Back to Journals » Psychology Research and Behavior Management » Volume 15
The Mediating Effects of Resilience on Perceived Social Support and Fear of Cancer Recurrence in Glioma Patients
Authors Zhong M, She F, Wang W, Ding L, Wang A
Received 17 May 2022
Accepted for publication 27 July 2022
Published 6 August 2022 Volume 2022:15 Pages 2027—2033
DOI https://doi.org/10.2147/PRBM.S374408
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Mengshi Zhong,1 Fei She,2 Weijie Wang,1 Lianshu Ding,1 Aifeng Wang1
1Department of Neurosurgery, Huai’an First Hospital Affiliated to Nanjing Medical University, Huai’an, 223300, People’s Republic of China; 2Department of Nursing Administration, Huai’an First Hospital Affiliated to Nanjing Medical University, Huai’an, 223300, People’s Republic of China
Correspondence: Lianshu Ding; Aifeng Wang, Department of Neurosurgery, Huai’an First Hospital Affiliated to Nanjing Medical University, Huai’an, 223300, People’s Republic of China, Email [email protected]; [email protected]
Objective: To investigate the mediating effect of resilience on perceived social support and fear of cancer recurrence (FCR) in glioma patients.
Methods: A total of 128 glioma patients were enrolled for the survey by Connor-Davidson resilience scale (CD-RISC), perceived social support scale (PSSS) and Chinese version of fear of progression questionnaire-short form (FoP-Q-SF). Structural equation model was used to analyze the effects of resilience.
Results: The score of FCR in glioma patients was 29.52± 8.30. A total of 47 patients had FCR (total score ≥ 34), with an incidence of 36.7%. There was a correlation between FCR, resilience and social support (P< 0.01). The resilience between perceived social support and FCR in glioma patients had good fitting with the structural equation model. Resilience played a mediating role between perceived social support and FCR, with a mediating effect of 48.4%.
Conclusion: The level of resilience can be improved by improving the perceived social support in patients with glioma to reduce the FCR of patients.
Keywords: glioma, fear of cancer recurrence, resilience, perceived social support, mediating effect
Introduction
Glioma is a high incidence intracranial tumor, accounting for 50%–60% of central nervous system tumors. Surgery is still the main treatment method for glioma, but the 5-year survival rate of glioma patients is very poor.1,2 Due to the high recurrence rate and progression rate of glioma, glioma not only brings physical discomfort to patients, but also causes a series of psychological problems that seriously affect the prognosis and quality of life of patients. Fear of cancer recurrence (FCR) is one of the most common psychological reactions.3 FCR refers to cancer patients’ fear of cancer recurrence, progression or metastasis, which is manifested in over examination, over vigilance and over attention to the body, and some symptoms such as pain and chest tightness are regarded as signs of aggravation of the disease. It has been shown that 39–97% of patients have different degrees of FCR.4
Perceived social support is an emotional response that individuals experience to be respected, understood and supported in the stress process, which can help individual reduce stress and respond to stress effectively. Resilience belongs to the category of positive psychology and is a process of positive response and good adaptation of individuals in traumatic events, which may reduce the impact of FCR.5 Studies have shown that individuals who perceive high social support tend to have a higher level of resilience, which can reduce the impact of traumatic events on themselves.6 At present, the relationship of resilience, perceived social support and FCR is unclear. The purpose of this study is to explore the effect of perceived social support on resilience and FCR and reduce FCR and improve the quality of life of glioma patients.
Subjects and Methods
Subjects
A total of 128 glioma patients hospitalized in the Department of Neurosurgery of Huai’an First Hospital Affiliated to Nanjing Medical University (Huai’an, China) from July 2018 to December 2019 were selected by a convenient sampling method. Inclusion criteria: pathologically diagnosed as glioma; aged 18–70 years old; conscious and able to communicate. Exclusion criteria: critically ill patients; patients who have a history of mental disorders and are unable to communicate; patients complicated with serious diseases such as heart, lung and kidney or tumors. All patients provided informed consent. This study was approved by the Ethics Committee of Huai’an First Hospital Affiliated to Nanjing Medical University and complied with the Declaration of Helsinki. All patients finished the questionnaire to obtain information on total 15 independent variables, including age, gender, residency, education, marriage, occupation, family income, insurance, disease grade, disease duration, surgery, recurrence or metastasis, FCR, resilience, and perceived social support.
Fear of Progression Questionnaire-Short Form (FoP-Q-SF)
The Chinese version of the FoP-Q-SF scale was used in this study. The scale was composed of 12 items in the two dimensions of health and social family, and a grade 5 scoring method (1–5 points) was used, with a total score of 12–60. The higher the score, the higher the patient’s fear of disease progression, and the total score ≥34 indicated dysfunctional fear of recurrence. The Cronbach’s α coefficient of the scale in this study was 0.883.
Connor-Davidson Resilience Scale (CD-RISC)
The Chinese version of CD-RISC contained 25 items in three dimensions of tenacity, strength and optimism, and a grade 5 scoring method (0–4 points) was used, with a total score of 0–100.7 The higher the score, the higher the level of resilience. The internal consistency coefficient of the scale was 0.91, and the Cronbach’s α coefficient of each dimension was 0.60–0.88. The Cronbach’s α coefficient of the scale in this study was 0.954.
