Back to Journals » ClinicoEconomics and Outcomes Research » Volume 14
The Long-Term Healthcare Utilization and Economic Burden of RSV Infection in Children ≤5 Years in Japan: Propensity Score Matched Cohort Study
Authors Chirikov V, Botteman M, Simões EAF
Received 22 July 2022
Accepted for publication 28 October 2022
Published 9 November 2022 Volume 2022:14 Pages 699—714
DOI https://doi.org/10.2147/CEOR.S382495
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Viktor Chirikov,1 Marc Botteman,1 Eric AF Simões2
1OPEN Health, Evidence & Access, Bethesda, MD, USA; 2Department of Pediatrics, University of Colorado School of Medicine, Department of Epidemiology, Center for Global Health, Colorado School of Public Health, and Section of Infectious Disease, Children’s Hospital Colorado, Aurora, CO, USA
Correspondence: Viktor Chirikov, OPEN Health Evidence & Access, Bethesda, MD, 20814, USA, Tel +1 240 821 9662, Email [email protected]
Background: The objective of this study was to estimate the long-term healthcare utilization and cost burden of RSV by chronological age of diagnosis (Year 1, Year 2 and Years 3– 5 cohorts) as well as by gestational age at birth in Japan.
Methods: The JMDC database was used to retrospectively identify RSV and control patients between February 1, 2011 and January 31, 2016 and follow them through December 31, 2017. Infants with RSV infection (n = 9028 in Year 1; n = 4929 in Year 2; n = 2004 in Years 3– 5) were matched to controls (n = 17,886; n = 9351; n = 3655, respectively) based on gestational age and year and quarter of birth; controls were assigned the index date (ie, diagnosis) of their respective match. Covariate-balancing propensity score weights were employed adjusting for remaining imbalances between cohorts. The main outcomes were average cumulative rates for all-cause, asthma/wheezing, and respiratory-related hospitalizations, physician and urgent care/emergency visits and associated costs (reported as 2018 ¥JPY) over 36-months of follow-up since index.
Results: Healthcare utilization was significantly higher among RSV cases for most comparisons. All-cause average differential cost burden was higher for RSV, compared to controls, among the following cohorts: Year 1 full-term (¥ 277,727); Year 2 preterm (¥ 530,302), late preterm (¥ 270,797), full-term (¥ 238,832); Years 3– 5 preterm (¥ 110,057), late preterm (¥ 486,670), full-term (¥ 289,986). While all-cause costs were similar for preterm and late preterm children in the Year 1 cohort, respiratory- and asthma/wheezing-related attributable costs were substantially higher for RSV.
Conclusion: RSV infection had a significant long-term health and economic burden among children infected during their first year of life and later in life. Study findings have import for prevention strategies, currently directed at maternal immunization and monoclonal antibodies for preventing primary RSV infections in the first six months of life and beyond but also for older age not targeted currently.
Keywords: respiratory syncytial virus, long-term follow-up, lower respiratory tract infection, prematurity
Introduction
Causing an estimated 33 million lower respiratory tract infections (LRTI) annually worldwide,1 respiratory syncytial virus (RSV) causes substantial morbidity and mortality among children ages 5 and under. Among children under the age of 5, RSV is responsible for approximately 3.2 million cases of severe LRTI2 and between 66,000 and 199,000 deaths per year.1 RSV infections occur in nearly every child by the age of 2 years,3 and are the leading cause of hospitalizations in this age group.1 Those under the age of 6 months are particularly vulnerable to severe infections requiring hospitalization,4 and about half of all annual deaths from RSV-related bronchiolitis occur within this age group.1,3
Most studies examining the long-term impacts of RSV on recurrent wheezing, asthma, healthcare utilization or costs, study the impacts of disease in the first year of life, sometimes in the first and second and rarely beyond that.5 The reason is that most primary infection with RSV occurs in the first two years of life,6 when most of the severe disease occurs.7 The global burden of disease studies estimate burdens in the first year of life and between one and five years of life, while it is estimated that at least a third of the burden occurs beyond the first year of life.2,8 In a previous study in the US, we observed that the majority of utilization and costs occurred in the first 2 to 3 years following an RSV infection.9,10
