Back to Journals » Drug Design, Development and Therapy » Volume 15
The Potential Use of Ceftazidime-Avibactam Against Carbapenem Resistant Klebsiella pneumoniae Clinical Isolates Harboring Different Carbapenemase Types in a Thai University Hospital
Authors Nasomsong W , Nulsopapon P, Changpradub D , Pongchaidecha M, Pungcharoenkijkul S, Juntanawiwat P, Simsiriporn W, Santimaleeworagun W
Received 20 May 2021
Accepted for publication 24 June 2021
Published 16 July 2021 Volume 2021:15 Pages 3095—3104
DOI https://doi.org/10.2147/DDDT.S321147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Worapong Nasomsong,1 Parnrada Nulsopapon,2,3 Dhitiwat Changpradub,1 Manat Pongchaidecha,2 Supanun Pungcharoenkijkul,4 Piraporn Juntanawiwat,5 Waristha Simsiriporn,5 Wichai Santimaleeworagun2,3
1Division of Infectious Diseases, Department of Internal Medicine, Phramongkutklao Hospital and College of Medicine, Bangkok, Thailand; 2Department of Pharmacy, Faculty of Pharmacy, Silpakorn University, Nakhon Pathom, Thailand; 3Pharmaceutical Initiative for Resistant Bacteria and Infectious Diseases Working Group [PIRBIG], Faculty of Pharmacy, Silpakorn University, Nakhon Pathom, Thailand; 4Pharmacy Unit, Nopparat Rajathanee Hospital, Bangkok, Thailand; 5Division of Microbiology, Department of Clinical Pathology, Phramongkutklao Hospital, Bangkok, Thailand
Correspondence: Wichai Santimaleeworagun
Department of Pharmacy, Faculty of Pharmacy, Silpakorn University, Nakhon Pathom, 73000, Thailand
Tel +6634 255 800
Fax +6634 255 801
Email [email protected]
Purpose: MBL and OXA-48 genes in carbapenem-resistant Enterobacterales (CRE) have emerged as a major public health problem worldwide, including Thailand. Due to the lack of susceptibility data and dosing regimens of ceftazidime-avibactam (CZA) against CRE in Thailand, especially in colistin-resistant era, we aimed to demonstrate in vitro susceptibility data of CZA and optimal dose based on Monte Carlo simulation of CZA to expand the treatment options.
Patients and Methods: We collected 49 carbapenem-resistant Klebsiella pneumoniae (CRKP) clinical isolates from unique patients at Phramongkutklao Hospital (June–October 2020). CZA disk diffusion and E-test testing were performed to obtain minimum inhibitory concentration (MIC). Each drug regimen was simulated using the Monte Carlo technique to calculate the probability of target attainment (PTA) and the cumulative fraction of response (CFR).
Results: The most common genotypes of CRKP were blaOXA-48 (53.1%) and blaOXA-48 +blaNDM (42.8%). CZA showed 47.7% and 90.5% susceptible rate against all genotypes of carbapenemases and OXA-48 type CRKP isolates. The MIC50 and MIC90 of CZA against CRKP were 2 and > 256 μg/mL. The categorical agreement (CA) between disk diffusion and E-test testing of CZA against CRKP was 95.4%. The CZA dosing regimens of 2.5 g infused 2– 3 h every 8 h achieved ≥ 90% of the target of free ceftazidime plasma concentration over MIC (%fTime >MIC) ≥ 50% and 100% against isolates MICs of ≤ 8 and ≤ 8 μg/mL, respectively. The avibactam regimens also provided 100%fTime at 0.5 μg/mL. Based on CFR ≥ 90%, no CZA regimens were effective against all of the studied CRKP isolates except CRKP carrying OXA-48.
Conclusion: CZA exhibited a fairly susceptible rate among the OXA-48-positive isolates in Thailand. The current suggested dose of CZA with prolonged infusion appears appropriate to achieve the pharmacokinetic/pharmacodynamic targets of ceftazidime and avibactam against CRKP carrying blaOXA-48.
