Back to Journals » International Journal of Women's Health » Volume 14
The Predictors of Intent to Prevent Obstetric Fistula Recurrence Among Women with Fistula in Ethiopia: A Facility-Based Cross-Sectional Study
Authors Hurissa BF , Koricha ZB, Dadi LS
Received 11 June 2022
Accepted for publication 25 August 2022
Published 14 September 2022 Volume 2022:14 Pages 1323—1335
DOI https://doi.org/10.2147/IJWH.S378162
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Bekana Fekecha Hurissa,1 Zewdie Birhanu Koricha,2 Lelisa Sena Dadi3
1School of Midwifery, Institute of Health, Jimma University, Jimma, Ethiopia; 2Department of Health, Behavior, and Society, Faculty of Public Health, Jimma University, Jimma, Ethiopia; 3Department of Epidemiology, Faculty of Public Health, Jimma University, Jimma, Ethiopia
Correspondence: Bekana Fekecha Hurissa, Email [email protected]
Background: Obstetric fistula recurrence predisposes to a decreasing success rate of fistula repair and accounts for the continued incidence of obstetric fistulas in low-income countries. Evidence has revealed that there are women’s intent gaps in the prevention of obstetric fistula recurrence. Assessments of predictors of intent to prevent obstetric fistula recurrence among women with fistula are scarce.
Objective: This study assessed the intent to prevent obstetric fistula recurrence and its predictive factors among women with obstetric fistula in Ethiopia.
Methods: Facility-based cross-sectional study was conducted from April 01, 2019, to August 01, 2019, with consecutively selected 478 women with fistulas in five fistula treatment centers in Addis Ababa and Oromia regions. Data were collected using an interviewer-administered structured questionnaire and analyzed using SPSS 23 software. Simple and multiple linear regression models were fitted for data analysis.
Results: Mean score of intent to prevent obstetric fistula recurrence among women with obstetric fistula was 27.72 ± 5.06. Living in a rural setting (β =− 2.27; 95% CI: − 3.62, − 0.93), being married (β =1.71, 95% CI: 0.56, 2.85), having one previous repair (β =2.14, 95% CI: 0.19, 4.08), high self-esteem (β =1.42, 95% CI: 0.09, 2.74), psychological health (β =0.05, 95% CI: 0.26, 3.79), living with fistula ≥ 5 years (β =1.82, 95% CI: 0.44, 3.21), high knowledge of risk factors (β =3.12, 95% CI: 1.99, 4.25), and a positive attitude (β =2.33, 95% CI: 1.12, 3.54) were significant predictors of the intent to prevent obstetric fistula recurrence.
Conclusion: Intent to prevent obstetric fistula recurrence among women with obstetric fistula was low. This indicates an urgent need to create awareness among women with an obstetric fistula on the risk factors of obstetric fistula recurrence, attitudinal changes towards prevention of obstetric fistula recurrence, and the availability of prevention measures.
Keywords: attitude towards fistula recurrence prevention, intent, women with fistula, predictive factors, knowledge of risk factors, Ethiopia
Introduction
Obstetric fistula is a serious, debilitating complication related to childbirth with devastating effects on a woman’s life. It remains a prominent cause of maternal morbidity in the developing world.1,2 Despite a 43% reduction in maternal deaths from 1990 to 2015, still, about 830 women die each day due to complications associated with pregnancy and childbirth. It is estimated that 2 to 3.5 million women currently suffer from untreated fistulas worldwide.3,4 Globally, the continued incidence of obstetric fistulas in low-income countries is one of the most explicit indicators of the big gaps in maternal health care between the developed and developing worlds.5
From 2010 to 2013, fewer than 2000 women had obstetric fistula surgery per year on average; although more than 110,000 Ethiopian women have a vaginal fistula, it will take decades of years to repair the existing fistula even if there is no new occurrence of obstetric fistula.6 Obstetric fistula recurrence predisposes to a decreasing success rate of fistula repair. On the other hand, success rates decrease with increasing numbers of previous attempts at surgical repair and diminish after a third attempt.7 History of prior repeat surgical repair is a risk factor for surgical repair failure.8 A single-center study shows that the success rates for the first, second, third, and fourth repeat repairs were found to be 68.8%. 56.2%, 50%, and 0%, respectively.9
Different initiatives such as the United Nations Population Fund (UNFPA), Maternal Health Task Force (MHTF), countdown, Global Strategy for Women’s health, and others have devoted efforts to reducing preventable maternal mortality.10,11 Despite such efforts, obstetric fistula still compromises the well-being of affected women in all dimensions of their health.12,13
