Back to Journals » Research and Reports in Urology » Volume 12
The Prevalence of Detrusor Underactivity and its Symptoms Co-relation with Urodynamic Study Findings in Patients with Lower Urinary Tract Symptoms
Authors Sawaqed F , Abughosh Z , Suoub M
Received 23 May 2020
Accepted for publication 3 August 2020
Published 24 September 2020 Volume 2020:12 Pages 415—422
DOI https://doi.org/10.2147/RRU.S264237
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Fadi Sawaqed,1 Zeid Abughosh,2 Mohammed Suoub1
1Section of Urology, Department of Special Surgery, Faculty of Medicine, Mu’tah University, Karak, Jordan; 2Istishari Urology Center, Istishari Hospital, Amman, Jordan
Correspondence: Fadi Sawaqed Tel +962 797350996
Email [email protected]
Purpose: This study determines the prevalence and clinical presentation of detrusor underactivity (DU) and its urodynamic characteristics in adult patients with lower urinary tract symptoms (LUTS).
Patients and Methods: This retrospective study has reviewed the symptoms and urodynamic study (UDS) findings of 283 patients with LUTS. Chi-square analysis was used to present the prevalence of UDS characteristics in both sexes.
Results: Out of records of 206 patients included in this study, fifty-one (24.76%) patients were diagnosed with DU based on bladder contractility index. Storage lower urinary tract symptoms were the most prevalent characteristic presentation in both sexes as compared to the difficulty in voiding, recurrent urine retention, and urinary incontinence. Bladder outlet, sphincter EMG findings, and degree of DU were significantly correlated with gender.
Conclusion: DU is a prevalent and sophisticated bladder pathology rather than a simple one. It requires more attention from the urologists, and evaluations, including UDS, to differentiate it from other pathologies.
Keywords: detrusor underactivity, prevalence, lower urinary tract symptoms, urodynamic study
Introduction
Although detrusor underactivity (DU) has neither a standard, detailed definition, nor widely accepted diagnostic criteria in clinical practice, it has started to gain more interest in clinical practice and research.1 The pathogenesis of DU is also under research, and the absence of effective treatments has caused many urologists to consider DU as an incurable, inconvenient concern.2 DU is also assumed to be a contributing factor in the development of more significant post-void residuals and recurrent urinary tract infections, which constitute a significant health problem, especially in adult population.3 Therefore, the health problem becomes complicated by antibiotic resistance.
The International Continence Society has defined DU as a contraction of reduced strength and/or duration, resulting in a failure to achieve complete bladder emptying within a normal time span.4 Recently, this definition was modified by D’Ancona et al5 as DU is a low detrusor pressure or short detrusor contraction time, usually in combination with a low-urine flow rate, resulting in prolonged bladder emptying and/or a failure to achieve complete bladder emptying within a normal time span.
Up till now, there lacks evidence to evaluate the prevalence of DU separately. However, DU is present in 9–28% of men <50 years of age than in 48% men >70 years. In older women, prevalence ranges from 12–45%.6 In the Korean population, the prevalence of DU in patients older than 65 years was 40.2% and 13.3% in men and women with lower urinary tract symptoms (LUTS), respectively.7 Another study from Australia has stated that the prevalence of DU in this study was 23%.8 DU was previously considered as secondary to the aging process,9 but it affects different patient groups, suggesting a multifactorial etiology including both myogenic and neurogenic etiologies.9–11
Recently, DU as a cause of LUTS in both men and women has been increasingly gaining attention. There is a major issue in the differentiation of underactive bladder symptoms and other causes of lower urinary tract symptoms such as detrusor hyperactivity and impaired contractility (DHIC), hypersensitive bladder (HSB), detrusor overactivity (DO), bladder outlet obstruction (BOO)12 and Dysfunctional Voiding (DV).13 In this regard, this study aims to determine the prevalence of DU along with its symptomatic and urodynamics (UDS) characteristics of DU in the Jordanian population.
The prevalence of DU is assumed to be higher among the institutionalized elderly, specifically in incontinent nursing home residents. Also, DU has been associated with a low rate of enhancement in both quality of life and individual symptoms following mid-urethral sling procedure in women and prostate surgery in men. On the contrary, the prevalence and clinical implications of DU remain mostly unknown in the elderly population in the elderly population since no standard measurement techniques or quantitative diagnostic criteria have been developed. In particular, appropriate management and diagnosis of this condition become challenging for physicians caring for elderly patients with LUTS.