In recent years, the number of new RSV cases in Japan has been reported at an all-time high,−rising from weekly number of reported cases of about 3000 at the peak of the season in 2008 to 2009 to more than 7000 at the peak of season from 2014 to 2015.11 The reason for the increase has partially been attributed to an increase in testing and reporting sites, expansion of the insurance system, as well as an increase of RSV cases seen at outpatient clinics.11 With the spread of the coronavirus-19 pandemic and associated imposed infection control measures, the prevalence of RSV in Japan in 2020 was extremely low; however, due to accumulation of susceptible persons during the pandemic and loosening of social restrictions, the year 2021 saw a multi-fold increase in cases compared to the historical norm.12
Estimates of the longitudinal impacts of RSV infection with respect to healthcare resource use (HCRU) and costs are largely unquantified in Japan. Previously published estimates suggest that annual resource use and costs are substantial for children <5 years of age, with an average hospital stay between 6 and 7.5 days, and total healthcare costs between approximately ¥JPY 262,000 ($USD 2374 in 2018) and ¥JPY 420,000 ($USD 3806 in 2018).13,14 However, prior estimates may underestimate the economic burden of RSV based on limited follow-up, which would inadequately capture downstream costs associated with the RSV infection. Beyond initial infections, children who recover from RSV frequently live with long-term respiratory tract complications that commonly require additional healthcare visits and resource use.1,15,16 For example, early life exposure to RSV has been associated with the development of respiratory morbidity including asthma (8–76%), wheezing (4–47%), reduced pulmonary function, and allergic sensitization for up to 13 years.5,17,18
In the context of the resurging RSV epidemic in Japan, the objective of this study was to compare all-cause, respiratory-related, asthma/wheezing-related HCRU and costs between children ages <5 years old who develop RSV and a matched cohort of those who do not over 36 months after the first RSV episode. Three matched cohorts were constructed for those diagnosed with RSV in their first year of life (Year 1 cohort), diagnosis in the second year (Year 2), and diagnosis in third year and after (Years 3–5). The main body of this paper describes results for the Year 1 cohort, while the Supplementary Materials cover results for the other two matched cohorts.
Methods
Data Source and Study Design
Deidentified medical claims data from the Japanese Medical Data Center (JMDC) database were used in accordance with the criteria set forth in the data use agreement. The JMDC is a nationally representative administrative payer database of employed individuals and their families and has been used in a number of publications.19,20 Data elements captured in the database include patient-level demographic and plan enrollment information, inpatient (including admissions billed under the Diagnosis Procedure Combinations (DPC) lump-sum payment system) and outpatient medical claims (eg, diagnosis codes, procedure codes, provider specialty), as well as pharmacy claims (eg, prescription fill/refill dates, drug name/code, dosage, cost). The study protocol was approved by the central investigation review board (IRB) of Advarra. The need for obtaining informed consent was considered exempt from IRB oversight due to the retrospective, de-identified nature of the data maintaining patients’ confidentiality and as such the study complies with the Declaration of Helsinki.
The study design was longitudinal matched birth cohort, where children were matched on calendar year and quarter of birth. The index date for RSV cases was the first date of an RSV event. The pre-index period was defined as the time between birth, during which healthcare resource utilization (HCRU), prophylaxis with palivizumab and costs were measured. Demographic and other clinical characteristics were measured at the birth hospitalization through the subsequent 6 months. HCRU and costs were captured and aggregated on a monthly basis after the index date. The RSV season was defined as the 7 months from September 1 through March 30 based on the distribution of diagnoses observed in the JMDC dataset from 2011 to 2016. This seasonality distribution was consistent with previous estimates for the period up to 2016, in which cases typically began in autumn.21,22
Study Population
Children were identified at birth during the period from February 1, 2011, to January 31, 2016, with follow-up through December 31, 2017. Of those identified, children under the age of 5 years old with continuous health plan enrollment from birth through the first RSV event (index date) and at least 24 months of follow-up after index were included. Children with fewer than 24 months of available claims and those without a birth hospitalization claim were excluded.
