Back to Journals » Orthopedic Research and Reviews » Volume 15
The Outcome of Orthopedics Treatment of Lombok Earthquake Victim 2018: A Cohort of One-Year Follow-Up Study-Lesson Learned After Lombok Earthquake
Authors Anshori F , Kamal AF , Prabowo Y, Kekalih A , Febrianto R, Purnaning D, Dilogo IH
Received 21 October 2022
Accepted for publication 25 March 2023
Published 9 May 2023 Volume 2023:15 Pages 91—103
DOI https://doi.org/10.2147/ORR.S387625
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Clark Hung
Fahmi Anshori,1 Achmad Fauzi Kamal,1 Yogi Prabowo,1 Aria Kekalih,2 Rudi Febrianto,3 Dyah Purnaning,3 Ismail Hadisoebroto Dilogo1
1Departement of Orthopaedic and Traumatology, Faculty of Medicine, Universitas Indonesia-Cipto Mangunkusumo Hospital, Jakarta, Indonesia; 2Community Medicine Department, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 3Orthopaedic and Traumatology Division, Department of Surgery, Faculty of Medicine University of Mataram -Regional General Hospital of West Nusa Tenggara, Mataram, Indonesia
Correspondence: Fahmi Anshori, Department of Orthopaedic and Traumatology, Faculty of Medicine Universitas Indonesia, Dr. Cipto Mangunkusumo Hospital, Jl. Diponegoro no. 71, Jakarta, 10430, Indonesia, Tel +62 81281710266, Email [email protected]
Introduction: There was a magnitude 7 on the Richter scale earthquake on Lombok Island in 2018, causing more than 500 deaths. In the event of earthquakes, there is often an imbalance between overcrowding in hospitals and inadequate resources. The initial management of earthquake victims with musculoskeletal injuries is controversial, arguing over whether to utilize debridement, external or internal fixation, or conservative or operative treatment in an acute onset disaster situation. This study aims to determine the outcome of initial management after the 2018 Lombok earthquake, between immediate open-reduction and internal fixation (ORIF) and Non-ORIF procedures after one year follow-up.
Methods: This is a cohort study to evaluate radiological and clinical outcomes one year after orthopedic treatment in the Lombok earthquake 2018. The subjects were recruited from eight public health center and one hospital in Lombok in September 2019. We evaluate radiological outcomes (non/malunion and union) and clinical outcomes (infection and SF-36 score).
Results: Based on 73 subjects, the ORIF group has a higher union rate than the non-ORIF group (31.1% vs. 68.9%; p = 0.021). Incidence of infection only appeared in the ORIF group (23.5%). Clinical outcome as measured by SF36 showed the ORIF group had a lower mean of general health (p = 0.042) and health change (p = 0.039) clinical outcomes than the non-ORIF group.
Discussion: The most affected public group is the productive age with significant impact on social-economy. ORIF procedure is a major risk factor of infection in initial treatment after earthquake. Therefore, definitive operation with internal fixation is not recommended in the initial phase of a disaster. Damage Control Orthopedic (DCO) surgery protocol is the treatment of choice in acute disaster setting.
Conclusion: The ORIF group had better radiological outcomes than the non-ORIF group. However the ORIF group had higher cases of infection and lower SF-36 than the non-ORIF group. Definitive treatment in acute onset disaster setting should be prevented.
Keywords: ORIF/non-ORIF, infection, acute onset disaster, SF-36, union rate
Background
The earthquake has a devastating effect either on the environment and the inhabitants of the region affected.1 More than 500,000 earthquakes are documented annually in Indonesia resulting in around 3000 victims and deaths.2–6 Indonesia, one of the countries with the most active plate tectonic activity locations, is one of the five most frequent natural disasters in the last decade.7
On 5 August 2018, there was a magnitude 7 on the Richter scale earthquake on Lombok Island. This earthquake caused more than 500 deaths and more than 40,000 minor injuries. As the Lombok earthquakes showed a quadruplet pattern of earthquakes in which four large earthquakes hit subsequently and small-scale earthquakes in between, this causes uncertainty in the condition of the safety status of buildings and other health facilities. Therefore, the government collaborates with other non-government organizations or institutions to build emergency health facilities into container operating rooms and field hospitals.