To date, the prevalence of DU among the community-dwelling elderly population has been reported by several studies14,15 even though there has been no standard definition of urodynamic DU. These studies have merely considered small populations and did not assess the clinical attributes of DU. Thereby, most of the appropriate information has been inferred from epidemiological studies of urinary retention regarding the clinical characteristics of DU. This study has hypothesized to determine the prevalence and clinical characteristics of DU in an adult population with LUTS; to develop a better understanding and to establish a foundation for additional studies in this domain.
It is, therefore, necessary to be clear on its classification based on the potential etiologic mechanisms induced by different risk factors. However, one possible dilemma is that so far, no universally approved criteria have been ascertained for the classification of LUTS. Interest in DU among urologists has increased recently since it is a common occurrence that elevates with age, and it remains unexplored in clinical practices. Therefore, DU needs a urodynamic assessment for proper diagnosis. Previous studies, as well as reviews, have explained voiding dysfunction in women with an emphasis on its association with dysfunctional voiding attributes.12,16
Patients and Methods
Study Design and Patients
The study has reviewed a retrospective chart for 283 patients with LUTS who underwent UDS from July 2016 to August 2019. The study was approved by the Institutional Review Board (IRB). Records of patients 77 were excluded in the initial stage either due to missing data (4 cases) or exclusion criteria (73 cases). Following were the exclusion criteria: patients with neurogenic bladder (NB) due to known underlying neurological disease, history of open pelvic surgery or major abdominal surgery, or using indwelling catheters or clean intermittent catheterization (CIC) due to anatomical deformation of the lower urinary tract, impaired general health that influenced voiding or a neurogenic impairment influencing micturition function.
Therefore, the final study population was considered to be 206 patients. All patients in this study underwent comprehensive history taking, detailed physical examinations, and invasive urodynamic examinations, including filling cystometry, pressure-flow study urethral sphincter Electromyography (EMG) using Perineal patch electrodes. The ICS Good Urodynamic Practice Standards were followed to perform clinical urodynamic practice.17 The bladder contractility index below 100 was used as an objective parameter to define DU. Furthermore, DU was classified into three categories: mild, moderate, and severe based mainly on detrusor pressure considering the maximum urinary flow rate (Pdet@Qmax) values. A Pdet@Qmax of >40 cmH2O is accepted as normal; 30–40 cmH2O as mild; 20–30 cmH2O as moderate, and <20 cmH2O as severe DU.9 All patients have signed a formal written consent to perform UDS and to use their anonymous information in clinical research as part of the IUC policy.
Urodynamic Evaluations
All participants have had a thorough symptomatic evaluation for LUTS by completing the Arabic version of the International Prostate Symptom Score (IPSS),18 as well as the Arabic version of the International Consultation on Incontinence short-form questionnaire (ICIQ-UI SF).19 All participants had also gone through the urodynamic testing based on ICS standards. The assessment of urodynamic variables was based on: cytometric bladder capacity, presence of detrusor overactivity (DO), detrusor underactivity (DU), bladder volume at first sensation of bladder filling, normal and strong desire for urination, detrusor overactivity and impaired contractility (DOIC), Hypersensitive Bladder (HSB), detrusor pressure at maximum flow (PdetQmax), maximum flow rate (Qmax) volume voided, the post-void residual urine volume (PVR), and sphincter EMG characteristics.
Secondary urodynamic voiding parameters of Bladder Contractility Index (BCI) (PdetQmax + 5Qmax) and Bladder Outlet Obstruction Index (BOOI) (PdetQmax – 2Qmax) were calculated and included in the study. DU defined as a bladder contractility index of less than 100, for which the index was computed from the findings of the pressure-flow study (PFS).5,20
Statistical Analysis
Data were entered into Microsoft Office Excel. The IBM SPSS version 21.0 (IBM Co., New York, NY, USA) was used to present frequency tables through mean and standard deviation (SD). Median and proportions were used to present non-normally distributed variables and categorical variables, respectively. Chi-square analysis was used to determine the relationship between urodynamic characteristics and DU prevalence. A 2-tailed p-value <0.05 was used to determine the statistical significance.