RSV cases were identified using ICD-10-CM diagnosis codes for RSV for inpatient and outpatient visits.13,23 Patients without RSV but with unspecified bronchiolitis or pneumonia (UBP), who may exhibit RSV-like symptoms, were also identified and stratified by whether their first UBP diagnosis occurred during the RSV season. This was done with the intent to exclude from the study those with UBP diagnosis during the RSV season and address potential misclassification bias of attributing them to the control group.9,10 Therefore, for the control cohort, children without evidence of RSV or UBP at any time were included and pooled together with children without RSV but with UBP diagnoses outside of the RSV season months; those without RSV but with a diagnosis of UBP during the RSV season were excluded. RSV cases meeting the core definition with a UBP diagnosis within 14 days were assumed to be the same event and the date of the first diagnosis, regardless of whether it was RSV or UBP diagnosis, was used. RSV cases were also grouped by chronological age at diagnosis. Children were grouped according to whether the first RSV diagnosis occurred in the first (within 12 months), second (13 to 24 months), and third or later year (24–60 months) following birth. Additionally, children were grouped into one of the following subgroups by gestational age: preterm (≤34 weeks of gestational age [GA]); late preterm (35–36 weeks); and term (≥37 weeks). In the absence of direct measures of gestational age in JMDC claims, a validated claims algorithm by was used (Supplemental Table 1).24
Outcomes Evaluated/Measured
All-cause, respiratory-related, and asthma/wheezing-related HCRU and costs attributable to RSV for infants <5 years old and matched controls were compared. HCRU was assessed using inpatient, outpatient and emergency/urgent care visits, as well as inpatient supplemental oxygen use, all measured as rates per 100 patient-years; inpatient length of stay was measured in days. Respiratory and asthma – and/or wheezing-related HCRU were differentiated by the presence of select conditions (Supplemental Table 2). Costs were derived from the adjudicated JMDC claims and adjusted to 2018 dollars using the medical care component of the Japanese Consumer Price Index (CPI). Incremental cost differences between the RSV and matched-control cohorts were calculated for all-cause, respiratory-, and asthma/wheezing-related costs.
Statistical Analysis
RSV cases and controls were first matched 1:2 according to the calendar year and quarter of birth. Infants in the control cohort were assigned the index date of the matched RSV cases. These index dates were assigned by sampling from the distribution of the time between the dates for birth hospitalization and first RSV event in the RSV case cohort. The covariate-balancing propensity score (CBPS) methodology was then used to weight matched RSV and control patients and address measurable imbalances between the two groups at baseline.25,26 Covariates used in the propensity score model included clinical and HCRU variables and the pre-index monthly cost trajectory, similar to a prior study.10 Baseline characteristics were compared using weighted summary statistics. Follow-up data were segmented into monthly increments, and the weighted survey means procedure in SAS 9.4 was used to calculate average cumulative cost, similar to previously conducted longitudinal follow-up studies.27,28 Confidence intervals and p-values for the significance of comparisons were obtained using the variance estimates provided by the survey means procedure, which calculates a correction factor accounting for the unequal probability of selection due to the propensity score weights.29,30
Results
Study Population and Characteristics
A total of 15,961 cases of RSV and 30,892 control cases were included in the matched cohorts (Figure 1). Cohorts of increasing prematurity were associated at baseline with a correspondingly higher proportion of multiple births, higher proportion of neonatal intensive care unit (NICU) admission and longer length of NICU stay in the first month of life, higher use of mechanical ventilation, prophylaxis with palivizumab, higher cost, and more chronic conditions. Propensity score weighting resulted in balanced sub-cohorts of RSV children diagnosed in the first (Table 1), second (Supplemental Table 3), and third year or later (Supplemental Table 4) and their associated controls. Total average pre-index costs as well as the receipt of prophylaxis pre-index also were balanced. Among late preterm (71.5 vs 53.9 mg) and term infants (3.2 vs 2.1 mg) in the Year 1 cohort, the control groups had received a slightly higher average cumulative dose of palivizumab compared to those with RSV (Table 1).
 |
Table 1 Demographics and Clinical Characteristics of Matched Cohorts Diagnosed in Year 1 |
 |
Figure 1 Patient disposition. Abbreviations: DOB, date of birth; wGA, weeks of gestational age. |
In instances where large sample sizes led to statistically significant differences between cohorts, these differences were only modest. Residual bias and confounding were investigated by comparing the trajectory of the average cumulative costs between birth and index dates of the matched, propensity-score weighted RSV cases and control cohorts. Constructed cost trajectories through the respective index dates suggested that the RSV case and control cohorts diagnosed in Year 1 were well-balanced (Supplemental Figures 1–3). For Year 2 cohorts, cost trajectory differences pre-index remained slightly imbalanced for preterm and term children. For cases with index dates in Years 3–5, trajectory differentials were more variable with pre-index costs for children in the RSV full-term cohort much higher than their respective matched controls. Term RSV children diagnosed in Year 3–5 remained having higher average cost pre-index (¥980,000 vs ¥708,000) (Supplemental Table 4).
