Back to Journals » International Journal of General Medicine » Volume 14
The Prognostic Value of the Serum Levels of Brain Natriuretic Peptide, Troponin I, and D-Dimer, in Addition to the Neutrophil-to-Lymphocyte Ratio, for the Disease Evaluation of Patients with Acute Pulmonary Embolism
Authors Bi W, Liang S, He Z, Jin Y, Lang Z, Liu H, Wang Y, Li S
Received 6 November 2020
Accepted for publication 31 December 2020
Published 28 January 2021 Volume 2021:14 Pages 303—308
DOI https://doi.org/10.2147/IJGM.S288975
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wenmiao Bi,1,* Shaoqing Liang,2,* Zhihong He,2 Ying Jin,2 Zhe Lang,2 Hongjuan Liu,2 Yi Wang,2 Shuhong Li2
1Department of Respiratory Medicine, Shijiazhuang People’s Hospital, Shijiazhuang, Hebei 050031, People’s Republic of China; 2Department of Emergency Medicine, Shijiazhuang People’s Hospital, Shijiazhuang, Hebei 050031, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhihong He; Ying Jin
Department of Emergency Medicine, Shijiazhuang People’s Hospital, 365 Jianhuanan Street, Yuhua District, Shijiazhuang City, Hebei 050031, People’s Republic of China
Tel/Fax +86 311-69089120
Email [email protected]; [email protected]
Objective: The present study aims to investigate whether the serum levels of brain natriuretic peptide (BNP), troponin I (TnI), and D-dimer, in addition to the neutrophil-to-lymphocyte ratio (NLR), can be used to determine the prognosis of patients with acute pulmonary embolism (APE).
Methods: Data were collected from 72 patients that were diagnosed with APE in our hospital from January 2015 to December 2018. These patients were divided into three groups: a high-risk group (n = 10), a moderate-risk group (n = 33), and a low-risk group (n = 29). The serum levels of BNP, TnI, and D-dimer were determined, and the NLR was measured. The receiver operating characteristic (ROC) curve was used to analyze the diagnostic value of the single and combined detection of BNP, TnI, and D-dimer, and the NLR was used to determine the prognosis of patients with APE.
Results: The serum levels of BNP, TnI, and D-dimer were significantly higher in the high-risk group than they were in the moderate-risk and low-risk groups (P < 0.05). The serum levels of BNP, TnI, and D-dimer were also significantly higher in the moderate-risk group than they were in the low-risk group (P < 0.05). The serum levels of BNP, TnI, and D-dimer, as well as the NLR, were all significantly higher in the death group than they were in the survival group (P < 0.05). For the combined detection of the four indices, the area under the ROC curve was 0.92, the sensitivity was 0.889, and the specificity was 0.904; each of these values was higher than the corresponding values of single detection.
Conclusion: In patients with APE, higher serum levels of BNP, TnI, D-dimer and NLR are associated with a higher risk stratification, greater severity of disease, and an increased risk of death.
Keywords: brain natriuretic peptide, troponin I, D-dimer, neutrophil-to-lymphocyte ratio, pulmonary thromboembolism, acute pulmonary embolism
Introduction
Pulmonary thromboembolism, a clinical and pathophysiological disorder of the pulmonary circulation, occurs when an endogenous or exogenous embolus blocks the trunk or branch of a pulmonary artery. It is associated with high clinical mortality. Previous work has shown that the incidence and mortality of acute pulmonary embolism (APE) are high in China.1 Because APE is often misdiagnosed, it is of great clinical significance for patients with APE to obtain a definite diagnosis and assessment as soon as possible. Although right heart catheterization and pulmonary angiography can be used to determine the location of the embolus and the condition of the collateral circulation, these procedures are expensive, difficult, and associated with poor compliance in patients. In the present study, the serum levels of brain natriuretic peptide (BNP), troponin I (TnI), and D-dimer, in addition to the neutrophil-to-lymphocyte ratio (NLR), were measured in patients with APE at our hospital. The aim was to explore the correlation of the severity of APE with these three serum levels and to determine whether the combined detection of these indices with the NLR can aid the evaluation of prognosis and, in doing so, provide a reference for the clinical treatment of APE.