Several studies have examined the profile of injuries after earthquakes around the world, and most of these studies conclude that musculoskeletal injuries are the most frequent earthquake-related injuries. Of all of the musculoskeletal injuries recorded, fractures are the most common ones which represent more than 50% of injuries caused by earthquakes.2,8–10
In the early periods after acute onset disaster, the most urgent orthopedic protocols needed are external fixation, amputation, and debridement. In multiple trauma patients, it is necessary to adhere to the principle of “damage control” which is preventing complications and performing recovery operations after the patient’s condition is stable, the study conducted by Mishra et al about the Nepal earthquake of 2015 found that the most commonly performed procedure was damage control orthopedic-like (DCO) external fixation application and debridement, they found external fixators are valuable tools of DCO in natural disasters.4,6,11–13
Sudden increase in the number of victims causing surge of patients coming to the hospitals in the affected region causing serious crises for healthcare centers.1,14 In acute disaster periods, when there was an explosion in the number of patient casualties to the health service, it is advisable to use the temporary stabilization method for the fracture. When this condition has improved and when the life threatening conditions have been eliminated, it is recommended to use the temporary method of functional stable osteosynthesis for the final fixation of the fracture.4,6
Often in the aftermath of an earthquake, surgery is avoided because of a lack of suitable equipment, an insufficient number of qualified surgeons, or a lack of proper training. Many surgeons choose the wrong implant or repair the fracture aggressively which results in complications of soft tissue infection and bone infection (osteomyelitis). On the other hand, it is known that the use of internal fixation for open fractures of the tibia and femur has a lower incidence of reoperation, with a lower risk of superficial infection, when compared to external fixation.4,6,14 This suggests that the initial management of earthquake victims with musculoskeletal injuries is controversial; it remains unclear whether external or internal fixation is preferable for these cases. Every major disaster warrants retrospective studies so we can learn how to improve all levels of Emergency Medical Services. Proper management of post-earthquake injuries is very important in terms of decreasing morbidity and mortality.6,14 Problems that may arise in the provision of healthcare services due to infrastructural damage and lack of personnel after an earthquake may lead to an increase in the loss of life and injuries caused by the earthquake.14–16
In Indonesia, there are still no guidelines regarding the management of musculoskeletal injuries after an earthquake. In order to provide input and outcomes, of course, an understanding of the clinical and radiological outcomes of orthopedic surgery in earthquake victims with injuries is needed, so that effective management strategies can be planned. Previously, there were no studies regarding clinical and radiological outcomes of musculoskeletal injuries after an earthquake. The aim of this study is to determine the profile of radiological and clinical outcomes of musculoskeletal injuries after the 2018 Lombok earthquake and to evaluate and compare outcomes between immediate ORIF and Non-ORIF procedures after one year follow up.
Methods
This is a cross sectional study which was conducted to evaluate clinical and radiological outcome after orthopedic treatment during acute onset disaster Lombok earthquake of 2018. The study was conducted in September 2019. Subjects from eight primary healthcare facilities in North Lombok district and two primary healthcare centers in West Lombok district were included in this study. The subjects were later referred to North Lombok general hospital and a radiological evaluation was performed.
The inclusion criteria consisted of the existence of orthopedic fractures injury and treatment related to Lombok Earthquake of 2018, which was a minimum of 6 months after treatment. Subjects who did not have any severe comorbidities and declined to participate were excluded from this study. Radiological outcome with a plain radiograph were performed and the results were categorized into non-union, malunion and union. Thereafter, clinical outcomes of the subjects were determined using SF-36 functional score and the sign of infection based on clinical and microbiological culture.17 The demographic variables were age, sex, diagnosis, fracture location and Independent variable were immediate open reduction and internal fixation (ORIF) or Non ORIF. In the data collection we analyze bivariate data using a Chi-square test, Fisher test, independent t-test, Mann–Whitney test and Multivariate data using one-way ANOVA and post-hoc analysis.
Results
Demographic distribution, diagnosis and location of the injury, ORIF, union rate, and infection were presented in Table 1 below.
 |
Table 1 Demographic Distribution Risk Factor and Outcome Infection and Union Rate |
It can be inferred that the majority subjects in this study are female and adult. The most common diagnosis was closed fractures of the lower extremities and the majority of unions and cases of infection reached 16.2%. In the diagnosis category, the most common diagnosis was closed fracture lower limb (52.7%) and the second was open fracture lower limb (25.7%), and this is also in accordance with the category of site injury. The comparison of risk factors with union rate and infection was presented in Table 2 below.
The total ORIF operations was 68.9% with a malunion rate of 17.6% and the Non-Union rate was 36.5% of all cases. In the comparison table of risk factors with union rate outcomes, it was found that the diagnosis risk factor had a significant relationship with the union rate (p = 0.038) and the risk factor for ORIF had a significant relationship with the union rate (p = 0.021). In the comparison table of risk factors with infection outcomes, the analysis showed that the risk factors of diagnosis had a significant relationship with infection (p = 0.001) and the risk factors of ORIF had a significant relationship with infection (p = 0.011). The results of the analysis of risk factors on the union rate found that the type of injury diagnosis had a significant relationship with the union rate (p = 0.038) where open fracture upper limb had the highest non-/malunion rate (80%) followed by open fracture lower limb (78.9%). Risk factors ORIF/non-ORIF procedure had a significant difference to the union rate (p = 0.021) with ORIF group had non-/malunions rate lower (45.1%) than non-ORIF group (73.9%), this can be seen that although the mal-/nonunion rate is higher in the non-ORIF procedure, however, the incidence of mal-/non-union is large enough to nearly half of the total population receiving ORIF procedure.
