Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
The Link Between Health Literacy and Three Conditions of Metabolic Syndrome: Obesity, Diabetes and Hypertension
Authors Tajdar D , Schäfer I, Lühmann D, Fertmann R, Steinberg T, van den Bussche H, Scherer M
Received 24 February 2022
Accepted for publication 23 April 2022
Published 26 May 2022 Volume 2022:15 Pages 1639—1650
DOI https://doi.org/10.2147/DMSO.S363823
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Daniel Tajdar,1 Ingmar Schäfer,1 Dagmar Lühmann,1 Regina Fertmann,2 Tim Steinberg,1 Hendrik van den Bussche,1 Martin Scherer1
1Department of Primary Care at Hamburg University Medical Center, Hamburg, Germany; 2Hamburg Authority for Work, Health, Social Affairs, Family and Integration, Hamburg, Germany
Correspondence: Daniel Tajdar, Department of Primary Care at Hamburg University Medical Center, Building W37 Martinistraße 52, Hamburg, 20246, Germany, Tel +4940741052400, Fax +4940741040225, Email [email protected]
Purpose: Health literacy (HL) intervention could be a potential prevention strategy to reduce the risk of metabolic syndrome (MS), but the association between low HL and MS is controversial. Therefore, the aim of this study was to investigate whether low HL is associated with obesity, diabetes, and hypertension, considering them as one cluster.
Methods: We used data from the Hamburg Diabetes Prevention Survey, a population-based cross-sectional study in Germany. The 1349 eligible subjects were 18– 60 years old. The European Health Literacy Questionnaire (HLS-EU-Q16) was used to assess HL. Depending on the reported number of metabolic syndrome conditions (CMS), four groups were categorized as follows: “ 0”, any “ 1”, any “ 2” and “ 3” CMS. Ordered logistic regression was used to analyze the relationship between HL level (independent variable) and the reported number of CMS (dependent variable) adjusted for age, gender and education.
Results: 63.9% of subjects (n=862) reported having “ 0”, 25.7% (n=346) only “ 1”, 8.2% (n=111) only “ 2” and 2.2% (n=30) “ 3” of the three CMS. In the group with sufficient HL, rates of “ 1,” “ 2,” or “ 3” CMS were lower than in the group with problematic or inadequate HL. Subjects with inadequate HL showed a 1.62-fold higher risk of having a higher number of CMS than subjects with sufficient HL (OR 1.62; 95% CI 1.13 to 2.31). The risk increased with each life year (OR 1.05; 95% CI 1.04 to 1.06), and was higher in persons with low education (OR 2.89; 95% CI 2.08 to 4.01) than in highly educated persons. Women showed lower risk (OR 0.73; 95% CI 0.58 to 0.91) than men.
Conclusion: Lower HL was associated with a higher number of MS conditions. Our findings suggest that HL intervention on health-promoting behaviors could help reduce MS risk in people with limited HL.
Keywords: diabetes, overweight, health literacy intervention
Introduction
It is estimated that twenty to twenty-five percent of the world’s adult population suffer from metabolic syndrome (MS), which is a cluster of abdominal obesity, elevated fasting plasma glucose or diabetes, high blood cholesterol and hypertension.1 People with MS are three times more likely to have a heart attack or stroke than people without MS.1 While abdominal obesity and insulin resistance are recognized as causative factors of MS, physical activity and a healthy diet are protective factors.1–3 One potentially modifiable risk factor is health literacy (HL), as low HL is associated with behaviors4 that increase the risk of MS, such as smoking,5 inactive lifestyle and poor diet.3 HL is an individual’s ability to access and understand health information in order to make decisions about health care, disease prevention and health promotion.6 As studies have shown, HL status can be improved through educational interventions, leading to changes in health behaviors and better medical outcomes.7–9 In Europe, every second person has limited HL,10 so improving HL seems to be important in the prevention of MS.
However, the relationship between HL and MS conditions such as obesity, type 2 diabetes and hypertension is controversial.11 Some studies have shown associations of lower HL with higher rates of hypertension,12–14 a higher prevalence15,16 and risk17,18 of diabetes, or a higher BMI.11,19 Others found no association with the occurrence of hypertension,16,20 with diabetes prevalence20 or BMI.16,20 Since the evidence is contradictory, the aim of this study was to investigate whether low HL is associated with obesity, diabetes, and hypertension, considering them as one cluster. The results might help develop appropriate intervention programs in order to reduce MS risk in people with limited HL.
