Back to Journals » Vascular Health and Risk Management » Volume 19
The Outcomes of PBMV in Pregnancy, and When is the Best Time?
Authors Hussein A , Eid M , Mahmoud SED , Sabry M, Altaher A
Received 5 September 2022
Accepted for publication 5 January 2023
Published 14 January 2023 Volume 2023:19 Pages 13—20
DOI https://doi.org/10.2147/VHRM.S388754
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Takashi Kajiya
Ahmed Hussein,1 Mohamed Eid,1 Sharaf E D Mahmoud,1 Mohamed Sabry,2 Ali Altaher1
1Cardiology Unit, Department of Internal Medicine, Faculty of Medicine, Sohag University Egypt, Sohag, Egypt; 2Department of OB/GYN, Faculty of Medicine, Sohag University Egypt, Sohag, Egypt
Correspondence: Ahmed Hussein, Cardiology Unit, Department of Internal Medicine, Faculty of Medicine, Sohag University, Nasser City, Sohag, 82524, Egypt, Tel +2 01011145537, Fax +2 0934600349, Email [email protected]
Background: Percutaneous balloon mitral valvuloplasty (PBMV) is considered the most suitable option for managing symptomatic severe mitral valve stenosis (MS) during pregnancy with favorable anatomy. We do not know the best time to perform PBMV during pregnancy to achieve the best maternal and fetal outcomes. Therefore, we conducted this study to clarify the best procedure timing.
Methods: This prospective, observational, single-center study involved 44 pregnant patients suffering from symptomatic MS who underwent PBMV from May 2017 to May 2020. A detailed history is taken, full clinical examination, laboratory assessment, 2 D echocardiography, and follow-up during the hospital stay and monthly until labor.
Results: We found that the mean mitral valve area (MVA) had significantly increased from 1.12 ± 0.24 to 2.09 ± 0.46 cm2 (P < 0.001). The mean pressure gradient across the mitral valve reduced from 17.22 ± 5.55 to 8.94 ± 3.75 mmHg (P < 0.001). The procedures were successful in 91% of the patients. Regarding obstetric outcomes, the incidence of preterm labor, fetal death, and composite adverse outcomes was significantly lower in patients who had the procedure during the second trimester than those who had the procedure during the third trimester. All preterm deliveries and intrauterine fetal deaths occurred at least 21 days after PBMV. The patients showed a statistically significant improvement in NYHA functional classification.
Conclusion: We can conclude that PBMV performed in pregnant patients is an effective and safe treatment modality, and we observed better obstetric outcomes achieved with early intervention during the second trimester.
Keywords: rheumatic heart disease, mitral stenosis, PBMV, pregnancy, obstetric outcomes
Introduction
Rheumatic MS is a leading cause of acquired cardiovascular disease that complicates pregnancy. The increased hemodynamic burden related to pregnancy causes symptomatic deterioration, including higher blood volume, heart rate, mean left atrial pressure, and pulmonary venous pressure, which might induce pulmonary edema. Palpitation, chest discomfort, thrombosis, hepatomegaly, ascites, and edema are frequent signs of mitral stenosis.1 It is linked to bad maternal outcomes such as arrhythmia, pulmonary edema, and thromboembolism, as well as bad neonatal outcomes such as intrauterine growth retardation, preterm delivery, low birth weight, and neonatal or fetal death.2
Despite the availability of various non-invasive diagnostics, echocardiography is the preferred imaging method to evaluate MS patients.3 MS treatment options include medical therapy, PBMV, and surgery. In symptomatic individuals, medical therapy is the primary line of treatment. PBMV is a minimally invasive technique that can be used in both symptomatic and asymptomatic MS patients. Surgical management is suggested when PBMV is contraindicated in moderate-to-severe MS because of mitral regurgitation (MR).4 We do not know the best time to perform PBMV during pregnancy to achieve the best maternal and fetal outcomes. Therefore, we conducted this study to clarify the best procedure timing.
