Back to Journals » Vascular Health and Risk Management » Volume 15
The prevalence, awareness, treatment, and control of hypertension among adults: the first cross-sectional national population-based survey in Laos
Authors Pengpid S , Vonglokham M , Kounnavong S, Sychareun V, Peltzer K
Received 21 December 2018
Accepted for publication 22 January 2019
Published 27 February 2019 Volume 2019:15 Pages 27—33
DOI https://doi.org/10.2147/VHRM.S199178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Harry Struijker-Boudier
Supa Pengpid,1,2 Manithong Vonglokham,3 Sengchanh Kounnavong,4,5 Vanphanom Sychareun,6 Karl Peltzer7,8
1ASEAN Institute for Health Development, Mahidol University, Salaya, Nakhon Pathom, Thailand; 2Office of the Deputy Vice Chancellor (Research and Innovation), North West University, Potchestroom, South Africa; 3Department of Health Policy and Health System Research, Lao Tropical and Public Health Institute, Vientiane, Laos; 4Lao Tropical and Public Health Institute, Vientiane, Laos; 5Ministry of Health, Vientiane, Laos; 6Faculty of Postgraduate Studies, University of Health Sciences, Ministry of Health, Vientiane, Laos; 7Department for Management of Science and Technology Development, Ton Duc Thang University, Ho Chi Minh City, Vietnam; 8Faculty of Pharmacy, Ton Duc Thang University, Ho Chi Minh City, Vietnam
Aim: The aim of this study was to determine the national prevalence of hypertension and its awareness, treatment, and control in Laos.
Methods: A national cross-sectional study was conducted in 2013. Using stratified cluster random sampling, 2,543 individuals aged 18–64 years were included from Laos. According to WHO STEPS methodology, questionnaire interview, anthropometric and blood pressure measurements, and biochemistry tests were conducted. Logistic regressions were used to estimate the determinants of hypertension (SBP [and/or DBP] ≥140 [90] mmHg or use of antihypertensive medications).
Results: Overall, 20.0% of the population had hypertension, 18.5% among men and 21.1% among women. Among hypertensives, 29.4% were aware, 18.2% were currently using antihypertensive medication, and 16.7% had controlled their blood pressure (<140 mmHg SBP and
DBP <90 mmHg). In fully adjusted models in both men and women, older age and general obesity were positively associated with hypertension. In addition, among men having raised cholesterol and completed primary education, and among women central obesity and hazardous or harmful alcohol users were positively associated with hypertension.
Conclusion: The study found a significant prevalence of hypertension and low awareness, treatment, and control rates of hypertension among adults in Laos.
Keywords: hypertension, awareness, treatment, control, determinants, population survey, Laos
Introduction
In low- and middle-income countries, the health burden of chronic noncommunicable diseases (NCDs) have been increasing,1 including in Southeast Asian countries, such as in Laos.2 NCDs and their risk factors, such as hypertension, stroke, and diabetes, are largely contributing to morbidity and mortality of the Lao population.3–5 In a 2008 Lao STEPS survey, conducted only in one municipality (Vientiane), a hypertension prevalence of 22.3% among 25- to 64-year olds (24.9% among men and 20.5% among women) was found.3 There is a lack of national data on the prevalence and associated factors of hypertension in Laos.