Results Table 2 Analysis of risk factors for clinical outcome of infection. It was found that the diagnosis of injury had a significant difference in the incidence of infection (p = 0.0001).
 |
Figure 1 SF-36 physical function comparison based on diagnosis and location of the injury. *Indicates©significant with p-value <0.05 between groups compared. |
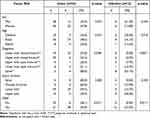 |
Table 2 Comparison of Risk Factors with Union Rate and Infection |
The analysis results of risk factor data with SF-36 physical function (physical function) showed that the risk factors for diagnosis and location of the injury had significant differences with the SF 36 physical function (physical function quality of life) values, respectively P = 0.001 and P = 0.002.
In this Figure 1 tabulation graph, it is shown that the physical function in the spinal cord injury group are the lowest SF-36 score in diagnosis group and also the same for the location of thefracture injury group, the lowest physical function was in the spine location group.
From Figure 2 risk factor data analysis with SF-36 social functioning, it was found that the risk factors for diagnosis and injury location had a significant difference to the SF 36 social functioning (social function aspects of quality of life) value, respectively P = 0.042 and P = 0.012 and in and in Figure 3 had the lowest score of SF-36 because of persistent pain problem.
In Table 3, the analysis results showed a psychometric description that ORIF action has a significant relationship in SF-36 general health (p = 0.042) and SF-36 health change (p = 0.039) and the median in the two groups non-ORIF is higher than ORIF. The general health score has a higher mean value in the non-ORIF group (52) than the ORIF group (40), for the health change group the mean non-ORIF group (68) is also higher than the ORIF group (50).
 |
Table 3 Comparison of SF 36 Between Subjects with ORIF and Without ORIF |
there are several failed cases we documented, Figure 4 sample of implant failure of the tibia fracture, and in Figure 5 is a sample case of infected union lower extremity fracture, regardless all of these cases are direct ORIF in acute onset of disaster.
Discussion
Demographics Data
In this study, 62.2% of patients are female and 75.5% are adult age. This study has a similar result from the epidemiological study of the earthquake in Palu-Indonesia in September 2018, conducted by Prabowo et al. Their study showed that the largest distribution age is same that are adult age. But the sex distribution is more common male (52.6%) than female (47.4%), we compare with study by Prabowo et al because of the similar region, landmarks and people within Indonesia.18 This result is same as the study conducted by Pang et al in western Sumatra about the 2009 earthquake; they found majority of fracture locations are lower extremity and gender sex majority was female.18,19 A study and literature review conducted by Mortazavi et al in Musculoskeletal Related Injuries After the 2017 Kermanshah Earthquake, Iran, found the most common location of fracture is lower extremity (37%), most of them are productive, aged between 18–65 years old and the gender sex majority was female (53%) and another study of the Nepal earthquake (2015), by Vaishya et al had similar result with the most common cases is lower extremity fracture but the sex distribution is more commonly male (57.5%).20,21 The majority of patients in this study were female, possibly because women find it more difficult to save themselves when an earthquake occurs, but in the largest age distribution for adults this is a concern because the most affected group is the productive age group, so this has an impact on the economy. In our study the children's age group is 13.5%, its is another consideration because of the potential disability impact in the future. Gamulin et al stated that pediatric group patients in earthquake disasters had long term long-term physical and psychosocial disabilities if not treated adequately.22 It is estimated that the total economic loss is IDR 7.7 trillion (528 million dollars) and that 431,416 people have lost their homes.23,24
The most common location of the injury is the lower limb, this is the same result as the study conducted by Prabowo et al.18 In an epidemiological study conducted by Prabowo et al about the 2018 Palu earthquake, they found that the highest incidence of orthopedic cases was lower limb fracture (64.5%) and the most common procedures performed were debridement (43.3%) and then ORIF (33.3%), but debridement and external fixation was only 3.3%. In another study conducted by Guner et al in Turkey’s Van earthquake (2011), they reported the most common location of fracture is the lower extremity and the most commonly performed procedure was debridement.25 A systematic review study conducted by McKenzie et al on epidemiological studies and management of orthopedic injuries after earthquake disasters in developing countries found that 59% of the injuries that occurred were lower limb fractures and the most common procedure performed was debridement (33%). This is probably due to injuries while rescuing themselves and the more exposed area while earthquake incident occur is the lower extremity area.