Many women with obstetric fistulas experience varying degrees of social stigma that can prevent them from seeking care early.5 In addition, lack of sexual and reproductive health knowledge, or cultural inhibitions to discuss these topics, lead a woman to accept these conditions as normal postpartum healing rather than seeking care.14 Factors such as cultural norms, gender discrimination, and poor health care providers’ attention to the needs of women in planning and delivering health services impede women with obstetric fistulas from seeking and receiving help early when they have had obstetric complications in a previous pregnancy.15 Lack of a good relationship and care from health care providers leads clients to dissatisfaction with the health system, diminishing the likelihood of their timely health care seeking and directly affecting the well-being of patients.15–17 Inadequate knowledge of signs and symptoms of illness, lack of service availability, cost of services, lack of transport options, and poor quality of care are also other factors that prevent women with fistula not to seek care early.16–18 Many women and/or their families, especially those who lack skilled care during delivery, may not even know that fistula treatment exists and when, where, and how to seek care.19 Seeking out the option of surgery versus vaginal birth in certain places is also thought to be less womanly and unnatural.20
Intent to prevent a fistula was defined as the extent to which women with a fistula plan to prevent the recurrence of a fistula. It was based on a scoring method.21–23 Evidence has revealed that there are women’s intent gaps in the prevention of obstetric fistula recurrence.24 Most of the studies conducted on obstetric fistulas were qualitative studies and a few quantitative studies focused on the prevalence, causes, and social implications of fistulas.4,6,23,25–29 There is a gap in evidence on the predictors of intent to prevent obstetric fistula recurrence among women with fistula in developing countries, and there is no such study in Ethiopia. Therefore, this study aimed to assess the predictors of intent to prevent obstetric fistula recurrence among women with fistula in Ethiopia.
Materials and Methods
Study Area, Design, and Period
A cross-sectional study was conducted at five fistula treatment centers in Ethiopia on 478 consecutively selected women with obstetric fistulas from April 01, 2019, to August 01, 2019.
Study Population and Inclusion Criteria
The populations included in this study were all women with obstetric fistula (mostly vesicovaginal fistula cases). These included: women who were diagnosed with obstetric fistula and waiting for surgery; those after one week of surgery before their discharge; and women who have been appointed for a checkup after surgical treatment.
Exclusion Criteria
In this study, twenty-one women with fistulas who were not volunteered to participate, those with severe fistulas with complications (infections or comorbidities), cases of fistula secondary to trauma/surgery, and who cannot be able to respond to the study were excluded from the study.
Sample Size and Sampling Technique
The sample size was estimated using the single population proportion formula. This was based on the assumptions (1.2% prevalence of obstetric fistula in the Oromia Region,2 95% confidence level, 1% precision, and 5% nonresponse rate). Accordingly, 478 samples of women living with obstetric fistula were included in the study. The quotas of women consecutively selected during the study period from each study area were: 256 women from Addis Ababa Hamlin fistula center, 54 from Harar Hamlin fistula center, 42 from Asella hospital, 40 from Mettu Hamlin fistula center, and 86 from Jimma University Medical Center (see Figure 1).
 |
Figure 1 Diagrammatic representation of the sampling technique. |
Operational Definitions
Domain: indicates the four health components of quality of life.
Intent: - what someone plans to do.21–23
Knowledge: - It is measured based on twelve items of the knowledge of the risk factors questionnaire. Classification schemes for knowledge of risk factors among participants were based on questions used to assess knowledge adapted from a previous study.14
High knowledge: - Scoring 7–12 on knowledge of the risk factors of obstetric fistula recurrence questions.14
Low knowledge: - Scoring 0–6 on knowledge of the risk factors of obstetric fistula recurrence questions.14
Attitude: - Is the way that one considers and feels around something or the way one carries on with someone. Classification schemes for attitudes towards fistula recurrence prevention among participants were based on a previous study.21
Positive attitude: - Scoring 86–170 on attitude questions on obstetric fistula prevention.21
Negative attitude: - Scoring 1–85 on attitude questions on obstetric fistula prevention.21
Self Esteem: - It is someone’s set consideration and sentiments, almost her/him worth and significance that’s a wholly positive or negative state of mind towards oneself.21
Paid work:- Means work done for financial gain as payment or in expectation of payment and includes all types of work such as working as a government or non-government employee with salary.