Increasing trends have been shown in the prevalence of hypertension in high-, middle-, and low- income countries.2 Between 1975 and 2015, “mean SBP might have increased in men and women in southeast Asia”.6 In southeast Asia, three-quarters or more of the rise in raised blood pressure is attributable to population growth and aging, and the remainder is due to an increase in prevalence.6 In other national population-based surveys in Southeast Asia, the prevalence of hypertension was in Cambodia 15.3% (25–64 years in 2010),7 in Malaysia 43.5% (≥30 years in 2011),8 in Myanmar 30.1% (15- to 64-year olds in 2009),9 in Sri Lanka 23.7% (≥18 years in 2005–2006),10 Thailand 22.0% (15 years and older in 2004),11 and Vietnam 25.1% (≥25 years in 2002–2008).12
Although hypertension is a preventable disease, recent studies found, however, a low prevalence of antihypertensive medication treatment. In the 2008 Lao STEP survey, 83.8% of the people diagnosed as hypertensive were not on medication.3 In the previously reported national population-based surveys in China, 42.6% were aware of their hypertension status and 34.1% received antihypertensive treatment,13 in Iran 34% were aware and 24.8% were treated,14 in Thailand 30.2% were aware,11 and in Vietnam 48.4% were aware and 29.5% received treatment.12 In a community study with participants (35–70 years) from 17 mainly low- and middle-income countries, 46.5% were aware of their hypertension diagnosis and 32.5% were treated.15 These studies indicate the very important need for the improvement in the diagnosis and treatment of hypertension.15
Various risk factors have been found to be linked with hypertension, including socio-demographics (older age, women or men, lower education level, lower household income),9–12,14–16 urban residence,9,12 and other risk factors including body weight status and health risk behavior and psychosocial stress and support. Higher body mass index (BMI) has been found to be positively9,13,15–17 and underweight status negatively10 associated with hypertension. Other metabolic risk factors for hypertension include diabetes17–19 and dyslipidemia or low high-density lipoproteins.19,20 Various dietary behaviors, including insufficient fruit and vegetable intake,21–23 and consumption of fatty foods24,25 and fast foods26 increased the odds of having hypertension. A number of studies found an association between physical inactivity,9,13,27 smoking,28 problem, or habitual drinking13,29 and hypertension. The aim of this study was to assess the prevalence of hypertension and its awareness, treatment, and control in Laos.
Methods
Study design and participants
A multi-stage cluster survey (villages and urban/rural) using WHO STEPS methodology was conducted among adults (18–64 years) in Laos in 2013; the response rate was 98%. More details regarding the survey are discussed in a study by Vonglokham et al.30
Written informed consent was obtained from study participants and the research protocol was approved by the “National Ethical Committee for Health Research” (Deliberation No 019/NECHR of 03 January, 2013) in Laos.
Measures
According to WHO STEPS methodology,31 interviews, anthropometric and blood pressure measurements, and biochemistry tests were conducted.30 Interview questions included dietary behavior (fruit and vegetable consumption), alcohol use, tobacco use, physical activity, and sociodemographic variables. Based on the “Global Physical Activity Questionnaire”,32 the levels of physical activity were classified into low, moderate, and high. Participants consuming >7 (women) or >14 (men) standard alcoholic units in the past week were considered hazardous or harmful alcohol users.33
BMI was classified according to Asian criteria: normal weight (18.5 to <23.0 kg/m2), overweight (23.0 to <25.0 kg/m2), and obese (25+ kg/m2).34 Central obesity was classified as “waist circumference (WC) 90 cm or more in men and 80 cm or more in women”.35 Each of the three SBP and DBP readings were averaged arithmetically. Hypertension was defined as “SBP ≥140 mmHg and/or DBP ≥90 mmHg or where the participant is currently on antihypertensive medication”.36
Raised cholesterol was classified as “raised fasting total cholesterol ≥5.0 mmol/L or currently on medication for raised cholesterol”.30 Raised fasting blood glucose was classified as “blood glucose ≥6.1 mmol/L and/or on diabetes medication”.30
Data analysis
Post-stratification weighting accounted for population distribution by districts, gender, and age groups from the national population census projection for 2012 based on the Laos National Census conducted in 2005.30 Individual weight was determined with the inverse of the probability of selection for each respondent, which was considered as the weight for the individual household.30
Descriptive statistics on frequency, weighted prevalence, and 95% CI was used for sociodemographic and risk factor variables. Logistic regression was performed to assess associations between sociodemographics, health variables, and prevalence of hypertension. All analyses were adjusted for the multi-stage sampling design and conducted with STATA software version 14.0 (StataCorp LLC, College Station, TX, USA).
Results
Sample characteristics
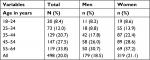
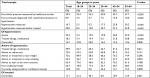
The total sample included 2,543 individuals aged 18–64 years (women, 59.3%; mean age, 38.7 years, SD =12.8) from Laos. Overall, 20.0% of the population had hypertension, 18.5% among men and 21.1% among women, 8.0% among 18- to 24-year olds and 33.8% among 55- to 64-year olds. Among hypertensives, 29.4% were aware that they had hypertension, which was higher in women (32.0%) than in men (25.0%). Of the population with hypertension, 18.2% were currently using antihypertensive medication, and 16.7% had controlled their blood pressure (<140 mmHg and DBP <90 mmHg). Mean SBP was 3.7 mmHg higher for men than for women, while mean DBP was 1.2 mmHg higher for women than for men. The prevalence of BMI obesity as well as central obesity was higher in women (28.0% and 39.4%, respectively) than in men (21.4% and 13.0%, respectively), while the current tobacco use prevalence was significantly higher in men (56.3%) than in women (18.5%) (Tables 1 and 2).
