Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
The Knowledge Profile, Competence and Pending Problems of Chinese Anesthesiologists in Dealing with Malignant Hyperthermia: A Cross-Sectional Survey
Authors Tan L, Yu H, Yan J, Liu C, Xiao K, Yin J, Zuo Y , Zhu T, Deng X
Received 2 September 2022
Accepted for publication 5 December 2022
Published 17 January 2023 Volume 2023:16 Pages 133—142
DOI https://doi.org/10.2147/JMDH.S387025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Lingcan Tan,1 Hong Yu,1 Junyu Yan,2 Chunyuan Liu,3 Kun Xiao,4 Jin Yin,5 Yunxia Zuo,1 Tao Zhu,1 Xiaoqian Deng1
1Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, 610041, People’s Republic of China; 2Department of Anesthesiology, Karamay Hospital of Integrated Traditional Chinese and Western Medicine, Karamay, People’s Republic of China; 3Department of Anesthesiology, Chongqing Liangping District People’s Hospital, Chongqing, 405200, People’s Republic of China; 4School of Information and Software Engineering, University of Electronic Science and Technology of China, Chengdu, 610054, People’s Republic of China; 5West China Biomedical Big Data Center, West China Hospital, Sichuan University, Chengdu, 610041, People’s Republic of China
Correspondence: Xiaoqian Deng, Department of Anesthesiology, West China Hospital, Sichuan University, No. 37 Guoxue Alley, Chengdu, 610041, People’s Republic of China, Email [email protected]
Purpose: The National Remote Emergency System for Malignant Hyperthermia (MH-NRES) is an applet in China, designed to help anesthesiologists manage MH crisis. However, there is limited information about encountered difficulties in dealing with MH among Chinese anesthesiologists. The purpose of the study was to explore the current competency and encountered difficulties in the management of MH, as a key first step for assessing the potential user needs to develop the MH-NRES.
Methods: The hospitals of different levels in different provinces across China were invited to participate in an online survey from November to December 2021. Anesthesiologists completed the online questionnaire containing four sections including demographic information, knowledge, competency, and continuing education about MH.
Results: A total of 1357 valid questionnaires were completed from anesthesiologists, most respondents (66.7%, n = 905) correctly answered the MH trigger drugs included volatile anesthetics and succinylcholine. However, most respondents (77.0%, n = 1045) did not know that the recommended initial dose of domestic dantrolene. Up to 83.9% (n = 1138) stated that their hospitals did not store dantrolene for MH emergency. More than half of respondents thought that it would take more than one hour to obtain dantrolene in emergency. Less work experiences, lower levels of hospital and educations and professional titles were associated with lower competency scores in managing MH. Only 31.0% (n = 936) reported that their hospital had ever conducted MH continuing education curricula. Scenario simulation is the training method that most interests the participants (79.0%, n = 1072) but a whopping 46.9% (n = 637) never received simulation.
Conclusion: The study indicated that difficulty in obtaining dantrolene, lack of competency in management of MH, difficulty in obtaining professional help, and poor teamwork were the main problems of most anesthesiologists in face of MH.
Keywords: malignant hyperthermia, questionnaire, competency, dantrolene, education
Introduction
Malignant hyperthermia (MH) is a rare pharmacogenetic disorder of the skeletal muscle, which is associated with mutations in RYR1 and CACNA1S genes, commonly triggered by halogenated inhalational agents or succinylcholine.1–4 MH is considered as one of the most severe anesthesia-related rare diseases associated with rapid progress and high mortality rate.5,6 Early recognition and timely aggressive treatment are essential for the successful management of MH. A key component of the treatment is prompt administration of dantrolene.7,8 In the USA, the MH mortality has dropped from 70% in the 1970s to 9.5% in 1981 with the abundant dantrolene stock in most hospitals, according to a report from the Malignant Hyperthermia Association of the United States (MHAUS).9 However, the latest study analyzed the reported MH case in China from 1985 to 2020, indicating the total mortality was 45.7%.10,11 The high mortality may be attributable to the extremely lack of intravenous (IV) dantrolene in most Chinese hospitals. In the last decades, the imported IV dantrolene was not on the list of government-approved drugs in China, furthering hindering the access of dantrolene in Chinese hospitals. The good news is that domestic IV dantrolene produced by a Chinese pharmaceutical company (Livzon Pharmaceutical Group Co., Ltd, Zhuhai, China) has been approved by the Chinese Food and Drug Administration (CFDA) in October 2020.12 Although increasing hospitals are stocking dantrolene, it will take a long time to achieve the legislation of dantrolene stock for each hospital in China. During this transition period, it may be helpful to use information technology to help anesthesiologists pull through MH crisis.