Keywords: CRE, metallo-beta-lactamase, Monte Carlo, oxacillinase
Introduction
The carbapenemase-producing enzyme in carbapenem-resistant Enterobacterales (CRE) has been since 1990.1,2 The global spread of CRE has become a major public health concern especially regarding limited treatment options, increasing challenges for clinicians.3–6 The principal mechanisms of CRE consist of β-lactamase activity combined with structural mutations and production of carbapenemases, enzymes that hydrolyze carbapenem antibiotics.7 According to the Ambler classification system, carbapenemases are classified by their molecular structures in three classes of β-lactamases, ie, class A, eg, Klebsiella pneumoniae carbapenemases [KPCs], B, metallo-β-lactamases [MBLs], eg, New Delhi metallo-β-lactamase [NDM-1], and D, eg, OXA-48 type carbapenemase. Class A and D carbapenemases enzyme require serine at their active sites, while class B, the MBLs, requires zinc for β-lactam hydrolysis. For this reason, the MBLs are uninhibited by commercially available β-lactamase inhibitors.7,8
The global spread of CRE has occurred involving different epidemic strains across the region.9 In Thailand, the prevalence of CRE rapidly increased from 1.4 to 2.2% from 2009 to 201110,11 to 10 to 15% from 2018 to 2019.12 The main carbapenemase enzymes in Thailand were MBLs (blaIMP-14 and blaNDM) and OXA type (blaOXA).10,11,13 A recent report from a Thai university hospital revealed the two most common genotypes among CRE isolates were blaNDM (blaNDM-1, −4, −5, −9) of 71.75% and blaOXA (blaOXA-48, −181, −232) of 50.22%.13
Ceftazidime-avibactam (CZA) is a combination antibiotic composed of broad-spectrum cephalosporin ceftazidime (CAZ) and the β-lactamase inhibitor avibactam (AVI).14,15 AVI is a member of a novel class of nonβ-lactam β-lactamase inhibitors, the diazabicyclooctanes, and acts as a reversible, covalent inhibitor.16 AVI retrieves the activity of ceftazidime by inhibiting Ambler class A, class C, and some class D β-lactamases, including the KPC and OXA-48 carbapenemases. Nevertheless, CZA is inactive against MBLs, such as NDM.16,17 CZA is indicated for treating complicated urinary tract and complicated intra-abdominal infections (combined with metronidazole) among adults. CZA displayed promising clinical results in treating CRE with limited treatment options and was recommended as a preferable antibiotic to treat infections caused by CRE in some guidelines.18,19
Data from the National Antimicrobial Resistance Surveillance Thailand Center (NARST), Klebsiella pneumoniae was the second most common bacterium and second most common bacterium overall isolated from blood specimens in 2019. Unfortunately, around 10% of K. pneumoniae isolates exhibit carbapenem resistance.20 Moreover, in our setting, Santimaleeworagun et al reported 17.3% of the studied 150 K. pneumoniae isolates from blood culture revealed colistin resistance.21
As described above, CZA seems an attractive agent for carbapenem resistant-K. pneumoniae (CRKP) treatment; however, the in vitro susceptibility data among CZA against CRKP in Thailand (either polymyxin susceptible or resistant clinical isolates) has never been reported. Thus, this study aimed to demonstrate in vitro CZA activity against CRKP either polymyxin intermediate or resistant clinical isolates. Additionally, we developed a potentially appropriate CZA dosage regimen based on Monte Carlo simulation to achieve pharmacokinetic/pharmacodynamic (PK/PD) targets for efficacy to increase the treatment options in CRE, especially in various types of MBLs and OXA type CRKP with or without colistin resistance.
Materials and Methods
Bacterial Isolate
The CRKP clinical isolates from unique patients were collected by the microbiology laboratory at Phramongkutklao Hospital, a 1200-bed teaching hospital of Phramongkutklao College of Medicine, Royal Thai Army, Bangkok, Thailand from June to October 2020. All studied CRKP isolated from patients underwent species identification as K. pneumoniae using matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS).
