Back to Journals » Infection and Drug Resistance » Volume 15
The Pattern of Antimicrobial Prescription at a Tertiary Health Center in Egypt: A Point Survey and Implications
Authors Ashour RH , Abdelkader EA, Hamdy O, Elmetwally M, Laimon W, Abd-Elaziz MA
Received 8 July 2022
Accepted for publication 13 October 2022
Published 31 October 2022 Volume 2022:15 Pages 6365—6378
DOI https://doi.org/10.2147/IDR.S380693
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Rehab H Ashour,1,2 Eman A Abdelkader,3 Omar Hamdy,4 Mohamed Elmetwally,4 Wafaa Laimon,5 Mohamed A Abd-Elaziz1
1Clinical Pharmacology Department, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 2Pharmacology & Toxicology Department, Faculty of Medicine at Al-Qunfudah, Umm Al-Qura University, Al-Qunfudah, Kingdom of Saudi Arabia; 3Internal Medicine Department, Faculty of Medicine, Mansoura University, Specialized Medical Hospital, Mansoura, Egypt; 4Surgical Oncology Department, Faculty of Medicine, Oncology Center Mansoura University “OCMU”, Mansoura, Egypt; 5Pediatric Endocrinology and Diabetes Unit, Department of Pediatrics, Faculty of Medicine, Mansoura University, Mansoura University Children’s Hospital, Mansoura, Egypt
Correspondence: Rehab H Ashour, Clinical Pharmacology Department, Faculty of Medicine, Mansoura University, 60 El-Gomhoria Street, Mansoura, Al-Dakahlia, 35516, Egypt, Tel +2 01005409956, Fax +20 50 2248203, Email [email protected]; [email protected]
Background: The misuse of antimicrobials has major consequences, particularly antimicrobial resistance (AMR) and antimicrobials’ related adverse effects. So, the WHO proposed antimicrobial surveillance to improve antimicrobials use. This point prevalence survey (PPS) was conducted to illustrate the prevalence of antimicrobial use at Mansoura University hospitals (MUH), Egypt.
Methods: The survey process used was adapted from the European survey of antimicrobial resistance with modifications. The survey was conducted from 8 AM to 8 PM daily within 2 weeks.
Results: A total of 300 patients received antimicrobials and the prevalence rate of antimicrobial prescription was 79.15%. The major indications of antimicrobials were surgical prophylaxis followed by the treatment of community-acquired infection. The most commonly prescribed initial antimicrobial group was Aminopenicillin ± β-lactamase inhibitors. Although the purpose for antimicrobial administration was recorded in all cases, the stop/review history was recorded only in 19.6% and local guidelines were not available for 77.6% of antimicrobial prescriptions. The use of combined antimicrobials was common (46.6%), particularly in orthopedic and cardiothoracic surgery.
Conclusion: The prevalence of antimicrobial prescription at MUH was high which requires serious actions including reviewing the antimicrobial indication, implementing local prescription guidelines, initiating an antimicrobial stewardship program (ASP), and optimizing infection control measures.
Keywords: antimicrobial prescription pattern, Egypt, Mansoura, point prevalence survey, quality indicators
Key Points
- The WHO proposed antimicrobial surveillance to improve antimicrobial use.
- A total of 300 patients received antimicrobials, the prevalence rate was 79.15% at MUH.
- Surgical prophylaxis and treatment of community-acquired infection were the major indications.
- Aminopenicillin ± β-lactamase inhibitors were the most commonly prescribed.
- The combined antimicrobials were common in cardiothoracic and pediatric surgery.
Introduction
Since the evolution of antibiotics, the treatment of microbial infections has improved dramatically. Appropriate use of these antimicrobials led to a high cure rate of serious infectious diseases and reduced infection in the patient undergoing surgical interventions. However, the unwise use of antimicrobials has become a major health problem with either individual receiving unnecessary antibiotics or taking an improper antimicrobial course.1,2
Misuse, overuse, and abuse are interchangeable words used to describe the inappropriate use of antibiotics particularly when they are not the proper treatment. Unfortunately, it is a common practice in developing countries including Egypt due to multiple and interconnected factors.3 The most important of these factors are uncontrolled access to antibiotics, low patient compliance, and limited availability of health insurance systems which push the citizens to self-medication with antibiotics or refilling old prescriptions.4
Moreover, another important factor that determines the misuse of antimicrobials is the prescription pattern in the health care system which includes inappropriate antimicrobial prescription (ie, when not indicated), incorrect choice, dosage, or duration, lack of effective regulations by the health authority, and overuse in the animal industry and agriculture.5,6 Egypt is classified as a Low-Middle Income Country (LMIC). In a survey in Cairo, 74% of pharmacists agreed that there is a public misuse of antibiotics.7 Another study in Egypt reported that dentists tend to over-prescribe antibiotics.8
Misuse of antimicrobials has major consequences particularly the emergence of antimicrobial resistance (AMR) and antimicrobials’ related adverse effects. Competing AMR requires worldwide, district, and national programs to assess, implement, and improve antimicrobial practice.9,10 In 2018, the WHO announced that Egypt has framed its National Action Plan (NAP) for AMR. The Egyptian NAP objectives are community awareness of AMR, optimum human and animal use of antimicrobials, supporting the One Health action, and implementing rational antimicrobial practices.11 Raising community awareness requires targeting stakeholders including health professionals, and assessing their antimicrobial practice. So, the WHO proposed antimicrobial Point Prevalence Survey (PPS) as an approach to evaluate antimicrobial use and also to limit AMR.12 In addition, the WHO suggested performing Knowledge, Attitude, and Practice (KAP) studies in the community and the healthcare professionals to understand the problems behind antibiotics misuse and resistance.13