As mobile health (mHealth) apps are changing the ways of modern medical practice, we planned to develop the National Remote Emergency System for Malignant Hyperthermia (MH-NRES) as an applet of the WeChat app in China,13 which is composed of six functions: quick clinical diagnosis, dantrolene mobilization, instruction on dantrolene use, MH treatment, MH genetic testing and MH case study. However, there is limited information about knowledge, capability, and problems encountered about MH among Chinese anesthesiologists. Thus, we conducted the first online questionnaire survey among Chinese anesthesiologists to determine the competency and pending problems about MH, as a key first step for assessing the potential needs of applet users.
Materials and Methods
After obtaining approval from the Ethics Committee of West China Hospital, Sichuan University (protocol number 2021–1387), this online survey had been conducted among anesthesiologists from hospitals of different levels, from November to December 2021. Based on previous studies and extensive literature search,7,8,14,15 a structured, self-administered, electronic questionnaire was developed and improved entirely by ourself, which took less than 10 min to complete. Participation of the study was entirely voluntary and completely anonymous. Informed consent was included on the front page of the questionnaire, every participant was inquired the willingness to join this survey and only informed consent was obtained, the participant could continue completion of the survey. Before data collection, a pilot study was conducted on 34 anesthesiologists to ensure the validity and practicability, as well as interpretation of respondents. After last modification, the structured electronic questionnaire survey was distributed widely to the anesthesiologists. It was guaranteed that questionnaires were sent to at least one hospital in each province and municipality in China was included, except for Hong Kong, Macao, and Taiwan.
The online questionnaire was conducted by www.wjx.cn (a Chinese questionnaire software platform, providing functions equivalent to Amazon Mechanical Turk). The questionnaire included required fields to prevent incomplete responses, and each WeChat account could only fill out the questionnaire once. The software generated an electronic link and a 2D image code, which could be scanned by participants through the WeChat app on the mobile phone to access and complete the questionnaire.
The questionnaire included four sections. Section 1 addressed demographic information: age, gender, education background, professional title, type of hospital, and work experience as an anesthetist (years). Section 2 contained questions about knowledge about MH, including symptoms, diagnosis and treatments of MH and individual clinical practice to manage MH. Section 3 addressed three questions about participants’ competencies in the management of MH: are you familiar with MH clinical grading score? Do you feel competent in identifying MH patients? Do you feel competent in managing MH crisis? Response choices for the three topics were presented as a 5-point Likert Scale (1 = not at all competent to 5 = extremely competent). For each participant, the total competency score was the sum of the scores of the three questions. In the last section, participants needed to evaluate the current continuing education about MH. Except age, there were no open questions and options were offered a priori for questions.
Statistical analyses were performed using SPSS version 25.0. Frequencies, percentages, and mean (standard deviation, SD) were used to describe the data. Differences between participant groups were tested using independent samples t-tests, chi-square tests, or rank-sum tests. A P value less than 0.05 was considered significant for all tests.