Methods
Design of the Study
From May 2017 to May 2020, we conducted our study on 44 pregnant patients with a symptomatic moderate-to-severe Rheumatic MS with a mean age of 29.51 ± 6.22 years, who underwent PBMV at the Cardiology Unit of the Sohag University Hospitals. All participants provided written informed consent prior to participating in the study. The study protocol conformed to the ethical guidelines of the 1975 Helsinki Declaration. The ethics committee of the Sohag Faculty of Medicine approved the study protocol https://medsohagedu-my.sharepoint.com/:b:/g/personal/ahmed_hussien_med_sohag_edu_eg/Ee1vaCiHnH5FgLK_VUjr0aMBOPI98CGEXSXW2K7tnSEfVw?e=5nmBLL. All participants gave informed written consent.
A full clinical and obstetric evaluation, electrocardiogram, transthoracic echocardiogram, and transesophageal echocardiography were done for all patients. The assessment of the severity of MS was done pre- and post-procedure using 2D and Doppler echocardiography. Valve area, mean transvalvular pressure gradient, degree of mitral regurge (MR) if present and valvular morphology were also assessed.
We included all patients fulfilling the criteria for being suitable for PBMV: 1) patients with New York Heart Association (NYHA) functional classification III or IV despite receiving optimum medical therapy; 2) echocardiographic assessment revealed moderate-to-severe MS with less than grade III mitral regurgitation; and 3) all patients exceeding their first trimester after 14 weeks of gestational age.
Evaluation of obstetric and fetal outcomes was done before, and immediately after the procedure, during the hospital stay, and monthly until delivery.
Patients with left atrial (LA) appendage thrombus by transesophageal echocardiographic assessment, acute rheumatic activity, the presence of coexisting infection, those with highly unfavorable mitral valve morphology, multi-valvular affection, the presence of massive or bi-commissural calcification, hypertension, or gestational diabetes were excluded.
Patients with a high MV score (>8) without the presence of significant commissural calcification, including 12 patients were referred for PBMV because they are considered to be at increased risk of cardiac surgery.
After consultation with senior obstetricians and inhibiting uterine contraction, patients received indomethacin (40 mg) rectal suppository 6 hours pre-procedure. For ensuring fetal safety and limited radiation exposure, we omitted left ventriculography. Fluoroscopy was used only when necessary. The patient’s abdomen and pelvis were shielded with a folded 5-mm lead Apron shield throughout the procedure.
For all patients, PBMV was done using the Inoue balloon technique. Septostomy &Trans septal catheterization with an 8F Mullins transseptal dilator and then transseptal left-sided catheterization were done in a standard method then anterograde mitral commissurotomy. Maternal outcomes were recorded through assessment of standard hemodynamics, including trans-mitral pressure gradient and pulmonary artery systolic pressure, throughout the procedure. All hemodynamic measurements were obtained both before and immediately after PBMV. Heparin was given (100 IU/kg of body weight) after the transseptal puncture. The Color Doppler technique was used to assess interatrial communication and the severity of MR. The size of the balloon was selected according to the patient’s body surface area modulated by the valve anatomy and confirmed the selection of the balloon size was by directly measuring the mitral annular diameter using 2-dimensional echocardiography. The maneuver is considered successful when meeting the criteria of the definition of optimal results referred to by “Block & Palacios”,5 In which a decrease in the transmitral pressure gradient of <10 mmHg, post-procedural MVA of ≥1.5 cm2, and an increase in MVA of >25% compared to MVA before dilatation.
Finally, patients were transferred to the intensive care unit of the cath lab for monitoring with full obstetric reassessment. 2D and Doppler echocardiographic evaluations were done 24 hours after PBMV.
The mode of delivery was decided based on obstetric indications, and a senior pediatrician assessed neonatal outcomes.
Analysis of Data
Data were analyzed using SPSS version 20. We performed the test of normality for the provided data (Shapiro–Wilk test), the p-value was >0.05, so the data were normally distributed, and we used a t-test. We analyzed Quantitative data using the Student’s t‐test to compare the means between groups. Qualitative data were compared using the Chi-square test and we used Fisher’s exact correction when the expected cell count is less than 5. A paired sample t‐test or Marginal homogeneity test was used to assess the significance between means when we compare paired samples. A P-value less than 0.05 is considered significant.