Methods
Study Design and Data Sources
For this study, we analyzed data from the Hamburg Diabetes Prevention Survey (HDPS). The HDPS was a population-based cross-sectional study in Germany conducted between December 2017 and March 2018 using computer-assisted telephone interviews. For the HDPS, a sample of private households in Hamburg was selected by randomly dialing landline numbers. The selection was made according to the selection framework for telephone samples of the Arbeitskreis Deutscher Markt- und Sozialforschungsinstitut (ADM).21 ADM is a business association for German market and social research that records all German telephone numbers. For each chosen telephone number a maximum of 10 contact attempts were made on different days of the week and at different times of the day. The telephone interviews were conducted by an independent market and social research institute (USUMA: Unabhängiger Service für Umfragen, Methoden und Analysen).22
A minimum sample size of 1000 randomly selected participants was established for the study. In order to represent low socioeconomic groups more adequately, two additional waves of data collection were conducted to recruit 1) at least 150 individuals with no high school diploma or low secondary education and 2) at least 150 individuals with low or middle secondary education. Due to the HDPS initial design as an observational study with multiple outcomes, we were not able to perform a sample size calculation. Instead, the sample size was determined on the principal investigators’ experience with similar studies. The population was selected by two screening questions at the beginning of the interviews (“What is your highest general education qualification?” and “What is your highest vocational or higher education qualification?”). If subjects from the additional waves did not meet the inclusion criteria of 1) inadequately completed general education, basic general education, or basic vocational qualification, or 2) intermediate education or A-level equivalent but no tertiary education, the interview was terminated after the screening questions and subjects were excluded from the study.
The HDPS included validated instruments such as the 8-item Short-Form Health Survey (SF8) to measure health-related quality of life,23 the short form European Health Literacy Questionnaire (HLS-EU-Q16) to measure health literacy16,24 and items to assess sociodemographic data, health status and subject empowerment. The descriptive results of the HDPS have been published elsewhere.25,26 This manuscript was written according to the STROBE guidelines.27
Study Population
Individuals 18–60 years old who answered the phone, and spoke German were included in the HDPS sample (Figure 1). If several household members were eligible to participate, one was selected at random using the “Kish selection grid”.28 Non-German speaking people were excluded. For our study, we used the HDPS sample. To calculate a summary health literacy assessment, we excluded persons with more than two missing items in the HLS-EU-Q16.
 |
Figure 1 Selection of study subjects *Socio Economic Status. **Health Literacy Score. |
Independent Variables
Independent variables were age, gender, educational level and HL. Age was measured in years, and four age groups were categorized: 18 to 29, 30 to 39, 40 to 49 and 50 to 60 years. Gender was recorded as female or male.
The classification of the Comparative Analysis of Social Mobility in Industrial Nations (CASMIN) was used to assess the educational level of the subjects.29 Three educational levels were categorized according to the CASMIN criteria: Low (insufficiently completed general education, general elementary education or initial vocational qualification), medium (intermediate qualification or equivalent A level qualification) and high (lower or higher tertiary education).29
The HLS-EU-Q16 was used to assess self-reported HL.24,30 The questionnaire has already been validated and applied in several studies.16,20,30–32 The HLS-EU-Q16 consists of 16 questions (Supplementary Material) focusing on four HL dimensions: accessing, understanding, appraising and applying information to make decisions concerning health care (question 1 to 7), disease prevention (question 8 to 12) and health promotion (question 13 to 16).16,31,33 Individuals were asked to answer the HLS-EU questions on a four-point Likert scale with the response categories “very difficult”, “fairly difficult”, “fairly easy”, “very easy” and – as category for missing values – “I do not know”. The HL score was calculated according to the HLS-EU-Q16 manual.30 The answers “fairly easy” and “very easy” were dichotomized to the value 1, the answers “fairly difficult” and “very difficult” were dichotomized to the value 0, and the response “I don’t know” was treated as missing item.30–32 The answer values were then summed (minimum of 0 and maximum of 16 points) and categorized according to the HLS-EU-Q16 criteria as follows:30 0–8 “inadequate”, 9–12 “problematic” and 13–16 “sufficient” HL. For subjects with more than two missing values, the score was not calculated.16,31
Dependent Variables
The dependent variables included 1) the prevalence of each condition of metabolic syndrome (CMS: diagnosed hypertension, diagnosed type 2 diabetes and abdominal obesity), and 2) the number of CMS (0 to 3) reported by the subjects. The operationalization of MS and CMS was based on the definition of the International Diabetes Federation (IDF) which defined MS as abdominal obesity plus having two of the following four factors:1,34
- Elevated triglycerides ≥150 mg/dL or specific treatment for lipid abnormality.