Results
A total of 1511 anesthesiologists completed and responded the electronic questionnaires, and valid questionnaires were retrieved from 1357 of them. The anesthesiologists involved in this survey were from 32 provinces and autonomous regions in China, except for Hong Kong, Macao, and Taiwan. Table 1 lists the characteristics of the 1357 respondents.
 |
Table 1 The Characteristics of the Respondents (n = 1357) |
Knowledge of the Anesthesiologists About MH
Of all valid responses, only 2 of 1357 participants were able to correctly answer the entire set of seven knowledge statements. The majority of respondents (66.7%, n = 905) correctly answered that MH reaction is commonly triggered by volatile anesthetics or succinylcholine, or both. Referring to the common clinical manifestations of MH, 28.4% (385) correctly answered the most common early symptoms, and 9.1% (123) correctly answered the advanced symptoms. Only 5.0% (68) respondents both correctly answered the early and advanced symptoms of MH. More than half of the respondents (57.9%, n = 786) correctly answered that in vitro muscle contraction test was the standard diagnosis of MH, while 28.2% chose genetic testing. However, only 33.8% (n = 458) understood that the correct way to dispense dantrolene is to be dissolved in sterile water. What is more, the majority of respondents (77.0%, n = 1045) did not know that the recommended initial dose of domestic dantrolene is 1mg/kg, 37.9% (n = 514) still chose 2~3mg/kg as the initial dose. Most respondents (96.2%, n = 1305) indicated that end-tidal carbon dioxide was the routine monitoring during general anesthesia. Whereas, up to 58.9% (n = 800) anesthesiologists did not routinely monitor temperature during surgeries that last more than 30 minutes. Table 2 lists the details of MH knowledge items and responses.
 |
Table 2 MH Knowledge Items and Responses |
Stock and Availability of Dantrolene
A whopping 83.86% (n = 1138) of anesthesiologists stated that their hospitals did not store dantrolene for MH emergency. The preferred choice of obtaining dantrolene quickly was to borrow urgently from the nearest hospital that stocks dantrolene (67.0%, n = 909). Nerveless, only 28.3% (n = 384) of the anesthesiologists reported that they were within 50 km of the nearest hospital stockpiling dantrolene. In addition, more than half of respondents stated that it would take more than one hour to obtain dantrolene. Details are shown in Table 3.
 |
Table 3 Availability of Dantrolene |
Competencies of Anesthesiologists in the Management of MH
Table 4 shows the summary results for mean confidence scores about management of MH in terms of different characteristics. Compared with BD and other degrees, both MD and PhD group got higher mean competency scores (P = 0.002 and P = 0.004, respectively). Also, compared with tertiary hospital, anesthesiologists from secondary and lower-level hospitals got lower competency scores (P = 0.003 and P = 0.006, respectively). In addition, the relation between professional titles and competency scores showed a significant trend with higher professional title (P<0.001, Table 4). Besides, the confidence scores increased with increasing work experiences (P<0.001, Table 4).
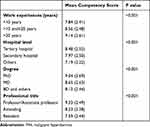 |
Table 4 Competencies of Anesthesiologists in the Management of MH |
Figure 1 shows the summary of main difficulties that may arise during emergency resuscitation of MH patients. Apart from difficulty in obtaining dantrolene (76.6%), lack of confidence in the diagnosis and treatment of MH (47.5~56.0%), difficulty in obtaining professional help (47.8%) and poor teamwork (34.5%) also presents a distinct challenge.
 |
Figure 1 Summary of main difficulties that may arise during emergency resuscitation of MH patients (n = 1357). Abbreviation: MH, malignant hyperthermia. |
MH Continuing Education for Anesthesiologists
Among a total of 1357 respondents, only 31.0% (n = 936) of respondents reported that their hospital had conducted MH continuing education curricula. In terms of individual MH simulation training experience, just 27.0% (n = 366) received MH simulation training with one year, 26.1% (n = 354) received simulation training a year ago, and a whopping 46.9% (n = 637) never received simulation. In the last year, the three ways that anesthesiologists most often received information about MH included textbooks and literatures (75.8%, n = 1028), web science knowledge (74.1%, n = 1006) and intra-departmental teaching (57.4%, n = 779). Overall, although most anesthesiologists never received MH training, scenario simulation is the training method that most interests the anesthesiologists (79.0%, n = 1072). As a type of simulation, scenario simulation can be depicted by an event timeline, which was used for an exercise or to support scenario-based training. It. Details are shown in Table 5.