The European Surveillance of Antimicrobial Consumption (ESAC) Survey found that the prevalence of antimicrobial use among patients in different hospitals distributed in 20 countries was 30.1%.14 Repeated PPS in European countries showed an increased number of contributing hospitals to 172 and teaching and tertiary hospitals had significantly greater use of antimicrobial combination.15 Several studies have evaluated antibiotic use in LMICs and showed a high prevalence of antimicrobial use and resistance.16–18 A recent PPS in the Kurdistan region of Northern Iraq reported a high prevalence of antibiotic use (93.7%) and the 3rd generation cephalosporins were the top prescribed (52.6%).19
One study conducted in eighteen Egyptian hospitals reported that 59% of included patients received at least one antibiotic, and the 3rd generation cephalosporins were the most commonly prescribed with a percentage of 28.7;20 however, Mansoura University hospitals (MUH) were not included in this study. So, our study was designed to illustrate the prevalence and pattern of antimicrobial use at MUH to specify benchmarking data essential for initiating local antimicrobial guidelines and upgrading them to national antimicrobial stewardship programs (ASP). Also, to identify goals for infection control programs and quality improvement.
Participants and Methods
The study was conducted at MUH in July 2019 and involved only inpatients in the following departments/centers: General Surgery, Chest, Internal Medicine & its units, Oncology Center, and Children Hospital. These departments/centers were chosen because they have the highest number of patient admissions per day. MUH is a tertiary healthcare facility that includes 44 different departments and several specialized health centers with a total inpatient capacity of 1512 beds. The admission rate at MUH in the year 2017–2018 was 27,540 from the outpatient clinic and 17,935 emergency admissions.
Data Set
A multidisciplinary team of health professionals and academic staff surveyed the selected departments/centers. Training and piloting of the study process were performed for the survey team before starting the study. The survey was conducted from 8 AM to 8 PM daily within 2 weeks. The survey team performed a prospective data collection using a standardized case report form which primarily comprise a structured template for documenting antimicrobial use on the day of the survey as well as the total number of inpatients in each department. The survey form “Supplementary: Datasheet.pdf” was adopted from the ESAC survey14 with modifications. Antimicrobial use was defined as any inpatient who received systemic antimicrobial even if it was a single dose at the time of the survey. This survey focused on the systemic (not the topical) use of antimicrobials including systemic antifungal and antiviral drugs. Relevant data elements including patients’ characteristics, diagnosis, antimicrobials used, and their indication were retrieved. The antimicrobial indications were categorized as either prophylaxis (antimicrobials prescribed to prevent possible infection) or treatment (antimicrobials prescribed to cure either community- or hospital-acquired infections “CAI or HAI, respectively”).21 Data were collected from both the patients and the medical records.
Other information collected included quality indicators (QIs) of antimicrobial practice that were selected from previous PPS,16 eg, the indication of antimicrobial, the route of administration, dosages, dosing intervals, records of antimicrobial review/stop, and whether the choice of antimicrobial was based on local guidelines and/or clinical, radiological, or laboratory microbiological evidence from a relevant patient sample. Lastly, the prescribed antimicrobials were grouped according to the WHO AWaRe (Access, Watch, Reserve) classification.22
Statistical Analysis
Data were analyzed by statistical package for social sciences (SPSS version 24) for Windows 10.0. Continuous data were presented as the median and range and were analyzed by Kruskal–Wallis test followed by Mann–Whitney U-test. Categorical data were presented as frequencies and proportions and the X2 test or Fisher’s exact test was used for comparisons, as appropriate. Statistical significance was defined as p <0.05.
Results
Prevalence of Antimicrobial Use, Hospital Departments, and Patients’ Characteristics
A total number of 379 inpatients were hospitalized at MUH during July 16–29, 2019. Out of them, 300 patients received antimicrobials and were included in this point survey. This gives a prevalence rate of antimicrobial use of 79.15%. The majority of them were females (55.3%). These patients were distributed in various departments as follows: Specialized Medical Hospital “SMH” (n = 81), Orthopedics (n = 26), General Surgery (n = 25), Oncology center Mansoura University “OCMU” (n = 75), Intensive Care Units “ICUs” (n = 19), Cardiothoracic Surgery (n = 7), and Mansoura University Children Hospital “MUCH” (n = 67). The median age of adult patients (older than 18 years, 77.7%) was 54 years. Children (more than 28 days and up to 18 years) comprised 20% of cases with a median age of 2.5 years, followed by neonates (<28 days, 2.3%, 71.4% males) with a median age of seven days. The majority of the patients had one co-morbidity (49.0%); mostly malignancy (26.3%), Table 1.
 |
Table 1 Demographic Characteristics of Inpatients Admitted to MUH and Who Participated in Antimicrobial Point Prevalence Surveys |
Indications of the Prescribed Antimicrobials
The 300 patients involved in the survey received a total of 589 antimicrobial drugs. The indications were surgical prophylaxis (45.3%, n = 136), treatment of CAI (28.7.0%, n = 86), medical prophylaxis (17.0%, n = 51), and treatment of HAI (9.0%, n = 27). Antimicrobials were prescribed for medical prophylaxis to prevent infection in immune-compromised patients with several chronic co-morbidities.
