Back to Journals » Risk Management and Healthcare Policy » Volume 14
The Integrated Management of Hypertension in General Hospitals and Community Hospitals
Authors Xie K , Gao X, Bao L, Shan Y, Shi H, Li Y
Received 15 February 2021
Accepted for publication 24 May 2021
Published 18 June 2021 Volume 2021:14 Pages 2537—2545
DOI https://doi.org/10.2147/RMHP.S306735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Kun Xie, Xiufang Gao, Liwen Bao, Ying Shan, Haiming Shi, Yong Li On behalf of the UPPDATE Investigators
Cardiology Department, Huashan Hospital, Fudan University, Shanghai, People’s Republic of China
Correspondence: Xiufang Gao; Yong Li
Cardiology Department, Huashan Hospital, Fudan University, No. 12 Mid Wulumuqi Road, Shanghai, 200040, People’s Republic of China
Tel +86-021-52887061
Email [email protected]; [email protected]
Purpose: We sought to investigate and improve the integrated management of hypertension in general and community hospitals in China.
Patients and Methods: We carried out a cross-sectional study in 90 centers from 15 cities in China from 2017 to 2018. Patients with primary hypertension were included.
Results: Of the total 4286 patients included, 43.2% of them controlled blood pressure (BP) below 140/90 mmHg while only 11.5% controlled BP below 130/80 mmHg. The control rate of low-density lipoprotein-C (LDL-C) in patients with concomitant coronary artery disease (CAD), diabetes (DM), and chronic kidney disease (CKD) was 24.7%, 49.4%, and 40.6%, respectively. Thirty-one percent of the DM patients had HbA1c levels greater than 8% while 21.7% of the non-DM patients had HbA1c≥ 6.5%. The control rate of body mass index (BMI) was 54.4% in men and 59.8% in women. As compared to patients from community hospitals, patients from general hospitals had poorer control of BP< 140/90 mmHg (OR 0.63, 95% CI 0.55– 0.73, p< 0.001), comparatively better attainment of LDL-C, particularly < 1.8 mmol/L in CAD (OR 3.25, 95% CI 2.02– 5.24, p< 0.001), similar control of HbA1c < 8.0% in diabetes (OR 0.64, 95% CI 0.41– 1.00, p=0.052) and comparatively worse achievement of BMI< 25 kg/m2 (OR 0.72, 95% CI 0.63– 0.83, p< 0.001).
Conclusion: The integrated management of hypertension needs to be improved. Besides LDL-C, the management of BP, blood glucose (BG), and BMI need to be strengthened in not only community hospitals but also general hospitals.
Keywords: hypertension, hypercholesterolemia, diabetes, body mass index, abdominal circumference
Introduction
Cardiovascular disease has been stated to be the majority of preventable mortality in non-communicable disease at the 65th World Health Assembly.1 To reduce cardiovascular morbidity and mortality, a lot of effort needs to be adopted including lifestyle management, risk factor management, and optimal medical treatment. Although there is common agreement on cardiovascular disease prevention,2 the risk assessment and management in individual patients remain insufficient. Integrated evaluation and guideline implementation should be encouraged to improve preventive cardiology.
Hypertension is highly prevalent and is the major cause of cardiovascular, cerebrovascular, and kidney disease. Therefore, lowering blood pressure (BP) will surely reduce the risks of major cardiovascular events. Unfortunately, BP control is unsatisfactory worldwide even if the target is 140/90 mmHg. Increasing evidence suggests that BP goes lower than 130/80 mmHg will be more beneficial and modern guidelines focusses on lower BP targets.3,4 Thus, there will be a huge gap between guideline recommendations and the current BP management.
Additionally, metabolic disorders and other risk factors are not always taken into account by patients or specialized physicians. A large proportion of patients with hypertension are overweight, have concomitant coronary artery disease (CAD), diabetes, prediabetes, dyslipidemia, and have other risk factors like smoking. The knowledge of integrated management of hypertension is still lacking. A comprehensive management mode is critically important to further reduce the cardiovascular risks both in the primary and secondary prevention of cardiovascular disease.5,6
A lot of effort has been previously made, but cardiovascular morbidity and mortality still rank high among the entire population. In the EUROASPIRE IV study of coronary patients from 78 centers in 24 European countries, 42.7% had blood pressure (BP) ≥140/90mmHg, 80.5% had low-density lipoprotein cholesterol (LDL-C) ≥1.8 mmol/l, 26.8% had self-reported diabetes and 37.6% had body mass index (BMI) ≥30 kg/m2.7 Not only in secondary prevention but also in primary prevention, there is still a lot that can be done to narrow the gap between the guidelines and the current undertreatment of hypertensive patients.
Concerning integrated management of hypertension for primary and secondary prevention, general hospitals and community hospitals should both be involved. To investigate the current management of hypertension in China and the roles that general hospitals and community hospitals play in this field, we carried out a national observational study to illustrate the integrated management in hypertension. We aimed to identify the main differences between general and community hospitals and to improve the preventive cardiology in both settings.