 |
Table 5 MH Training and Responses |
Discussion
There is a paucity of literature regarding Chinese anesthesiologists’ competency and difficulties encountered about MH. To our knowledge, this is the first survey to evaluate the knowledge, competency, and continuing education regarding MH among anesthesiologists in China. Our results demonstrated imbalanced results regarding MH knowledge. Although most respondents knew well about MH causative drugs and clinical manifestations, the number of respondents who did not know the standard diagnosis and treatment of MH was relatively high. For example, unlike the recommended dosage of 2~3mg/kg from European and USA guidelines,7,8 expert consensus on prevention and treatment of malignant hyperthermia in China (2020 edition) recommends an initial dose of 1 mg/kg of domestic dantrolene, which derives from the package inserts of domestic dantrolene (Livzon Pharmaceutical Group Co., Ltd, Zhuhai, China).14 More than 70% participants did not know the correct dissolution, correct dose and the considerable withdrawal criteria of dantrolene. This could be considered an adverse factor during MH management.
In contrast to earlier findings,9,15–19 our results showed that more than half of the anesthesiologists did not use body temperature monitoring. Moreover, although domestic IV dantrolene has been introduced in October 2020 and there is general agreement that dantrolene should be stocked wherever inhalational anesthetics and succinylcholine are used, the truth in China is that most hospitals lacked preparations of dantrolene in stock. The reluctance to store dantrolene could be explained that it is relatively expensive, has a limited shelf life, and might expire unused as the rarity of MH reactions.3,20–23 Undoubtedly, inadequate intraoperative monitoring methods would impede early detection of MH, furthermore, lack of supplies of dantrolene would delay the appropriate treatment.24 We consider that each hospital manager and chief anesthesiologist have the responsibility to store dantrolene for locations where MH trigger drugs are regularly used, the recommended stock level should be 24–36 vials of dantrolene, and if further dantrolene cannot be obtained within 30 min, an increased stock level should be 48 vials.7
The study showed that, followed by difficulty in obtaining dantrolene, lack of confidence in the diagnosis and treatment of MH, difficulty in obtaining professional help, and poor teamwork were the main concerns of most anesthesiologists during the rescue of MH patients. Furthermore, our findings confirm that Chinese anesthesiologists lacked training for MH. It might imply the necessity to establish an MH website and a telephone hotline available, as well as mHealth apps to offer guidance for anesthesiologists in China.10,13,21,25 In addition, we could find that less work experiences, lower levels of hospital, educations and professional titles were associated with lower competencies in managing MH. This suggests that training should focus more on anesthesiologists with less experienced, lower educations and from primary hospitals. High-quality simulation-based training can be an effective method for developing clinical competency, standardizing the experience, continuing to build base knowledge, and increasing mastery of team functions.26,27 Implementation of a rapid, comprehensive MH crisis management plan may be improved with the use of Stanford MH crisis checklists in a simulated MH scenario, which prompts staff to remember key interventions in the midst of rapid patient deterioration and potential confusion.28 Especially in remote areas that dantrolene is still not readily available, enhanced training for early warning, diagnosis, and prompt effective therapies of MH are crucial to ensure patient safety. It will take a long time to realize the legislation of dantrolene stock for each hospital in China. During this transition period, development of the MH-NRES applet may help anesthesiologists to solve these thorny problems like quick diagnosis, rapid dantrolene mobilization, instruction on treatment and MH simulation.
Some limitations also exist in the study design, because the study was initiated by the West China Hospital of Sichuan University, with easier access to publicize and promote the study in Sichuan province, resulting in 40.97% of the respondents being from Sichuan province. Furthermore, more than half of the hospitals are tertiary A hospitals, with fewer actual primary hospitals participating. Multiple anesthesiologists from the same hospital were invited to join the survey. All the limitations mentioned above could result in bias. Nevertheless, we thought that the hospitals included in our study reflect medical institutions of various levels in various provinces across China, and the study still gives insight on the state of MH rescue practice in China.