Treatment of CAI was empirically started in 32 cases (37.2%); however, the infection was verified by imaging in 21 cases (24.4%), bacterial culture in 17 cases (19.8%), a laboratory test in 9 cases (10.5%), and presence of pus in 7 cases (8.1%). On the other hand, the antimicrobial prescription for HAI was mainly based on sample culture and imaging (37.0% and 29.6%, respectively).
The Source of Infection
Anatomically, the respiratory system was the most common infection site in community-acquired (9.7%) and hospital-acquired infections (6.7%). The body system involved was undefined in 3.3% of antimicrobial treatments; possibly bacteremia or septicemia. Surgical and medical prophylaxis without body system localization composed 45.3% and 16.0% of cases, respectively, Table 2.
 |
Table 2 Source of Infection for Antimicrobial Prophylaxis and/or Treatment |
Antimicrobials’ Quality Indicators (QIs)
Along with the global PPP recommendation, antimicrobial indications and dosage were recorded in all prescriptions at MUH. Nearly all antimicrobials were administered parenteral (n = 296/300, 98.6%) regardless of the ward type. The stop/review history was only reported in 19.6% of included inpatients (n = 59/300) with the highest reviewing percentage at MUCH-ICUs. At the time of the survey, local antimicrobial guidelines were lacking for about 77.6%; but, present at MUCH (surgical, medical wards, and ICUs). The presence of infection was verified in 25% of the participants either by clinical examination (the presence of pus), culture and sensitivity testing, imaging, or other laboratory tests (eg, CBC). The prescription of antimicrobials combination was reported an overall of 46.6% (n = 140/300) of surveyed inpatients. The top three specialties that reported high use of antimicrobials combination were orthopedic surgery, cardiothoracic surgery, and medical wards of children’s hospital, Table 3.
 |
Table 3 Quality Indicators of Antimicrobial Use at MUH, Egypt versus Previously Reported African Indicators |
More than 50% of the prescribed antimicrobials belonged to the “Access” WHO-AWaRe groups, with the frequency varying between the different wards although lower in medical wards, orthopedic surgery, and adult ICU indicating the high use of the “Watch” group in these departments. Overall, the use of antimicrobials from the “Reserve” group was the lowest across all the screened departments, Table 3.
Characteristics of Indication-Based Antimicrobial Use
Regarding antimicrobial use for surgical prophylaxis, a great proportion of patients started the selected drug after the surgical incision (n = 93/136, 68.38%). The duration of antibacterial prophylaxis for surgery was more than 24 hours in the majority of the patients (n = 134/136, 98.52%). This duration had a median of 3 days (range, 2–9 days). Single-dose preoperative prophylaxis was not used at all, Table 4.
 |
Table 4 Descriptive Statistics of Patients Who Received Antimicrobials for Surgical Prophylaxis, n (%) |
The duration of antimicrobial use for medical prophylaxis had a median of 3 days and ranged from 2 to 13 days (Mann–Whitney U-test, p < 0.001 vs surgical prophylaxis). While, the median duration of antimicrobial administration for treatment of CAI was 5 days (range, 2–21 days). The median duration of HAI was 8 days (range, 3–21 days) and it was not significantly different compared to the duration of treatment of CAI (Mann–Whitney U-test, p = 0.052).
Antimicrobial Drug Overview
The selection of antimicrobial drug classes varied among the departments. In surgical oncology, general surgery, pediatric departments, and cardiothoracic surgery, the most commonly prescribed initial antimicrobial drug group was aminopenicillin ± β-lactamase inhibitors. However, 3rd generation cephalosporins were the first group to be prescribed in the specialized medical hospital, ICUs, and orthopedic departments, Figure 1.
The use of antimicrobials combination was not uncommon; but, variable from one department to another. In general surgery and surgical oncology, the use of a single antimicrobial was the greatest with a percent of 88.0 and 82.67, respectively. The use of two antimicrobials was prevalent in orthopedic surgery (76.92%), pediatric medicine (62.5%), and ICUs (59.09%). Three antimicrobials were used frequently in cardiothoracic surgery (71.43%) and pediatric surgery unit (46.15%), Figure 2. There was no statistically significant difference between the prescription of a single antimicrobial agent in surgical versus medical prophylaxis (X2 test value = 0.755, p = 0.355) and treatment of CAI versus HAI (X2 test value = 0.333, p = 0.564).
