Back to Journals » Cancer Management and Research » Volume 11
The prognostic value of pretreatment inflammatory biomarkers in primary angiosarcoma
Authors Wang M, Wu S, Tong A, Cui X, Ma X
Received 12 June 2019
Accepted for publication 1 August 2019
Published 22 August 2019 Volume 2019:11 Pages 7981—7989
DOI https://doi.org/10.2147/CMAR.S219237
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chien-Feng Li
Manni Wang, Shuang Wu, An Tong, Xiwei Cui, Xuelei Ma
Department of Biotherapy, Cancer Center, State Key Laboratory of Biotherapy, West China Hospital, Sichuan University and Collaborative Innovation Center for Biotherapy, Chengdu, People’s Republic of China
Correspondence: Xuelei Ma
Department of Biotherapy, Cancer Center, State Key Laboratory of Biotherapy, West China Hospital, Sichuan University and Collaborative Innovation Center for Biotherapy, No. 37, Guoxue Alley, Chengdu 610041, People’s Republic of China
Email [email protected]
Background: Recent studies have suggested a significant relationship between inflammatory indexes such as the neutrophil-to-lymphocyte ratio (NLR) and survival outcomes in various cancers. The aim of the present study was to evaluate the prognostic value of 6 pretreatment inflammatory markers in patients with primary angiosarcoma (AS) which is a rare and highly malignant type of soft tissue sarcoma.
Methods: Fifty-six patients diagnosed with primary AS at West China Hospital between August 2009 and July 2016 were retrospectively enrolled. The value of each biomarker was calculated for its correlation with patients’ overall survival.
Results: The low tumor grade, tumor size <5 cm, metastatic status, surgical treatment and low level of monocyte-to-lymphocyte ratio, NLR and lactate dehydrogenase (LDH) were correlated with better survival outcome in univariate analyses. In multivariate analyses, high levels of NLR (HR 2.673, 95% CI 1.253–5.703, p=0.011) and LDH (HR 2.964, 95% CI 1.464–5.998, p=0.003) were selected as independent prognostic factors.
Conclusion: This study identifies the elevated pretreatment levels of NLR and LDH as prognostic markers in patients with primary AS.
Keywords: inflammatory biomarker, prognosis, angiosarcoma
Background
Angiosarcoma (AS) is a rare and highly malignant type of soft tissue sarcoma derived from vascular endothelial cells. It accounts for only 1–4% of all soft tissue sarcomas.1,2 Clinical symptoms vary considerably based on the primary sites including the skin, soft tissue and viscera. For example, patients with cutaneous ASs usually present bruise-like patches, violaceous nodules or plaques,3 whereas symptoms of visceral ASs include abdominal pain, hepatosplenomegaly or anemia.4
The prognosis for primary AS is generally poor. Previous studies have addressed the poor prognosis of AS of the face and scalp (ASFS) which is a particular subgroup of sarcomas characterized by high frequencies of local recurrence or distant metastasis, with a 5-year survival rate of 11.1–53.8%.5 Due to a low rate of clinical suspicion and unusual clinical presentation, a significant portion of patients present inoperable AS or metastasis at the time of initial diagnosis.4,6,7 Surgery was considered the initial treatment, but was also observed with high rates of local recurrence.8 Although the most effective treatments for the primary AS should vary according to individuals, the multimodal treatment (surgery followed by chemotherapy and/or radiotherapy) is considered the optimal option.3,9 However, the majority of patients will ultimately develop distant metastases even after treatment, with local or systemic failure approaching 70% of all cases of complete resections.4,10–13 It was reported that the rupture of cystic metastases in the lung would cause repeated pneumothorax and hemothorax and was the major cause of death.14,15
Several tumor biomarkers such as platelet-derived growth factor receptor-β and vascular endothelial growth factor receptor-2 have been investigated about their correlations with AS prognosis.16 However, detecting these biomarkers as routine clinical tests is not feasible due to the high cost and absence of standardization system. Therefore, it is intriguing to identify a set of accessible biomarkers to predict prognosis before treatment. Recently, pretreatment systemic inflammatory indexes including neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and monocyte-to-lymphocyte ratio (MLR) have been reported to be associated with the prognosis of soft tissue sarcomas.17–19
Owing to the extreme rarity of this tumor, reports on clinicopathological features and prognostic factors of primary angiosarcoma (PAS) are limited and most of them are case reports or small case series, of which the selection bias makes the results difficult to interpret. Gen Suzuk et al have investigated the role of 3 inflammatory markers in prognosis of 17 patients with AS.20 Our study aims to identify a set of accessible biomarkers in patients’ peripheral blood and clarify their relationships with the overall survival (OS). To the best of our knowledge, this is the first study to analyze the 6 pretreatment inflammatory indexes including NLR, PLR, MLR, systemic immune-inflammation index (SII), lactate dehydrogenase (LDH) and ALP, in a relatively large clinical setting of 56 patients with this rare sarcoma.