- Reduced high density lipoprotein <40 mg/dL in males and <50 mg/dL in females.
- Elevated blood pressure systolic BP ≥130 or diastolic BP ≥85 mm Hg or treatment of previously diagnosed hypertension.
- Elevated fasting plasma glucose ≥100 mg/dL, or previously diagnosed type 2 diabetes.
During the HDPS interviews individuals were asked about their height and weight, and whether they had been diagnosed with hypertension and/or type 2 diabetes mellitus. Taking ethnicity specific values into consideration, abdominal obesity was defined as having waist circumference (wC) ≥ 80cm in female and ≥ 94cm in male Europeans.1,34 According to the IDF, abdominal obesity can also be assumed without measuring wC if the body mass index (BMI) is >30kg/m2.1,34 Since most people do not know their individual wC, the question was omitted during the HDPS interviews. To include abdominal obesity into our analysis, we calculated the individual BMI (weight in kilograms divided by height in squared meters) using the self-reported weight and height.
Furthermore, HDPS subjects were not asked about lipid abnormalities. Also, laboratory measures were not included into the assessment. Therefore, MS was considered according to the IDF criteria, if subjects reported having the following three conditions simultaneously: abdominal obesity plus diagnosed hypertension plus diagnosed type 2 diabetes. To better understand the relationship between MS and potentially influencing factors, we divided our study population into four groups according to the self-reported number of CMS: “0”, any “1”, any “2” and “3” of the three CMS (abdominal obesity, hypertension, type 2 diabetes).
Statistical Analysis
Descriptive statistics and chi-square tests were performed to investigate differences in the prevalence of each CMS between groups with “inadequate”, “problematic” and “sufficient” HL. Descriptive analyses were also performed to investigate differences in the reported number of CMS (0 to 3) by age, gender, education and HL. We analyzed the relationship between HL level (independent variable) and the reported number of CMS (dependent variable) by an ordered logistic regression analysis adjusted for age, gender and educational level. Coefficients (ß) and odds ratios (OR) were reported with 95% confidence interval (CI). The level of statistical significance was set at P<0.05. All tests were performed using the Stata software version 15.1.
Results
Originally, 1147 people were interviewed for the HDPS. For a better representation of the low socioeconomic groups, an additional 150 persons without school-leaving qualifications or with low secondary education and 158 persons with low or medium secondary education were interviewed. We used the HDPS sample which comprised a total of 1455 subjects. For our study, 106 subjects were excluded due to missing values which resulted in a sample size of 1349 subjects for our analyses (Figure 1).
Characteristics of Subjects
627 (46.5%) subjects were men and the average age was 43.5 years (SD: 12.0). The smallest age group consisted of subjects aged 18–29 years while subjects aged 50–60 years formed the largest age group (Table 1). According to the CASMIN criteria, 248 (18.4%) subjects showed low, 653 (48.4%) medium and 447 (33.2%) high education. According to the criteria of the HLS-EU-Q16, 144 (10.7%) subjects had inadequate, 452 (33.5%) problematic and 753 (55.8%) sufficient HL (Table 1).
 |
Table 1 Subjects Characteristics (N = 1349) |
Prevalence of CMS
In total, 17.1% (n=231) of the study population had abdominal obesity. The proportion of abdominal obesity was slightly higher in subjects with inadequate HL than in subjects with problematic or sufficient HL (Table 2). There was no significant difference between the HL groups (P=0.213). In the study sample, the prevalence of diabetes was 4.1% (n=55). The prevalence of diabetes decreased with increasing HL level (Table 2), and the group difference was not significant (P=0.736). Also, 27.6% (n=372) of the participants had been diagnosed with hypertension (Table 2). In the sufficient HL group, the rate of hypertension was significantly lower than in the problematic or inadequate HL group (P<0.001).