Results
Out of 206 patients, 51 patients (26 males and 26 females) had bladder contractility index below 100 and were labeled as DU, yielding a prevalence rate of 24.76%. Only patients with DU proceeded for further analysis while the rest of the patients were dropped from the study and diagnosed as healthy. The reason behind dropping-off those healthy patients was that the pressure characteristics are difficult to standardize, and, therefore, focusing only on DU patients and associated symptoms would help the researcher to define a predictable pattern. Table 1 shows the clinicodemographic characteristics of patients. The findings indicate that patients were more prevalent in reporting storage symptoms as compared to other indications for UDS, such as urinary incontinence (UI), recurrent urine retention (RUR), and voiding symptoms. The most prevalent symptom reported according to the IPSS questionnair was day time-frequency (74.5%). However, the prevalence of incomplete emptying, intermittency, straining, weak stream, nocturia, and urgency was 45.1%, 60.8%, 66.6%, 68.6%, 70.5%, and 72.5% respectively (Figure 1). All patients reported a significant impact on the quality of life due to urinary symptoms, as their responses to the 8th question of the IPSS questionnaire were mixed(3.9%), unhappy(41.2%), mostly dissatisfied(31.4%), and terrible(23.5%) .
 |
Table 1 Clinical-Demographic Characteristics |
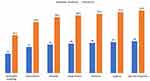 |
Figure 1 Prevalence of urinary symptoms among patients with DU according to their responses to the IPSS questionnaire. |
Tables 2 and 3 present the UDS findings associated with DU, and revealed that the mean PdetQmax was (29.71 cmH2O), and the mean Qmax was (8.1 mL/sec) with a mean BCI of (68.01). Furthermore, bladder contractility was found to be weak in both sexes (84.3%). Dysfunctional voiding was prevalent in 34 patients (66.7%) as compared to normal urethral function.
 |
Table 2 UDS Parameters |
 |
Table 3 UDS Findings Associated with DU |
The association between UDS findings and gender are shown in Table 4. The findings indicated an insignificant association of bladder sensitivity, detrusor function during filling cytometry, bladder contractility, and PSHx by gender (p >0.005). However, bladder outlet, sphincter EMG, and degree of DU were significantly correlated with both sexes. Females showed a greater degree of DU (p = 0.007) and a greater association with dysfunctional voiding (p = 0.010) on EMG. On the contrary, males showed more bladder outlet obstruction as compared to females (p = 0.006). Table 5 shows the association of urodynamic characteristics to diagnosis. The relationship between diagnosis and urodynamic characteristics was statistically significant based on bladder sensitivity, degree of DU, and gender.
 |
Table 4 Chi-Square Analysis Between Urodynamic Characteristics and Gender |
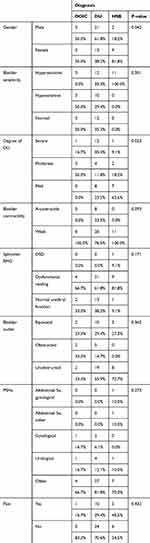 |
Table 5 Chi-Square Analysis Between Urodynamic Characteristics and Diagnosis |
Discussion
The bladder contractility becomes impaired with age, resulting in a high prevalence of DU in both males and females. DU has received a little scientific attention even though it was assumed to be a common geriatric condition because the urodynamic characteristics have not been demonstrated and lack a gold standard diagnostic criterion. The actual prevalence of DU among the community-dwelling individuals remains unidentified. Therefore, this study has aimed to determine the prevalence and clinical presentation of DU and its urodynamic characteristics in both sexes in adult patients. To the best of the researcher’s knowledge such kind of study has not been conducted in the Jordanian population before.
This study has focused on patients with LUTS who were over 18 years of age and were capable of performing regular tasks by themselves. Patients were assumed to influence micturition function, having neurogenic abnormalities, or regularly utilized a catheter for urine drainage were excluded from the study population. It was believed that emphasizing this population elevated the clinical similarity of this study cohort with community-dwelling elderly as compared to the elderly in chronic care facilities.