Methods
Patients
A total number of 56 patients diagnosed with PAS at West China Hospital between August 2009 and July 2016 were retrospectively enrolled in this study from our cancer database. The median follow-up time was 18.5 (11.05–32.55) months. The end date of follow-up was May 2017 or death. Patients meeting the following criteria were included: (1) patients were pathologically confirmed of AS; (2) patients with complete clinical information; (3) inflammatory biomarkers were obtained before any treatment.
Data extraction and follow-up
The demographics, laboratory tests and pathologic reports of patients were extracted from electronic medical records. Patient characteristics included the gender, age, tumor size, tumor location and treatments. All biopsy or surgical specimens were reviewed by board-certified pathologists to determine the grade (low vs intermediate or high). The primary tumor was categorized by its location as head and neck, breast, viscera (organs and bones) and soft tissue (trunk and extremities).3 For patients with multiple primary tumors, the size of the tumor was reported from the largest lesion available from surgeries or biopsies. The platelet, lymphocyte, monocyte and neutrophil counts, LDH and ALP were obtained from the last blood test before treatment and NLR, PLR, MLR and SII were calculated, respectively. The SII was calculated using platelet counts times NLR (P × NLR). Patients were retrospectively evaluated by telephone and outpatient follow-up. The OS was selected as primary endpoints. The OS was defined as the period from the date of pathologic diagnosis to death or last follow-up. Patients that are alive without progression were recorded as censored at the end of the follow-up.
Statistical analysis
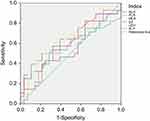
NLR, PLR, MLR, SII, LDH and ALP were calculated with receiver operating curves (ROC) to determine the optimal cutoff values and then dichotomized into 2 categories: less than, and greater than or equal to the cutoff values. Survival curves were obtained by Kaplan–Meier survival analysis and compared among groups by log-rank test. Only variables revealing significant association on univariate analyses (p<0.10) were then performed with multivariate analyses. Multivariate analyses were performed using Cox proportional hazards regression, reported with 95% CIs to estimate the association between variables and survival outcome. All the statistical analyses were performed using SPSS version 21.0, and p<0.05 was considered statistically significant in multiple cox regression analyses.
Results
Baseline characteristics
This study analyzed 56 patients pathologically confirmed of AS treated at West China Hospital between 2010 and 2017. Table 1 presents the baseline characteristics of patients such as the age and gender distribution and of their primary tumors. The median OS was 21.00 (95% CI 10.465–31.535) months. Tumors larger than 5 cm on clinical assessment accounted for 51.8% of all tumors. Furthermore, the majority (62.5%) of the tumors were classified as high grade (G3) according to pathology reports, whereas 37.5% of patients were recorded as low and medium grade (G1&G2). Sixteen patients (28.6%) were characterized as metastatic at initial diagnosis, and 40 patients (71.4%) were nonmetastatic. A total number of 22 (39.3%) tumors developed in the viscera included liver, spleen and bone. The head and neck (33.9%) was another common site for primary tumor. Six (10.7%) tumors occurred in the breast and in 9 (16.1%) cases in extremities or the trunk. Surgery was considered the first treatment option with certain indications and in this study, and most patients (67.9%) had undergone surgeries. Twenty-three patients (41.1%) received chemotherapy treatment whereas 33 patients (58.9%) did not.
 |
Table 1 Baseline characteristics of 56 patients with angiosarcoma |
Cutoff values for inflammatory indexes
Of the 6 inflammatory indexes of patients enrolled in this study, the median values of NLR, PLR, MLR and SII were 2.56 (1.80–5.22), 126 (89–192), 0.29 (0.22–0.44) and 462.5 (252.8–937.0), respectively. LDH had a median value of 169.5 (145.5–249.0) IU/L and that of ALP was 86.0 (63.3–100.0) IU/L. The ROC was used to identify optimal cutoff value for indexes. The area under curve was presented in Table 2 and Figure 1. By analyzing the specificity and sensitivity of each value, the optimal cutoff values of NLR, PLR, MLR, SII, LDH and ALP were taken as 5.22, 154, 0.38, 1048.5, 184 and 89.5, respectively. Patients were therefore dichotomized into 2 categories: less than, and greater than or equal to the cutoff values.