 |
Table 2 Prevalence of Obesity, Diabetes and Hypertension in Different HL Groups (N = 1349) |
Number of CMS
The majority of subjects (63.9%, n=862) had none (0 of 3) of the three conditions of metabolic syndrome (CMS), while 25.7% (n=346) had only “1” and 8.2% (n=111) only “2” of the three CMS in any possible combination. According to the IDF criteria, 2.2% (n=30) of the participants showed MS (“3” CMS) as they reported abdominal obesity plus hypertension plus type 2 diabetes.
In regard to age, the older age groups had more CMS than younger groups (Table 3). Also, the risk of having a higher number of CMS increased with age (OR 1.05 for one life year difference; 95% CI 1.04 to 1.06) (Table 4). Overall, female groups had fewer CMS than male groups (Table 3). Women were less likely to have a higher number of CMS (OR 0.73; 95% CI 0.58 to 0.91) than men (Table 4).
 |
Table 3 Reported Number of CMS* by Age, Gender, Education and HL (N = 1349) |
 |
Table 4 Potential Influencing Variables of the Number of CMS* (N = 1349) |
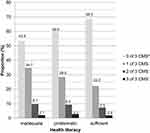
Subjects with high education had fewer CMS than subjects with low education (Table 3 and Figure 2). The number of CMS was inversely associated with the level of education (Table 4). The risk for subjects with low educational level was 2.89 times higher (95% CI 2.08 to 4.01) than for subjects with high educational level.
 |
Figure 2 Comparison of the number of CMS* between educational levels**. *Conditions of metabolic syndrome: obesity, hypertension, type 2 diabetes. **Categorized according to the CASMIN criteria. |
The group with sufficient HL had the highest proportion of subjects with “0” CMS compared to the group with problematic or inadequate HL (Table 3). In addition, the rates of “1,” “2,” or “3” CMS were lowest in the group with sufficient HL, although the rate of “3” CMS (2.0%, n=15) was similar to that in the group with problematic (2.7%, n=12) and inadequate HL (2.1%, n=3) (Figure 3). The risk of having a higher number of CMS increased as the HL level decreased (Table 4). Subjects with inadequate HL were 1.62 times more likely (95% CI 1.13 to 2.31) to have more CMS than subjects with sufficient HL.
Discussion
Statement of Principal Findings
The main objective of this study was to investigate whether low HL is associated with metabolic syndrome conditions (CMS) such as abdominal obesity, type 2 diabetes, and hypertension. We examined the relationship by considering the three CMS as one cluster. Our results suggest an inverse relationship between HL and the reported number of these CMS. Subjects with inadequate HL had a higher risk of having more CMS than subjects with sufficient HL.
Strengths and Limitations
A strength of our study was the use of the short version of the European Health Literacy Questionnaire (HLS-EU-Q16), which had previously been used in several studies.16,24,30–32 The HLS-EU-Q16 can be easily applied and evaluated using online tools. Therefore, this tool is suitable for the identification of individuals with limited HL in future prevention programs. The comparison of our results with other findings was limited as previous studies used different tools to assess HL,10–14,16,31,35 or assessed and categorized the HLS-EU-Q16 differently altogether. In some studies, the questionnaire was given a score of 0 to 50 points and divided into four categories (inadequate, problematic, sufficient and excellent)10,16,20 while in other studies it was given a score of 0 to 16 points and divided into three categories (inadequate, problematic and sufficient).30–32 We applied the HLS-EU-Q16 with three categories due to its short and easy handling.24,32 However, distribution of HL in our study population was consistent with the results of the German Health Update and the European Health Literacy Survey.10,31
Also, type 2 diabetes is most commonly seen in elderly people36 but with an age range of 18–60 years, our study population was comparatively young, which may have led to an underestimation of the prevalence of diabetes. In some cases, the information of the respondents about the values needed to calculate our dependent variable might have been outdated (eg, if the patients last measured their weight a long time ago). Therefore, some of the conditions of metabolic syndrome might have been misclassified in our study. As our data were questionnaire-based and laboratory testing was omitted we cannot compare the rate of MS in our study population (2.2%) to the results of the prevalence studies (>20%).1,37 Thus, subjects with elevated fasting plasma glucose, high blood cholesterol, and unknown hypertension could not be identified and were therefore not included in our analyses. However, the aim of our study was to investigate the association between HL and conditions of MS such as obesity, type 2 diabetes, and hypertension, as these CMS can easily be evaluated by questionnaires and without laboratory measurements. This could help to identify people at high MS risk, and provide support in cost-effective prevention approaches.