Healthcare Resource Use
HCRU was compared at 36 months post-index, as this was the common time of available follow-up for the 3 cohorts by diagnosis year (Table 2, Supplemental Tables 5 and 6). RSV cases generally had higher HCRU than controls. Over the 36-month follow-up period, respiratory-related
 |
Table 2 Average Cumulative Healthcare Resource Utilization Since Index Among Those Diagnosed in Year 1 (at 36 Months of Follow-Up) |
hospitalizations accounted for most of the differential rates of all hospitalizations between cases and controls, while asthma or wheezing-related hospitalizations accounted for approximately one-third to half of the difference in hospitalization rates.
Cost Burden
For preterm children in the Year 1 cohort, while all-cause costs were similar, attributable respiratory- and asthma/wheezing-related costs were substantially higher for RSV cases, with higher burdens totaling ¥460,748 and ¥167,598, respectively (Table 3). A similar observation was made for late preterm RSV children in Year 1, who had higher attributable respiratory (¥325,146) and asthma/wheezing-related (¥158,208) costs but similar all-cause costs. Full-term infants from the Year 1 cohort were the only cohort with higher all-cause (¥277,727) and respiratory (¥271,605) and asthma/wheezing-related cost burden (¥182,723), respectively.
 |
Table 3 Average Cumulative Total Cost Since Index Among Those Diagnosed in Year 1 (at 36 Months of Follow-Up) |
For the Year 2 cohorts, the all-cause cost burden was ¥530,302 higher for preterm RSV cases, late preterm – ¥270,797 higher, and full term – ¥238,832 higher (Supplemental Table 7).
Costs followed a similar trend for children diagnosed in Years 3–5 for RSV late preterm (¥486,670 higher costs) and for full-term children (¥289,986 higher costs) (Supplemental Table 8); although numerically higher, costs were not statistically different for RSV preterm children, possibly due to small sample size to detect a difference.
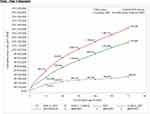
For a holistic view of total costs since birth, average cumulative all-cause costs were graphed by chronological age among the matched, propensity score adjusted cohorts. For the Year 1 cohort, full-term infants with RSV had ¥163,017 higher cost at one year of age, which increased to ¥350,307 at six years of age (Figure 2). For full-term children from the Year 2 cohort, RSV cases had ¥330,730 higher cost by age six (Supplemental Figure 4); for the Year 3–5 cohort – it was ¥605,873 by age six (Supplemental Figure 5).
Figure 2 Continued. Figure 2 Average cumulative total costs since birth by gestational age among matched cohorts diagnosed in Year 1.
Discussion
In our study, we estimated the excess burden of illness and direct costs to the healthcare system, for 36 months following the index case regardless of whether RSV occurred in the first year, second year of 3 to 5 years of life. In our study, we extended our observations to the incremental burden of disease and costs associated with acquiring RSV infection in the 3rd to 5th years of life. Here, we show that regardless of which age RSV was acquired in the first five years of life, and regardless of whether the baby was born preterm, late preterm of full-term, there are significantly higher total respiratory related HCRU and respiratory related costs since index.
It should be noted that for most comparisons, we found healthcare utilization to be significantly higher among RSV cases while all-cost burden was higher only for some of the comparisons. This could be due to the nature of the Japanese healthcare reimbursement system, where certain types of resource utilization are subject to capitated payments and episode of care reimbursement aimed at lowering the cost of care. Japan is one of the countries where healthcare reimbursement is closely regulated, via the adoption of a fee schedule payment system, which sets the price for medical services and pharmaceutical products as well as the rules of billing providers need to follow in order to receive payment.31 Although payment could be made on a fee-for-service basis, billing requirements control the volume of services paid for. Extra billing and balance billing are limited, while the fee schedule and conditions for billing of services are subject to revisions so that total expenditure fits the global budget. As such, the cost burden captured in our study is representative of the specifics of HCRU reimbursement in Japan and higher utilization may not necessarily lead to higher payment like it does in other fee-for-service systems.