Results
As regards demographic and baseline characteristics, we found that the mean age of participating patients was 29.51 ± 6.22 (21–35 years). Forty patients were in class III NYHA functional classification and four patients were in class IV. The mean gestational age was 23.27 ± 7.11 weeks. The echocardiography score using Wilkin’s score showed 12 patients (27.3%) had Wilkin’s ˃8 (range 9–11) without the presence of significant commissural calcification (Table 1).
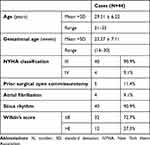 |
Table 1 Demographic and Baseline Data of Studied Patients |
As regards the procedure outcomes, the procedure significantly increased the presence of or the grade of MR (Table 2). Post-procedure, there was a significant decrease in the mean pulmonary artery systolic pressure (PASP), the mean LA pressure, and the mean transvalvular pressure gradient. The mean (MVA) was 1.12 ± 0.24 cm2 and had significantly increased to 2.09 ± 0.46 cm2 after balloon dilatation (P < 0.001) (Tables 3).
 |
Table 2 Mitral Regurge Before and After the PBMV Procedure |
 |
Table 3 Echocardiographic Parameters Before and After the PBMV Procedure |
MVA increased to ˃ 25% in all patients without the occurrence of a significant degree of MR. Four patients showed a ˃25% increase in MVA; however, the final area was still ˂1.5 cm2. Therefore, we achieved a 91% success rate. The patients showed a statistically significant improvement in NYHA functional classification (Table 4).
 |
Table 4 NYHA Functional Classification Before and After PBMV Procedure |
The mean procedural time was 50.24 ± 16.11 minutes with a range from 20 to 120 minutes. There were no reported major complications such as pericardial effusion and consequent tamponade, severe MR, thrombotic or embolic events and death.
Regarding obstetrics outcomes, the incidence of preterm labor was significantly lower in patients who had the procedure during the second trimester compared to those who had the procedure in the third trimester (p values = 0.03), while the incidence of low birth weight showed no significant difference. The incidence of intrauterine fetal deaths was significantly lower in patients who had the procedure during the second trimester compared to those who had the procedure in the third trimester (p values = 0.03). The incidence of composite adverse outcomes was significantly lower in patients who had the procedure during the second trimester compared to those who had the procedure in the third trimester (p values = 0.005) (Table 5, Figure 1).
 |
Table 5 Procedure Adverse Outcomes During the Second and Third Trimesters |
 |
Figure 1 Post procedure adverse obstetric outcomes during the second and third trimesters. |
All preterm deliveries and intrauterine fetal deaths occurred at least 21 days after PBMV, and so the obstetric complications mostly were not related to our procedure. All patients were delivered by cesarean section and no obstetric complications were observed.
Discussion
The changes in hemodynamics that occur during pregnancy may be considered a normal physiological adaptation to the 15–20% elevation in fetal oxygen consumption.7 The first trimester shows a 60% increase in blood volume above the non-pregnant.3,6–8 The Cardiac output (COP) starts to increase during the first trimester, reaching a peak of 30–45% over resting in non-pregnant women around the 20th-week gestation.2,3 Increased COP is related to reduced systemic vascular resistance, resulting in lower or no change in blood pressure and a wide pulse pressure range.3,7,8 An increase of about 10–20 beats/min of mean heart rate when reaching the term.7,8 Other cardiovascular changes occur during delivery due to increased demands. Pain during uterine contraction and the increased venous return from these contractions represents another 20% increase in COP.7 Another large amount of fluid shifts occurs during the postpartum period, normal pregnant women may have an elevation in COP reaching up to 65% immediately after delivery.6 The hemodynamic stress associated with pregnancy leads to decompensation of asymptomatic patients, especially those with moderate-to-severe MS.9,10
PBMV is considered the treatment of choice for MS during pregnancy if the anatomy is favorable. In our study, the mean gestational age was 23.27 ± 7.11 weeks at the time of PBMV, which was comparable to the previously published studies showing a range of 21–25 weeks, but different from a study conducted in India by Vijayvergiya R, who reported a mean gestational age 29.5 ± 6.68 weeks.11 The safety and effectiveness of PBMV during pregnancy have been shown by great clinical and hemodynamic outcomes.11–35 It is considered an excellent and beneficial procedure in many studies with a success rate of 82–94% and in some instances it reaches up to 100% of the patients.11,32–37 Similar results were found in our study, as we achieved a 91% success rate with a significant improvement in MVA and decreased transvalvular gradient and pulmonary artery pressure.