Materials and Methods
Study Objects
The study enrolled 72 patients that were treated for APE in our hospital from January 2015 to December 2018. The patient group included 31 males and 41 females. The inclusion criteria were as follows: (1) The diagnosis was in accordance with the relevant diagnostic criteria for pulmonary embolism as formulated by the respiratory branch of the Chinese Medical Association,2 and (2) the diagnosis was confirmed by a computed tomography pulmonary angiogram and pulmonary angiography. The exclusion criteria were as follows: (1) patients with coronary atherosclerotic heart disease, left ventricular dysfunction, myocarditis, myocardial disease, chronic pulmonary hypertension, or chronic obstructive pulmonary disease; (2) patients with hematological diseases; (3) patients with obvious symptoms of infection; (4) patients that had used immunosuppressants or steroids within the previous two weeks; and (5) patients with severe hepatic or renal disease.
In accordance with the standards of the cardiovascular branch of the Chinese Medical Association, patients were classified as high-risk (n = 10) if they exhibited shock or persistent hypotension with hemodynamic instability. Patients were classified as moderate-risk (n = 33) if they had right ventricular dysfunction, an elevated serum level of TnI, or both. Patients were classified as low-risk (n = 29) if they had normal right ventricular function, a normal serum level of TnI, or both.
Detection Methods
Blood samples were collected from the elbow vein at admission to detect the serum levels of BNP, TnI, and D-dimer. The levels of BNP and TnI were measured using chemiluminescence with the Access 2 immunoassay system (Beckman Coulter, Inc., Fullerton, CA, USA). The level of D-dimer was measured using transmission immunoturbidimetry with the ACL TOP 700 hemostasis testing system (Instrumentation Laboratory, Bedford, CA, USA). The levels of neutrophils and lymphocytes were measured using the LH 750 hematology analyzer (Beckman Coulter, Inc., Fullerton, CA, USA). The normal reference range of BNP was <250 μg/mL, the normal reference range of TnI was 0–0.1 ng/mL, and the normal reference range of D-dimer was 0–300 ng/mL.
Statistical Analysis
SPSS 19.0 software (IBM Corp., Armonk, NY, USA) was used for data analysis. The measurement data were expressed as mean ± standard deviation (x̄ ± s). A χ2 test was used to compare the enumeration data between groups, and a one-way ANOVA was used for comparison within groups. The ROC curve was used to analyze the diagnostic value of the single and combined detection of BNP, TnI, D-dimer, and the NLR for determining the prognosis of patients with APE. P < 0.05 was considered statistically significant.
Results
Comparison of the General Characteristics of the Three Groups
The general characteristics of the patients in the three groups were compared. As shown in Table 1, there was no statistical difference in the age or gender makeup of the three groups (P > 0.05).
 |
Table 1 Comparison of the General Characteristics of the Three Groups |
Comparison of the Serum Levels of BNP, TnI, and D-Dimer in the Three Groups
In patients with APE, the serum levels of BNP, TnI, and D-dimer in the high-risk group were 418.23 ± 29.68, 2.69 ± 0.7730, 1327.89 ± 463.62, respectively. The serum levels of BNP, TnI, and D-dimer in the moderate risk group were 287.35 ± 46.74, 1.71 ± 0.2961, 876.45 ± 305.63, respectively. The serum levels of BNP, TnI, and D-dimer in the low-risk group were 119.10 ± 16.41, 0.04 ± 0.0118, 643.00 ± 291.83, respectively. In the high-risk and moderate-risk groups, the serum levels of BNP, TnI, and D-dimer were significantly higher than they were in the low-risk group (P < 0.05). In addition, the levels of BNP, TnI, and D-dimer were significantly higher in the high-risk group than they were in the moderate-risk group (P < 0.05). The results are presented in Table 2. These results suggest that higher serum levels of BNP, TnI, and D-dimer are associated with a higher risk stratification and a greater severity of disease.
 |
Table 2 Comparison of the Serum Levels of BNP, TnI, and D-Dimer in the Three Groups ( |
Comparison of the Serum Levels of BNP, TnI, and D-Dimer Combined with the NLR in Patients with Different Prognoses
The serum levels of BNP, TnI, D-dimer and NLR in the death group were significantly higher than those in the survival group (P < 0.05). The results are presented in Table 3.
 |
Table 3 Comparison of the Serum Levels of BNP, TnI, and D-Dimer and the NLR in Patients with Different Prognoses |
The Diagnostic Value of the Single and Combined Detection of BNP, TnI, D-Dimer, and the NLR for Determining Patient Prognosis
As shown in Table 4, the area under the ROC curve (AUC) for BNP, TnI and D-dimer were between 0.7 and 0.85, the serum levels of these three indices were of certain value for the assessment and prognosis of acute pulmonary embolism. The AUC for NLR was 0.861 (greater than 0.85), the sensitivity was 0.779, and the specificity was 0.890. Compared with BNP, TnI and D-dimer, NLR has a higher value in the assessment and prognosis of acute pulmonary embolism. For the combined detection of the four indices, the AUC was 0.92, the sensitivity was 0.889, and the specificity was 0.904. Each of these values was higher than the corresponding values of single detection.