An important observation is that for the RSV cohorts, consistently regardless of the age of acquisition of RSV or whether the cohorts were preterm, late preterm or term, about two-thirds of the overall healthcare utilization related to hospitalizations or ER/UC visits were due to respiratory-related causes. In contrast in the control cohorts, respiratory-related causes were closer to a third of this burden. For outpatient visits, by far the largest burden, about a quarter to a fifth of RSV-related visits were respiratory related, similar to the control cohorts. This is not surprising, given the number of well-child visits that every child undergoes. However, consistently, the differential burden of outpatient respiratory visits was significantly higher in every RSV cohort, compared to the controls.
Study findings have import for prevention strategies, currently directed at maternal immunization and monoclonal antibodies for preventing primary RSV infections in the first six months of life.32,33 Meta-analyses of controlled trials of RSV prevention strategies have shown that prevention of RSV in the first year of life has been associated with a reduction in recurrent wheezing for at least the subsequent 3 to 5 years.34 Palivizumab administration to preterm Japanese infants of 33–35 weeks gestation age has been shown to significantly reduce subsequent recurrent wheezing up to 6 years.35 The observations from this study suggest that prevention of RSV should not be limited to the early months of life, but it would be important to consider extending this strategy to older ages.36–40 In the asthma literature, focus has been on unraveling the mechanisms of the association between RSV and subsequent wheezing disease.41 It does appear that an allergic/atopic diathesis predisposes infants to develop severe RSV disease and hospitalization.42 While we did not examine this directly in this study, it can be seen in the trajectories of cost burden since birth that even in the otherwise propensity score matched cohorts, preterm, late preterm and full-term infants from the 3–5-year index groups consistently had higher costs in the RSV cohort and diverged most significantly in the full-term cohort, perhaps supporting this thesis. We were not able to determine whether the RSV subjects in the older cohorts had previously had symptomatic but undiagnosed RSV early in life that led to this divergence, or whether it was an allergic diathesis that underlies this difference. Taken together, our data would suggest that, for preterm and late preterm infants at least, there were no significant differences in the pre-index costs up to the first five years of life, and that perhaps prevention strategies should be directed against these groups for up to 5 years of life.
For the full-term cohort, preventing disease in the first two years of life, might have an impact on not only the burden of disease but on the long-term respiratory healthcare utilization and associated costs. We found in our study that full-term infants who developed RSV had a consistently higher healthcare utilization and cost burden compared to controls, regardless of whether the diagnosis of RSV was made in the first year of life (Tables 2 and 3, Figure 2), the second year of life (Supplemental Tables 5 and 7, Supplemental Figure 4) or between 3 and 5 years of life (Supplemental Tables 6 and 8, Supplemental Figure 5). Most of this burden was respiratory related burden and costs. This is in contrast to the preterm and late preterm infants in the first year of life, in which groups the RSV cohorts had a higher HCRU compared to controls, while the average cumulative costs in the control population were higher than the RSV cohort, resulting in negative differentials. This observation could be because term infants generally were not eligible for prophylaxis with palivizumab, which may have been an important driver to the costs of preterm and late preterm cohorts, who had much higher average dose costs of palivizumab.
The general limitations of using administrative claims data for research purposes apply to our study and residual misclassification bias is possible. Additionally, some of the included infants had received palivizumab prophylaxis after the index date, which might have influenced outcomes observed for preterm infants even after incorporating matching procedures (Supplemental Figure 6). By requiring continuous enrollment since birth, our study could have excluded children who died; however, we expect this to lead to only small bias in burden estimates.
We compared our results to a US study on the total cost burden costs among infants diagnosed with RSV in their first year of life,10 using 2018 exchange rate of $1 = ¥110.34. A main difference between the two studies is that our definition for preterm children included those ≤34 weeks GA, while in the US study it covered <29 weeks and 29–34 weeks separately categorized as early premature and premature. The choice of differing definition in our study was driven by sample size considerations. Followed until 60 months since index among the Year 1 diagnosis cohorts, the attributable total all-cause RSV differential was negative -¥79,433 (-$719.9, not statistically significant) vs approximately $23,160 for preterm/premature; ¥76,642 (USD $694.6, not statistically significant) vs $13,755 for late preterm, and ¥331,136 (USD $3001) vs $6631 for term infants. The cross-country comparison with respect to full-term children diagnosis in the first year of life is especially relevant, given that the US spends on health per capita more than twice than Japan.43 The lack of statistically significant results in pre-term infants could be due to the fact that our Japanese study had 4–5 times lower sample size than the US study. Additionally, there were differences with respect to the extent of palivizumab prophylaxis used among the control arms in the Japanese and US studies. Before propensity score adjustment (but still matched on year and calendar quarter), the proportion of controls pre-index that had palivizumab prophylaxis was 60.7% (Japan) vs 38.9% (US) for those <29 weeks of GA, 36.4% vs 32.7% for 29–34 weeks GA, 21.0% vs 11.8% for 35–36 weeks of GA (ie, late preterm), and 0.5% vs 0.15% for ≥37 weeks of GA (ie, term children). Among the RSV cases, the proportion of children with palivizumab prophylaxis was 71.4% (Japan) vs 49.8% (US) for <29 weeks of GA, 39.9% vs 37.5% for 29–34 weeks of GA, 27.9% vs 16.9% for 35–36 weeks of GA, and 1.1% vs 0.30% for ≥37 weeks of GA. Therefore, the higher use of prophylaxis in Japan may set the expectation for lower scale of differences between RSV and controls as compared to a similar analysis in the US.