Furthermore, the link between HL and MS should be viewed with caution as our analyses were based on a cross-sectional survey. Socially desirable responses and selection bias cannot be excluded due to HDPS data collection through telephone interviews. Non-German speaking adults were excluded since the survey was conducted in German language only. This may have led to overestimation of HL32,38 and underestimation of MS conditions.39 In addition, the HDPS was only conducted in a metropolitan area which could have had an influence on the perception of medical care and in thus on HL.
The low rate of participants (21.4%, n = 6272) who completed the telephone interview has to be mentioned as another limitation. Here, we need to point out that many of the randomized phone numbers had a free line signal but did not belong to a household hence, lowering the response rate. It should also be noted that the study had to be conducted without a sample size calculation. Therefore, we may have missed significant predictors of our results due to limited statistical power.
Comparison with Literature
The distribution of HL in our study population was consistent with findings reported in the German Health Update and the European Health Literacy Survey.10,31 Our results did not show an association between HL and diabetes prevalence. Yet, two previous studies showed such an association.15,16 The first study was based on data from older US Americans with a mean age of 75.6 years15 while the CARLA study, included an older Eastern German urban population with a mean age of 69.9 years.16 As type 2 diabetes is more common in older people,36 the older age of the study populations may explain why a link was found between HL and diabetes prevalence. Compared to both studies, our study population was younger with an average age of 43.5 years. However, a representative survey of users of the German statutory health insurance (WIDO study) also found no association between HL and diabetes prevalence.20
We found no association between HL and obesity. Using the European HLS Questionnaire, the CARLA and the WIDO study also showed no association between HL and BMI,16,20 while a study from Portugal reported an association between HL and BMI.19 The German Health Update also showed a higher prevalence of obesity among adults with inadequate HL.31 Using the Mandarin HLS Questionnaire, a recent study from Taiwan suggested that high HL was associated with less obesity.11
We found a significantly higher rate of hypertension in subjects with lower HL. A cohort study of over 46,000 hospitalized patients showed that hypertension was more common in people with low HL.13 In addition, two studies from South Korea (n=103) and Japan (n=320) demonstrated that low HL was associated with higher rates of hypertension.12,14 Population-based studies in Germany such as the WIDO and the CARLA studies did not show an association between low HL and the occurrence of hypertension.16,20
According to the IDF criteria, subjects with abdominal obesity plus type 2 diabetes plus hypertension were classified as patients with metabolic syndrome (MS).1 We observed similar rates of MS in different HL groups. The MS rate in our study population was very low (2.2%) as no laboratory measures were performed and therefore, subjects with elevated fasting plasma glucose, high blood cholesterol and unknown hypertension were not identified. However, two previous studies revealed inconsistent results regarding the association between HL and MS. Yokokawa et al showed that HL was inversely associated with MS prevalence only in men,35 while Cheng et al found that lower HL was associated with MS in women but not in men.11
With regard to CMS prevalence, our results were similar to those in previous publications with conflicting evidence that low HL may be associated with higher occurrence of obesity,11,16,19,20,31 type 2 diabetes15,16,20 or hypertension.12–14,16,20 The inconsistency could be explained by the use and evaluation of HL with different instruments in previous studies. Also, the study design of most studies, including our approach, were cross-sectional.11,12,19,20,31,35 As obesity, type 2 diabetes and hypertension are highly interlinked2,36 they may occur in different order over the course of life. When analyzing the relationship between them and HL in a cross-sectional approach, these MS conditions should be considered as one cluster rather than analyzing them separately. Therefore, we analyzed the reported number of CMS (0 to 3) in groups with different HL level (inadequate, problematic, sufficient HL) and observed more CMS in groups with limited HL. Using this method, our results could confirm the results of the CARDIA study, a prospective study of 4192 adults aged 18–30 years, which were followed for 15 years.3 The CARDIA study revealed that the risk of MS increased with age and was higher in people with low education. Women showed lower risk of MS than men.3 In line with these findings, our analyses showed the risk of having a higher number of CMS increased with age and was higher in people with low education than in highly educated people. Women showed a lower risk than men. In addition, we found that subjects with inadequate HL had a 1.62-fold higher risk of having more CMS than subjects with sufficient HL.