Antimicrobial susceptibility testing was performed using the broth microdilution method (Sensititre, TREK Diagnostic Systems, Inc., Cleveland, OH, USA) and was interpreted according to the recommendations of the Clinical and Laboratory Standards Institute (CLSI) 22 and the European Committee on Antimicrobial Susceptibility Testing (EUCAST).23 The CRKP isolate was defined as K. pneumoniae being resistant to at least one of the antibiotics imipenem, meropenem, doripenem or ertapenem.24 Colistin resistant K. pneumoniae (CoRKP) was included in the studied isolates with an MIC ≥4 µg/mL to colistin using the broth microdilution method according to the CLSI guidelines.22
The clinical specimen was part of the routine hospital laboratory procedure. The use of cultured pathogens from human specimens was approved by the institutional review board of the Royal Thai Army (Ethics number: Q011h/63) and was carried out in accordance with the approved guidelines.
Phenotypic Study of Antimicrobial Susceptibility Testing
CRKP isolates were subcultured on Mueller-Hinton agar (Becton, Dickinson and Company, Sparks, MD, USA). CAZ-AVI disk (30 µg/20 µg) (bioMérieux, Marcy-I’Etoile, France) as the Kirby–Bauer method was conducted following CLSI and EUCAST guidelines. E-test testing was also performed (Liofilchem, Teramo, Italy). CLSI criteria were used to interpret MICs and disk diffusion zone diameters.22,25 Categorical agreement (CA) was defined using standardized criteria. In the present study, CA was defined as a more than 90% agreement in interpretive results between the E-test and disk diffusion.26
Molecular Study of Resistant Genes in Carbapenem Resistant K. pneumoniae
All CRKP isolates were freshly cultured on Mueller-Hinton broth (Beckton Dickinson Company, Baltimore, MD, USA) at 35°C. Then the genomic DNA of the clinical CRKP isolate was extracted using a commercial kit (Thermo Fisher Scientific, Waltham, MA, USA). Multiplex-PCR as previously described was used to detect carbapenemase genes (IMP, VIM, KPC, NDM, and OXA-48) to confirm carbapenem resistance mechanisms via enzyme destroying carbapenems.27 PCR mixture and PCR condition for mcr-1 (305 bp) were as previously described.28 PCR was conducted using a Thermocycler (Biometra, Gottingen, Germany). The PCR amplicons were visualized using a UV light box after electrophoresis on a 1% agarose gel comparing the band of known carbapenemase and mcr-1 genes as positive control along with the 1 kb plus DNA ladder (Thermo Fisher Scientific)
Monte Carlo Simulation
All pharmacokinetic parameters obtained from published studies of ceftazidime and avibactam among critically ill patients were collected.29 The concentration versus time curve was generated using a one-compartment model for CAZ and AVI. The targeted PK and PD indexes of ceftazidime were represented as the percentage of free drug time exceeding MIC (%fTime>MIC), and the target value was 50 and 100%. However, avibactam has free trough concentrations (fCtrough) exceeding 1 µg/mL at least 50% of the time interval between doses or had a fCtrough exceeding 0.5 µg/mL of the entire time interval of CZA administration for the remaining enzyme inhibitor activity.30
The optimized dosing regimens of ceftazidime and avibactam were identified using Monte Carlo simulations (Oracle Crystal Ball Classroom Faculty Edition-Oracle 1-Click Crystal Ball 201, Thailand). The Monte Carlo simulation produced 10,000 subjects based on the PK parameters of the studied antibiotics to generate the drug concentration over 24 h. The %fTime>MIC (CAZ) and trough concentrations exceeding 0.5 and 1 µg/mL (AVI) were analyzed to indicate the efficacy in each regimen.
The simulation was conducted for various CAZ and AVI dosing regimens. The PTA was estimated at each MIC, and the CFR was calculated as the sum of each %PTA against the antibiotic MIC distributions for CRKP. Dosing regimens that reached above 90% of PTA and CFR were highly recommended for documented therapy and empirical therapy against CRAB, respectively.