The top five prescribed drug classes were aminopenicillin ± β-lactamase inhibitors (n = 130, 43.3%), 3rd generation cephalosporins (n = 87, 29.0%), fluoroquinolones (n = 26, 8.7%), 1st generation cephalosporins (n = 19, 6.3%), and 4th generation cephalosporins (n = 12, 4.0%). All these drugs were given 100% parenteral except ciprofloxacin (parenteral, 92.3%) and for variable duration according to their indication. The aminopenicillin ± β-lactamase inhibitors and 1st generation cephalosporins were used for surgical prophylaxis (64.7% and 14.0%, respectively). The 3rd generation cephalosporins were the top used for medical prophylaxis (66.7%). The 3rd generation cephalosporins and aminopenicillin ± β-lactamase inhibitors take the upper hand in the treatment of CAI (36.0% and 26.7%, respectively). The most commonly prescribed antimicrobials for HAI were aminopenicillin ± β-lactamase inhibitors (29.6%), 3rd generation cephalosporins (18.5%), fluoroquinolones (11.1%), and glycopeptides (11.1%). All the top 5 antimicrobials were more than 70% funded by MUH, Table 5.
 |
Table 5 Pharmaco-Epidemiology of Top Five Prescribed Initial Antimicrobials |
Analysis of adult prescribed daily dose (PDD) for the top 5 antimicrobials revealed that aminopenicillin ± β-lactamase inhibitors were prescribed in a dosage of 3 g/day in 80.5% of patients; ceftriaxone dosage was 2 g/day in 88.0% of patients; ciprofloxacin dosage was 750 mg/day in 53.8% of patients; cefazolin dosage was 2 g/day in 94.7% of patients; cefepime dosage was 2 and 3 g/day equally prescribed in 33.3% of patients. Dose adjustment was required in a percent of adult patients who received 3rd generation cephalosporins (36.7%), 4th generation cephalosporins (25.0%), fluoroquinolones (19.2%), and aminopenicillin ± β-lactamase inhibitors (2.3%), Table 5. Pediatric prescribed dosage for aminopenicillin ± β-lactamase inhibitors was 150 mg/kg/day in 88.4% of cases, ceftriaxone dosage was 100 mg/kg/day in 75.0% of cases, and cefepime dosage was 100 mg/kg /day in 66.3% of cases. Fluoroquinolones and 1st generation cephalosporins were not prescribed in our pediatric patient sample. In addition, no dose adjustment was required in all pediatric cases.
Table 6 shows that some patients received other medications which may interact with the prescribed antimicrobial drug. Examples of these drugs include: omeprazole was chronically used in 6.0% of patients; digoxin and warfarin were chronically used in 2.33% of patients, and theophylline was used temporarily in 0.67% of patients.
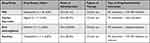 |
Table 6 Patient Medications Interacting with the Prescribed Antimicrobials |
Discussion
In the current study, we adopted the survey method used by the ESAC14 to determine the prevalence and pattern of antimicrobial use at Mansoura University Hospitals (MUH), Egypt. The present survey comes in line with the Egyptian NAP which includes conducting baseline surveys of antimicrobial use among health professionals as a prerequisite for the implementation of awareness programs.11 Our survey revealed a high prevalence of antimicrobial use, mostly given by intravenous route, with the preference for broad-spectrum groups and combinations, few targeted therapy, limited stop/review history, and a shortage of local antimicrobial prescribing guidelines. Although the current survey reported some good points like documentation of antimicrobial indication and dosage, it demonstrates the necessity of building up and adhering to local guidelines and implementing ASP to reduce the development of AMR in Egypt.
Our study revealed that 79.15% of the surveyed inpatients at MUH received one or more antimicrobial drugs. This percentage is higher than what was reported by one Egyptian study which stated a prevalence rate of 59% in eighteen participating Egyptian hospitals20 and also higher than a prevalence of 50.0% reported in Africa by the global PPP.16 Similar studies conducted in Europe showed a lower prevalence of antimicrobial drug use23 reaching 40.9% in 38 French hospitals.24 Several factors can affect the prevalence of antimicrobial use in different countries and hospitals. These factors may be related to patient characteristics and co-morbidities, the infection rate among hospital wards, and the effectiveness of infection control measures. Meanwhile, the current survey creates a good opportunity to improve antimicrobial use practices by implementing local guidelines and ASP aiming to limit the overall use of antimicrobials, associated side effects, and economic cost.