Relationship Between Risk Factors and Clinical & Radiological Outcomes
In this study, we found the total infection rate was 12 cases (16.2%), and from non-ORIF group 100% showed no sign of infection. The results showed that most infections were found in post-ORIF treatment patients at RSUDP NTB (Regional General Hospital of West Nusa Tenggara) as many as 5 cases (33%) and the second was found in post-ORIF action patients at KRI Hospital Dr. Soeharso (Indonesia warship floating hospital) has as many as 4 cases (25%), one case infection from Mataram University hospital, one infection found patient at Narmada General Hospital and another one from Mataram Bhayangkara Hospital. The study reported by Tan et al about Singapore Armed Forces (SAF) medical and surgical teams in the 2009 Sumatra earthquake found 56% of the 102 surgical procedures were performed on dirty or infected wounds.26 The high incidence of infection occurred in both hospitals (RSUDP NTB Hospital and KRI dr. Soeharso Hospital) may be due to the lack of sterilization equipment, limited resources for wound treatment and aggressive methods of treatment to perform definitive treatment in the acute phase disaster period in Lombok. Besides poor conditions, implementation of orthopedic surgery at a field hospital is usually limited due to a lack of coordination, equipment, and drugs. Infection control remains key to the success of orthopedic management in earthquake acute onset disaster.3,18,27
The highest infection cases occurred in cases of open fracture lower limb (42.1%). This is consistent with the literature because open fracture injuries of the lower extremities are prone to infection leading to chronic osteomyelitis.28 In the risk factors group ORIF/non-ORIF, there was a significant difference in the incidence of infection (p = 0.011). The population group that received ORIF procedure, cases of infection was 23.5% and in the population group that did not receive ORIF procedure, cases of infection were 0%. A retrospective study by Alvarado et al between 2007–2014 from three Médecins sans Frontières (MSF) emergency surgical interventions; in Haiti (following the 2010 earthquake) and three MSF projects in Kunduz (Afghanistan), Masisi (Democratic Republic of the Congo) and Tabarre (Haiti) postoperative infection rates from 2.4% to 3.5%, because the most commonly performed procedures were external fixation and closed reduction.29 This suggests that the ORIF procedure is a major risk factor for causing infection. This is in accordance with the guidelines issued by the Arbeitsgemeinschaft für Osteosynthesefragen (AO; Association of the Study of Internal Fixation) and WHO that in a disaster emergency condition, if an area cannot be ascertained, the availability of a referral hospital for optimal orthopedic surgery, adequate surgical and nursing teams, complete sterile equipment and adequate postoperative care is recommended for only external fixation debridement for open fractures, casting with plaster of Paris and skin/skeletal traction for closed fractures.4,30
Guidelines issued by the AO, International Committee of the Red Cross (ICRC) and WHO state that all cases of closed fracture should be treated with closed reduction to minimize complications, especially infection, even though this management results in prolonged management of the patient. Articular and periarticular fractures where ORIF action is required are proven to be more profitable to be postponed in disaster conditions and should only be done in good health facilities and adequate sterility. The use of internal fixation in limited health facilities causes high infection rates. Therefore, ORIF procedures should only be carried out in good health facilities, with good and safe clean water facilities, sterile equipment, orthopedic surgery teams, sound nursing teams and physiotherapist and postoperative care teams. For open fracture cases, the guidelines expressly prohibit primary initial management with internal fixation at any level of healthcare facility, because the principle of open fracture management in a disaster condition is to stabilize the fracture so that it has a safe environment for wound care, wound healing and primary closure from the wound in the easiest and safest way.4,30
The experience of MSF in the 2010 Haiti earthquake stated that external fixation in a sudden onset disaster can be the definitive therapy and is best adapted in the context of a major disaster in 1–2 weeks of the initial phase of the disaster.31 A prospective study by Delauche et al of the outcome of patients with limb trauma following the Haitian earthquake in 2010 found that only half the patients with severe limb injuries, whether managed with amputation or limb salvages, regain satisfactory functional status at 2 years post disaster, and more than 25% patient needed further surgical management. Another report from Talbot et al regarding the Canadian force team in Haiti 2010 earthquake, found that two weeks after the earthquake, operations were was unrelated to the earthquake.32,33 In the initial phase of a disaster, a definitive operation with internal fixation is not recommended because in that phase there can be a collapse of both the structural facilities and functional human