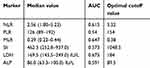 |
Table 2 Optimal cutoff values for each inflammatory marker |
Prognostic value of inflammatory indexes
The univariate analysis suggested that high levels of NLR were significantly correlated with poorer OS (p=0.001). Favorable OS was also observed in patients with lower levels of MLR (p=0.048). Compared to those with high LDH, the OS of LDH was markedly improved (37.6 months vs 12.3 months, p<0.001). Moreover, patients with high tumor grade had a poor prognosis with a median OS of 16.3 months compared with 51.7 months in patients with low & intermediate grade. While the metastatic status demonstrated significant relevance to survival in univariate analyses, with a median survival of 15.2 months in metastatic patients vs 37.6 months in nonmetastatic patients (p=0.010). The tumor size served as another potential predictor for poor prognosis with a median survival of 16.3 months in tumors ≥5 cm vs 31.5 months in tumors <5 cm. However, no significant difference in prognosis was identified between patients receiving surgery/chemotherapy or not. Similarly, age, gender, tumor location, PLR, SII and ALP were not correlated with OS. The Kaplan–Meier survival curves were also displayed to show the association of the grade, size, metastatic status, NLR, MLR, LDH and surgical treatment with patients’ survival outcomes (Figure 2).
Multivariate analysis was accordingly performed to identify any independent prognostic factors for AS. After being adjusted by other potential factors including the tumor grade, size, MLR and surgical history, high levels of pretreatment NLR (HR 2.673, 95% CI 1.253–5.703, p=0.011) and LDH (HR2.964, 95% CI 1.464–5.998, p=0.003) were proved to be independent predictors of poor survival outcomes (Table 3).
 |
Table 3 Univariate and multivariate analysis of factors associated with overall survival in patients with laryngeal cancer |
Discussion
To the best of our knowledge, this is the first study to explore the prognostic value of a set of pretreatment inflammatory indexes including NLR, PLR, MLR, SII, LDH and ALP, in a relatively large clinical setting of 56 patients with this rare sarcoma. There was only one study specifically targeting AS which evaluated the prognostic role of 3 serum markers in 17 patients with ASFS.20 The OS of AS patients at any location was relatively short21 and the major problem is the absence of treatment standards. Based on the histopathology of PAS, some studies have suggested the concomitant use of antiangiogenic agents such as bevacizumab with chemotherapy22 and that the molecular disorders like p53, PI3K, or mTOR pathways observed in PAS patients would be a future research direction.23
Consistent with previous studies,24–27 the head and neck (33.9%) and viscera (organs and bones) were two most common sites for AS. One of the previous studies suggested that breast ASs had better survival than other parts of AS,3 whereas in some other studies of breast AS,28,29 such favorable survival could not be observed. Our results demonstrated the visceral AS was associated with the worst prognosis with a median OS of 14.6 months, which is in accordance with the research of Fayette et al.4 Therefore, further studies are warranted to assess the correlation of tumor sites with AS prognosis. Interestingly, although our univariate analysis demonstrated that patients with high tumor grade had a poor prognosis with a median OS of 16.3 months compared with 51.7 months in patients with low & intermediate grade, the multivariate analysis failed to identify significant differences. This finding is in accordance with a previous study11 in 1996 which reported the association of tumor grades with survival outcomes, but only in univariate analyses. However, some studies have suggested contrary results that the grade is not a prognostic factor for PAS.30 Furthermore, the tumor size has been considered as a hallmark of AS prognosis, with previous evidence suggesting that tumor larger than 5 cm predicts poor prognosis.11,31–34 We found that patients with tumors ≥5 cm had a median survival of 16.3 months vs 31.5 months of tumors <5 cm. Currently, the radical surgery remains the primary treatment modality for this highly malignant sarcoma, with other treatments such as chemotherapy or radiotherapy concomitantly used under certain circumstances. Our results showed the prolonged survival of patients receiving surgery (32.9 months vs 12.4 months without surgery). Although it was reported that the survival of malignant vascular tumors was related to complete surgical resection,35 the aggressive nature of AS made it difficult to completely clear surgical margins.