Results
In vitro Susceptibility of Ceftazidime-Avibactam and Comparator Agents
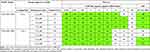
Forty-nine strains of CRKP from unique patients were isolated. The susceptibility result of CZA and other comparator agents are shown in Table 1. The most susceptible agents were amikacin (97.9%) and gentamicin (91.8%). Among these isolates, colistin MIC ≤2 µg/mL, which was interpreted as intermediate susceptible, exhibited only 67.3%. Tigecycline displayed a very low MIC90 of 1 µg/mL.
 |
Table 1 In vitro Susceptibility and Percentage of Susceptibility Among Ceftazidime-Avibactam (CZA) and Comparator Agents Against Carbapenem-Resistant Klebsiella pneumoniae (CRKP) Clinical Isolates |
Among 44 isolates, CZA showed 47.7% (21 of 44 isolates) and 90.5% (19 of 21 isolates) susceptible rate for all carbapenemase types and for OXA-48 type CRKP isolates, respectively. Whereas, CZA showed 100% and 38.9% susceptible rate for colistin intermediate KP (CoIRKP) isolates and CoRKP, respectively. The MIC50 and MIC90 of CZA against CRKP were 2 and >256 µg/mL. The MIC distribution of CZA against CRKP isolates using the E-test method is shown in Table 2. All the CZA resistant K. pneumoniae strains exhibited an extremely high MIC of >256 µg/mL while the susceptible strains exhibited a low MIC of ≤2 µg/mL. The categorical agreement between the E-test and disk diffusion of CZA against CRKP isolates was 95.4% (42 of 44 isolates) for CLSI interpretation and 54.5% (24 of 44 isolates) for EUCAST interpretation.
 |
Table 2 CZA Minimum Inhibitory Concentration Values, Zone Inhibition of CZA and Interpretive Categories by CLSI and EUCAST Against Various Carbapenemase Types of CRKP Clinical Isolates (n=49) |
Genotypic Characterization of Carbapenem-Resistant
K. pneumoniae Isolates
The most common genotypes of 49 CRKP isolates in this study were blaOXA-48 (53.1%) and co-existence between blaOXA-48 and blaNDM (42.8%). The CRKP carrying blaOXA-48 showed a promising susceptibility result of CZA at 90.5% susceptible. In contrast, in the presence of blaNDM regardless of the co-existence of other genotypes, CZA usually revealed a resistant pattern (Table 2).
PTA
Regarding PTA for various CZA regimens, for pathogens with an MIC of 8 µg/mL (the current susceptibility breakpoint for CZA), the optimal PTA target of fTime>MIC ≥50% was achieved in all studied regimens (Table 3). For ≥90% PTA target of fTime>MIC 100%, the current CZA recommended dose, namely, 2.5 g every 8 h, had to be infused longer up to 2 to 3 h to optimally cover CRKP with a CZA MIC of 8 µg/mL. Whereas, the regimen of 2.5 g every 8 h with standard infusion time (0.5 h) was effective against only isolates with CZA MICs of ≤4 µg/mL. This approach of prolonged infusion was also able to achieve a PK/PD index of AVI at a AVI fCtrough exceeding 0.5 µg/mL the entire time interval of CZA administration (Table 3).
CFR
Based on a CFR of ≥90%, no CZA regimens were effective against all studied CRKP isolates with various types of carbapenemase. Focusing on only CRKP isolates carrying only blaOXA-48, the optimal CFR target of fTime>MIC ≥50% was achieved in all studied CZA regimens. Whereas, for fTime>MIC 100%, regimens of 2.5 g infused longer times up to 2 to 3 h every 8 h showing CFR ≥90% among critically ill patients with OXA-48 type CRKP infection or isolates exhibiting susceptibility to CZA using disk diffusion based on CLSI guidelines (Table 4).
 |
Table 4 CFR (%) of CZA Regimens with Various Dosing Regimens According to Carbapenemase Types and Disk Diffusion Interpretation |
Discussion
The treatment options against CRKP are very limited. The most frequently used active antimicrobials so far have been “second-line” agents, including polymyxins, tigecycline, and aminoglycosides.31 Regarding the new β-lactamase inhibitors, AVI inhibits KPC and also OXA-48 but not MBLs. Because the options are so limited, all potentially active drugs should be tested in vitro including CZA.18,32 In Thailand, which shows a high epidemic rate of MBLs and OXA type CRE, the in vitro susceptibility result of CZA against CRE has never been reported.