  | Table 1 Sample characteristics |
  | Table 2 Prevalence of hypertension by age and sex |
Only 39.9% of the population sample indicated that they had ever their blood pressure measured by a healthcare worker; this rate increased from 29.4% among 18- to 24-year olds to 47.7% among 55- to 64-year olds. Of the individuals aware of their hypertension status, half (49.9%) indicated that they were currently taking antihypertensive medication; this was above 60% among 18- to 24- and 55- to 64-year olds, while this was only 26.7% among 35- to 44-year olds. More than 65% of participants being aware of their hypertension status were given advise to reduce salt, lose weight, and start or do more exercise, while only 44.2% overall and 14.7% among 25- to 34-year olds had been advised to stop using tobacco. More than one in four (26.7%) of the participants who were aware of their hypertension status had ever consulted a traditional healer for their hypertension problem, and 12.8%, in particular among older age groups, were currently taking a herbal or traditional remedy for their hypertension. Among participants who were using antihypertensive medication, overall only 17.1% were controlled; this was the highest among 25- to 34-year olds (40.1%) and lowest among 35- to 44-year olds (0.0%) (Table 3).
  | Table 3 Awareness and treatment pattern for hypertension by age group among 2,543 adults in the Laos STEPS Survey, 2013 |
Associations between risk factors and hypertension
Table 4 shows associations (ORs) between independent variables and the prevalence of hypertension among men and women, separately. In fully adjusted models for both men and women, older age and general obesity were positively associated with hypertension. In addition, among men having raised cholesterol and having completed primary education, and among women central obesity and hazardous or harmful alcohol use were positively associated with hypertension (Table 4).
  | Table 4 Predictors of hypertension by gender Notes: aAdjusted for age; badjusted for all covariates. ***P<0.001, **P<0.01, *P<0.05. Abbreviations: AOR, adjusted odds ratio; COR, crude odds ratio. |
Discussion
In this first nationally representative population-based survey on hypertension in Laos, the prevalence of hypertension in adults (18–64 years) was 20.0% in 2013, which is similar to the prevalence among 25- to 64-year olds in the 2008 Lao STEP survey in nine health districts of Vientiane Capital City (22.3%).3 This figure is lower than in the Myanmar survey in 2009 of 30.1% in 15- to 64-year olds,9 22.0% in Thailand (15 years and older in 2004)11 and the China survey in 2010 of 29.6% in individuals 18 years and older,13 and the global adult (≥20 years) prevalence in low- and middle-income countries (31.5%),37 similar to the prevalence of hypertension in Iran (25- to 64-year olds),14,38 Sri Lanka (≥18 years),11 and Vietnam (≥25 years),12 but higher than in Cambodia (15.3% in 25- to 64-year olds).7
Of those who had hypertension, only 29.3% were aware and 18.2% were using antihypertensive medication. Similarly, among 25- to 64-year-old hypertensives in the 2008 Lao STEP survey in nine health districts of Vientiane Capital City, 16.2% were on antihypertensive medication.3 The proportion of awareness was lower in this study compared to figures reported from China,13 Vietnam,12 and globally in low- and middle-income countries,15,37 and the proportion of reported treatment was also significantly lower in this study than in other countries, including China,13 Iran,14 Vietnam,12 and globally in low- and middle-income country studies.15,37 The awareness and treatment of hypertension was in this study greater among women than men, as reported previously.16 These results suggest that awareness and treatment of hypertension needs to be strongly improved, particularly among men.
This study found, in agreement with various studies,9–12,14–16 that older age (among both men and women) was associated with hypertension. Previous studies9,12 found an association between urban residence and hypertension, while this study found this association only in bivariate analysis. Regarding weight variables, general obesity increased the odds of having hypertension in men and women. The relationship between obesity and hypertension has been confirmed in several previous studies.9,13,15–17 Obesity may be associated with hypertension independently but it could also be mediated through unhealthy diet and inadequate physical activity.14 Other metabolic risk factors for hypertension include diabetes17–19 and dyslipidemia,19,20 while in this study only in bivariate analysis among women an association between diabetes and hypertension was found, and among men an association between dyslipidemia and hypertension was found.