Unpaid work:- This means work that does not receive any direct financial gain and includes all routine household chores.
Data Collection Tool
Tools for the assessment of intent to prevent obstetric fistula recurrence with 8 items (five Likert scales: strongly disagree, disagree, uncertain, agree, and strongly agree) and predicted factors were adopted after a review of relevant literature. Eight items of intent to prevent fistula recurrence were: delivering by a skilled birth attendant, staying close to the health facility after 36 weeks of gestation, going to the health facility immediately after labor begins, delivering at the health facility, having a vaginal delivery, having a cesarean section, using traditional medicine to speed up labor, and attending antenatal care as stipulated throughout pregnancy.21 The predictor term quality of life was measured using the World Health Organization (WHO) quality of Life shortened version (WHOQOL-BREF) tool with 24 items and a four-domain structure (five Likert scales).30 The predictor term self-esteem was based on four Likert scales with ten items adapted from the Rosenberg self-esteem scale.31 The tool for attitude towards fistula recurrence prevention was with 34 items (five Likert scales).21
The tools were translated from the English language to local languages (Afan Oromo and Amharic) and translated back to English and pretested on 5% of the sample size and found reliable with Cronbach’s Alpha value of (Intent to prevent obstetric fistula recurrence=0.81, attitude towards obstetric fistula recurrence prevention=0.86, self-esteem=0.78, and quality of life=83).
Data Collection Procedure
Data collectors and supervisors were trained for two days to acquaint them with the research instruments and objectives. Data were collected through face-to-face interviews with fifteen MSc Midwives and supervised by five senior MSc Midwifery staff.
Statistical Analysis
Data were entered into Epi data version 3.5.3 (Odense Denmark) for double data entry verification and then exported to International Business Machines Corporation Statistical Product and Service Solutions (IBM SPSS) version 23 for analysis. Descriptive statistics such as frequency and percentages were done to summarize socio-demographic and reproductive health-related variables. Item total scores were computed for eight intent items each on five Likert scales, and then the medians of each item, the mean intent score, and standard deviations were estimated. Independent variable items’ total scores, value labels, and dummy coding was also made for attitude, knowledge, and self-esteem; which were then categorized as positive/negative attitude, high/low knowledge, and high/low self-esteem based on below half/ above half of each factor’s item total scores (S1 Table). Simple and multiple linear regression analyses were used to test the predicting factors of intent to prevent fistula recurrence. All assumptions of linear regression were tested and satisfied. First, all socio-demographic characteristics and reproductive health-related factors were regressed on the dependent variable using simple linear regression. Then all significant variables were analyzed using multiple linear regression. Statistical significance was declared at P < 0.05.
Results
Socio-Demographic Characteristics of Women with Obstetric Fistula
Out of the 499 women who were contacted for the interview, 478 were included in the study. Twenty-one women were excluded from the study per the exclusion criteria. Among those included in this study three-fourths (75.5%) were rural residents, 60.6% were married, more than two-thirds (83.5%) of the women’s occupation was unpaid employment and two-thirds (66.3%) of them were not able to read and write. (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Women with an Obstetric Fistula at Fistula Centers of Addis Ababa and Oromia, 2019 (n=478) |
Reproductive Health Characteristics of Women with Obstetric Fistula
At the time of this study, nearly half (48.3%) of the women were waiting for their turn to get fistula repair and among those who got treatment, more than a quarter (27.5%) had been successfully repaired. Above half (56.5%) had lived with fistula from six weeks to two years. Close to half (45.4%) and a bit more than half (55.9%) of them had a low level of knowledge of the risk factors of obstetric fistula recurrence and had a negative attitude towards the prevention of obstetric fistula recurrence, respectively (Table 2).