By reviewing the indications of antimicrobials in this survey, it was reported that surgical prophylaxis had the highest percentage accounting for 45.3% of all prescriptions compared to 23.2% in Africa by the global PPP.16 The timing of the first antimicrobial dose was after the incision in 68.38% of patients. In addition, most of the patients (98.52%) received long courses of prophylactic antimicrobials (>24 h). This MUH practice is not in agreement with the guidelines for antimicrobial prophylaxis in surgery recommended by the American Society of Health-System Pharmacists (ASHP)25 that recommend optimal time for administration of preoperative doses is within 60 min before surgical incision and a single antimicrobial dose or less than 24 hours course. In contrast, the European survey (ESAC) in 2009 demonstrated surgical antimicrobial prophylaxis was given for >24 h in 53% of patients.23 Similarly, long antimicrobial surgical prophylaxis duration was stated in 21% of patients in 38 French hospitals24 and all regions by the global PPP.16
The selection of antimicrobial agents varied according to the indication. Aminopenicillins ± β-lactamase inhibitors and 1st generation cephalosporins were the top two antimicrobials prescribed for surgical prophylaxis. Our results are in agreement with the French survey which reported that the 1st generation cephalosporins and penicillins combined with β-lactamase inhibitors were the most commonly used antibiotics for surgical prophylaxis.24 Likely, the choice of antimicrobial agent for surgical prophylaxis at MUH is in line with guidelines for surgical antimicrobial prophylaxis recommended by ASHP for most of the procedures.25 Contrarily, 1st generation cephalosporins, penicillins, and vancomycin represented only 12% of the whole antimicrobials provided for surgical prophylaxis in one Egyptian survey.20 Moreover, ceftriaxone was the top prescribed antimicrobial for surgical prophylaxis in Africa.16
Broad-spectrum antimicrobials such as 3rd generation cephalosporins were the mainstay for medical prophylaxis (39%) in the current survey. Compared to our findings, the French survey demonstrated the frequent use of co-trimoxazole (43.4%) and penicillin (16.1%) for medical prophylaxis.24 Similarly, co-trimoxazole was the most frequently used for medical prophylaxis (63.4%) worldwide.16 In a recent study, cephalosporins, anti-anaerobic, and vancomycin were the most commonly used drug classes across the internal medicine wards in Tikur Anbessa Specialized Hospital, Addis Ababa University, Ethiopia.26 Our findings highlight the importance to review with the physicians the exact indication of medical prophylaxis and avoid the unnecessary antimicrobial practice for inpatients. In an Egyptian survey, a large percentage of patients (14% of all antibiotic used) received antibiotics for medical prophylaxis with no medically accepted justification.20
Regarding the treatment of CAI, the 4th generation cephalosporins and fluoroquinolones were the most frequently used antimicrobials at MUH. Our results are in parallel with the European survey.14 On the other hand, the global PPP revealed that penicillins + β-lactamase inhibitor and the 3rd generation cephalosporins were the most commonly prescribed antibiotics for CAI followed by fluoroquinolones.16 Moreover, our survey revealed that aminopenicillin ± β-lactamase inhibitors, 3rd generation cephalosporins, fluoroquinolones, and glycopeptides were prescribed for HAI. In line with our findings, global PPP documented the use of penicillins with a β-lactamase inhibitor, fluoroquinolones, carbapenems, and glycopeptides for the treatment of healthcare-associated infections.16
Quality indicators (QIs) are used to assess antimicrobial prescription and set benchmarks for improvement. In the current survey, the indications of antimicrobial and dosage were reported in all cases which guarantee a good connection of diagnosis and treatment among all healthcare providers, and allow for reporting prescription reviewing and dose adjustment. In contrast, a lower percentage of reasoning was found in hospitals in Western (80.5%) Eastern (64%) and Southern (70%) Europe, Africa (70.4%), and Asia (73%).16 Parenteral antimicrobial administration is another QI that showed a high use percentage (98.6%) in our survey. Similarly, parenteral administration was common in eastern and southern Europe, Latin America, and West and Central Asia; although it was lower in Africa (62.7).16 This is probably due to the high use of broad-spectrum antimicrobials where their oral dosage forms are limited. Deciding the method of administration should be determined by some factors such as the infection severity, availability of an oral dosage form, and the sensitivity of the organism. Shifting from parenteral to oral administration of antimicrobials should be encouraged because it has many advantages including decrease in catheter-associated complications, costs, hospital stay, and is recognized as a key metric for stewardship programs in hospitals.27
Another QI is the stop/review history of the prescribed antimicrobial. In the present survey, it was reported to be 19.6%; meanwhile, it was 36.6% in Africa, 19.8% in West and Central Asia, and 51.6% in Northern Europe.16 Proper review of the antimicrobial administration within 48 h of the initiation, particularly when antimicrobials are started empirically, indicates the presence of a policy to prevent unnecessarily and/or long antimicrobial courses and ensures that the selected preparation and its administration route are appropriate for the patient when more diagnostic utilities become available.28
Concerns should be taken about the existence and adherence to local antimicrobial treatment guidelines. Unfortunately, local guidelines at MUH were not available in 77.6% of antimicrobial prescriptions. Also, a lack of treatment guidelines was reported among 19.2% of hospitals in the Global PPS and 26.7% in Africa; however, guidelines were more available in the West and Central Asia region (40.5%).16 Local guidelines are very crucial to monitor prescribing, improve adherence, and lower AMR. Hopefully, local guidelines were established at Mansoura University Oncology Center early in 2021 and more steps are going on at MUH.
In the current survey, the overall verification of infection and targeted treatment was 25% for antimicrobial prescription and greater in adult and pediatric ICUs. The global PPP documented nearly similar targeted antimicrobial treatment in Western Europe (26.1%), North America (23.9%), Latin America (26.5%); but a lower value in Africa (14.6%).16 This lower value of targeted therapy at MUH may be explained by greatly increased surgical prophylaxis at the time of the survey.