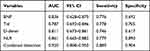 |
Table 4 The Diagnostic Value of the Single and Combined Detection of BNP, TnI, D-Dimer, and the NLR for Determining Patient Prognosis |
Discussion
As a disease with a high incidence and mortality, pulmonary embolism is a serious health threat. Epidemiological studies conducted outside of China have found the incidence of pulmonary embolism to be 122–146 cases per 10 million individuals.3 No precise epidemiological data have been collected in China, but the number of reported cases has gradually increased in recent years. While individuals with mild cases may experience only transient dyspnea or no symptoms at all, cardiogenic shock or even sudden death is possible in severe cases. Unfortunately, the rates of missed diagnosis and misdiagnosis are very high in the early stage of the disease. However, mortality can be significantly reduced with a timely diagnosis and effective treatment according to risk stratification.
BNP is a neuropeptide active substance that is primarily produced by ventricular myocardial cells. The serum level of BNP is low in healthy individuals, but a large amount of BNP can be secreted into the blood when pressure increases and the ventricular myocytes are stretched to an abnormal degree; thus, an elevated level of BNP can indicate ventricular dysfunction and reflect the degree of injury to the myocardial cells.4 When a pulmonary embolism occurs, the mechanical blockage that it causes can reduce the effective pulmonary vascular bed, increase the resistance of pulmonary circulation, and lead to pulmonary hypertension. This results in increased tension in the right ventricular wall and, in turn, causes the synthesis and secretion of BNP to increase.5
Because the serum level of BNP is a sensitive indicator of an increased ventricular load, an increase in the level of BNP may appear earlier than other clinical symptoms; as a result, the level of BNP is an early indicator of the risk and degree of right ventricular dysfunction and pulmonary embolism.6 In line with other studies conducted in China,7 the present study found that the low, moderate, and high-risk groups of patients with APE had significantly different serum levels of BNP (P < 0.05). In addition, the serum level of BNP was significantly higher in patients in the high-risk group than it was in either the low-risk or moderate-risk groups (P < 0.05). Furthermore, with the progression from low-risk to high-risk, the level of BNP increased significantly. This suggests that the serum level of BNP is positively correlated with the severity of APE. The reason for this correlation might be that high-risk patients with APE have a wider range of embolism, which causes more obvious hypoxemia. The aggravation of pulmonary hypertension would increase the right heart load and cause the right ventricular myocardial cells to stretch abnormally, resulting in a significant increase in the serum level of BNP. Thus, BNP can be used as an index of the severity in APE.
As a specific marker of myocardial injury, TnI has a high sensitivity and specificity for myocardial injury.8 An increase in the level of TnI indicates the necrosis of the myocardium at a microscopic level, a process that is often used to diagnose acute myocardial infarction. Previous work has shown that both pulmonary artery and right ventricular pressure may rise sharply as a result of the pulmonary vascular blockage and contraction that occur during APE. This sudden rise can lead to right ventricular dilatation, right ventricular myocardial ischemia, and even myocardial infarction, which causes the level of TnI to increase.9 In addition, pulmonary embolism causes a sharp increase in tension in the right ventricle and pericardium, which can squeeze the coronary artery and lead to partial myocardial ischemia and the injury and necrosis of myocardial cells; these processes also lead to the release of TnI.10 Thus, a higher serum level of TnI in patients with APE indicates an impairment of the right ventricular function, which is associated with a marked increase in the risk of right heart failure and cardiogenic shock. Walter et al11 found that the serum level of TnI increased in patients with APE with right ventricular dysfunction, where the magnitude of this increase was positively correlated with the risk of death. As a result, patients with APE and an elevated level of TnI have a higher risk of death even if their hemodynamics remain stable.12,13 The present study found that the serum level of TnI was significantly higher in the high-risk group than it was in either the low-risk or moderate-risk groups (P < 0.05), where a higher level of TnI corresponded to more severe APE. Therefore, if patients with APE are found to have a significantly elevated level of TnI, then they may have a right ventricular myocardial injury, which is a serious condition with a high mortality rate.