 |
Table 2 Reproductive Health-Related Factors of Women with an Obstetric Fistula at Fistula Centers of Addis Ababa and Oromia, 2019 (n=478) |
Intent to Prevent Fistula Recurrence Among Women with Obstetric Fistula
The mean score of intent to prevent fistula recurrence among women with obstetric fistula was 27.72 ± 5.06 (Table 3). The intent items’ median score revealed that six items had a median of four, indicating women’s agreement with the items. Median scores for the intent items of using vaginal delivery and traditional medicine to prevent fistula recurrence were three and two, indicating women’s uncertainty and disagreement with the items, respectively (Figure 2).
 |
Table 3 Intent to Prevent Fistula Recurrence and Items Mean Score Among Women with Obstetric Fistula at Fistula Centers of Addis Ababa and Oromia, 2019 (n=478) |
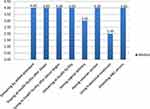 |
Figure 2 Intent items median scores among women with an obstetric fistula at fistula centers of Addis Ababa and Oromia, 2019 (n=478). |
Predictors of Intent to Prevent Fistula Recurrence Among Women with Obstetric Fistula
A multiple regression analysis revealed that predictors explained 43% of the variance in the intent to prevent fistula recurrence (F (27, 212) =5.96, P<0.001). Women’s previous living site, marital status, number of previous repairs, length of time lived with fistula, self-esteem, knowledge of risk factors of fistula recurrence, attitude towards fistula recurrence prevention, and psychological health quality of life domain were significant predictors of the intent to prevent obstetric fistula recurrence at P < 0.05.
Women with obstetric fistula who lived in rural areas had a two-point lower intent score to prevent obstetric fistula recurrence than those who lived in urban areas (β=−2.27, P=001). Women with married marital status had a 1.71 higher intent score to prevent fistula recurrence than those who divorced (β=1.71, P=0.004). Women who had been living with a fistula for more than or equal to five years had a 1.82 higher intent score to prevent obstetric fistula recurrence compared to those who had been living with it for less than two years (β =1.82, P=0.01).
Women with obstetric fistula who had one previous repair had a 2.14 higher intent score to prevent fistula recurrence compared to those who had three and more repairs (β= 2.14, P=0.031). Similarly, women with obstetric fistula who had high self-esteem had a 1.42 higher intent score to prevent obstetric fistula recurrence than those who had low self-esteem (β =1.42, P=0.036). For every one-unit increase in the psychological health quality of life domain score of women with fistula, the intent to prevent fistula recurrence increases by 0.05 (β=0.05, P=0.038). Women with obstetric fistula who had a high level of knowledge on the risk factors of fistula recurrence and those who had a positive attitude towards fistula recurrence prevention had 3.12 and 2.33 higher intent scores to prevent fistula recurrence compared to their counterparts (β=3.12, P<0.001) and (β=2.33, P<0.001), respectively (Table 4).
 |
Table 4 Factors Predicted the Intent to Prevent Obstetric Fistula Recurrence Among Women with an Obstetric Fistula at Fistula Centers of Addis Ababa and Oromia, 2019 (n=478) |
Discussion
In this study, which included 478 women with obstetric fistula, the mean intent score to prevent obstetric fistula recurrence was 27.72 ± 5.06. Being married, living with fistula for more than five years, having a high knowledge of the risk factors of fistula recurrence, having high self-esteem, being healthy psychologically, having a single previous fistula repair, and having a positive attitude towards fistula recurrence prevention were positively related to the intent to prevent fistula recurrence. Living in rural areas was negatively related to the intent to prevent fistula recurrence.