Conclusions
As the first online survey to explore the competency and pending problems about MH among anesthesiologists in China, the study shows that difficulty in obtaining dantrolene, lack of confidence in management of MH, difficulty in obtaining professional help, and poor teamwork were the main problems of most anesthesiologists in face of MH crisis. In addition to the pressing need to promote the stock of dantrolene in China, future research could be directed to develop MH-NRES applet to offer professional guidance in solving MH problems, as well as applicable in other developing countries.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to individual privacy of the patients included but are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of West China Hospital, Sichuan University (protocol number 2021-1387). Signed informed consent was obtained from all participants. All participants volunteered to participate and could withdraw from the study at any time. Participants were informed that their personal information would be kept confidential. De-identified data were stored in a locked cabinet in the laboratory.
Consent for Publication
All the patients included signed the consent for publication.
Acknowledgments
We would like to acknowledge the membership of China Malignant Hyperthermia Emergency Assistance WeChat-based Group for their assistance in completing the questionnaires.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The project is funded by National Natural Science Foundation of China (No.72074162).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Rosenberg H, Pollock N, Schiemann A, Bulger T, Stowell K. Malignant hyperthermia: a review. Orphanet J Rare Dis. 2015;10:93. doi:10.1186/s13023-015-0310-1
2. Broman M, Islander G, Müller CR. Malignant hyperthermia, a Scandinavian update. Acta Anaesthesiol Scand. 2015;59(8):951–961. doi:10.1111/aas.12541
3. Correia ACDC, Silva PCB, Silva BAD. Malignant hyperthermia: clinical and molecular aspects. Rev Bras Anestesiol. 2012;62(6):820–837. doi:10.1016/S0034-7094(12)70182-4
4. Litman RS, Smith VI, Larach MG, et al. Consensus statement of the malignant hyperthermia association of the United States on unresolved clinical questions concerning the management of patients with malignant hyperthermia. Anesth Analg. 2019;128(4):652–659. doi:10.1213/ANE.0000000000004039
5. Jones PM, Allen BN, Cherry RA, et al. Association between known or strongly suspected malignant hyperthermia susceptibility and postoperative outcomes: an observational population-based study. Can J Anesth. 2019;66(2):161–181. doi:10.1007/s12630-018-1250-8
6. Rüffert H, Bastian B, Bendixen D, et al. Consensus guidelines on perioperative management of malignant hyperthermia suspected or susceptible patients from the European Malignant Hyperthermia Group. Br J Anaesth. 2021;126(1):120–130. doi:10.1016/j.bja.2020.09.029
7. Glahn KPE, Bendixen D, Girard T, et al. Availability of dantrolene for the management of malignant hyperthermia crises: European Malignant Hyperthermia Group guidelines. Br J Anaesth. 2020;125(2):133–140. doi:10.1016/j.bja.2020.04.089
8. Hopkins PM, Girard T, Dalay S, et al. Malignant hyperthermia 2020: guideline from the association of anaesthetists. Anaesthesia. 2021;76(5):655–664. doi:10.1111/anae.15317
9. Larach MG, Brandom BW, Allen GC, Gronert GA, Lehman EB. Malignant hyperthermia deaths related to inadequate temperature monitoring, 2007–2012: a report from the North American malignant hyperthermia registry of the malignant hyperthermia association of the United States. Anesth Analg. 2014;119(6):1359–1366. doi:10.1213/ANE.0000000000000421
10. Gong X. Malignant hyperthermia when dantrolene is not readily available. BMC Anesthesiol. 2021;21(1):1–11. doi:10.1186/s12871-021-01328-3
11. Xu ZH, Luo AL, Guo XY, et al. Malignant hyperthermia in China. Anesth Analg. 2006;103(4):983–985. doi:10.1213/01.ane.0000237289.66136.cd