D-dimer is derived from the cross-linked fibrin clot that is dissolved by plasmin. Although the serum level of D-dimer has long been known to have diagnostic value in cases of pulmonary embolism, the level of D-dimer can also be elevated in patients with thrombosis, which may occur as a result of surgery, trauma, infection, hepatic disease, pregnancy, convulsion, heart disease, and certain cancers. Whereas it has generally been suggested that D-dimer has a high negative predictive value for APE,14,15 the present study demonstrates that there are significant differences in the serum levels of D-dimer in the low, moderate, and high-risk groups, thus concluding that the level of D-dimer is positively correlated with the severity of APE. This result is in line with the results of another study conducted in China.16 In addition, the level of D-dimer was significantly higher in the death group than it was in the survival group, which suggests that a higher level of D-dimer corresponds to more severe APE and a higher risk of death.
Some studies also indicate that pulmonary embolism in patients with plasma osmolality is higher than normal. The change in plasma osmolality may increase the activity of the immune system with proinflammatory effects.17 The development of thrombosis is closely associated with inflammation,18 which can stimulate the production of neutrophils and accelerate the apoptosis of lymphocytes. The status of activation of neutrophil refers to the process by which neutrophils adhere to the vascular endothelium through adhesion molecules on the cell surface. This results in neutrophil accumulation in the microvasculature and the release of lysosomal enzymes, histamine, leukotrienes, and other active substances, as well as cytokines, such as IL-6, IL-10, and TNF. These active substances and cytokines can damage endothelial cells and the vessel wall and promote vasoconstriction, platelet adhesion and aggregation, finally inducing thrombosis.
Neutrophils produce oxygen free radicals, elastase, myeloperoxidase, and other inflammatory mediators. High levels of inflammatory mediators cause tissue injury and release tissue factors, leading to the onset of embolism.19 The NLR represents the balance between neutrophils and lymphocytes, and a high NLR indicates a high degree of inflammation.20 A high NLR has been proposed to be an inflammatory index that can predict the short-term mortality of patients with APE.21–23 The present study shows that the NLR of the patients in the death group is higher than it is in the survival group. This result suggests that the NLR can be used as a risk predictor of in-hospital mortality in patients with APE, a conclusion that would be consistent with previous studies.24 The researchers found that PNI, calculated based on serum albumin level and lymphocyte count, is an independent prognostic factor for survival of patients with APE.25 Therefore, whether NLR can be used as a long-term prognostic factor for patients with APE remains to be further researched.
The present study has found that the serum levels of BNP, TnI, and D-dimer and the NLR were all higher in the death group than they were in the survival group. This suggests that these four indices can be used as indicators to evaluate the prognosis of patients with APE. In addition, the results of analysis using the ROC curve demonstrates that the AUC, sensitivity, and specificity of the combined detection of the serum levels of BNP, TnI, and D-dimer and the NLR were higher than they were for single detection. This suggests that the combined detection of the four indices may improve the prognostic evaluation of patients with APE. However, the present study has certain limitations: For some patients, it was difficult to distinguish between pulmonary embolism alone and pulmonary embolism complicated by infection; this has the potential to result in biased results. Furthermore, because it is a single-center, retrospective case-control study, the sample size is limited. Also, the strict inclusion and exclusion criteria of this study, as well as the difficulty in clinical case collection, has further limited the sample size. However, the results of our study are consistent with results reported in the published literature. Thus, though small sample size is a major limitation, our study still has good value in prognosis of patients with APE. We will continue to collect related cases and further expand the study samples.
In conclusion, the serum levels of BNP, TnI, and D-dimer in patients with APE can predict the severity of APE. In addition, the combined detection of the serum levels of BNP, TnI, and D-dimer and the NLR can improve the evaluation of the clinical prognosis of patients with pulmonary embolism.
Data Sharing Statement
We declared that materials described in the manuscript, including all relevant raw data, will be freely available to any scientist wishing to use them for non-commercial purposes, without breaching participant confidentiality.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Shijiazhuang people’s Hospital. This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Consent for Publication
All participants signed a document of informed consent.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
No external funding received to conduct this study.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Fang JJ, Li B, He XJ, et al. Significance of plasma troponin I, B-type natriuretic peptide and D-dimer in prognosis evaluation of acute pulmonary embolism. Chin J Respir Crit Care Med. 2012;11(1):61–64.
2. Respiratory disease branch of Chinese Medical Association. Guidelines for diagnosis and treatment of pulmonary thromboembolism (draft). Zhonghua Yi Xue Hui. 2001;24(5):259–264.
3. Daquarti G, March Vecchio N, Mitrione CS. High-sensitivity troponin and right ventricular function in acute pulmonary embolism. Am J Emerg Med. 2016;34(8):1579–1582. doi:10.1016/j.ajem.2016.05.071.
4. Zhou ZL, Ji QY, Ma X, Jin KP. Relationship between plasma brain natriuretic peptide and right ventricular function in patients with acute pulmonary embolism and its prognostic value. Zhejiang Med J. 2013;35(15):1432–1434.