Implications for Clinical Practice
Our results showed an inverse relationship between HL and the reported number of MS conditions. The association of low HL with behaviors4 that increase the risk of MS such as smoking,5 poor diet and an inactive lifestyle could count as one explanation.3 The aspect that people with higher HL have higher self-efficacy and self-care behaviors could count as another.40 Interlinked with type 2 diabetes and hypertension,2,36 abdominal obesity is a prerequisite risk factor of MS.1 Lifestyle changes such as healthy diet and physical activity can help to lose weight and reduce the risk of MS.1–3,41 As shown in two intervention studies, high HL levels correlate significantly with weight loss success.42,43 Other studies have demonstrated that HL intervention can improve HL7–9 and also lead to lifestyle changes. Therefore, our results suggest that people with limited HL and increased risk of MS could be identified cost-effectively by questionnaires and without laboratory measurements. For example, the use of online tools could be implemented in this context. HL interventions could then help improve the HL in order to reduce the MS risk.
Conclusion
Our study confirmed previous findings that increasing age, low educational attainment and male gender are associated with MS. Also, our findings indicate that low HL may be another risk factor for MS. Appropriate questionnaires such as the HLS-EU-Q16 can be used in cost-effective prevention programs to identify people with low HL and increased risk of MS. HL interventions on health-promoting behaviors could then help reduce the MS risk.
Abbreviations
ADM, Arbeitskreis Deutscher Markt- und Sozialforschungsinstitut; CASMIN, Comparative Analysis of Social Mobility in Industrial Nations; HL, Health Literacy; IDF, International Diabetes Federation; MS, Metabolic Syndrome; CMS, Conditions of Metabolic Syndrome; HLS, Health Literacy Score; HLS-EU-Q16, European Health Literacy Survey Questionnaire, 16 items version; HDPS, the Hamburg Diabetes Prevention Survey; USUMA, Unabhängiger Service für Umfragen, Methoden und Analysen.
Data Sharing Statement
The data that support the findings of this study are available from the Department of Primary Care at Hamburg University Medical Center. Restrictions apply to the availability of these data which were used under license for the current study, and so are not publicly available. However, data are available from the authors upon reasonable request and with permission of the Hamburg Authority of Health and Consumer Protection.
Ethics Approval and Informed Consent
For this analysis we used data from the Hamburg Diabetes Prevention Survey which were collected between December 2017 and March 2018. The informed consent to participate was verbally obtained as the survey was conducted by using telephone interviews, and the data were collected in anonymized form. The use of the survey data for our study was approved by the “Local Psychological Ethics Committee at the Center for Psychosocial Medicine of the University Medical Center Hamburg-Eppendorf” on July 24th 2019 (Approval-No. LPEK-0057). We confirm that our study complies with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The HDPS study was supported by the Hamburg Authority for work, health, social affairs, family and integration. The funding body participated in the study design, but had no role in collection, analysis, and interpretation of data and in writing the manuscript.
Disclosure
Prof. Dr. Martin Scherer reports A+ Videoclinic GmbH; M. Scherer is Partner and Medical Director President of the German College of General Practitioners and Family Physicans (DEGAM). The authors declare that they have no competing interests.
References
1. IDF. Consensus worldwide definition of the metabolic syndrome. Available from: https://www.idf.org/our-activities/advocacy-awareness/resources-and-tools/60:idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html.
2. Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi:10.1056/NEJM200105033441801
3. Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K. Risk factors for the metabolic syndrome: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985–2001. Diabetes Care. 2004;27(11):2707–2715. doi:10.2337/diacare.27.11.2707
4. World Health Organization. Health literacy. The solid facts. Self; 2018.
5. Sun K, Liu J, Ning G. Active smoking and risk of metabolic syndrome: a meta-analysis of prospective studies. PLoS One. 2012;7:10.
6. Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi:10.1186/1471-2458-12-80
7. Tavakoly Sany SB, Doosti H, Mahdizadeh M, Orooji A, Peyman N. The health literacy status and its role in interventions in Iran: a systematic and meta-analysis. Int J Environ Res Public Health. 2021;18(8):4260. doi:10.3390/ijerph18084260
8. Walters R, Leslie SJ, Polson R, Cusack T, Gorely T. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health. 2020;20(1):1–17. doi:10.1186/s12889-020-08991-0
9. Tavakoly Sany SB, Behzhad F, Ferns G, Peyman N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res. 2020;20(1):1–10. doi:10.1186/s12913-020-4901-8
10. Sørensen K, Pelikan JM, Röthlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. 2015;25(6):1053–1058. doi:10.1093/eurpub/ckv043
11. Cheng Y-L, Shu J-H, Hsu H-C, et al. High health literacy is associated with less obesity and lower Framingham risk score: sub-study of the VGH-HEALTHCARE trial. PLoS One. 2018;13(3):e0194813. doi:10.1371/journal.pone.0194813
12. Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. 2009;18(16):2337–2343. doi:10.1111/j.1365-2702.2008.02739.x
13. McNaughton CD, Kripalani S, Cawthon C, Mion LC, Wallston KA, Roumie CL. Association of health literacy with elevated blood pressure: a cohort study of hospitalized patients. Med Care. 2014;52(4):346. doi:10.1097/MLR.0000000000000101
14. Shibuya A, Inoue R, Ohkubo T, et al. The relation between health literacy, hypertension knowledge, and blood pressure among middle-aged Japanese adults. Blood Press Monit. 2011;16(5):224–230. doi:10.1097/MBP.0b013e32834af7ba
15. Sudore RL, Mehta KM, Simonsick EM, et al. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54(5):770–776. doi:10.1111/j.1532-5415.2006.00691.x
16. Tiller D, Herzog B, Kluttig A, Haerting J. Health literacy in an urban elderly East-German population – results from the population-based CARLA study journal article. BMC Public Health. 2015;15(1):883. doi:10.1186/s12889-015-2210-7
17. Tajdar D, Lühmann D, Fertmann R, et al. Low health literacy is associated with higher risk of type 2 diabetes: a cross-sectional study in Germany. BMC Public Health. 2021;21(1):1–12. doi:10.1186/s12889-021-10508-2
18. O’Meara L, Williams SL, Ames K, Lawson C, Saluja S, Vandelanotte C. Low health literacy is associated with risk of developing type 2 diabetes in a nonclinical population. Diabetes Educ. 2019;45(4):431–441. doi:10.1177/0145721719857548
19. Cunha M, Gaspar R, Fonseca S, Almeida D, Silva M, Nunes L. Implications of literacy for health for body mass index. Aten Primaria. 2014;46:180–186. doi:10.1016/S0212-6567(14)70088-5
20. Zok K. Unterschiede bei der Gesundheitskompetenz. Ergebnisse einer bundesweiten Repräsentativ. 2014;11(2):1–12.
21. ADM. Business association for German market and social research. Available from: http://www.adm-ev.de.
22. USUMA. Independent market and social research institute. Available from: http://www.usuma.com/&lang=en/_0.
23. Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln. 2001;15(10):5.
24. Consortium H-E. HLS-EU-Q16. The European health literacy survey questionnaire - short version. Available from: https://www.healthliteracyeurope.net/hls-eu.
25. FHH-BGV/Freie und Hansestadt Hamburg. Behörde für Gesundheit und Verbraucherschutz (2018): Risikofaktoren und Prävention von Diabetes in Hamburg [FHH-BGV/Freie und Hansestadt Hamburg. Authority for Health and Consumer Protection (2018): Risk factors and prevention of diabetes in Hamburg.]. Available from: https://www.hamburg.de/contentblob/12186100/3328c8a0b570a44eeaeb647bdaaec0aa/data/download-diabetesbericht.pdf.