The values of neutrophil, platelet and lymphocyte, monocyte, LDH and ALP values can be easily obtained with minimally invasive procedures. Recently, these markers have been evaluated in many studies to predict the prognosis in patients with various types of cancer including hepatocellular carcinoma, renal cell carcinoma, lung cancer, urinary cancer and colorectal cancer.36–41 These markers such as NLR, PLR and MLR are believed to reflect the interplay between the systemic inflammatory responses with the tumor microenvironment. Elevated NLR, PLR and MLR are able to increase the resting energy expenditure, hypoalbuminemia and malnutrition, which ultimately leads to weight loss and tumor progression.42,43 The exact mechanisms of this interaction remain incompletely defined. One possible explanation is that neutrophilia is related to the inhibition of cytotoxic activity of T cells and NK cells and at the same time lymphocyte infiltration has been shown to promote an effective antitumor cellular immune response.44–46 In this study, the multivariate analyses identified pretreatment NLR (HR 2.673, 95% CI 1.253–5.703, p=0.011) and LDH (HR 2.964, 95% CI 1.464–5.998, p=0.003) levels as independent indicators for AS prognosis.
One limitation of the present study is the number of patients enrolled. Owing to its extreme rarity, previous reports on AS could only reach a relatively small patient group and their results often lack consensus. In this study, the reason why prognostic values of tumor grade and size failed to reach statistical significance in multivariate analyses might be the limited number of primary AS patients. Further studies involving larger patient groups are therefore required. In addition, we were unable to retrieve patients’ TNM staging. Staging of AS follows the TNM system for soft tissue sarcoma by American Joint Committee on Cancer. However, because AS represents a unique type of all sarcomas, and there is no standardized treatment regime for each specific stage, TNM staging is of little benefit in clinical practice.47
Conclusion
In summary, AS is an extremely rare type of cancer with poor prognosis. This study identifies pretreatment serum levels of NLR and LDH as clinically useful markers to predict survival in patients with PAS. In addition, although survival curves suggested that patients with surgical treatment, low tumor grade and small tumor size have prolonged OS, the difference failed to reach statistical significance in multivariate analyses. Future studies involving larger patient groups with longer follow-up periods are warranted to verify the results.
Ethics approval and consent to participate
This retrospective study was approved by the institution ethics commission of Sichuan University, and due to its retrospective nature, a waiver of consent was granted for the proposed patient record review. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Abbreviations
NLR, neutrophil-to-lymphocyte ratio; OS, overall survival; LDH, lactate dehydrogenase; PLR, platelet-to-lymphocyte ratio; MLR, monocyte-to-lymphocyte ratio; SII, systemic immune-inflammation index; ALP, alkaline phosphatase; AS, angiosarcoma; PAS, primary angiosarcoma; ASFS, angiosarcoma of the face and scalp; ROC, receiver operating curves; AJCC, American Joint Committee on Cancer.
Data sharing statement
All data generated or analyzed during this study are included in this article.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rouhani P, Fletcher CD, Devesa SS, Toro JR. Cutaneous soft tissue sarcoma incidence patterns in the U.S.: an analysis of 12,114 cases. Cancer. 2008;113(3):616–627. doi:10.1002/cncr.23571
2. Toro JR, Travis LB, Wu HJ, Zhu K, Fletcher CD, Devesa SS. Incidence patterns of soft tissue sarcomas, regardless of primary site, in the surveillance, epidemiology and end results program, 1978-2001: an analysis of 26,758 cases. Int J Cancer. 2006;119(12):2922–2930. doi:10.1002/ijc.22239
3. Wang L, Lao IW, Yu L, Wang J. Clinicopathological features and prognostic factors in angiosarcoma: a retrospective analysis of 200 patients from a single Chinese medical institute. Oncol Lett. 2017;14(5):5370–5378. doi:10.3892/ol.2017.6892
4. Fayette J, Martin E, Piperno-Neumann S, et al. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol. 2007;18(12):2030–2036.
5. Shin JY, Roh SG, Lee NH, Yang KM. Predisposing factors for poor prognosis of angiosarcoma of the scalp and face: systematic review and meta-analysis. Head Neck. 2017;39(2):380–386.
6. Kunkiel M, Maczkiewicz M, Jagiello-Gruszfeld A, Nowecki Z. Primary angiosarcoma of the breast-series of 11 consecutive cases-a single-centre experience. Curr Oncol. 2018;25(1):e50–e53.