In this study, the mean intent score of women with obstetric fistula towards prevention of fistula recurrence was low. This is because in this study most of the women with fistulas were rural residents and so may not have adequate awareness of the prevention of fistula; they had a negative attitude towards obstetric fistula recurrence prevention and most of the women’s previous repair outcome was unsuccessful which may influence their decision and need not to have further repair, these all may contribute to their low intent. This is in agreement with an explorative study conducted in Nigeria, which shows that the majority of the study participants’ intent to prevent obstetric fistula recurrence is very low related to their belief that the fistula has no cure and can be treated with herbal products by experienced traditional birth attendants.32
Those women with obstetric fistula who lived in rural areas had a lower intent score to prevent obstetric fistula recurrence compared to those who lived in urban areas. This might be because those women who live in an urban setting have more access to maternal and obstetric care, fistula treatment centers, information about obstetric fistula recurrence risk factors, and obstetric fistula recurrence prevention measures than their rural counterparts. This is consistent with a study conducted in Burkina Faso, which indicates that women with fistulas who are rural residents have less preventive knowledge of recurrent fistulas than urban residents.14 Similarly, women with married marital status had a higher intent score to prevent fistula recurrence than those who divorced. This is maybe women who are in union with their husbands, are more stabilized psychologically, and get more supports to prevent the recurrence of fistula than those who are divorced from marriage. A recent study in Kenya supports this premise that women with obstetric fistulas who are with their husbands, get financial and psychosocial support from spouses and family members and are better able to access repair care and adequate follow-up.33
In this study, women who had lived with obstetric fistula for more than or equal to five years had a higher intent score to prevent obstetric fistula recurrence than those who lived with obstetric fistula for less than two years. This may be because women who live more years with this devastating condition encounter more problems and complications related to fistula than those who live less with this condition and so more intend to prevent fistula recurrence to get relief from such problems. Furthermore, women who live more years with their fistulas may also get more chances of being counseled on risk factors of fistula recurrence and on the appropriate time to seek care. This is in line with a study conducted in Tanzania which depicts that the duration of living with a fistula before surgical repair greatly influences women’s experience after repair as well.34
Women with obstetric fistula who had a high level of knowledge on risk factors of fistula recurrence had a higher intent score to prevent obstetric fistula recurrence than those who had a low level of knowledge. This is because those women who have more knowledge of the risk factors of fistula recurrence have more plans and readiness to prevent obstetric fistula recurrence than those who have less knowledge. This is coherent with the findings of a study done in Cameroon which has shown that knowledge of risk factors influences intent to prevent obstetric fistula recurrence.35 A similar study in Benin & West Africa revealed that women with obstetric fistula may not know the actual risk factors of obstetric fistula recurrence and how to prevent it.36,37 A descriptive study conducted in Uganda also implies that most of the women with obstetric fistula have inadequate knowledge of whether the condition is repairable and 58.7% do not know whether it is preventable.38
Similarly, in this study, women with obstetric fistula who had a positive attitude towards fistula recurrence prevention had a higher intent score to prevent obstetric fistula recurrence than those who had a negative attitude towards fistula recurrence prevention. This may be because having a positive attitude towards fistula recurrence prevention measures makes women have more plans to prevent recurrence than those who have a negative attitude. This is consistent with the findings of a study conducted in Benin, which revealed that 56.6% of obstetric fistula respondents have a positive attitude and feel that hospital delivery is an obstetric fistula recurrence preventive measure.39 However, a study conducted in Pakistan shows that despite the availability of transport throughout the community, women’s attitude towards health care facility delivery is poor, and cannot access emergency obstetric care and are intended to deliver by unskilled personnel.40 A study conducted in Eritrea among women with obstetric fistulas also shows that they perceive health facilities as unlucky and filled with evil and as a result, most women labor at home with the assistance of older female relatives, neighbors, and traditional birth attendants, showing that women with obstetric fistulas who have a negative attitude towards professional care are at greater risks of developing obstetric fistula recurrences.4
Women with high self-esteem had a higher intent score to prevent fistula recurrence than those with low self-esteem. Similarly, in this study, as the women’s psychological health improves/increases, their intent to prevent fistula recurrence also increases. These indicate that having high self-esteem and being fit psychologically makes women plan more for the prevention of fistula recurrence. This is coherent with the study conducted in Zambia, which depicted that fistula patients who are ashamed of themselves due to vaginal leaking fell into a deeper emotional decline, which in turn affected their self-esteem not to seek care for help to prevent obstetric fistula recurrence.41
Women who had one previous repair had a higher intent score to prevent fistula recurrence than those who had more repeated repairs. This is because as the number of obstetric fistula recurrences and repeated repairs increases, the chance to be a successful repair decreases, which may put the women in despair for not seeking further repair and diminish their intent to prevent the recurrence of the fistula. This is supported by the study in Niger, which shows that success rates decreased with increasing numbers of previous attempts at surgical repair.7 Furthermore, a study conducted in Kenya shows that past unsuccessful repairs represent barriers to care-seeking among women living with obstetric fistulas.33
Strengths
This study has some strengths. First, it is an original study for determining the intent to prevent obstetric fistula recurrence among women with obstetric fistula in Ethiopia. Second, a relatively large sample of women with obstetric fistulas was included in the study. Third, this study is one of the few studies that assessed factors that predicted the intent to prevent obstetric fistula recurrence among women with fistulas in developing countries.