The current survey revealed that antimicrobial combination therapy is widely used in orthopedic and cardiothoracic surgery, ICUs, and pediatric medical wards. Similarly, 40% of patients in the French survey received more than one antimicrobial agent and one-third of them were hospitalized outside ICUs.24 The prescription of combined antimicrobial therapy outside ICUs is questionable and should be revised. Though, it was suggested that combination regimens may decrease mortality in severely ill patients with pneumococcal bacteremia29 and septic shock;30 such patients should be managed within ICUs according to the authors. Thus, it is important to further analyze the combined antimicrobial regimens prescribed at MUH to reach proper antimicrobial use.
We found that more than half of the prescribed antimicrobials in our survey were from the “Access” group of the WHO AWaRe classification,22 which have the highest use priority but retain the greatest risk of AMR. In addition, the relatively high use of the “Watch” group (43%) should be revised particularly the high use of ceftriaxone. However, the use of the “Reserve” group was low (5%) and mostly for HAI. In a recent PPP in Iraq, 62% of the prescribed antibiotics were from the “Watch” group and the “Reserve” group antibiotics were 9.8%.19
The WHO has set an adult-defined daily dose (DDD) for each antimicrobial agent which is the single most commonly prescribed daily dose worldwide. In the current survey, we reported that the prescribed daily dose (PDD) is the same as the DDD in the majority of patients who received parenteral aminopenicillins ± β-lactamase inhibitors, 1st and 3rd generation cephalosporins, and fluoroquinolones. Only 4th generation cephalosporins showed lower parenteral PDD than the WHO DDD in 33.3% of patients. This could be explained in part by variation in the drug choices, antimicrobial combination, and the duration of therapy and suggests that the WHO DDD should not be used as the sole measure of antimicrobial use.31
In this survey, we reviewed the drug history of the participants to assess possible drug–drug interactions with antimicrobials. Our results showed that 6% of the participants were on chronic oral omeprazole therapy. Omeprazole acts as an inhibitor of CYP2C19; thus, it can prolong the elimination of drugs that are metabolized by oxidation in the liver, eg, diazepam, warfarin, and phenytoin. Importantly, the combination of omeprazole with clarithromycin has been studied earlier because of its wide use in peptic ulcer treatment. Clarithromycin increased omeprazole plasma level which may affect either CYP3A4 substrates or hinder the absorption of drugs requiring gastric acidity.32 In addition, digoxin was reported to be prescribed to 2.33% of the participants in the current survey. Elevated digoxin serum concentration in patients receiving concomitant clarithromycin has been reported.33 Thus, serum digoxin concentration should be monitored in this situation.
Regarding oral anti-coagulants, our results showed that 2.33% of the participants were taking oral warfarin therapy at the time of the survey. It was reported that amoxicillin ± clavulanic acid led to an elevation of the INR when combined with warfarin, possibly by reducing vitamin K-producing gut flora.34 The FDA recommends close monitoring of prothrombin time and INR during and shortly after concomitant therapy with amoxicillin ± clavulanic acid or ciprofloxacin and warfarin. We surveyed also theophylline where only 0.67% of the participants received it for a temporal indication. It was reported that theophylline clearance was decreased by 19–32% when combined with ciprofloxacin (1000 mg).35–37 Moreover, clinafloxacin or grepafloxacin reduced theophylline clearance by about 50%.38,39 If concomitant use cannot be avoided, it is recommended to monitor serum theophylline levels and adjust dosage as appropriate to avoid adverse reactions.40
The current point survey has strong points and some limitations. The strength includes the use of a simple data collection form that grantee data uniformity and validation. This allowed a good opportunity for comparisons with national, regional, and global PPP results. In addition, we assessed several quantifiable QIs to highlight benchmarking standards for use in establishing treatment guidelines and ASP. The limitations are first, we did not include all MUH wards or the specialized centers in this survey. So, antimicrobial practice does not employ the whole MUH use; however, specific recommendations and guidelines may be inferred at the ward level. Second, this point survey was the first to be conducted at MUH with no previous data for comparison. Because of the great value of repeated point prevalence surveys,41 repeated point surveys at MUH would be considered in the future and would be easier in data collection and analysis due to the new era of electronic filing.
Conclusion
The current point survey is the first to be conducted at MUH to assess the antimicrobial practice within the inpatient wards. We used a validated survey adopted by the ESAC method and subsequently our data could be compared to worldwide surveillance. Although it reports a high prevalence of antimicrobial use and combined antimicrobial therapy at a tertiary center in Egypt, it highlights key points for improving antimicrobials practice including the establishment of local guidelines and the implementation of ASP. The QIs studied showed good documentation, limited stop/review history, minimal route switching, and few targeted therapies. In addition, the survey tracked some important drug–drug interactions common with antimicrobial use.
Abbreviation
ASP, Antimicrobial Stewardship Programs; AMR, Antimicrobial resistance; ASHP, American Society of Health-System Pharmacists; CAI, community-acquired infections; CYP, Cytochrome P450; DDD, defined daily dose; ESAC, European Surveillance of Antimicrobial Consumption; HAI, hospital-acquired infections; ICUs, Intensive Care Units; INR, International Normalized Ratio; LMICs, Low and Middle-Income Countries; MUH, Mansoura University hospitals; NAP, National Action Plan; PDD, prescribed daily dose; PPS, point prevalence survey; QIs, quality indicators.