resources, facilities and infrastructure for health services as well as the management of human resources for medical personnel who deal with the injured victims of the earthquake which jumped at one time causing fatigue and can reduce post-traumatic patient care. In the case of natural disasters due to earthquakes, we cannot predict how long aftershocks will last and experts estimate that two weeks after the initial earthquake is a critical time for stabilization of the patient’s condition, both with conservative plaster of Paris, external fixation and skeletal traction. In the third week, definitive surgery can be done with the condition that qualified health facilities, a team of doctors, a team of nurses and the availability of complete sterile equipment to adequate postoperative care and rehabilitation. If these facilities cannot be reached in the area either with a field hospital or a floating/emergency hospital, it is advisable to evacuate outside the area where the referral hospital for orthopedic and trauma service centers are available.4,28,30,31,34
On the other hand, we know that almost all of referral hospitals in Lombok regions have suffered serious damage and the main referral hospital, namely the West Nusa Tenggara regional general hospital, serves orthopedic trauma cases with excess capacity and treatment in the hallway and hospital parking lot when the service lasts the third day. After the initial earthquake, suddenly a large aftershock occurred which caused the hospital management to stop surgical services in the operating room at that time. A prospective study by Giri et al about the Nepal earthquake disaster, they stated in efficient prehospital management and good strategic evacuation are significantly decrease morbidity and mortality of the patient.35 The systematic review research conducted by McKenzie et al states that it is unrealistic to treat definitive internal fixation in conditions immediately after an earthquake/acute onset disaster. The focus of action on the surgical team that is initially present at the disaster site is to carry out disaster triage, control bleeding, debridement of wounds, stabilization of soft tissue so that the DCO surgery protocol in disaster conditions is the treatment of choice and the key to management of orthopedic case treatment in acute onset disaster setting.3,34,36 This has been proven in the experience of the IDF medical team in handling the earthquake in Pakistan in 2005 and by Lebel et al in Haiti in 2010 installing external fixation follow-up 2 weeks after the action showed no sign of infection and the team from the Israel defense force waited 2 weeks after the initial disaster and waited until the preparations were made. A sufficient number of medical teams, nurses, equipment, sterilization and new wound care can then perform definitive action with internal fixation, the initial team that comes only performs external fixation, plaster of Paris (casting) and amputation.3,17,33,37
The patient group with ORIF had lower SF-36 in general health and health change values than the non-ORIF group, and in the previous discussion, it had been proven that action ORIF increases the risk of postoperative infection. For cases of spinal cord injury, both in the injury location category and the diagnosis was found to have a low value on the SF-36 physical function, role limitations due to emotional problems and social functioning, and all spinal cases in this study were post-posterior stabilization surgery and decompression in the first two weeks following the earthquake. Research conducted by Sudaryo et al was a prospective cohort study on the quality of life of patients who experienced the 2009 Padang earthquake. It showed a significant reduction in quality of life with QLA scores in the earthquake-injured group and the most common injured group were limb fractures and dislocations.38 The probable cause of the lower score of SF-36 in ORIF group than the non-ORIF group is due to the general effect of the earthquake injury in this study. Orthopedic injury affects mostly productive age and from Indonesia Central Bureau of Statistics 2018–2019 data stated that in north Lombok region majority the employee of people is peasant, farmer and merchant, and this brings about loss of job due to orthopedic injury. This result is similar to the result from the by study Stroebe et al about chronic disaster impact in the Netherlands which stated that earthquakes can have negative health consequences for inhabitants over time, especially people that experience repeated damage or earthquake.39 Another study conducted by Gallardo et al about systematic review and meta-analysis data of medium- and long-term health effects of earthquakes in high-income countries found an increased mortality rate for all causes, myocardial infarction and stroke from the first month to up to 3 years after an earthquake.40 Our theory that the effect of the Lombok earthquake of the quadruplet type (four big attacks of earthquake) still persist for at least 3–4 years afterward.39–41