In the present study, we demonstrated one half of CRKP isolates in a Thai university hospital was susceptible to CZA. Compared with other studies, the susceptible rate of CZA in CRE was diverse across the region, ranging from 53.3 to 96.6%.15,33–35 The genotype of epidemic CRE strains in each region was the key contributor to the CZA susceptible rate. In regions with a high susceptible rate of CZA, KPCs was the major epidemic genotype.15,34,35 Whereas, in the study of the Arabian Peninsula a susceptible rate of CZA (53.3%) against CRE was observed and OXA was the most common CRE genotype similar to our result.33 Hence, in a KPC epidemic region, CZA are recommended in some guidelines as the first-line antimicrobial agent against CRE.18
Categorical agreement between the E-test and disk diffusion of CAZ-AVI against CRKP was satisfactory, only based on CLSI guidelines. Verifications of the E-test and disk diffusion of CZA against CRKP, consisting of few strains of OXA and NDM type carbapenemase, have been studied, resulting in an acceptable essential and categorical agreement.25,36 The present study indicated the acceptable performance of CAZ-AVI (30 µg/20 µg) using the disk diffusion test among OXA and NDM type CRE. This additional information supported the use of the CAZ-AVI disk diffusion test based on CLSI interpretation among CRE which is more available in clinical practice than using the broth microdilution method (BMD) or E-test in some institutes, especially in a resource limited country.
Interestingly, colistin, the mainstream of CRE treatment, revealed an extremely high rate of resistance (81.63%) in the studied CRKP isolates compared with other studies in which the resistance rate did not exceed 15%.37,38 Increasing use of colistin to treat infections caused by Gram-negative bacteria as well as horizontal gene transfer between drug resistance Gram-negative bacteria might be principal factors leading to the emergence of CoRKP worldwide.39 The molecular mechanisms of these clinical isolates should be further investigated.
For optimal CZA dosage regimens against CRKP isolates for fTime>MIC 100%, the current CZA recommended dose, 2.5 g every 8 h, was effective against isolates with CZA MICs of ≤4 µg/mL in spite of the CZA MIC susceptible breakpoint specified at ≤8 µg/mL. Additionally, this dosage was not only sufficient for all range of susceptible strains, particularly the nearest MIC susceptible breakpoint but it also did not reach ≥90% PTA of AVI at 100%fT ≥ 0.5 µg/mL. The critical threshold of AVI at 0.5 µg/mL was considered appropriate to completely inhibit the various types of beta-lactamases in Enterobacterales.30 Thus, as our finding simulated CZA dosing regimens supported by a related report,40 the current recommended CZA dose of 2.5 g every 8 h has to be infused longer time up to 2 to 3 h to optimally cover CRKP with an CZA MIC of ≤8 µg/mL and also achieve the optimal PK/PD index of AVI.
Unfortunately, our data illustrated that no CZA regimen achieved a CFR of ≥90% for fTime>MIC either ≥50 or 100% against all studied carbapenemase types of CRKP isolates. Nevertheless, the role of CZA is hopefully for CRKP carrying OXA-48 showing a 90.5% susceptible rate. However, genotypic studies of carbapenemase types are not routinely used as treatment guidance for CRE infections. Fortunately, because the disk diffusion was the most frequently used technique in microbiology laboratories, we firstly showed the suitability of disk diffusion to define potential CZA use. The disk diffusion interpreted by CLSI breakpoint was capable to guide CZA use for CRKP treatment with CFR of more than 98% for fTime>MIC either ≥50 or 100%. Whereas, the disk diffusion interpreted by EUCAST breakpoint lacked the ability to predict the opportunity of CZA use. Therefore, the disk diffusion method only according to CLSI criteria could be applied in practical use in case of unavailable genotypic carbapenemases. Similarly, we caution the use of disk diffusion based on the EUCAST interpretation for susceptibility of phenotypes of Enterobacterales due to high rate of discordance between disk diffusion and E-test results.