As found in a number of previous studies,9,13,27 bivariate analysis in this study also indicated that high physical activity among men but not among women was negatively associated with hypertension. The elevated blood pressure among the women participants of the study may not be attributable to physical inactivity but might be related to other factors such as obesity.39
Unlike previous studies,21–26 this study did not find an association between fruit and vegetable, saturated fat, fast food consumption (having meals prepared outside the home) and hypertension. Current tobacco use is a significant risk factor for hypertension.28 However, in this study no association was found. It is possible that the impact of current tobacco use on hypertension is delayed, and thus, current tobacco use may not be closely correlated with hypertension.40 In a “life-course impact of smoking on hypertension” study, Gao et al40 found that current number of cigarettes smoked per day was negatively associated with the risk of hypertension; however, the increase of “life-course-adjusted number of cigarettes smoked per day” was associated with higher risks of hypertension. This study found, in agreement with previous studies,13,29 that hazardous or harmful alcohol use was among women was associated with hypertension.
Limitations
Apart from blood chemistry, blood pressure, and anthropometric assessments, a study limitation was that the information assessed by questionnaire was based on self-report. Certain behaviors, such as substance use, may have been over- or under-reported. This study was cross-sectional, which hinders to establish causal relationships between risk factors and the development of hypertension. Another limitation was that salt intake, which is a determinant of hypertension, was not assessed in this study.
Conclusion
The study found a significant prevalence of hypertension in a representative sample of the general adult population in Laos. Less than one-third of hypertensives were aware and a minority were treated and controlled. Several risk factors, including sociodemographic variables (older age, completion of primary school), body weight status (obesity), health behavior (hazardous or harmful alcohol use), and raised cholesterol levels have been identified, which can facilitate in guiding hypertension control programs. Interventions strategies that operate at multiple levels are needed that can increase awareness of hypertension, access to high blood pressure treatment, and community-wide health promotion interventions that were identified and known to be effective in reducing high blood pressure levels. Future studies may want to include additional measures such as salt intake consumption.
Acknowledgment
The WHO supported this survey.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization (WHO). Global Status Report On Noncommunicable Diseases 2014. Geneva, Switzerland: WHO; 2014. | ||
Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380(9841):611–619. | ||
Vang C, Melanie C, Phoxay C, et al. Report on STEPS Survey on Non Communicable Diseases Rick Factors in Vientiane Capital city, Lao PDR, 2010. Available from: www.who.int/ncds/surveillance/steps/2008_STEPS_Report_Laos.pdf. Accessed June 12, 2018. | ||
Vang C. The burden of hypertension in the Lao PDR. Lao Med J. 2010;1:36–39. | ||
Loo KW, Gan SH. The burden of stroke in the Lao People’s Democratic Republic. Int J Stroke. 2013;8:273–275. | ||
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37–55. | ||
Gupta V, Logerfo JP, Raingsey PP, Fitzpatrick AL. The prevalence and associated factors for prehypertension and hypertension in Cambodia. Heart Asia. 2013;5(1):253–258. | ||
Naing C, Yeoh PN, Wai VN, Win NN, Kuan LP, Aung K. Hypertension in Malaysia: an analysis of trends from the national surveys 1996 to 2011. Medicine (Baltimore). 2016;95(2):e2417. | ||
Bjertness MB, Htet AS, Meyer HE, et al. Prevalence and determinants of hypertension in Myanmar – a nationwide cross-sectional study. BMC Public Health. 2016;16:590. | ||
Katulanda P, Ranasinghe P, Jayawardena R, Constantine GR, Rezvi Sheriff MH, Matthews DR. The prevalence, predictors and associations of hypertension in Sri Lanka: a cross-sectional population based national survey. Clin Exp Hypertens. 2014;36:484–491. | ||
Aekplakorn W, Abbott-Klafter J, Khonputsa P, et al. Prevalence and management of prehypertension and hypertension by geographic regions of Thailand: the third National health Examination Survey, 2004. J Hypertens. 2008;26(2):191–198. | ||