12. Li Z, Liu K, Guo X. Dantrolene available in China for malignant hyperthermia treatment. Anesthesiology. 2022;136(3):515–516. doi:10.1097/ALN.0000000000003998
13. Yu H, Tan L, Teng Y, et al. The First National Remote Emergency System for Malignant Hyperthermia (MH-NRES) in China: protocol for the design, development, and evaluation of a WeChat applet. JMIR Res Protoc. 2022;11(6):e37084. doi:10.2196/37084
14. Expert Consensus Working Group on the Prevention And Treatment of Malignant Hyperthermia in China. Expert consensus on the prevention and treatment of malignant hyperthermia in China (2020 edition). Chin J Anesthesiol. 2021;41(1):20–25. doi:10.3760/cma.j.cn131073.20210102.00107
15. Suyama H, Kawamoto M, Yuge O. Prevention and treatment of malignant hyperthermia in certified training hospitals in Japan: a questionnaire. J Anesth. 2002;16(3):207–210. doi:10.1007/s005400200026
16. Guglielminotti J, Rosenberg H, Li G. Prevalence of malignant hyperthermia diagnosis in obstetric patients in the United States, 2003 to 2014. BMC Anesthesiol. 2020;20(1). doi:10.1186/s12871-020-0934-0
17. Lu Z, Rosenberg H, Li G. Prevalence of malignant hyperthermia diagnosis in hospital discharge records in California, Florida, New York, and Wisconsin. J Clin Anesth. 2017;39:10–14. doi:10.1016/j.jclinane.2017.03.016
18. Urman RD, Rajan N, Belani K, Gayer S, Joshi GP. Malignant hyperthermia-susceptible adult patient and ambulatory surgery center: society for ambulatory anesthesia and ambulatory surgical care committee of the American Society of Anesthesiologists Position Statement. Anesth Analg. 2019;129(2):347–349. doi:10.1213/ANE.0000000000004257
19. Neira VM, Al Madhoun W, Ghaffari K, Barrowman N, Berrigan P, Splinter W. Efficacy of malignant hyperthermia association of the United States-recommended methods of preparation for malignant hyperthermia-susceptible patients using Dräger Zeus anesthesia workstations and associated costs. Anesth Analg. 2019;129(1):74–83. doi:10.1213/ANE.0000000000003441
20. Aderibigbe T, Lang BH, Rosenberg H, Chen Q, Li G. Cost-effectiveness analysis of stocking dantrolene in ambulatory surgery centers for the treatment of malignant hyperthermia. Anesthesiology. 2014;120(6):1333–1338. doi:10.1097/ALN.0000000000000257
21. Belani KG, Cao C, Daugherty D, et al. Malignant hyperthermia status in China: a summary of an international conference. Anesth Analg. 2016;122(2):574–577. doi:10.1213/ANE.0000000000001043
22. Burkman JM, Posner KL, Domino KB. Analysis of the clinical variables associated with recrudescence after malignant hyperthermia reactions. Anesthesiology. 2007;106(5):901–906. doi:10.1097/01.anes.0000265148.86566.68
23. Joshi GP, Desai M, Valedon A, Gayer S. Succinylcholine Use and Dantrolene Availability: comment. Anesthesiology. 2019;131(4):934. doi:10.1097/ALN.0000000000002949
24. Larach MG, Klumpner TT, Brandom BW, et al. Succinylcholine use and dantrolene availability: reply. Anesthesiology. 2019;131(4):935–936. doi:10.1097/ALN.0000000000002950
25. Wang YL, Luo AL, Tan G, Cui XL, Guo XY. Clinical features and diagnosis for Chinese cases with malignant hyperthermia: a case cluster from 2005 to 2007. Chin Med J. 2010;123(10):1241–1245. doi:10.3760/cma.j.issn.0366-6999.2010.10.002
26. Kim TW, Singh S, Miller C, et al. Efficacy and cost comparison of case-based learning to simulation-based learning for teaching malignant hyperthermia concepts to anesthesiology residents. J Educ Perioper Med. 2019;21:E631.
27. Gallegos E, Hennen B. Malignant hyperthermia preparedness training: using cognitive aids and emergency checklists in the perioperative setting. J Perianesthesia Nurs. 2022;37(1):24–28. doi:10.1016/j.jopan.2020.09.020
28. Cain Cindy L, Riess Matthias L, Gettrust L, Jutta N. Malignant hyperthermia crisis: optimizing patient outcomes through simulation and interdisciplinary collaboration. AORN J. 2014;99(2):301–8; quiz309–11. doi:10.1016/j.aorn.2013.06.012
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