Aligned with research priorities to comprehensively examine outcomes that extend beyond just the immediate effect of the acute disease and to follow-up infants until 6 years of age,44 our study examined the all-cause, respiratory-related, and asthma/wheezing-related long-term burden of RSV in Japanese infants diagnosed under 5 years of age. The results from our study suggest that prevention of RSV should not be limited to the early months of life, but it would be important to consider extending this strategy to older children for up to 5 years of life as well as to all children regardless of prematurity.
Data Sharing Statement
Aggregate dataset and data dictionary for healthcare utilization and cost burden at every 12 months of follow-up and associated sample size and confidence intervals can be shared upon request to the corresponding author. This dataset will be available as early as the date of publication. Although de-identified, patient-level datasets will not be shared as per license agreements with the data vendor for the study JMDC.
Ethics Approval and Consent to Participate
The study protocol #Pro00040757 was approved by the central investigation review board (IRB) of Advarra, and the study overall was considered exempt from IRB oversight due to the retrospective, de-identified nature of the data, according to Department of Health and Human Services regulations found at 45 CFR 46.104(d)(4).
Acknowledgments
Medical writing assistance was provided by Kristin Mickle, MPH of OPEN Health, Bethesda, MD. An early version of the analysis was presented at the 57th Annual Meeting of Japanese Society of Pediatric Allergy and Clinical Immunology.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported in part by a research grant from Investigator-Initiated Studies Program of Merck Sharp & Dohme Corp. The opinions expressed in this paper are those of the authors and do not necessarily represent those of Merck Sharp & Dohme Corp.
Disclosure
EAFS reports receiving grant support, paid to his institution, consulting fees, and travel support from AstraZeneca, Merck, Regeneron, Pfizer, and Roche; consulting fees, lecture fees, fees for serving on a data and safety monitoring board, and travel support from AbbVie; consulting fees from Alere; fees for serving on a data and safety monitoring board from GlaxoSmithKline; grant support, paid to his institution, from Johnson & Johnson; and grant support, paid to his institution, and travel support from Novavax. VC and MB report receiving grant support from the MISP program to conduct this study. VC is an employee of and shareholder in OPEN Health. MB is a shareholder in OPEN Health. The authors report no other conflicts of interest in this work.