The incidence of occurrence of major complications was considerably low ranging from 0% in a study conducted by Fawzy et al38 up to 9% in a study conducted by Ben Farhat et al12 and continues to decrease as expertise in this procedure improves with time. Similar results were achieved in our study, as the major unfavorable outcomes were 0%.
According to the time of the procedure, whether in the second or third trimester of pregnancy. We found a significant difference in obstetric outcomes. The incidence of preterm labor, fetal death, and composite adverse outcomes was significantly lower in patients who had the procedure during the second trimester than those who had the procedure in the third trimester (p values = 0.034, 0.031, and 0.005, respectively). While the incidence of low birth weight shows no significant difference. While Vijayvergiyaet al11 found no statistically significant difference in the incidence of preterm labor, fetal death, or low birth weight in patients performed the procedure before 24 weeks of pregnancy compared to those who had the procedure after 24 weeks. But we considered the third trimester to start after 28 weeks of pregnancy, not after 24 weeks, that may have an impact on the different results. Other studies reported the adverse obstetric outcomes happened mainly during the third trimester that matches with our results.33–35 All preterm deliveries and intrauterine fetal deaths occurred at least 21 days after PBMV, and so the obstetric complications mostly were not related to our procedure.
Strengths of Our Study
To our knowledge, no previous study assessed the best time to perform PBMV to achieve the best maternal and fetal outcomes.
Limitations of Our Study
Our study has some limitations to be considered. Firstly, the relatively small number of patients limited the comparative data analysis of those collected in the current study. Secondly, we have no control group because it is non-ethical to leave pregnant women with significant symptomatic MS without intervention. Finally, data comparing PBMV in pregnant women in the second trimester versus those performed late in the third trimester are lacking, therefore comparing our data with other similar studies is not possible.
Conclusion
We can conclude that PBMV performed in pregnant patients is an effective and safe treatment modality, and we observed better obstetric outcomes achieved with early intervention during the second trimester.
Abbreviations
COP, cardiac output; LA, left atrium; MR, mitral regurge; MS, mitral stenosis; MVA, mitral valve area; NYHA, New York Heart Association; PASP, pulmonary artery systolic pressure; PBMV, percutaneous balloon mitral valvuloplasty.
Declarations
● Ethics approval and consent to participate: All subjects provided written informed consent to participate in the study. The study protocol was approved by:
1.Medical Research Ethics Committee, Sohag Faculty of Medicine, Sohag University. The committee reference number is not applicable. Date of approval, May 2017.
● Availability of data and materials: the datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
● Authors’ contributions: All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgments
We thank all the patients who participated in this study. We thank all the cardiology unit and obstetric department staff at Sohag University Hospital.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Vinayakumar D, Vinod G, Madhavan S., et al. Maternal and fetal outcomes in pregnant women undergoing balloon mitral valvotomy for rheumatic mitral stenosis. Indian Heart J. 2016;68:780–782. doi:10.1016/j.ihj.2016.04.017
2. Adhikari CM, Malla R, Rajbhandari R, et al. Percutaneous transvenous mitral commissurotomy in elderly mitral stenosis patients. A retrospective study at Shahid Gangalal National Heart Centre, Bansbari, Kathmandu, Nepal. Maedica. 2013;8:333–337.