Perceived Social Support Scale (PSSS)
The PSSS was used to measure the degree of social support perceived by individuals, including a total of 12 items in 3 dimensions of family support, friend support and other support. A grade 7 scoring method (1–7 points) was used, with a total score of 12–84, the higher the score, the more the perceived social support. The Cronbach’s α coefficient of the scale was 0.88, and the test–retest reliability was 0.85. The Cronbach’s α coefficient of the scale in this study was 0.840.
Statistical Methods
SPSS 22.0 and AMOE 17.0 statistical software were used for data analysis. Counting data were expressed as frequency. The measurement data in line with the normal distribution were expressed as the mean ± standard deviation. Correlation analysis of the influencing factors and FCR was performed and the structural equation modeling (SEM) was constructed. In general, the closer χ2/df is to 1, the better the model fitting is. Goodness of fit index (GFI), adjusted goodness of fit index (AGFI), normed fit index (NFI), incremental fit index (IFI), comparative fit index (CFI) values were greater than 0.90, and root mean square error of approximation (RM-SEA) was smaller than 0.08, indicating that the fitting was reasonable. Pearson correlation was used to analyze the relationship between perception of social support, resilience and FCR in patients with glioma. P<0.05 was considered statistically significant.
Results
General Information of Patients with Glioma
As shown in Table 1, among the 128 subjects 76 cases were male and 52 cases were female. They were 27–69 years old (mean 42.54±5.54). For residence, 58 cases lived in rural area, and 70 cases lived in urban area. For education, 65 cases graduated from middle school and below, 45 cases graduated from high school, and 18 cases graduated from college and above. For marriage, 98 cases were married, and 30 cases were unmarried or others. The duration of disease of 48 cases was <6 months, that of 43 cases was 6–12 months, that of 23 cases was 13–24 months, and that of 14 cases was >24 months; and 36 cases had recurrence or metastasis.
 |
Table 1 General Information of Patients with Glioma |
FCR Scores in Glioma Patients
As shown in Table 2, the total score of FCR in glioma patients was 29.52±8.30, and the mean score of each item was 2.46±0.69. We found that 47 patients (36.72%) had total score of ≥34.
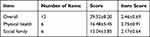 |
Table 2 The Scores of FCR in Glioma Patients |
The scores of perceived social support in glioma patients were shown in Table 3. Total score of perceived social support in glioma patients was 61.47±11.20, which was at the upper level, and the mean score of family support was the highest and the mean score of friend support was the lowest. The resilience scores in glioma patients are shown in Table 4. The total score of resilience in glioma patients was 52.94±10.05, which was at the medium level, and the mean score of tenacity dimension was the highest and the mean score of optimism dimension was the lowest.
 |
Table 3 The Scores of Perceived Social Support in Glioma Patients |
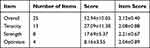 |
Table 4 The Scores of Resilience in Glioma Patients |
Correlation Analysis of Perceived Social Support, Resilience and FCR in Glioma Patients
The correlation analysis of perceived social support, resilience and FCR in glioma patients was shown in Table 5. The perceived social support in glioma patients was negatively correlated with FCR (P<0.01); resilience was negatively correlated with FCR (P < 0.01); perceived social support was positively correlated with resilience (P < 0.01). Among them, the dimensions of friend support and tenacity were significantly correlated with FCR.
 |
Table 5 Correlation Between Perceived Social Support, Resilience and FCR in Glioma Patients |
Path Analysis of Perceived Social Support, Resilience and FCR in Glioma Patients
Using FCR as the dependent variable, perceived social support as the independent variable and resilience as the mediating variable, we constructed path analysis model with resilience as the mediating effect. The fitting parameters of structural equation model were χ2/DF = 1.157, GFI = 0.976, AGFI = 0.94, NFI = 0.967, CFI = 0.986, RMSEA = 0.053, IFI = 0.974, and RMR = 0.006. The path analysis model of perceived social support, resilience and FCR in glioma patients is shown in Figure 1. The path coefficients between perceived social support, resilience and FCR were significant (P < 0.05). Perceived social support and resilience in glioma patients had direct effect on FCR (path coefficients were −0.544 and −0.890, respectively). Perceived social support also indirectly affected FCR through resilience (Table 6).
 |
Table 6 Effect Values of Influencing Factors of FCR in Glioma Patients |
 |
Figure 1 Path analysis model of perceived social support, resilience and FCR in glioma patients. Note: *P<0.05. |
Discussion
Resilience is inherent psychological quality of individuals and an important protective factor for mental health. The results of this study showed that the score of resilience in glioma patients was 52.94±10.05, lower than the norm score of resilience of 65% in healthy controls reported by Yu et al.7 It is expected that the level of resilience will decrease when individuals facing trauma or suffer from major diseases. We found that the score of family support was the highest and the score of friend support was the lowest, which may be related to the tradition of Chinese to regard family as the main source of support.