Regarding limitations, this study established the first in vitro susceptibility report of CZA against CRKP either CoIKP or CoRKP isolates in Thailand and only a few reports in OXA and NDM type CRE in an endemic region. Nevertheless, limitations were encountered. First, the BMD method, which is the gold standard of antimicrobial susceptibility testing, was not performed. However, the E-test method is a simple and accurate alternative method for susceptibility testing and the CZA E-test verification study showed very high CA compared with BMD.25 Second, whole-genome sequencing of CRKP was not performed. Multiplex PCR could not fully describe the molecular basis of those resistant bacterial strains. Third, even though appropriate CZA doses were 2.5 g infused over 2 h every 8 h for critically ill patients based on with mean creatinine clearance of 103 mL/min,29 doses of CZA for patients with creatinine clearance less than 50 mL/min had to be adjusted for their renal function.17 Fourth, our study only recommended the possible dose of studied antibiotics to meet the PK/PD target in each drug. The clinical studies of our recommended dosing had to confirm the benefits of CZA-prolonged infusion against CRKP infections. Finally, this involved a limited single-center experience. Thus, the less generalizable findings should be appraised and compared with other cohorts. A nationwide multicenter study using standardized antimicrobial susceptibility testing methods based on various types of carbapenemase should be further investigated.
Despite these limitations, this study provided important information useful for treating CRKP in clinical practice especially in an epidemic region of OXA type CRE, for which treatment options are very limited. CAZ-AVI by disk diffusion exhibited acceptable performance as a leading treatment of OXA type CRE but only with susceptible interpretation based on CLSI criteria in the case of a lack of molecular carbapenemase typing confirmation. Furthermore, multilocus sequence typing with pulsed-field gel electrophoresis using K. pneumoniae isolates was not performed. Further study on clonal relatedness of tested strains should be investigated.
Conclusion
CZA exhibited 47.7 and 90.5% susceptible rate among all genotype and OXA type CRKP clinical isolates in a Thai university hospital. The CAZ-AVI disk diffusion test showed an acceptable performance in CRKP compared with the E-test method. From our result, CZA should be tested in vitro and considered as an alternative agent to treat CRE, especially in OXA type CRE endemic regions. Additionally, to fulfill both PK/PD indexes of CAZ and AVI, the current recommended dose, namely, 2.5 g infused over 2-3 h every 8 h, is considered an appropriate regimen to treat against CRE isolates showing susceptibility to CZA based on the current susceptibility breakpoint.
Acknowledgments
The authors would like to express gratitude to the Research and Creativity Fund, Faculty of Pharmacy, Silpakorn University (RAF 009/2564) for their financial sponsorship.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lauretti LRM, Mazzariol A. Cloning and characterization of blaVIM, a new integron-borne metallo-beta-lactamase gene from a Pseudomonas aeruginosa clinical isolate. Antimicrob Agents Chemother. 1999;43:1584–1590. doi:10.1128/AAC.43.7.1584
2. Osano EAY, Wacharotayankun R. Molecular characterization of an enterobacterial metallo beta-lactamase found in a clinical isolate of Serratia marcescens that shows imipenem resistance. Antimicrob Agents Chemother. 1994;38.
3. Munoz-Price LSPL, Bonomo RA. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13:785–796. doi:10.1016/S1473-3099(13)70190-7
4. Poirel LHC, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48:15–22. doi:10.1128/AAC.48.1.15-22.2004
5. Yong DTM, Giske CG. Characterization of a new metallo-betalactamase gene, bla(NDM-1), and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–5054. doi:10.1128/AAC.00774-09
6. Ranjan ASS, Mondal A. Molecular epidemiology and genome dynamics of New Delhi metallo-β-lactamase-producing extraintestinal pathogenic Escherichia coli strains from India. Antimicrob Agents Chemother. 2016;60:6795–6805. doi:10.1128/AAC.01345-16
7. Bush K, Jacoby GA. Updated functional classification of beta-lactamases. Antimicrob Agents Chemother. 2010;54(3):969–976. doi:10.1128/AAC.01009-09
8. Logan LK, Weinstein RA. The epidemiology of Carbapenem-Resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017;215(suppl_1):S28–s36. doi:10.1093/infdis/jiw282
9. van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence. 2017;8(4):460–469. doi:10.1080/21505594.2016.1222343
10. Netikul T, Kiratisin P. Genetic characterization of Carbapenem-Resistant Enterobacteriaceae and the spread of Carbapenem-Resistant Klebsiella pneumonia ST340 at a university hospital in Thailand. PLoS One. 2015;10(9):e0139116. doi:10.1371/journal.pone.0139116
11. Rimrang B, Chanawong A, Lulitanond A, et al. Emergence of NDM-1- and IMP-14a-producing Enterobacteriaceae in Thailand. J Antimicrob Chemother. 2012;67(11):2626–2630. doi:10.1093/jac/dks267
12. Antibiogram 2018–2019. National Surveillance System for. Antimicrobial Resistance. Thailand; 2019. Available from: http://narst.dmsc.moph.go.th/.