3. Norrad RS, Salehian O. Management of severe mitral stenosis during pregnancy. Circulation. 2011;124:2756–2760. doi:10.1161/CIRCULATIONAHA.111.030601
4. Kannan M, Vijayanand G. Mitral stenosis and pregnancy: current concepts in anaesthetic practice. Indian J Anaesth. 2010;54:439–444. doi:10.4103/0019-5049.71043
5. Block PC, Palacios IF. Pulmonary vascular dynamics after percutaneous mitral valvotomy. J Thorac Cardiovasc Surg. 1988;96:39–43.
6. Clark SL, Phelan JP, Greenspoon J, et al. Labor and delivery in the presence of mitral stenosis: central hemodynamic observations. Am J Obstet Gynecol. 1985;152(8):984–988. doi:10.1016/0002-9378(85)90544-7
7. Ducey JP, Ellsworth SM. The hemodynamic effects of severe mitral stenosis and pulmonary hypertension during labor and delivery. Int Care Med. 1989;15:192–195. doi:10.1007/BF01058572
8. Bragwat AR, Engel PJ. Heart disease and pregnancy. CardiolClin. 1995;13:163–178.
9. Mehta LS, Warnes CA, Bradley E, et al. American Heart Association Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and Stroke Council. Cardiovascular Considerations in caring for pregnant patients: a scientific statement from the American Heart Association. Circulation. 2020;141:e884–e903. doi:10.1161/CIR.0000000000000772
10. Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165–3241. doi:10.1093/eurheartj/ehy340
11. Vijayvergiya R, Suri V, Sikka P, et al. Maternal and fetal outcomes following percutaneous transluminal mitral commissurotomy in pregnant women with critical mitral stenosis: an experience of a tertiary care center from Northern India. Anatol J Cardiol. 2022;26(7):552–558. doi:10.5152/AnatolJCardiol.2022.1644
12. Ben Farhat M, Gamra H, Betbout F, et al. Percutaneous balloon mitral commissurotomy during pregnancy. Heart. 1997;77:564–567. doi:10.1136/hrt.77.6.564
13. Smith R, Brender B, McCredie M. Percutaneous transluminal balloon dilatation of the mitral valve in pregnancy. Br Heart J. 1989;61:551–553. doi:10.1136/hrt.61.6.551
14. Esteves CA, Ramos AIO, Braga SN, et al. Effectiveness of percutaneous balloon mitral valvotomy during pregnancy. Am J Cardiol. 1991;68(9):930–934. doi:10.1016/0002-9149(91)90411-D
15. Brigui M, Remadi F, Belkhiria N, et al. Results of percutaneous mitral dilatation in 11 cases of poorly tolerated mitral stenosis during pregnancy. Ann Cardiol Angiol. 1994;43:129–134.
16. Drobinski G, Fraboulet P, Montalescot G, et al. Valvuloplastie mitrale au quatrième mois de grossesse. Protection foetale par un manteau de plomb [Mitral valvuloplasty during the 4th month of pregnancy. Fetal protection with a lead mantle]. Arch Mal Coeur Vaiss. 1991;84(2):249–251. French.
17. Gangbar EW, Watson KR, Howard RJ, et al. Mitral balloon valvuloplasty in pregnancy: advantages of a unique balloon. Cathet Cardiovasc Diagn. 1992;25:313–316.
18. Ledesma Velasco M, Ibarra Flores M, Campos Santaolalla A, et al. Percutaneous mitral commissurotomy with Inoue’s technique and pregnancy: the initial experience in Mexico. Arch Inst Cardiol Mex. 1993;63:335–338.
19. Loya YS, Desai DM, Sharma S. Mitral and pulmonary valvotomy in pregnant patients. Ind Heart J. 1993;45:57–59.
20. Mangione JA, Arie S, de Oliveira SA, et al. Valvoplastia mitral por cateter balão em pacientes grávidas. Relato de três casos [Mitral valvuloplasty with balloon catheterization in pregnant patients. Report of 3 cases]. Arq Bras Cardiol. 1989;52(2):99–101. Portuguese.