The findings indicated that the prevalence of DU was similar to DO in men and increased with age in both males and females. The study has not reached a conclusive demonstration of the higher occurrence of DU in adult men as compared to adult women. On the contrary, it was assumed that the higher prevalence of DU in adult men is likely to be multifactorial as compared to adult women. The prevalence of DU was 24.76%, and this was similar to previous studies.18,19 These outcomes have indicated that DU is considered as an essential element of the pathophysiology of LUTS in the adult population, as the patients get older. The prevalence of BOO might be partly classified to the exclusion of men with LUTS across the age spectrum indicative of BPH who received medication regardless of a urodynamic evaluation.21
The findings have also indicated that both sexes with DU were also prevalent to DO, HSB, and BOO. A previous study has also reported similar findings.15 This finding is a significant demonstration in the adult population for the clinical management of LUTS. The voiding difficulty might be aggravated by using antimuscarinics for the treatment of DO, resulting in chronic or acute urinary retention in patients with DU and DO respectively.22 Medical treatment has been given to the majority of the patients, which might be reflected with missed diagnosis due to the long duration of the prevalent problem and overlap of DU characteristics with other common symptoms such as bladder overactivity, urinary tract infections, and BOO.23,24 The findings of the current study are supported by the findings of Rademakers et al,25 who reported a prevalent increase of hesitancy, weak stream, and incomplete bladder emptying in women with DU as compared to men.
Cut-off values were used for the diagnosis of BOO or DU based on the PFS in women. However, the diagnosis of BOO or DU in women reflects barrier owing to the lack of predefined criteria compared to their diagnosis in men. The PFS cut-off values were adopted in this study for the diagnosis of DU in women. This series of criteria reflects on being stricter for the diagnosis of female DU as compared to the criteria utilized in previous studies. The population of this study includes both cohorts of intrinsic bladder dysfunction and bladder outlet obstruction. The value of UDS in differentiating bladder outlet dysfunction had been well-attributed in previous studies. However, this analysis has emphasized the sub-group of the intrinsic dysfunction, particularly for those with DU, and this approach was completely different from the previous work.
Strength and Limitations
Several limitations were found in this study. Firstly, the sample size prevalent in the bladder contractility index was small (n = 51). This limitation is may be due to the findings that were derived from a single tertiary center. In this regard, a multi-center prospective study will be required for confirming the findings. Secondly, patients were excluded from the study population who did not undergo a urodynamic assessment due to the retrospective design of the study. Lastly, the study has not included a control group of healthy cases for further comparison, which should be considered in future studies with more cases.
Conclusion
DU is a prevalent and sophisticated bladder pathology rather than a simple one. It requires more attention from the urologists, and comprehensive evaluations, including UDS, to differentiate it from other pathologies. Physicians who manage adult patients should understand the age-related pathophysiological changes, considering the findings of this study on the prevalence and clinical features of DU. Additional studies should make use of longitudinal trials as compared to cross-sectional trials for determining the natural history of DU in the adult population.
Clinical Trial Registration Number
NCT04336280.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Consideration
The study was approved by the Institutional Review Board (IRB) at the Istishari Hospital/Amman/Jordan, and it was performed in accordance with the Declaration of Helsinki.
Acknowledgment
The authors are very thankful to all the associated personnel in any reference that contributed to/for this research.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Yu YD, Jeong SJ. Epidemiology of underactive bladder: common but underresearched. Investig Clin Urol. 2017;58(Suppl 2):S68–S74. doi:10.4111/icu.2017.58.S2.S68
2. Nargund VH, Tanabalan CK, Kabir MN. Management of non–muscle-invasive (superficial) bladder cancer. Semin Oncol. 2012;39(5):559–572. doi:10.1053/j.seminoncol.2012.08.001