References
1. Piedra PA. Long-term healthcare costs associated with respiratory syncytial virus infection in children: the domino effect. J Infect Dis. 2020;221(8):1205–1207. doi:10.1093/infdis/jiz161
2. Shi T, McAllister DA, O’Brien KL, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390(10098):946–958. doi:10.1016/S0140-6736(17)30938-8
3. Fonseca W, Lukacs NW, Ptaschinski C. Factors affecting the immunity to respiratory syncytial virus: from epigenetics to microbiome. Front Immunol. 2018;9:226. doi:10.3389/fimmu.2018.00226
4. Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588–598. doi:10.1056/NEJMoa0804877
5. Fauroux B, Simões EAF, Checchia PA, et al. The burden and long-term respiratory morbidity associated with respiratory syncytial virus infection in early childhood. Infect Dis Ther. 2017;6(2):173–197. doi:10.1007/s40121-017-0151-4
6. Glezen WP. Risk of primary infection and reinfection with respiratory syncytial virus. Arch Pediatr Adolesc Med. 1986;140(6):543. doi:10.1001/archpedi.1986.02140200053026
7. Hall CB, Simőes EA, Anderson LJ. Clinical and epidemiologic features of respiratory syncytial virus. Curr Top Microbiol Immunol. 2013;372:39–57. doi:10.1007/978-3-642-38919-1_2
8. Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545–1555. doi:10.1016/S0140-6736(10)60206-1
9. Simões EAF, Chirikov V, Botteman M, Kwon Y, Kuznik A. Long-term assessment of healthcare utilization 5 years after respiratory syncytial virus infection in US infants. J Infect Dis. 2020;221(8):1256–1270. doi:10.1093/infdis/jiz278
10. Chirikov VV, Simões EAF, Kuznik A, Kwon Y, Botteman M. Economic-burden trajectories in commercially insured US infants with respiratory syncytial virus infection. J Infect Dis. 2020;221(8):1244–1255. doi:10.1093/infdis/jiz160
11. Kanou K, Arima Y, Kinoshita H, et al. Respiratory syncytial virus surveillance system in Japan: assessment of recent trends, 2008–2015. Jpn J Infect Dis. 2018;71(3):250–255. doi:10.7883/yoken.JJID.2017.261
12. Ujiie M, Tsuzuki S, Nakamoto T, Iwamoto N. Resurgence of respiratory syncytial virus infections during COVID-19 Pandemic, Tokyo, Japan. Emerg Infect Dis. 2021;27:11. doi:10.3201/eid2711.211565
13. Sruamsiri R, Kubo H, Mahlich J. Hospitalization costs and length of stay of Japanese children with respiratory syncytial virus: a structural equation modeling approach. Medicine. 2018;97(29):e11491. doi:10.1097/MD.0000000000011491
14. Goto S, Ispas G. LATE-BREAKING ABSTRACT: evaluation on RSV disease burden in Japanese children using a nationwide claims database. Eur Respir J. 2016;48(suppl 60):PA1324.
15. Ledbetter J, Brannman L, Wade SW, Gonzales T, Kong AM. Healthcare resource utilization and costs in the 12 months following hospitalization for respiratory syncytial virus or unspecified bronchiolitis among infants. J Med Econ. 2020;23(2):139–147. doi:10.1080/13696998.2019.1658592
16. Shi N, Palmer L, Chu BC, et al. Association of RSV lower respiratory tract infection and subsequent healthcare use and costs: a Medicaid claims analysis in early-preterm, late-preterm, and full-term infants. J Med Econ. 2011;14(3):335–340. doi:10.3111/13696998.2011.578188
17. Henderson J, Hilliard TN, Sherriff A, et al. Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol. 2005;16(5):386–392. doi:10.1111/j.1399-3038.2005.00298.x
18. Sigurs N, Aljassim F, Kjellman B, et al. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax. 2010;65(12):1045–1052. doi:10.1136/thx.2009.121582
19. Kimura S, Sato T, Ikeda S, Noda M, Nakayama T. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol. 2010;20(5):413–419. doi:10.2188/jea.JE20090066
20. Kobayashi Y, Togo K, Agosti Y, McLaughlin JM. Epidemiology of RSV in Japan: a nationwide claims database analysis. Pediatr Int. 2021;64(1):e14957
21. Yamagami H, Kimura H, Hashimoto T, Kusakawa I, Kusuda S. Detection of the onset of the epidemic period of respiratory syncytial virus infection in Japan. Public Health Front. 2019;7:39. doi:10.3389/fpubh.2019.00039
22. Miyama T, Iritani N, Nishio T, et al. Seasonal shift in epidemics of respiratory syncytial virus infection in Japan. Epidemiol Infect. 2021;149. doi:10.1017/S0950268821000340
23. Winterstein AG, Knox CA, Kubilis P, Hampp C. Appropriateness of age thresholds for respiratory syncytial virus immunoprophylaxis in moderate-preterm infants: a cohort study. JAMA Pediatr. 2013;167(12):1118–1124. doi:10.1001/jamapediatrics.2013.2636