21. Mangione JA, Zuliani MF, Del Castillo JM, et al. Percutaneous double balloon mitral valvuloplasty in pregnant women. Am J Cardiol. 1989;64(1):99–102. doi:10.1016/0002-9149(89)90663-2
22. Palacios IF, Block PC, Wilkins GT, et al. Percutaneous mitral balloon valvotomy during pregnancy in a patient with severe mitral stenosis. Cathet Cardiovasc Diagn. 1988;15:109–111.
23. Patel JJ, Hassen F, Patel N, et al. Percutaneous balloon mitral valvotomy in pregnant patients with tight pliable mitral stenosis. Am Heart J. 1993;125:1106–1109. doi:10.1016/0002-8703(93)90120-X
24. Rachor S, Kneissel GF, Fach A, et al. Balloon dilatation of the mitral valve in a pregnant patient: a case report. Z Kardiol. 1994;83:238–241.
25. Ribeiro PA. Percutaneous mitral valvotomy in pregnancy using the Inoue balloon technique.Rev. Port Cardiol. 1991;10:443–447.
26. Ribeiro PA, Fawzy ME, Awad M, et al. Balloon valvotomy for pregnant patients with severe pliable mitral stenosis using the Inoue technique with total abdominal and pelvic shielding. Am Heart J. 1992;124(6):1558–1562. doi:10.1016/0002-8703(92)90072-4
27. Ruzyllo W, Dabrowski M, Woroszylska M, et al. Percutaneous mitral commissurotomy with the Inoue balloon for severe mitral stenosis during pregnancy. J Heart Valve Dis. 1992;1(2):209–212.
28. Safian RD, Berman AD, Sachs B, et al. Percutaneous balloon mitral valvuloplasty in pregnant women with mitral stenosis. Cathet Cardiovasc Diagn. 1988;15:103–108.
29. Smith R, Brender D, McCredie M. Percutaneous transluminal balloon dilatation of the mitral valve in pregnancy. Br Heart J. 1989;61:551–553.
30. Zimarino M, Piovaccari G, Marzocchi A, et al. La stenosimitralicacritica en gravidanza: descrizione di un casotrattato con valvuloplasticapercutanea [The 24-hour hemodynamic changes after percutaneous mitral valvuloplasty]. Cardiologia. 1992;37:369–371.
31. Desai DK, Adanlawo M, Naidoo DP, et al. Mitral stenosis in pregnancy: a four‐year experience at King‐Edward VIII Hospital, Durban, South Africa. BJOG. 2000;107:953–958. doi:10.1111/j.1471-0528.2000.tb10395.x
32. Iung B, Cormier B, Elias J, et al. Usefulness of percutaneous balloon commissurotomy for mitral stenosis during pregnancy. Am J Cardiol. 1994;73:398–400. doi:10.1016/0002-9149(94)90017-5
33. Chatterjee K, Khanna R, Sahu A, et al. Immediate and long-term outcomes of balloon mitral valvotomy in pregnancy. Indian Heart J. 2020;72(4):248–251. doi:10.1016/j.ihj.2020.05.015
34. Abouzied AM, Al Abbady M, Al Gendy MF, et al. Percutaneous balloon mitral commissurotomy during pregnancy. Angiology. 2001;52(3):205–209. doi:10.1177/000331970105200308
35. Sharma JB, Yadav V, Mishra S, et al. Comparative study on maternal and fetal outcome in pregnant women with rheumatic heart disease and severe mitral stenosis undergoing percutaneous balloon mitral valvotomy before or during pregnancy. Indian Heart J. 2018;70(5):685–689. doi:10.1016/j.ihj.2018.01.018
36. Sananes S, Iung B, Vahanian A, et al. Fetal and obstetrical impact of percutaneous mitral commissurotomy during pregnancy. Fetal Diagn Ther. 1994;9(4):218–225. doi:10.1159/000263936
37. Wagner LK, Hayman LA. Pregnancy and women radiologists. Radiology. 1982;145:559–562. doi:10.1148/radiology.145.2.7134471
38. Fawzy ME, Abdulhalim JK, Stefadouros M, et al. Long term outcome of mitral balloon valvotomy in pregnant women. J Heart Valve Dis. 2001;10(2):153–157.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