3. Cortes-Penfield NW, Trautner BW, Jump RLP. Urinary tract infection and asymptomatic bacteriuria in older adults. Infect Dis Clin North Am. 2017;31(4):673–688. doi:10.1016/j.idc.2017.07.002
4. Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn. 2002;21(2):167–178. doi:10.1002/nau.10052
5. D’Ancona C, Haylen B, Oelke M, et al. The international continence society (ICS) report on the terminology for adult male lower urinary tract and pelvic floor symptoms and dysfunction. Neurourol Urodyn. 2019;38(2):433–477. doi:10.1002/nau.23897
6. Osman NI, Chapple CR, Abrams P, et al. Detrusor underactivity and the underactive bladder: a new clinical entity? A review of current terminology, definitions, epidemiology, aetiology, and diagnosis. Eur Urol. 2014;65(2):389–398. doi:10.1016/j.eururo.2013.10.015
7. Jeong SJ, Kim HJ, Lee YJ, et al. Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms: a comparison between men and women. Korean J Urol. 2012;53(5):342–348. doi:10.4111/kju.2012.53.5.342
8. Hoag N, Gani J. Underactive bladder: clinical features, urodynamic parameters, and treatment. Int Neurourol J. 2015;19(3):185–189. doi:10.5213/inj.2015.19.3.185
9. Ahmed A, Farhan B, Vernez S, Ghoniem GM. The challenges in the diagnosis of detrusor underactivity in clinical practice: a mini-review. Arab J Urol. 2016;14(3):223–227. doi:10.1016/j.aju.2016.06.005
10. Aldamanhori R, Osman NI, Chapple CR. Underactive bladder: pathophysiology and clinical significance. Asian J Urol. 2018;5(1):17–21. doi:10.1016/j.ajur.2017.02.003
11. Suskind AM, Smith PP. A new look at detrusor underactivity: impaired contractility versus afferent dysfunction. Curr Urol Rep. 2009;10(5):347–351. doi:10.1007/s11934-009-0055-2
12. Yang TH, Chuang FC, Kuo HC. Urodynamic characteristics of detrusor underactivity in women with voiding dysfunction. PLoS One. 2018;13(6):e0198764. doi:10.1371/journal.pone.0198764
13. Clothier JC, Wright AJ. Dysfunctional voiding: the importance of non-invasive urodynamics in diagnosis and treatment. Pediatr Nephrol. 2018;33(3):381–394. doi:10.1007/s00467-017-3679-3
14. Valentini FA, Robain G, Marti BG, Nelson PP. Urodynamics in a community-dwelling population of females 80 years or older: which motive? Which diagnosis? Int Braz J Urol. 2010;36(2):218–224. doi:10.1590/S1677-55382010000200013
15. Abarbanel J, Marcus EL. Impaired detrusor contractility in community-dwelling elderly presenting with lower urinary tract symptoms. Urology. 2007;69(3):436–440. doi:10.1016/j.urology.2006.11.019
16. Everaert K, Van Laecke E, De Muynck M, Peeters H, Hoebeke P. Urodynamic assessment of voiding dysfunction and dysfunctional voiding in girls and women. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(4):254–264. doi:10.1007/s001920070035
17. Schäfer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21(3):261–274. doi:10.1002/nau.10066
18. Hammad FT, Kaya MA. Development and validation of an Arabic version of the international prostate symptom score. BJU Int. 2010;105(10):1434–1438. doi:10.1111/j.1464-410X.2009.08984.x
19. Hashim H, Avery K, Mourad MS, Chamssuddin A, Ghoniem G, Abrams P. The Arabic ICIQ-UI SF: an alternative language version of the english ICIQ-UI SF. Neurourol Urodyn. 2006;25(3):277–282. doi:10.1002/nau.20212
20. Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int. 1999;84(1):14–15. doi:10.1046/j.1464-410x.1999.00121.x
21. Defreitas GA, Zimmern PE, Lemack GE, Shariat SF. Refining diagnosis of anatomic female bladder outlet obstruction: comparison of pressure-flow study parameters in clinically obstructed women with those of normal controls. Urology. 2004;64(4):675–679. doi:10.1016/j.urology.2004.04.089
22. Li X, Liao LM, Chen GQ, Wang ZX, Lu TJ, Deng H. Clinical and urodynamic characteristics of underactive bladder: data analysis of 1726 cases from a single center. Medicine (Baltimore). 2018;97(3):e9610. doi:10.1097/MD.0000000000009610
23. Gammie A, Kaper M, Dorrepaal C, Kos T, Abrams P. Signs and symptoms of detrusor underactivity: an analysis of clinical presentation and urodynamic tests from a large group of patients undergoing pressure flow studies. Eur Urol. 2016;69(2):361–369. doi:10.1016/j.eururo.2015.08.014
24. Jeong SJ, Lee JK, Kim KM, Kook H, Cho SY, Oh SJ. How do we diagnose detrusor underactivity? Comparison of diagnostic criteria based on an urodynamic measure. Investig Clin Urol. 2017;58(4):247–254. doi:10.4111/icu.2017.58.4.247
25. Rademakers K, Oelke M, Van Koeveringe G. Detrusor underactivity in females: significant correlation between standardised medical history assessment and urodynamic findings. Neurourol Urodyn. 2014;33:922.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