7. Fury MG, Antonescu CR, Van Zee KJ, Brennan MF, Maki RG. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer J. 2005;11(3):241–247.
8. Botti G, Scognamiglio G, Marra L, et al. Programmed death ligand 1 (PD-L1) expression in primary angiosarcoma. J Cancer. 2017;8(16):3166–3172.
9. Naka N, Ohsawa M, Tomita Y, et al. Prognostic factors in angiosarcoma: a multivariate analysis of 55 cases. J Surg Oncol. 1996;61(3):170–176.
10. Buschmann A, Lehnhardt M, Toman N, Preiler P, Salakdeh MS, Muehlberger T. Surgical treatment of angiosarcoma of the scalp: less is more. Ann Plast Surg. 2008;61(4):399–403. doi:10.1097/SAP.0b013e31816b31f8
11. Mark RJ, Poen JC, Tran LM, Fu YS, Juillard GF. Angiosarcoma. A report of 67 patients and a review of the literature. Cancer. 1996;77(11):2400–2406. doi:10.1002/(SICI)1097-0142(19960601)77:11<2400::AID-CNCR32>3.0.CO;2-Z
12. Maddox JC, Evans HL. Angiosarcoma of skin and soft tissue: a study of forty-four cases. Cancer. 1981;48(8):1907–1921. doi:10.1002/1097-0142(19811015)48:8<1907::aid-cncr2820480832>3.0.co;2-t
13. Holden CA, Spittle MF, Jones EW. Angiosarcoma of the face and scalp, prognosis and treatment. Cancer. 1987;59(5):1046–1057. doi:10.1002/1097-0142(19870301)59:5<1046::aid-cncr2820590533>3.0.co;2-6
14. Ito T, Tanaka K, Suzumura K, et al. Angiosarcoma arising in the non-operated, sclerosing breast after primary irradiation, surviving 6 years post-resection: a case report and review of the Japanese literature. Int J Surg Case Rep. 2016;24:26–31. doi:10.1016/j.ijscr.2016.05.001
15. Nomura M, Nakaya Y, Saito K, et al. Hemopneumothorax secondary to multiple cavitary metastasis in angiosarcoma of the scalp. Respiration. 1994;61(2):109–112. doi:10.1159/000196318
16. Yonemori K, Tsuta K, Ando M, et al. Contrasting prognostic implications of platelet-derived growth factor receptor-beta and vascular endothelial growth factor receptor-2 in patients with angiosarcoma. Ann Surg Oncol. 2011;18(10):2841–2850. doi:10.1245/s10434-011-1640-4
17. Choi ES, Kim HS, Han I. Elevated preoperative systemic inflammatory markers predict poor outcome in localized soft tissue sarcoma. Ann Surg Oncol. 2014;21(3):778–785. doi:10.1245/s10434-013-3418-3
18. Que Y, Qiu H, Li Y, et al. Preoperative platelet-lymphocyte ratio is superior to neutrophil-lymphocyte ratio as a prognostic factor for soft-tissue sarcoma. BMC Cancer. 2015;15:648. doi:10.1186/s12885-015-1584-3
19. Szkandera J, Gerger A, Liegl-Atzwanger B, et al. The lymphocyte/monocyte ratio predicts poor clinical outcome and improves the predictive accuracy in patients with soft tissue sarcomas. Int J Cancer. 2014;135(2):362–370. doi:10.1002/ijc.28677
20. Suzuki G, Yamazaki H, Aibe N, et al. Clinical usefulness of the platelet-to lymphocyte ratio in patients with angiosarcoma of the face and scalp. Int J Mol Sci. 2017;18(11). doi:10.3390/ijms18112402
21. Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11(10):983–991. doi:10.1016/S1470-2045(10)70023-1
22. Biswas B, Dabkara D. Bevacizumab in advanced angiosarcoma: what is the reality? J Clin Oncol. 2016;34(7):764. doi:10.1200/JCO.2015.64.2181
23. Italiano A, Chen CL, Thomas R, et al. Alterations of the p53 and PIK3CA/AKT/mTOR pathways in angiosarcomas: a pattern distinct from other sarcomas with complex genomics. Cancer. 2012;118(23):5878–5887. doi:10.1002/cncr.27614
24. Letsa I, Benson C, Al-Muderis O, Judson I. Angiosarcoma of the face and scalp: effective systemic treatment in the older patient. J Geriatr Oncol. 2014;5(3):276–280. doi:10.1016/j.jgo.2014.02.004
25. Bae SY, Choi MY, Cho DH, Lee JE, Nam SJ, Yang JH. Large clinical experience of primary angiosarcoma of the breast in a single Korean medical institute. World J Surg. 2011;35(11):2417–2421. doi:10.1007/s00268-011-1225-1
26. Meis-Kindblom JM, Kindblom LG. Angiosarcoma of soft tissue: a study of 80 cases. Am J Surg Pathol. 1998;22(6):683–697.