Limitations
This study has some limitations. First, it included women with obstetric fistula found only in five fistula treatment centers and used a consecutive sampling technique for feasibility purposes. Second, this study was cross-sectional by design, which might be subjected to recall bias while capturing past antecedents. Third, as obstetric fistula is a sensitive issue, there might also be a social desirability bias in accessing the real experiences of the study participants. Fourth, the lack of similar previous studies made it difficult to make enough comparisons.
Conclusion
In this study, the intent to prevent obstetric fistula recurrence among women with obstetric fistula was low. Residence, marital status, number of previous repairs, duration of living with the fistula, knowledge of risk factors, self-esteem, psychological health, and attitude towards fistula recurrence prevention were significant predictors of women’s intent to prevent fistula recurrence. Emphasis should be given to awareness creation among women with an obstetric fistula on the preventive measures of obstetric fistula recurrence, the risk factors of obstetric fistula recurrence, and attitudinal changes towards prevention of obstetric fistula recurrence. To prevent and end the recurrence of this tragic morbidity successfully, there should be community-based outreach interventions including early case identification and linkage to treatment centers, community education on fistula prevention, and health care providers training in the provision of compassionate care to ignite women’s early access to obstetric cares. Inclusive follow-up studies are needed to identify other potential factors influencing the intention to prevent fistula recurrence among women with obstetric fistula.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
The Institutional Review Board (IRB) of Jimma University approved the study; on 5 March 2019 (Ref.No:IRB 000281/2019). A letter of support was also secured from the Addis Ababa Hamlin Fistula Hospital head office and permissions were obtained from each fistula treatment center. Study procedures followed the Helsinki Declaration. Informed consent was obtained from the study participants after they were adequately informed and understood the objective/purpose of the study, confidentiality of the information, privacy, potential benefits and risks of the study, anonymity of their names, and their full right to refuse, withdraw, or completely reject part or all studies. Verbal consent of participation was obtained from each volunteer study participant, then they signed the consent form in the space provided within the participant information sheet with the assistance of data collectors. Additionally, the assent of those women below the age of 18 years was obtained with consent obtained from their parents or guardians. All necessary measures were taken and ensured the dignity, autonomy, interest, well-being, and rights of the study participants throughout the study.
Acknowledgments
The authors express the deepest gratitude to research assistants, health facility administrators, and health care providers for their respective support and guidance during the data collection process. Study participants are highly acknowledged for voluntarily providing information. Jimma University is greatly acknowledged for working on the ethical perspectives of the proposal and supporting us to do this study.
Author Contributions
BF and ZB made a significant contribution to the conception, execution, analysis, and interpretation of data. BF and LSD contributed to the study design, acquisition of data, statistical analysis, and interpretation. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received a student research fund for data collection from Jimma University. The funder has not played any role in the study design, collection of data, and development of this manuscript.
Disclosure
The authors declare that they have no competing interests.
References
1. Jokhio AH, Rizvi RM, Rizvi J, et al. Prevalence of obstetric fistula: a population-based study in rural Pakistan. BJOG. 2014;121(8):1039–1046. doi:10.1111/1471-0528.12739
2. Biadgilign S, Lakew Y, Reda AA, et al. A population-based survey in Ethiopia using questionnaire as a proxy to estimate obstetric fistula prevalence: results from demographic and health survey. Reprod Health. 2013;10(1):14. doi:10.1186/1742-4755-10-14