Data Sharing Statement
Data are available on request.
Ethical Approval and Informed Consent
The survey proposal was accepted and approved by the Mansoura Faculty of Medicine – Institutional Research Board (MFM-IRB) under the code R.18.06.214. MFM-IRB works according to the principles stated in the Declaration of Helsinki and requires written informed consent to be taken from each participant (or a parent/legal guardian in the case of patients under the age of 18) before enrollment in the study.
Acknowledgments
We thank the MUH administration and colleagues at the specified departments for their cooperation.
Author Contributions
All authors made a significant contribution to the work reported, in the means of conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work”.
Funding
This study was conducted as part of our routine work and did not receive any funds from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14(8):742–750. doi:10.1016/S1473-3099(14)70780-7
2. Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003;163(8):972–978. doi:10.1001/archinte.163.8.972
3. Mittal AK, Bhardwaj R, Mishra P, Rajput SK. Antimicrobials misuse/overuse: adverse effect, mechanism, challenges and strategies to combat resistance. Open Biotechnol J. 2020;14(1):107–112. doi:10.2174/1874070702014010107
4. Abdulah R. Antibiotic abuse in developing countries. Pharm Regul Aff. 2012;1(2):1000e–1006e. doi:10.4172/2167-7689.1000e106
5. Vazquez-Lago JM, Lopez-Vazquez P, López-Durán A, Taracido-Trunk M, Figueiras A. Attitudes of primary care physicians to the prescribing of antibiotics and antimicrobial resistance: a qualitative study from Spain. Fam Pract. 2012;29(3):352–360. doi:10.1093/fampra/cmr084
6. Habibzadeh F. Use and misuse of antibiotics in the Middle East. Lancet. 2013;382(1). doi:10.1016/S0140-6736(13)61636-0
7. Zakaa El-din M, Samy F, Mohamed A, Hamdy F, Yasser S, Ehab M. Egyptian community pharmacists’ attitudes and practices towards antibiotic dispensing and antibiotic resistance; a cross-sectional survey in Greater Cairo. Curr Med Res Opin. 2019;35(6):939–946. doi:10.1080/03007995.2018.1544119
8. Aly MM, Elchaghaby MA. The prescription pattern and awareness about antibiotic prophylaxis and resistance among a group of Egyptian pediatric and general dentists: a cross sectional study. BMC Oral Health. 2021;21(1):1–8. doi:10.1186/s12903-021-01685-y
9. Boucher HW, Bakken JS, Murray BE. The United Nations and the urgent need for coordinated global action in the fight against antimicrobial resistance. Ann Intern Med. 2016;165(11):812–813. doi:10.7326/M16-2079
10. World Health Organization . Global antimicrobial resistance surveillance system (GLASS) report: early implementation 2020 https://www.who.int/publications/i/item/9789240005587
11. World Health Organiation. Egypt: National action plan for antimicrobial resistance; 2018. Available from: https://www.who.int/publications/m/item/egypt-national-action-plan-for-antimicrobial-resistance.
12. World Health Organization. Antimicrobial Resistance Global Report on Surveillance: 2014 Summary https://apps.who.int/iris/handle/10665/112642
13. World Health Organization. Antibiotic resistance: key facts. World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance.
14. Ansari F, Erntell M, Goossens H, Davey P; Group EIIHCS. The European surveillance of antimicrobial consumption (ESAC) point-prevalence survey of antibacterial use in 20 European hospitals in 2006. Clin Infect Dis. 2009;49(10):1496–1504. doi:10.1086/644617
15. Zarb P, Goossens H. European surveillance of antimicrobial consumption (ESAC). Drugs. 2011;71(6):745–755. doi:10.2165/11591180-000000000-00000
16. Versporten A, Zarb P, Caniaux I, et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Heal. 2018;6(6):e619–e629. doi:10.1016/S2214-109X(18)30186-4
17. Sulis G, Adam P, Nafade V, et al. Antibiotic prescription practices in primary care in low-and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2020;17(6):e1003139. doi:10.1371/journal.pmed.1003139
18. Sartelli M, Hardcastle C, Catena F, et al. Antibiotic use in low and middle-income countries and the challenges of antimicrobial resistance in surgery. Antibiotics. 2020;9(8):497. doi:10.3390/antibiotics9080497
19. Kurdi A, Hasan AJ, Baker KI, et al. A multicentre point prevalence survey of hospital antibiotic prescribing and quality indices in the Kurdistan Regional Government of Northern Iraq: the need for urgent action. Expert Rev Anti Infect Ther. 2020;19:1–10.