27. Zheng YW, Zhang XW, Zhang JL, et al. Primary hepatic angiosarcoma and potential treatment options. J Gastroenterol Hepatol. 2014;29(5):906–911. doi:10.1111/jgh.12506
28. Vorburger SA, Xing Y, Hunt KK, et al. Angiosarcoma of the breast. Cancer. 2005;104(12):2682–2688. doi:10.1002/cncr.21531
29. Hodgson NC, Bowen-Wells C, Moffat F, Franceschi D, Avisar E. Angiosarcomas of the breast: a review of 70 cases. Am J Clin Oncol. 2007;30(6):570–573. doi:10.1097/COC.0b013e3181131d62
30. Nascimento AF, Raut CP, Fletcher CD. Primary angiosarcoma of the breast: clinicopathologic analysis of 49 cases, suggesting that grade is not prognostic. Am J Surg Pathol. 2008;32(12):1896–1904. doi:10.1097/PAS.0b013e318176dbc7
31. Abraham JA, Hornicek FJ, Kaufman AM, et al. Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol. 2007;14(6):1953–1967. doi:10.1245/s10434-006-9335-y
32. Lahat G, Dhuka AR, Lahat S, et al. Outcome of locally recurrent and metastatic angiosarcoma. Ann Surg Oncol. 2009;16(9):2502–2509. doi:10.1245/s10434-009-0569-3
33. Pawlik TM, Paulino AF, McGinn CJ, et al. Cutaneous angiosarcoma of the scalp: a multidisciplinary approach. Cancer. 2003;98(8):1716–1726. doi:10.1002/cncr.11667
34. Sher T, Hennessy BT, Valero V, et al. Primary angiosarcomas of the breast. Cancer. 2007;110(1):173–178. doi:10.1002/cncr.22784
35. Karpeh MS
36. Krishnamoorthy RV, Reddy VV. Hepatopancreatic amylase activity as a function of warm-adaptation in a fresh-water field crab. Experientia. 1968;24(10):1019–1020. doi:10.1007/bf02138720
37. Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y. Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev. 2015;41(10):971–978. doi:10.1016/j.ctrv.2015.10.003
38. Templeton AJ, McNamara MG, Seruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Journal of the National Cancer Institute. 2014;106(6):dju124. doi:10.1093/jnci/dju061
39. Kano S, Homma A, Hatakeyama H, et al. Pretreatment lymphocyte-to-monocyte ratio as an independent prognostic factor for head and neck cancer. Head Neck. 2017;39(2):247–253. doi:10.1002/hed.24576
40. Piciucchi M, Stigliano S, Archibugi L, et al. The neutrophil/lymphocyte ratio at diagnosis is significantly associated with survival in metastatic pancreatic cancer patients. Int J Mol Sci. 2017;18(4):730.
41. Luo H, Ge H, Cui Y, et al. Systemic inflammation biomarkers predict survival in patients of early stage non-small cell lung cancer treated with stereotactic ablative radiotherapy - a single center experience. J Cancer. 2018;9(1):182–188.
42. Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC. Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg. 1994;219(4):325–331.
43. Wang DS, Luo HY, Qiu MZ, et al. Comparison of the prognostic values of various inflammation based factors in patients with pancreatic cancer. Med Oncol. 2012;29(5):3092–3100.
44. Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73(3–4):215–220.
45. Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009;137(2):425–428.
46. Mando P, Rizzo M, Roberti MP, et al. High neutrophil to lymphocyte ratio and decreased CD69(+)NK cells represent a phenotype of high risk in early-stage breast cancer patients. Onco Targets Ther. 2018;11:2901–2910.
47. Fujisawa Y, Yoshino K, Fujimura T, et al. Cutaneous angiosarcoma: the possibility of new treatment options especially for patients with large primary tumor. Frontiers in Oncology. 2018;8:46.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.