3. Landry E, Frajzyngier V, Ruminjo J, et al. Profiles and experiences of women undergoing genital fistula repair: findings from five countries. Glob Public Health. 2013;8(8):926–942. doi:10.1080/17441692.2013.824018
4. Maheu-Giroux M, Filippi V, Samadoulougou S, et al. Prevalence of symptoms of vaginal fistula in 19 sub-Saharan Africa countries: a meta-analysis of national household survey data. Lancet Glob Health. 2015;3(5):e271–e278. doi:10.1016/s2214-109x(14)70348-1
5. Cowgill KD, Bishop J, Norgaard AK, et al. Obstetric fistula in low-resource countries: an under-valued and under-studied problem–a systematic review of its incidence, prevalence, and association with stillbirth. BMC Pregnancy Childbirth. 2015;15(1):193. doi:10.1186/s12884-015-0592-2
6. Ahmed S, Tunçalp Ö. The burden of obstetric fistula: from measurement to action. Lancet Glob Health. 2015;3(5):e243–e244. doi:10.1016/S2214-109X(15)70105-1
7. Ouedraogo I, Payne C, Nardos R, et al. Obstetric fistula in Niger: 6-month postoperative follow-up of 384 patients from the Danja Fistula Center. Int Urogynecol J. 2018;29(3):345–351. doi:10.1007/s00192-017-3375-7
8. Fu J, Liang Z, Zhu Y, et al. Surgical repair of rectovaginal fistulas: predictors of fistula closure. Int Urogynecol J. 2019;30(10):1659–1665. doi:10.1007/s00192-019-04082-w
9. Okunola TO, Yakubu E, Daniyan B, et al. Profile and outcome of patients with recurrent urogenital fistula in a fistula center in Nigeria. Int Urogynecol J. 2019;30:197–201. doi:10.1007/s00192-018-3738-8
10. Rushwan H, Khaddaj S, Knight L, et al. Need for a global obstetric fistula training strategy. Int J Gynaecol Obstet. 2012;119 Suppl 1:S76–79. doi:10.1016/j.ijgo.2012.03.022
11. Kuruvilla S, Bustreo F, Kuo T, et al. The Global strategy for women’s, children’s and adolescents’ health (2016–2030): a roadmap based on evidence and country experience. Bull World Health Organ. 2016;94:398–400. doi:10.2471/BLT.16.170431
12. Letchworth P, MacLaren E, Duffy S. Obstetric fistula: a paradigm shift is needed in research and prevention. BJOG. 2018;125(8):925–928. doi:10.1111/1471-0528.15110
13. Adler A, Ronsmans C, Calvert C, et al. Estimating the prevalence of obstetric fistula: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13(1):246. doi:10.1186/1471-2393-13-246
14. Banke-Thomas AO, Kouraogo SF, Siribie A, et al. Knowledge of obstetric fistula prevention amongst young women in urban and rural Burkina Faso: a cross-sectional study. PLoS One. 2013;8(12):e85921. doi:10.1371/journal.pone.0085921
15. Moselle LT, Kohi TW, Mvungi A, et al. Waiting for attention and care: birthing accounts of women in rural Tanzania who developed obstetric fistula as an outcome of labor. BMC Pregnancy Childbirth. 2011;11:1–13. doi:10.1186/1471-2393-11-1
16. Moselle LT, Moland KM, Mvungi A, et al. Why give birth in health facility? Users’ and providers’ accounts of poor quality of birth care in Tanzania. BMC Health Serv Res. 2013;13:1–12. doi:10.1186/1472-6963-13-1
17. Mannava P, Durrant K, Fisher J, et al. Attitudes and behaviors of maternal health care providers in interactions with clients: a systematic review. Global Health. 2015;11(1):1–17. doi:10.1186/s12992-015-0117-9
18. Keya KT, Sripad P, Nwala E, et al. “Poverty is the big thing”: exploring financial, transportation, and opportunity costs associated with fistula management and repair in Nigeria and Uganda. Int J Equity Health. 2018;17:1–10. doi:10.1186/s12939-018-0777-1
19. Singh S, Thakur T, Chandhok N, et al. Perceptions and experiences of women seeking treatment for obstetric fistula. Birth. 2017;44(3):238–245. doi:10.1111/birt.12291
20. Meurice ME, Genadry RR, Bradley CS, et al. Identifying barriers to accessing information and treatment for obstetric fistula in Niamey, Niger. Proc Obstet Gynecol. 2016;6(2):1–13. doi:10.17077/2154-4751.1304
21. Nambala N, Mweemba P, Labib M. Women’s intention to prevent vesico vaginal fistula recurrence in two repair centres in Zambia. Med J Zambia. 2012;39:54–58.
22. Lufumpa E. Doos L and Lindenmeyer A. Barriers and facilitators to preventive interventions for the development of obstetric fistulas among women in sub-Saharan Africa: a systematic review. BMC Pregnancy Childbirth. 2018;18(1):155. doi:10.1186/s12884-018-1787-0
23. Gebresilase YT. A qualitative study of the experience of obstetric fistula survivors in Addis Ababa, Ethiopia. Int J Womens Health. 2014;6:1033. doi:10.2147/IJWH.S68382
24. Bakundane C. Knowledge, Attitude and Practice of Women Regarding Prevention of Obstetric Fistula at Kabale Regional Referral Hospital. International Health Sciences University; 2016.