The score of FCR in glioma patients was 29.52±8.30, higher than the score of 25% reported previously.8 We found that perceived social support in glioma patients was negatively correlated with FCR. Perceived social support can predict negative psychological emotions of individuals, and is an important factor to promote behavior and development.9 Social support can help patients reduce psychological pain and reduce stress response. Individuals with high social support are more likely to seek the help of relatives, friends and medical staff, and improve the confidence in overcoming diseases, thereby reducing the level of FCR. In addition, we found a significant negative correlation between resilience and FCR in glioma patients. Fear conditioning is mainly mediated by the amygdala cortex, and high resilience can effectively inhibit the activity of the medial prefrontal cortex of the amygdala, thereby reducing fear.10 In addition, individuals with high resilience usually adopt a positive coping style to face diseases, thereby reducing the level of FCR. The results of this study showed a significant positive correlation between perceived social support and resilience in glioma patients. Perceived social support and resilience jointly reduce the level of FCR.
In fact, perceived social support can affect FCR through resilience.11 The direct effect of perceived social support on FCR is reflected in the emotional, material and information support from family, relatives and friends, and society, which help patients adapt to the difficulties and accelerate the recovery of mental health. Furthermore, resilience and perceived social support jointly act on FCR from internal and external aspects to help patients better face cancers. Social support has been proposed as effective method for cancer management.12–16
In conclusion, this study showed that 36.7% of glioma patients had FCR. The level of FCR in glioma patients decreased with the increase of their perceived social support and resilience, and resilience may play a mediating role in perceived social support and FCR. The resilience of glioma patients can be improved by enhancing the perceived social support, leading to reduced FCR.
Funding
This study received no funding.
Disclosure
The authors declare no conflicts of interest.
References
1. Alfonso JCL, Talkenberger K, Seifert M, et al. The biology and mathematical modelling of glioma invasion: a review. J R Soc Interface. 2017;14(136):20170490. doi:10.1098/rsif.2017.0490
2. Ozlem OZ, Novel A. Mutation in Neurofibromatosis Type 1 with Optic Glioma. Oncologie. 2020;22(3):155–160. doi:10.32604/oncologie.2020.014087
3. Lebel S, Ozakinci G, Humphris G, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016;24(8):3265–3268. doi:10.1007/s00520-016-3272-5
4. Simard S, Thewes B, Humphris G, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–322. doi:10.1007/s11764-013-0272-z
5. Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. 2011;52(3):199–209. doi:10.1016/j.psym.2011.01.036
6. Yang YS, Bae SM. Association between resilience, social support, and institutional trust and post-traumatic stress disorder after natural disasters. Arch Psychiatr Nurs. 2022;37:39–44. doi:10.1016/j.apnu.2022.01.001
7. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Pers. 2007;35(1):19–31. doi:10.2224/sbp.2007.35.1.19
8. Hinz A, Mehnert A, Ernst J, Herschbach P, Schulte T. Fear of progression in patients 6 months after cancer rehabilitation-a-validation study of the fear of progression questionnaire FoP-Q-12. Support Care Cancer. 2015;23(6):1579–1587. doi:10.1007/s00520-014-2516-5
9. Inhestern L, Bultmann JC, Beierlein V, et al. Parenting concerns and psychological burden in cancer patients with minor and young adult children. Psychother Psychosom Med Psychol. 2017;67(7):279–287. doi:10.1055/s-0043-110139
10. Egger S, Hughes S, Smith DP, et al. Factors associated with the use of complementary and alternative medicines for prostate cancer y long-term survivors. PLoS One. 2018;13(3):e0193686. doi:10.1371/journal.pone.0193686
11. Ferrari M, Ripamonti CI, Hulbert-Williams NJ, Miccinesi G. Relationships among unmet needs, depression and anxiety in non-advanced cancer patients. Tumori. 2019;105(2):144–150. doi:10.1177/0300891618765546
12. Wang Z, Peng H, Shi W, et al. Application of photodynamic therapy in cancer: challenges and advancements. Biocell. 2021;45(3):489–500. doi:10.32604/biocell.2021.014439
13. Committee of Diagnosis T, and Fertility Management of Chinese Young Breast Cancer Patients. Expert consensus on diagnosis, treatment and fertility management of young breast cancer patients. J National Cancer Center. 2021;1(1):23–30.
14. Kim SJ, Medina M, Delgado R, Miller A, Chang J. Healthcare Utilization Disparities Among Lung Cancer Patients in US Hospitals During 2010–2014: evidence from the US Hispanic Population’s Hospital Charges and Length of Stay. Int J General Med. 2022;15:1329–1339. doi:10.2147/IJGM.S348159
15. Ma F, Wu J, Fu L, et al. Interpretation of specification for breast cancer screening, early diagnosis, and treatment management in Chinese women. J National Cancer Center. 2021;1(3):97–100. doi:10.1016/j.jncc.2021.07.003
16. George M, Smith A, Ranmuthugula G, Sabesan S. Barriers to Accessing, Commencing and Completing Cancer Treatment Among Geriatric Patients in Rural Australia: a Qualitative Perspective. Int J General Med. 2022;15:1583–1594. doi:10.2147/IJGM.S338128
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
