175.
9. Randler C, Gomà-i-Freixanet M, Muro A, Knauber C, Adan A. Do different circadian typology measures modulate their relationship with personality? A test using the alternative five factor model. Chronobiol Int. 2015;32(2):281–288.
10. Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:2.
11. Montaruli A, Galasso L, Carandente F, Vitale JA, Roveda E, Caumo A. If the Morning-Evening Questionnaire (MEQ) is able to predict the actigraphy-based acrophase, how does its reduced, five-item version (rMEQ) perform? Chronobiol Int. 2017;34(4):443–444. doi:10.1080/07420528.2017.1306708
12. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
13. Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–621. doi:10.1001/archopht.118.5.615
14. Borisenkov MF, Perminova EV, Kosova AL. Chronotype, sleep length, and school achievement of 11- to 23-year-old students in Northern European Russia. Chronobiol Int. 2010;27(6):1259–1270. doi:10.3109/07420528.2010.487624
15. Tonetti L, Fabbri M, Natale V. Sex difference in sleep-time preference and sleep need: a cross-sectional survey among Italian pre-adolescents, adolescents, and adults. Chronobiol Int. 2008;25(5):745–759. doi:10.1080/07420520802394191
16. Giannotti F, Cortesi F, Sebastiani T, Vagnoni C. Sleeping habits in Italian children adolescents. Sleep Biol Rhythms. 2005;3(1):15–21. doi:10.1111/j.1479-8425.2005.00155.x
17. Cartwright RD. Alcohol and NREM parasomnias: evidence versus opinions in the international classification of sleep disorders, 3rd edition. J Clin Sleep Med. 2014;10(9):1039–1040. doi:10.5664/jcsm.4050
18. Vehof J, Snieder H, Jansonius N, Hammond CJ. Prevalence and risk factors of dry eye in 79,866 participants of the population-based lifelines cohort study in the Netherlands. Ocul Surf. 2021;19:83–93. doi:10.1016/j.jtos.2020.04.005
19. Korman M, Tkachev V, Reis C, et al. Outdoor daylight exposure and longer sleep promote wellbeing under COVID-19 mandated restrictions. J Sleep Res. 2022;31(2):e13471. doi:10.1111/jsr.13471
20. Gupta PC, Rana M, Ratti M, et al. Association of screen time, quality of sleep and dry eye in college-going women of Northern India. Indian J Ophthalmol. 2022;70(1):51–58. doi:10.4103/ijo.IJO_1691_21
21. Ishizawa M, Uchiumi T, Takahata M, Yamaki M, Sato T. Effects of pre-bedtime blue-light exposure on ratio of deep sleep in healthy young men. Sleep Med. 2021;84:303–307. doi:10.1016/j.sleep.2021.05.046
22. Saxvig IW, Evanger LN, Pallesen S, et al. Circadian typology and implications for adolescent sleep health. Results from a large, cross-sectional, school-based study. Sleep Med. 2021;83:63–70. doi:10.1016/j.sleep.2021.04.020
23. Tsubota K, Yokoi N, Shimazaki J, et al. New perspectives on dry eye definition and diagnosis: a consensus report by the Asia dry eye society. Ocul Surf. 2017;15(1):65–76. doi:10.1016/j.jtos.2016.09.003
24. Gubin D, Neroev V, Malishevskaya T, et al. Melatonin mitigates disrupted circadian rhythms, lowers intraocular pressure, and improves retinal ganglion cells function in glaucoma. J Pineal Res. 2021;70(4):e12730. doi:10.1111/jpi.12730
25. Tosini G, Baba K, Hwang CK, Iuvone PM. Melatonin: an underappreciated player in retinal physiology and pathophysiology. Exp Eye Res. 2012;103:82–89.
26. Martínez-águila A, Martín-Gil A, Carpena-Torres C, Pastrana C, Carracedo G. Influence of circadian rhythm in the eye: significance of melatonin in glaucoma. Biomolecules. 2021;11:3.
27. Galor A, Gardener H, Pouyeh B, Feuer W, Florez H. Effect of a Mediterranean dietary pattern and vitamin D levels on dry eye syndrome. Cornea. 2014;33(5):437–441.
28. Li SX, Chan NY, Man YMW. Eveningness chronotype, insomnia symptoms, and emotional and behavioural problems in adolescents. Sleep Med. 2018;47:93–99.
29. Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Lahti T, Partonen T. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol Int. 2012;29(3):311–317.
30. Lehnkering H, Siegmund R. Influence of chronotype, season, and sex of subject on sleep behavior of young adults. Chronobiol Int. 2007;24(5):875–888.
31. Hakki Onen S, Alloui A, Jourdan D, Eschalier A, Dubray C. Effects of rapid eye movement (REM) sleep deprivation on pain sensitivity in the rat. Brain Res. 2001;900(2):261–267.
32. Vitale JA, Roveda E, Montaruli A, et al. Chronotype influences activity circadian rhythm and sleep: differences in sleep quality between weekdays and weekend. Chronobiol Int. 2015;32(3):405–415.
33. Sun J, Chen M, Cai W, et al. Chronotype: implications for sleep quality in medical students. Chronobiol Int. 2019;36(8):1115–1123.
34. Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–943.
35. Ayaki M, Kawashima M, Negishi K, Tsubota K. High prevalence of sleep and mood disorders in dry eye patients: survey of 1000 eye clinic visitors. Neuropsychiatr Dis Treat. 2015;11:889–894.
36. Hallak JA, Tibrewal S, Jain S. Depressive symptoms in patients with dry eye disease: a case-control study using the beck depression inventory. Cornea. 2015;34(12):1545–1550.
37. Labbé A, Wang YX, Jie Y, Baudouin C, Jonas JB, Xu L. Dry eye disease, dry eye symptoms and depression: the Beijing Eye Study. Br J Ophthalmol. 2013;97(11):1399–1403.
38. Ciarleglio CM, Resuehr HES, McMahon DG. Interactions of the serotonin and circadian systems: nature and nurture in rhythms and blues. Neuroscience. 2011;197:8–16.
39. Chhadva P, Lee T, Sarantopoulos CD, et al. Human tear serotonin levels correlate with symptoms and signs of dry eye. Ophthalmology. 2015;122(8):1675–1680.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