25. Wall LL, Belay S, Haregot T, et al. A case-control study of the risk factors for obstetric fistula in Tigray, Ethiopia. Int Urogynecol J. 2017;28(12):1817–1824. doi:10.1007/s00192-017-3368-6
26. Tunçalp Ö, Tripathi V, Landry E, et al. Measuring the incidence and prevalence of obstetric fistula: approaches, needs, and recommendations. Bull World Health Organ. 2014;93(1):60–62. doi:10.2471/BLT.14.141473
27. Donnelly K, Oliveras E, Tilahun Y, et al. Quality of life of Ethiopian women after fistula repair: implications on rehabilitation and social reintegration policy and programming. Cult Health Sex. 2015;17(2):150–164. doi:10.1080/13691058.2014.964320
28. Barageine JK, Tumwesigye NM, Byamugisha JK, et al. Risk factors for obstetric fistula in Western Uganda: a case-control study. PLoS One. 2014;9(11):e112299. doi:10.1371/journal.pone.0112299
29. Ballard K, Ayenachew F, Wright J, et al. Prevalence of obstetric fistula and symptomatic pelvic organ prolapse in rural Ethiopia. Int Urogynecol J. 2016;27(7):1063–1067. doi:10.1007/s00192-015-2933-0
30. Webster J, Nicholas C, Vellacott C, et al. Validation of the WHOQOL-BREF among women following childbirth. Aust N Z J Obstet Gynaecol. 2010;50(2):132–137. doi:10.1111/j.1479-828X.2009.01131.x
31. Rosenberg M. 2. The measurement of self-esteem. In: Society and the Adolescent Self-Image. Princeton University Press; 2015:16–36.
32. Umoiyoho A, Inyang-Etoh E. Community misconception about the aetiopathogenesis and treatment of vesicovaginal fistula in northern Nigeria. Int Res J Med Bio Sci. 2012;1:193–198. doi:10.14194/ijmbr.136
33. Warren CE, Sripad P, Mwangi A, et al. “Sickness of shame”: investigating challenges and resilience among women living with obstetric fistula in Kenya. In: Global Perspectives on Women’s Sexual and Reproductive Health Across the Lifecourse. Springer; 2018:91–109.
34. Irani JN. Rebuilding Life: A Journey Through the Lives of Women Who Have Endured and Been Treated for Obstetric Fistula in Tanzania. The University of Bergen; 2012.
35. Tebeau PM, Maninzou SD, Jemma B, et al. Risk factors for obstetric vesicovaginal fistula at university teaching hospital Yaounde Cameroon. Int J Gynaecol Obstet. 2012;118(3):256–258. doi:10.1016/j.ijgo.2012.04.011
36. Maulet N, Berthé A, Traoré S, et al. Obstetric fistula “disease” and ensuing care: patients’ views in West Africa. Afr J Reprod Health. 2015;19(1):112–123.
37. Nathan LM, Rochat CH, Grigorescu B, et al. Obstetric fistulae in West Africa: patient perspectives. Am J Obstet Gynecol. 2009;200(5):e40–e42. doi:10.1016/j.ajog.2008.10.014
38. Meurice M, Genadry R, Heimer C, et al. Social experiences of women with obstetric fistula seeking treatment in Kampala, Uganda. Ann Glob Health. 2017;83(3–4):541–549. doi:10.1016/j.aogh.2017.07.003
39. Gharoro E, Agholor K. Aspects of psychosocial problems of patients with vesicovaginal fistula. J Obstet Gynaecol. 2009;29(7):644–647. doi:10.1080/01443610903100609
40. Farid FN, Azhar M, Samnani SS, et al. Psychosocial experiences of women with vesicovaginal fistula: a qualitative approach. J Coll Physicians Surg Pak. 2013;23:828.
41. Holme A, Breen M, MacArthur C. Obstetric fistulae: a study of women managed at the Monze Mission Hospital, Zambia. BJOG. 2007;114(8):1010–1017. doi:10.1111/j.1471-0528.2007.01353.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