13. Laolerd W, Akeda Y, Preeyanon L, Ratthawongjirakul P, Santanirand P. Carbapenemase-Producing Carbapenem-Resistant Enterobacteriaceae from Bangkok, Thailand, and their detection by the Carba NP and modified Carbapenem Inactivation Method Tests. Microb Drug Resist. 2018;24(7):1006–1011. doi:10.1089/mdr.2018.0080
14. Falcone M, Paterson D. Spotlight on ceftazidime/avibactam: a new option for MDR Gram-negative infections. J Antimicrob Chemother. 2016;71(10):2713–2722. doi:10.1093/jac/dkw239
15. Sader HS, Castanheira M, Shortridge D, Mendes RE, Flamm RK. Antimicrobial activity of Ceftazidime-Avibactam tested against multidrug-resistant Enterobacteriaceae and Pseudomonas aeruginosa Isolates from U.S. Medical Centers, 2013 to 2016. Antimicrob Agents Chemother. 2017;61(11). doi:10.1128/AAC.01045-17
16. Wong D, van Duin D. Novel beta-lactamase inhibitors: unlocking their potential in therapy. Drugs. 2017;77(6):615–628. doi:10.1007/s40265-017-0725-1
17. van Duin D, Bonomo RA. Ceftazidime-avibactam and Ceftolozane/Tazobactam: second-generation β-Lactam/β-Lactamase inhibitor combinations. Clin Infect Dis. 2016;63(2):234–241.
18. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America Guidance on the Treatment of Extended-Spectrum β-lactamase Producing Enterobacterales (ESBL-E), Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with Difficult-to-Treat Resistance (DTR-P. aeruginosa). Clin Infect Dis. 2020;27:ciaa1478.
19. Temkin E, Torre-Cisneros J, Beovic B, et al. Ceftazidime-Avibactam as salvage therapy for infections caused by Carbapenem-Resistant organisms. Antimicrob Agents Chemother. 2017;61(2):e01964–01916. doi:10.1128/AAC.01964-16
20. The National Antimicrobial Resistant Surveillance Thailand. Antibiogram; Published 2019. Available from: http://narst.dmsc.moph.go.th/.
21. Santimaleeworagun W, Thunyaharn S, Juntanawiwat P, et al. The prevalence of colistin-resistant Gram-negative bacteria isolated from hospitalized patients with bacteremia. J Appl Pharm Sci. 2020;10(2):56–59.
22. Performance standards for antimicrobial susceptibility testing; 30th ed. CLSI supplement M100. Clinical and Laboratory Standard Institute; 2020. Available from: https://clsi.org.
23. The European Committee on Antimicrobial Susceptibility Testing. European Committee on Antimicrobial Susceptibility Testing Breakpoint tables for interpretation of MICs and zone diameters Version 11; Published 2021. Available from: http://www.eucast.org/clinical_breakpoints/.
24. Facility Guidance for Control of Carbapenem-resistant Enterobacteriaceae (CRE). Update - CRE Toolkit 2015. Centers for Disease Control and Prevention; 2015. Available from: www.cdc.gov.
25. Shields RK, Clancy CJ, Pasculle AW, et al. Verification of Ceftazidime-Avibactam and Ceftolozane-Tazobactam susceptibility testing methods against Carbapenem-Resistant Enterobacteriaceae and Pseudomonas aeruginosa. J Clin Microbiol. 2018;56(2). doi:10.1128/JCM.01093-17.