24. Li Q, Andrade SE, Cooper WO, et al. Validation of an algorithm to estimate gestational age in electronic health plan databases. Pharmacoepidemiol Drug Saf. 2013;22(5):524–532. doi:10.1002/pds.3407
25. Austin PC, Tutorial A. Case study in propensity score analysis: an application to estimating the effect of in-hospital smoking cessation counseling on mortality. Multivariate Behav Res. 2011;46(1):119–151. doi:10.1080/00273171.2011.540480
26. Imai K, Ratkovic M. Covariate balancing propensity score. J R Stat Soc Series B Stat Methodol. 2014;76(1):243–263. doi:10.1111/rssb.12027
27. Griffiths RI, Gleeson ML, Danese MD, O’Hagan A. Inverse probability weighted least squares regression in the analysis of time-censored cost data: an evaluation of the approach using SEER-Medicare. Value Health. 2012;15(5):656–663. doi:10.1016/j.jval.2012.03.1388
28. Griffiths RI, Gleeson ML, Mikhael J, Dreyling MH, Danese MD. Comparative effectiveness and cost of adding rituximab to first-line chemotherapy for elderly patients diagnosed with diffuse large B-cell lymphoma. Cancer. 2012;118(24):6079–6088. doi:10.1002/cncr.27638
29. DuGoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303. doi:10.1111/1475-6773.12090
30. Bell BA, Onwuegbuzie AJ, Ferron JM, Jiao QG, Hibbard ST, Kromrey JD. Use of design effects and sample weights in complex health survey data: a review of published articles using data from 3 commonly used adolescent health surveys. Am J Public Health. 2012;102(7):1399–1405. doi:10.2105/AJPH.2011.300398
31. Ikegami N. Japan: achieving UHC by regulating payment. Global Health. 2019;15(1):1–6. doi:10.1186/s12992-019-0524-4
32. Griffin MP, Yuan Y, Takas T, et al. Single-dose nirsevimab for prevention of RSV in preterm infants. N Engl J Med. 2020;383(5):415–425. doi:10.1056/NEJMoa1913556
33. Madhi SA, Polack FP, Piedra PA, et al. Respiratory syncytial virus vaccination during pregnancy and effects in infants. N Engl J Med. 2020;383(5):426–439. doi:10.1056/NEJMoa1908380
34. Quinn LA, Shields MD, Sinha I, Groves HE. Respiratory syncytial virus prophylaxis for prevention of recurrent childhood wheeze and asthma: a systematic review. Syst Rev. 2020;9(1):269. doi:10.1186/s13643-020-01527-y
35. Mochizuki H, Kusuda S, Okada K, Yoshihara S, Furuya H, Simões EA. Palivizumab prophylaxis in preterm infants and subsequent recurrent wheezing. six-year follow-up study. Am J Respir Crit Care Med. 2017;196(1):29–38. doi:10.1164/rccm.201609-1812OC
36. Swanson KA, Settembre EC, Shaw CA, et al. Structural basis for immunization with postfusion respiratory syncytial virus fusion F glycoprotein (RSV F) to elicit high neutralizing antibody titers. Proc Natl Acad Sci U S A. 2011;108(23):9619–9624. doi:10.1073/pnas.1106536108
37. Glenn GM, Smith G, Fries L, et al. Safety and immunogenicity of a Sf9 insect cell-derived respiratory syncytial virus fusion protein nanoparticle vaccine. Vaccine. 2013;31(3):524–532. doi:10.1016/j.vaccine.2012.11.009
38. Anderson LJ. Respiratory syncytial virus vaccine development. Semin Immunol. 2013;25:160–171. doi:10.1016/j.smim.2013.04.011
39. Mazur NI, Higgins D, Nunes MC, et al. The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect Dis. 2018;18:e295–e311. doi:10.1016/S1473-3099(18)30292-5
40. Zhu Q, McLellan JS, Kallewaard NL, et al. A highly potent extended half-life antibody as a potential RSV vaccine surrogate for all infants. Sci Transl Med. 2017;9(388):eaaj1928. doi:10.1126/scitranslmed.aaj1928
41. Malinczak CA, Lukacs NW, Fonseca W. Early-life respiratory syncytial virus infection, trained immunity and subsequent pulmonary diseases. Viruses. 2020;12:5. doi:10.3390/v12050505
42. Stensballe LG, Kristensen K, Simoes EAF, et al. Atopic disposition, wheezing, and subsequent respiratory syncytial virus hospitalization in Danish children younger than 18 months: a nested case-control study. Pediatrics. 2006;118(5):E1360–E8. doi:10.1542/peds.2006-0907
43. Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024–1039. doi:10.1001/jama.2018.1150
44. Karron RA, Zar HJ. Determining the outcomes of interventions to prevent respiratory syncytial virus disease in children: what to measure? Lancet Respir Med. 2018;6(1):65–74. doi:10.1016/S2213-2600(17)30303-X
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