20. Talaat M, Saied T, Kandeel A, et al. A point prevalence survey of antibiotic use in 18 hospitals in Egypt. Antibiotics. 2014;3(3):450–460. doi:10.3390/antibiotics3030450
21. Cardoso T, Ribeiro O, Aragão I, Costa-Pereira A, Sarmento A. Differences in microbiological profile between community-acquired, healthcare-associated and hospital-acquired infections. Acta Med Port. 2013;26(4):377–384. doi:10.20344/amp.208
22. Sharland M, Pulcini C, Harbarth S, et al. Classifying antibiotics in the WHO essential medicines list for optimal use—be AWaRe. Lancet Infect Dis. 2018;18(1):18–20. doi:10.1016/S1473-3099(17)30724-7
23. Zarb P, Amadeo B, Muller A, et al. Identification of targets for quality improvement in antimicrobial prescribing: the web-based ESAC Point Prevalence Survey 2009. J Antimicrob Chemother. 2011;66(2):443–449. doi:10.1093/jac/dkq430
24. Robert J, Péan Y, Varon E, et al. Point prevalence survey of antibiotic use in French hospitals in 2009. J Antimicrob Chemother. 2012;67(4):1020–1026. doi:10.1093/jac/dkr571
25. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect. 2013;14(1):73–156.
26. Alemkere G, Tenna A, Engidawork E. Antibiotic use practice and predictors of hospital outcome among patients with systemic bacterial infection: identifying targets for antibiotic and health care resource stewardship. PLoS One. 2019;14(2):e0212661. doi:10.1371/journal.pone.0212661
27. Shrayteh ZM, Rahal MK, Malaeb DN. Practice of switch from intravenous to oral antibiotics. Springerplus. 2014;3(1):1–8. doi:10.1186/2193-1801-3-717
28. Pollack LA, Plachouras D, Sinkowitz-Cochran R, Gruhler H, Monnet DL, Weber JT. A concise set of structure and process indicators to assess and compare antimicrobial stewardship programs among EU and US hospitals: results from a multinational expert panel. Infect Control Hosp Epidemiol. 2016;37(10):1201. doi:10.1017/ice.2016.115
29. Baddour LM, Yu VL, Klugman KP, et al. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Respir Crit Care Med. 2004;170(4):440–444. doi:10.1164/rccm.200311-1578OC
30. Kumar A, Zarychanski R, Light B, et al. Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity-matched analysis. Crit Care Med. 2010;38(9):1773–1785. doi:10.1097/CCM.0b013e3181eb3ccd
31. Davey P, Ferech M, Ansari F, Muller A, Goossens H. Outpatient antibiotic use in the four administrations of the UK: cross-sectional and longitudinal analysis. J Antimicrob Chemother. 2008;62(6):1441–1447. doi:10.1093/jac/dkn386
32. Calabresi L, Pazzucconi F, Ferrara S. Pharmacokinetic interactions between omeprazole/pantoprazole and clarithromycin in healthy volunteers. Pharmacol Res. 2004;49(5):493–499. doi:10.1016/j.phrs.2003.10.010
33. Tanaka H, Matsumoto K, Ueno K, et al. Effect of clarithromycin on steady-state digoxin concentrations. Ann Pharmacother. 2003;37(2):178–181. doi:10.1177/106002800303700202
34. Davydov L, Yermolnik M, Cuni LJ. Warfarin and amoxicillin/clavulanate drug interaction. Ann Pharmacother. 2003;37(3):367–370. doi:10.1345/aph.1C243
35. Gillum JG, Israel DS, Scott RB, Climo MW, Polk RE. Effect of combination therapy with ciprofloxacin and clarithromycin on theophylline pharmacokinetics in healthy volunteers. Antimicrob Agents Chemother. 1996;40(7):1715–1716. doi:10.1128/AAC.40.7.1715
36. Batty KT, Davis TM, Ilett KF, Dusci LJ, Langton SR. The effect of ciprofloxacin on theophylline pharmacokinetics in healthy subjects. Br J Clin Pharmacol. 1995;39(3):305–311. doi:10.1111/j.1365-2125.1995.tb04453.x
37. Loi CM, Parker BM, Cusack BJ, Vestal RE. Aging and drug interactions. III. Individual and combined effects of cimetidine and ciprofloxacin on theophylline metabolism in healthy male and female nonsmokers. J Pharmacol Exp Ther. 1997;280(2):627–637.
38. Randinitis EJ, Alvey CW, Koup JR, et al. Drug interactions with clinafloxacin. Antimicrob Agents Chemother. 2001;45(9):2543–2552. doi:10.1128/AAC.45.9.2543-2552.2001
39. Efthymiopoulos C, Bramer SL, Maroli A, Blum B. Theophylline and warfarin interaction studies with grepafloxacin. Clin Pharmacokinet. 1997;33(1):39–46. doi:10.2165/00003088-199700331-00008
40. Fish DN. Fluoroquinolone adverse effects and drug interactions. Pharmacother J Hum Pharmacol Drug Ther. 2001;21(10P2):253S–272S. doi:10.1592/phco.21.16.253S.33993
41. Willemsen I, Groenhuijzen A, Bogaers D, Stuurman A, van Keulen P, Kluytmans J. Appropriateness of antimicrobial therapy measured by repeated prevalence surveys. Antimicrob Agents Chemother. 2007;51(3):864–867. doi:10.1128/AAC.00994-06
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