Referring to the results of the analysis above, the researcher suggests definitive measures for spinal cord injuries that require immediate surgery in the acute phase of a disaster, so it is better to evacuate victims to a referral center for qualified orthopedic services, having standard spine surgery and ICU wards, both in terms of facilities and human resources for orthopedic medical rehabilitation specialists and a team of orthopedic nurses. In an analysis of the 2005 earthquake in Pakistan, as many as 194 spinal cord injury patients were treated at one time at the Rawalpindi medical college and its allied hospital, the majority of injuries to the lumbar area were 61.85% and as many as 41% of patients had paraplegia, many victims did not receive treatment and rehabilitation accordingly so that there were several cases of paraplegic patients with large decubitus ulcers in the sacral area (20%), so they underline from the experience of the 2005 Pakistan earthquake that the management of the spine should be comprehensive. So that the establishment of a spinal injury management center at a referral hospital in the earthquake disaster area or evacuation to the nearest hospital outside the earthquake-hit area whose services and human resources are not affected by the earthquake disaster and ICU services and post-operative handling and proper rehabilitation is an inevitability for acute earthquake disaster conditions.24 Another report by Awais et al about the 2005 Pakistan earthquake, stated external fixator are valuable damage control orthopedic tools in major natural disasters, and had saved many limb injuries during the 2005 Pakistan earthquake.24,42
Research Implications and Follow-Up Research Plans
In conclusion, the risk factors that influence the union rate status, infection and SF-36 functional score are age, diagnosis, location of injury and ORIF action. Direct ORIF action in the initial phase of a disaster is a risk factor that can be intervened to reduce the morbidity that will occur due to infection, infection causing new problems and causing the need for repeated operations in patients, then by the AO-ICRC-WHO in its management guide, in the initial acute disaster phase is conservative management of closed fractures (POP, scalp traction, etc.) and external fixation for open fractures.4,30
This research implies that the government, in this case, the Ministry of Health of the Republic of Indonesia, National Disaster Management Authority Indonesia and association organizations, in this case, the Indonesian Orthopedic Association, should make guidelines for the management of actions for orthopedic cases in disaster conditions, given the high number of natural disasters that occur annually in Indonesia which are namely earthquakes, landslides and floods, and manmade disasters such as victims of bombs, terrorist attacks, collapsed buildings. This management guide follows adaptations or references from the management guidelines previously prepared by AO-ICRC-WHO and other textbooks specializing in disasters, and adapting to local wisdom, culture, culture and characteristics of the Indonesian society, therefore the researcher recommends the need for research on post-earthquake clinical outcomes in other locations such as the Aceh tsunami earthquake, the Yogyakarta earthquake, the Palu earthquake and the Banten tsunami earthquake. Researchers saw that there was no comprehensive research on follow-up clinical and radiological outcomes after orthopedic action in acute disaster conditions and the importance of developing management guidelines together with other surgical colleges regarding initial and advanced management in conditions of mass disasters.
Limitation
A major limitation of this study is the limited amount of samples that we collected because of the scattered victims of the earthquake on the outer edges of the region. We only conducted a cross-sectional study then it was difficult to investigate risk factors and outcomes and had some bias. There is a limitation of literature that follows clinical and radiological outcomes after a disaster we could not make a similar comparison with this study.
Conclusion
The largest distribution of age was adult age and the most distribution of injuries was closed fractures of the lower extremities and the second was open fractures of the lower limbs. The population group that received the ORIF procedure had better radiological outcomes than the non-ORIF group, however, the ORIF group had higher infection rate and lower clinical outcome of SF-36 general health and health changes than the Non-ORIF group. It is recommended to perform debridement and external fixation for open fracture type and conservative treatment for closed fracture in an acute onset disaster setting or evacuate in case that needs urgent immediate treatment. Definitive treatment in acute onset disaster settings should be prevented due to the risk of infection.
Abbreviations
ORIF, Open Reduction Internal Fixation; AO, Arbeitsgemeinschaft für Osteosynthesefragen; ICRC, International Committee of the Red Cross; WHO, World Health Organization.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethical Approval
Ethical approval clearance from ethics committee board Faculty of Medicine, Universitas Indonesia with protocol number 19-04-0441. All of data patient details and images being published are anonymously and blinded, and compliance with the declaration of Helsinki.