26. Patel JB, Sharp S, Novak-Weekley S. Verification of antimicrobial susceptibility testing methods: a practical approach. Clin Microbiol Newsl. 2013;35(13):103–109. doi:10.1016/j.clinmicnews.2013.06.001
27. Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011;70(1):119–123. doi:10.1016/j.diagmicrobio.2010.12.002
28. Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–168. doi:10.1016/S1473-3099(15)00424-7
29. Stein GE, Smith CL, Scharmen A, et al. Pharmacokinetic and pharmacodynamic analysis of Ceftazidime-avibactam in critically ill patients. Surg Infect (Larchmt). 2019;20(1):55–61. doi:10.1089/sur.2018.141
30. Nichols WW, Newell P, Critchley IA, Riccobene T, Das S. Avibactam pharmacokinetic/pharmacodynamic targets. Antimicrob Agents Chemother. 2018;62(6). doi:10.1128/AAC.02446-17
31. Morrill HJ, Pogue JM, Kaye KS, LaPlante KL. Treatment options for Carbapenem-resistant Enterobacteriaceae infections. Open Forum Infect Dis. 2015;2(2):ofv050–ofv050. doi:10.1093/ofid/ofv050
32. Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Machuca I, Pascual A. Treatment of infections caused by Extended-Spectrum-Beta-Lactamase-, AmpC-, and Carbapenemase-producing Enterobacteriaceae. Clin Microbiol Rev. 2018;31(2):e00079–00017. doi:10.1128/CMR.00079-17
33. Sonnevend Á, Ghazawi A, Darwish D, et al. In vitro efficacy of ceftazidime-avibactam, aztreonam-avibactam and other rescue antibiotics against carbapenem-resistant Enterobacterales from the Arabian Peninsula. Int J Infect Dis. 2020;99:253–259. doi:10.1016/j.ijid.2020.07.050
34. Zou C, Wei J, Shan B, Chen X, Wang D, Niu S. In vitro activity of Ceftazidime-Avibactam and Aztreonam-Avibactam against Carbapenem-resistant Enterobacteriaceae isolates collected from three secondary hospitals in Southwest China Between 2018 and 2019. Infect Drug Resist. 2020;13:3563–3568. doi:10.2147/IDR.S273989
35. Kim T, Lee SC, Bae M, et al. In vitro activities and inoculum effects of Ceftazidime-Avibactam and Aztreonam-Avibactam against Carbapenem-resistant Enterobacteralesisolates from South Korea. Antibiotics (Basel. 2020;9(12). doi:10.3390/antibiotics9120912.
36. Sader HS, Rhomberg PR, Chandrasekaran S, et al. Correlation between broth microdilution and disk diffusion results when testing Ceftazidime-Avibactam against a challenge collection of Enterobacterales isolates: results from a multilaboratory study. J Clin Microbiol. 2020;58(4). doi:10.1128/JCM.01757-19.
37. Rojas LJ, Salim M, Cober E, et al. Colistin resistance in Carbapenem-Resistant Klebsiella pneumoniae: laboratory detection and impact on Mortality. Clin Infect Dis. 2017;64(6):711–718. doi:10.1093/cid/ciw805
38. Amladi AU, Abirami B, Devi SM, et al. Susceptibility profile, resistance mechanisms & efficacy ratios of fosfomycin, nitrofurantoin & colistin for carbapenem-resistant Enterobacteriaceae causing urinary tract infections. Indian J Med Res. 2019;149(2):185–191. doi:10.4103/ijmr.IJMR_2086_17
39. Bialvaei AZ, Samadi Kafil H. Colistin, mechanisms and prevalence of resistance. Curr Med Res Opin. 2015;31(4):707–721. doi:10.1185/03007995.2015.1018989
40. Soukup P, Faust AC, Edpuganti V, Putnam WC, McKinnell JA. Steady-State Ceftazidime-Avibactam serum concentrations and dosing recommendations in a critically ill patient being treated for Pseudomonas aeruginosa Pneumonia and Undergoing Continuous Venovenous Hemodiafiltration. Pharmacotherapy. 2019;39(12):1216–1222. doi:10.1002/phar.2338
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.