26. FHH-BGV/Freie und Hansestadt Hamburg. Behörde für Gesundheit und Verbraucherschutz [FHH-BGV/Freie und Hansestadt Hamburg. Authority for Health and Consumer Protection.]. Available from: https://www.hamburg.de/contentblob/12694606/549bef6d45d1fd957a702edf5bb7512d/data/gesundheitskompetenz-in-hamburg-2018-%E2%80%93-ergebnisse-einer-telefonischen-befragung.pdf.
27. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31. doi:10.4103/sja.SJA_543_18
28. Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44(247):380–387. doi:10.1080/01621459.1949.10483314
29. Brauns H, Steinmann S. Educational reform in France, West-Germany and the United Kingdom: updating the CASMIN educational classification. Zuma Nachrichten. 1999;23(44):7–44.
30. Röthlin F, Pelikan J, Ganahl K. Die Gesundheitskompetenz der 15-jährigen Jugendlichen in Österreich. Abschlussbericht der österreichischen Gesundheitskompetenz Jugendstudie im Auftrag des Hauptverbands der österreichischen Sozialversicherungsträger (HVSV) [The health literacy of 15-year-old adolescents in Austria. Final report of the Austrian Health Competence Youth Study commissioned by the Main Association of Austrian Social Insurance Institutions (HVSV).]. The health competence of; 2013.
31. Jordan S, Hoebel J. Health literacy of adults in Germany: findings from the German health update (GEDA) study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2015;58(9):942–950. doi:10.1007/s00103-015-2200-z
32. Wångdahl J, Lytsy P, Mårtensson L, Westerling R. Health literacy among refugees in Sweden – a cross-sectional study. journal article. BMC Public Health. 2014;14(1):1030. doi:10.1186/1471-2458-14-1030
33. Domanska OM, Firnges C, Bollweg TM, Sørensen K, Holmberg C, Jordan S. Do adolescents understand the items of the European health literacy survey questionnaire (HLS-EU-Q47)–German version? Findings from cognitive interviews of the project “Measurement of Health Literacy Among Adolescents”(MOHLAA) in Germany. Arch Public Health. 2018;76(1):46. doi:10.1186/s13690-018-0276-2
34. Zimmet P, Alberti KGM, Serrano Ríos M. A new international diabetes federation worldwide definition of the metabolic syndrome: the rationale and the results. Rev Esp Cardiol. 2005;58(12):1371–1375. doi:10.1016/S0300-8932(05)74065-3
35. Yokokawa H, Fukuda H, Yuasa M, Sanada H, Hisaoka T, Naito T. Association between health literacy and metabolic syndrome or healthy lifestyle characteristics among community-dwelling Japanese people. Diabetol Metab Syndr. 2016;8(1):30. doi:10.1186/s13098-016-0142-8
36. IDF. IDF Diabetes Atlas.
37. Moebus S, Hanisch J, Bramlage P, et al. Regional differences in the prevalence of the metabolic syndrome in primary care practices in Germany. Dtsch Ärztebl int. 2008;105(12):207. doi:10.3238/artzebl.2008.0207
38. Berens E-M, Vogt D, Messer M, Hurrelmann K, Schaeffer D. Health literacy among different age groups in Germany: results of a cross-sectional survey. BMC Public Health. 2016;16(1):1151. doi:10.1186/s12889-016-3810-6
39. Bennet L, Groop L, Lindblad U, Agardh C-D, Franks PW. Ethnicity is an independent risk indicator when estimating diabetes risk with FINDRISC scores: a cross sectional study comparing immigrants from the Middle East and native Swedes. Prim Care Diabetes. 2014;8(3):231–238. doi:10.1016/j.pcd.2014.01.002
40. Khorasani EC, Sany SBT, Orooji A, Ferns G, Peyman N. Health literacy in Iranian women: a systematic review and meta-analysis. Iran J Public Health. 2020;49(5):860.
41. Group DPPR. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi:10.2337/diacare.25.12.2165
42. Carels RA, Selensky JC, Rossi J, Solar C, Hlavka R. A novel stepped-care approach to weight loss: the role of self-monitoring and health literacy in treatment outcomes. Eat Behav. 2017;26:76–82. doi:10.1016/j.eatbeh.2017.01.009
43. Zoellner J, You W, Almeida F, et al. The influence of health literacy on reach, retention, and success in a worksite weight loss program. Am J Health Promot. 2016;30(4):279–282. doi:10.1177/0890117116639558
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.