Informed Consent to Participate
Written informed consent was obtained from the patient for publication of this research article and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Kang P, Tang B, Liu Y, et al. Profile and procedures for fractures among 1323 fracture patients from the 2010 Yushu earthquake, China. Am J Emerg Med. 2016. doi:10.1016/j.ajem.2016.07.064
2. Kang P, Zhang L, Liang W, et al. Medical evacuation management and clinical characteristics of 3255 inpatients after the 2010 Yushu earthquake in China. J Trauma Acute Care Surg. 2012;72(6):1626–1633. doi:10.1097/TA.0b013e3182479e07
3. MacKenzie JS, Banskota B, Sirisreetreerux N, Shafiq B, Hasenboehler EA. A review of the epidemiology and treatment of orthopaedic injuries after earthquakes in developing countries. World J Emerg Surg. 2017;12(1). doi:10.1186/s13017-017-0115-8
4. Lerner A, Roshal L. Orthopedics in Disasters: Orthopedic Injuries in Natural Disasters and Mass Casualty Events. Springer; 2016. doi:10.1007/978-3-662-48950-5
5. Morelli I, Sabbadini MG, Bortolin M. Orthopedic injuries and their treatment in children during earthquakes: a systematic review. Prehosp Disaster Med. 2015;30(5):478–485. doi:10.1017/S1049023X15004951
6. Bortolin M, Morelli I, Voskanyan A, Joyce NR, Ciottone GR, Bortolin M. Earthquake-related orthopedic injuries in adult population: a systematic review. Prehosp Disaster Med. 2017;32(2):201–208. doi:10.1017/S1049023X16001515
7. Guha-sapir D, Hoyois P, Below R. Annual disaster statistical review 2016. CRED. 2011. doi:10.1093/rof/rfs003
8. Phalkey R, Reinhardt JD, Marx M. Injury epidemiology after the 2001 Gujarat earthquake in India: a retrospective analysis of injuries treated at a rural hospital in the Kutch district immediately after the disaster. Glob Health Action. 2011;4(1):7196. doi:10.3402/gha.v4i0.7196
9. Xie J, Du L, Xia T, Wang M, Diao X, Li Y. Analysis of 1856 inpatients and 33 deaths in the West China Hospital of Sichuan University from the Wenchuan earthquake. J Evid Based Med. 2008;1(1):20–26. doi:10.1111/j.1756-5391.2008.00010.x
10. Bulut M, Fedakar R, Akkose S, Akgoz S, Ozguc H, Tokyay R. Medical experience of a university hospital in Turkey after the 1999 Marmara earthquake. Emerg Med J. 2005;22(7):494–498. doi:10.1136/emj.2004.016295
11. Genthon A, Wilcox SR. Crush syndrome: a case report and review of the literature. J Emerg Med. 2014;46(2):313–319. doi:10.1016/j.jemermed.2013.08.052
12. Smith J, Greaves I. Crush injury and crush syndrome: a review. J Trauma Acute Care Surg. 2003;54(5):226–230. doi:10.1097/01.TA.0000047203.00084.94
13. Mishra A, Adhikari V, Chalise P, Singh R. Role for damage control orthopaedics in natural disaster like earthquake. Nepal Med Coll. 2017;19(2):75–78.
14. Ramirez M, Peek-Asa C. Epidemiology of traumatic injuries from earthquakes. Epidemiol Rev. 2005;27(1):47–55. doi:10.1093/epirev/mxi005
15. Indah LK, Triatmodjo B, Triatmadja R, et al. Evaluasi sistem mitigasi penanganan bencana gempabumi di kecamatan bantul propinsi daerah istimewa yogyakarta. Forum Tek Sipil. 2008;18:959–971.
16. Ergen E, Kaya O, Yılmaz Ö, et al. Which is more dangerous, earthquake, or the panic?Evaluation of the 24 January 2020 Elazig/Türkiye earthquake related musculoskeletal injuries. Ulus Travma Acil Cerrahi Derg. 2022. 28(9):1335–1339. English. PMID: 36043928. doi:10.14744/tjtes.2021.57606
17. Ware J, Snow K, Kosinski M, Gandek B. SF-36 health survey manual and interpretation guide. Bost New Engl Med Cent. 1993. doi:10.1523/JNEUROSCI.2235-04.2004
18. Prabowo Y, Saputra D. Epidemiology of orthopaedic injuries at the local hospital following earthquake in Palu, Indonesia, 2018. J Orthop Trauma Surg Relat Res. 2019;14(3):41–44.
19. Pang H-N, Lim W, Chua W-C, Seet B. Management of musculoskeletal injuries after the 2009 western Sumatra earthquake. J Orthop Surg. 2011;19(1):3–7. doi:10.1177/230949901101900102
20. Mortazavi SMJ, Ebrahiminasab M, Farhoud AR, Mirzashahi B, Ghadimi E. Musculoskeletal related injuries after 2017 Kermanshah earthquak. J Orthop Spine Trauma. 2017;3(2):4–9. doi:10.5812/jost.67518.Research
21. Vaishya R, Agarwal AK, Vijay V, Hussaini M, Singh H. Surgical management of musculoskeletal injuries after 2015 Nepal earthquake: our experience. Cureus. 2015. doi:10.7759/cureus.306
22. Gamulin A, Armenter-Duran J, Assal M, Hagon O, Dayer R. Conditions found among pediatric survivors during the early response to natural disaster: a prospective case study. J Pediatr Orthop. 2012;32(4):327–333. doi:10.1097/BPO.0b013e31825197ec
23. Muttalib A, Mashur M. Analisis dampak sosial ekonomi masyarakat pasca bencana gempa bumi di Kabupaten Lombok Utara (Klu) [Analysis of the socio-economic impact of the community after the earthquake disaster in North Lombok Regency]. J Ilm Mandala Educ. 2019;5(2):84. doi:10.58258/jime.v5i2.785
24. Tauqir SF, Mirza S, Gul S, Ghaffar H, Zafar A. Complications in patients with spinal cord injuries sustained in an earthquake in Northern Pakistan. J Spinal Cord Med. 2007;30(4):373–377. doi:10.1080/10790268.2007.11753955
25. Guner S, Guner SI, Isik Y, et al. Review of Van earthquakes form an orthopaedic perspective: a multicentre retrospective study. Int Orthop. 2013;37(1):119–124. doi:10.1007/s00264-012-1736-x
26. Tan CM, Lee VJ, Chang GH, Ang HX, Seet B. Medical response to the 2009 Sumatra earthquake: health needs in the post-disaster period. Singapore Med J. 2012;53(2):99–103.