5. Chen YX, Li M, Chen XX, Zhang YJ. Clinical significance of plasma N-terminal pro brain natriuretic peptide, D-dimer and fibrinogen in patients with chronic obstructive pulmonary disease complicated with pulmonary embolism. Hainan Med J. 2017;28(1):23–25.
6. Ma T, Yan J. Clinical value of plasma N-terminal pro-B-type natriuretic peptide and cardiac troponin I in patients with acute pulmonary embolism complicated with right ventricular dysfunction. Chin Circ J. 2015;30(5):446–448.
7. Wei Q, Wang CM. Clinical value of plasma B-type natriuretic peptide combined with D-dimer in evaluating prognosis of pulmonary embolism. J Med Res. 2015;44(11):143–146.
8. Chen J, Jiang B, Cui TP. Clinical value of detection of serum homocysteine and high sensitivity C-reactive protein in patients with pulmonary embolism. Chin J Thromb Haemost. 2014;20(2):74–75.
9. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632–1636. doi:10.1016/s0735-1097(00)00905-0
10. Giannitsis E, Müller-Bardorff M, Kurowski V, et al. Independent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolism. Circulation. 2000;102(2):211–217. doi:10.1161/01.cir.102.2.211.
11. Walter T, Apfaltrer P, Weilbacher F, et al. Predictive value of high-sensitivity troponin I and D-dimer assays for adverse outcome in patients with acute pulmonary embolism. Exp Ther Med. 2013;5(2):586–590. doi:10.3892/etm.2012.825
12. Wu XH, Liu DM, Xu ZS. Diagnostic and prognostic value of troponin I in patients with acute pulmonary embolism. Prog Cardiovasc Dis. 2012;33(4):507–510.
13. Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. 2008;117(1):93–102. doi:10.1161/CIRCULATIONAHA.107.709204
14. Wang RS. Analysis of plasma D-dimer in patients with pulmonary embolism. China Pract Med. 2009;4(4):100–101.
15. Wang MN, Wu XF, Huang DQ, Guo KP, Wu SL. Diagnostic value of combined detection of plasma D-dimer and cTnI in acute pulmonary embolism. China Foreign Med Treat. 2012;2:1–2.
16. Jin BX, He TH, Zhang J. The value of D-dimer detection in the diagnosis of pulmonary embolism. Chin J Gerontol. 2012;32(14):3052–3053.
17. Ahmet Ö, Çınar T, Hayıroğlu Mİ, Avşar Ş, Keskin M, Orhan AL. The predictive value of plasma osmolality for in-hospital mortality in patients with acute pulmonary embolism. Clin Respir J. 2019;13(3):174–183. doi:10.1111/crj.13001.
18. Zagorski J, Kline JA. Differential effect of mild and severe pulmonary embolism on the rat lung transcriptome. Respir Res. 2016;17(1):86. doi:10.1186/s12931-016-0405-9
19. Balta S, Demırkol S, Kucuk U. The platelet lymphocyte ratio may be useful inflammatory indicator in clinical practice. Hemodial Int. 2013;17(4):668–669. doi:10.1111/hdi.12058
20. Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. Neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Int Arch Med. 2012;5(1):2. doi:10.1186/1755-7682-5-2
21. Kayrak M, Erdoğan HI, Solak Y, et al. Prognostic value of neutrophil to lymphocyte ratio in patients with acute pulmonary embolism: a restrospective study. Heart Lung Circ. 2014;23(1):56–62. doi:10.1016/j.hlc.2013.06.004
22. Ma Y, Mao Y, He X, Sun Y, Huang S, Qiu J. The values of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in predicting 30 day mortality in patients with acute pulmonary embolism. BMC Cardiovasc Disord. 2016;16(1):123. doi:10.1186/s12872-016-0304-5
23. Karataş MB, İpek G, Onuk T, et al. Assessment of prognostic value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in patients with pulmonary embolism. Acta Cardiol Sin. 2016;32(3):313–320. doi:10.6515/acs20151013a
24. Bakirci EM, Topcu S, Kalkan K, et al. The role of the nonspecific inflammatory markers in determining the anatomic extent of venous thromboembolism. Clin Appl Thromb Hemost. 2015;21(2):181–185. doi:10.1177/1076029613494469
25. Mert IH, Muhammed K, Keskin T. A novel independent survival predictor in pulmonary embolism: prognostic nutritional index. Clin Appl Thromb Hemost. 2018;24(4):633–639. doi:10.1177/1076029617703482.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