Son PT, Quang NN, Viet NL, et al. Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. J Hum Hypertens. 2012;26(4):268–280. | ||
Wang J, Zhang L, Wang F, Liu L, Wang H. China national survey of chronic kidney disease Working Group. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014;27:1355–1361. | ||
Esteghamati A, Abbasi M, Alikhani S, et al. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the National survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens. 2008;21(6):620–626. | ||
Chow CK, Teo KK, Rangarajan S, et al; PURE (Prospective Urban Rural Epidemiology) Study investigators. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. | ||
Hussain MA, Mamun AA, Reid C, Huxley RR. Prevalence, awareness, treatment and control of hypertension in Indonesian adults aged ≥40 years: findings from the Indonesia family life Survey (IFLS). PLoS One. 2016;11(8):e0160922. | ||
Naly N, Sanong T, Vang C, Mayfong M. Risk factors associated with hypertension among Lao adults in Vientiane, Laos. Lao Med J. 2010;1:40–45. | ||
Rahman M, Zaman MM, Islam JY, et al. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. J Hum Hypertens. 2018;32:334–348. | ||
Gupta V, LoGerfo JP, Raingsey PP, Fitzpatrick AL. The prevalence and associated factors for prehypertension and hypertension in Cambodia. Heart Asia. 2013;5(1):253–258. | ||
Soubeiga JK, Millogo T, Bicaba BW, Doulougou B, Kouanda S. Prevalence and factors associated with hypertension in Burkina Faso: a countrywide cross-sectional study. BMC Public Health. 2017;17:64. | ||
Li B, Li F, Wang L, Zhang D. Fruit and vegetables consumption and risk of hypertension: a meta-analysis. J Clin Hypertens (Greenwich). 2016;18:468–476. | ||
Wang L, Manson JE, Gaziano JM, Buring JE, Sesso HD. Fruit and vegetable intake and the risk of hypertension in middle-aged and older women. Am J Hypertens. 2012;25:180–189. | ||
Zhao D, Qi Y, Zheng Z, et al. Dietary factors associated with hypertension. Nat Rev Cardiol. 2011;8:456–465. | ||
Ezekwesili CN, Ononamadu CJ, Onyeukwu of , Mefoh NC. Epidemiological survey of hypertension in Anambra state, Nigeria. Niger J Clin Pract. 2016;19:659–667. | ||
El-Badawy AM, Al-Kharusi HM, Al-Ghanemy SA. Health habits and risk factors among Omanis with hypertension. Saudi Med J. 2005;26(4):623–629. | ||
Xu X, Byles J, Shi Z, McElduff P, Hall J. Dietary pattern transitions, and the associations with BMI, waist circumference, weight and hypertension in a 7-year follow-up among the older Chinese population: a longitudinal study. BMC Public Health. 2016;16:743. | ||
Börjesson M, Onerup A, Lundqvist S, Dahlöf B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. 2016;50:356–361. | ||
Leone A. Smoking and hypertension: independent or additive effects to determining vascular damage? Curr Vasc Pharmacol. 2011;9(5):585–593. | ||
Miller PM, Anton RF, Egan BM, Basile J, Nguyen SA. Excessive alcohol consumption and hypertension: clinical implications of current research. J Clin Hypertens (Greenwich). 2005;7:346–351. | ||
Vonglokham M, Kounnavong S, Sychareun V, Pengpid S, Peltzer K. The prevalence and social and health determinants of pre-diabetes and diabetes among adults in Laos: a cross-sectional national population-based survey, 2013. Trop Med Int Health. 2019;24(1):65–72. | ||
World Health Organization. STEP wise approach to noncommunicable disease risk factor surveillance (STEPS). Available from: http://www.who.int/chp/steps/riskfactor/en/. Accessed March 18, 2018. | ||
World Health Organization. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. Geneva: World Health Organization; 2012. | ||
Force U. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140:554–556. | ||
Wen CP, David Cheng TY, Tsai SP, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009;12(4):497–506. | ||
World Health Organization (WHO).Waist circumference and waist-hip ratio report of a WHO expert consultation Geneva, 8–11 December 2008; 2011. Available from: http://whqlibdoc.who.int/publications/2011/9789241501491eng.pdf. Accessed May 15, 2018. | ||
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. | ||
Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. | ||
Hosseini M, Yousefifard M, Baikpour M, et al. Twenty-year dynamics of hypertension in Iranian adults: age, period, and cohort analysis. J Am Soc Hypertens. 2015;9:925–934. | ||
Krauss RM, Winston M, Fletcher BJ, Grundy SM. Obesity: impact on cardiovascular disease. Circulation. 1998;98:1472–1476. | ||
Gao K, Shi X, Wang W. The life-course impact of smoking on hypertension, myocardialinfarction and respiratory diseases. Sci Rep. 2017;7:4330. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