27. Zheng W, Hu Y, Xin H. Successful implementation of thirty five major orthopaedic procedures under poor conditions after the two thousand and fifteen Nepal earthquake. Int Orthop. 2016;40(12):2469–2477. doi:10.1007/s00264-016-3284-2
28. Emami MJ, Tavakoli AR, Alemzadeh H, et al. Strategies in evaluation and management of bam earthquake victims. Prehosp Disaster Med. 2017;20:327–330. doi:10.1017/S1049023X0000279X
29. Alvarado O, Trelles M, Tayler-Smith K, et al. Orthopaedic surgery in natural disaster and conflict settings: how can quality care be ensured? Int Orthop. 2015;39(10):1901–1908. doi:10.1007/s00264-015-2781-z
30. Veen H, Norton I. Management of limb injuries during disasters and conflicts [internet]. WHO-ICRC-AO Guideline; 2016:184. Available from: https://www.researchgate.net/publication/315471392_Management_of_Limb_Injuries_During_disasters_and_conflicts.
31. Boillot F, Herard P. External fixators and sudden-onset disasters: médecins Sans Frontières experience. Int Orthop. 2014;38(8):1551–1554. doi:10.1007/s00264-014-2344-8
32. Delauche MC, Blackwell N, Le Perff H, et al. A prospective study of the outcome of patients with limb trauma following the Haitian Earthquake in 2010 at one- and two- year (The SuTra2 study). PLoS Curr. 2013. doi:10.1371/currents.dis.931c4ba8e64a95907f16173603abb52f
33. Talbot M, Meunier B, Trottier V, et al. 1 Canadian field hospital in Haiti: surgical experience in earthquake relief. Can J Surg. 2012;55(4):271–274. doi:10.1503/cjs.039010
34. Dhar SA, Bhat MI, Mustafa A, et al. “Damage control orthopaedics” in patients with delayed referral to a tertiary care center: experience from a place where Composite Trauma Centers do not exist. J Trauma Manag Outcomes. 2008;2(1):1–6. doi:10.1186/1752-2897-2-2
35. Giri S, Risnes K, Uleberg O, et al. Impact of 2015 earthquakes on a local hospital in Nepal: a prospective hospital-based study. PLoS One. 2018;13(2):1–16. doi:10.1371/journal.pone.0192076
36. Wolfson N. Orthopaedic triage during natural disasters and mass casualties: do scoring systems matter? Int Orthop. 2013;37(8):1439–1441. doi:10.1007/s00264-013-1997-z
37. Lebel E, Blumberg N, Gill A, Merin O, Gelfond R, Bar-On E. External fixator frames as interim damage control for limb injuries: experience in the 2010 Haiti earthquake. J Trauma. 2011;71(6):E128–E131. doi:10.1097/TA.0b013e3182147654
38. Sudaryo MK, Besral EAT, Rivany R, et al. Injury, disability and quality of life after the 2009 earthquake in Padang, Indonesia: a prospective cohort study of adult survivors. Glob Health Action. 2012;5(1):1–11. doi:10.3402/gha.v5i0.11816
39. Stroebe K, Kanis B, Richardson J, et al. Chronic disaster impact: the long-term psychological and physical health consequences of housing damage due to induced earthquakes. BMJ Open. 2021;11(5):e040710. doi:10.1136/bmjopen-2020-040710
40. Gallardo AR, Pacelli B, Alesina M, et al. Medium- and long-term health effects of earthquakes in high-income countries: a systematic review and meta-analysis. Int J Epidemiol. 2018;47(4):1317–1332. doi:10.1093/ije/dyy130
41. Statistik badan pusat. Kabupaten lombok utara dalam data. In BPS kabupaten Lombok Utara; 2017:1–353.
42. Awais S, Saeed A, Ch A. Use of external fixators for damage-control orthopaedics in natural disasters like the 2005 Pakistan earthquake. Int Orthop. 2014;38(8):1563–1568. doi:10.1007/s00264-014-2436-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