Patients and Methods
We carried out a cross-sectional study (UPPDATE STUDY) in 90 centers from 15 cities in China from 2017 to 2018. Patients with primary hypertension were recruited from the out-patient clinics using convenience sampling in both general hospitals and community hospitals. The inclusion criteria were patients with primary hypertension who were older than 18 years old. The exclusion criteria were patients with secondary hypertension, active tumor, or cognitive impairment. Information was collected with a detailed questionnaire for each participant. All participants provided written informed consent and approved the information to be published. Research protocols were approved by the Ethics Committee of Huashan Hospital, Fudan University (2017-282-1). The study was conducted in accordance with the Declaration of Helsinki. The patient and public were involved to provide patient-centered healthcare services.
Office BP was measured three times with one-minute interval at each visit and the average of the last two readings was recorded. The targets were defined as office BP < 140/90 mmHg or office BP < 130/80 mmHg according to the guidelines. LDL-C targets were defined according to the 2016 Chinese guideline of dyslipidemia as <1.8 mmol/L for very high risk, <2.6 mmol/L for high risk, and <3.4 mmol/L for mid and low risk. The targets of glycemic control were defined according to 2019 ADA guidelines of diabetes as <6.5% (more stringent), <7.0% (reasonable), and <8.0% (less stringent).8 CKD was defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73m2 (MDRD Equation). Overweight was defined as 25 kg/m2 ≤BMI<30 kg/m2 and obesity was defined as BMI≥ 30 kg/m2 according to the 2000 WHO standard.9 Elevated waist circumference was defined according to the 2005 AHA guideline as greater than 90 cm in males and greater than 80 cm in females (Asian).10
Student’s t-test was used for continuous variables and Chi-square test was used for categorical variables. Logistic regression was used to compare the control rate in general hospitals and community hospitals. A forward stepwise method was used in the logistic regression model. Odds ratios (OR) and 95% confidence intervals were used for the estimation. P<0.05 was considered statistically significant. Stata 13.0 was used for statistical analysis.
Results
General Characteristics
A total of 4286 participants were included (Figure 1). Among them, 56% were male. The average age was 64.81±12.71 years. 92.5% of them were on antihypertensive therapy and had an average BP of 141.65±17.35/83.45±11.88 mmHg. The average BMI was 24.88±4.04 kg/m2. The Smoking rate was 14.3% in total participants and 24.3% in males. 54.8% of participants were receiving statin therapy. 22.4% of them had diabetes and 20.6% had CAD. 22.0% of the participants had CKD and the average eGFR was 79.24±29.18 (Table 1).
 |
Table 1 General Characteristics of Patients with Hypertension |
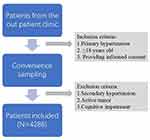 |
Figure 1 The flow charts of the inclusion/exclusion steps of the cross-sectional study. |
The Integrated Management of Hypertension
In patients with hypertension, 92.5% were on antihypertensive medication. Only 43.2% achieved BP < 140/90 mmHg and 11.5% achieved BP < 130/80 mmHg. The proportion of patients with BP<140/90 mmHg ranged from 18.2% to 47.5% according to the age groups. Patients in their 20’s had the lowest control rate of 18.2% and patients in their 60’s had the highest control rate of 47.5%. The proportion of patients with BP<130/80 mmHg ranged from 0% to 15.7% according to the age groups. The control of BP was poor particularly in young patients (Figure 2).
According to the 2016 Chinese Guideline of Dyslipidemia, patients with LDL-C lower than 1.8 mmol/L accounted for 14.2%, 1.8–2.6 mmol/L accounted for 29.3% and 2.6–3.4 mmol/L accounted for 30.1%. 26.4% of the patients did not achieve the LDL-C target of 3.4 mmol/L (≥3.4mmol/L) (Figure 1).
CAD accounted for 20.5% of the participants. But only 24.7% of patients with CAD achieved the target of LDL-C < 1.8 mmol/L. Diabetes accounted for 22.3% of the participants. 50.5% of patients with diabetes did not achieve the target of LDL-C <2.6 mmol/L. CKD accounted for 22.0% of the participants. 59.5% of patients with CKD did not achieve the target of LDL-C<2.6 mmol/L. Unfortunately, smoking rates did not decrease in hypertension with CAD, diabetes, or CKD. BMI value did not decrease either. Hypertensive patients with diabetes and CKD had increased BMI values (Table 2).
 |
Table 2 LDL-C Management in Patients with Concomitant CAD, Diabetes and CKD |
22.3% of the total patients had self-reported diabetes. BG was poorly controlled. HbA1c levels greater than 8.0% reached 31% in patients with diabetes. In patients without self-reported diabetes, 40.5% of them had FBG in the range of 5.6–7.0 mmol/L and 21.8% of them had HbA1c greater than 6.5%, which met the diagnosis of pre-diabetes and diabetes.11 (Table 3)
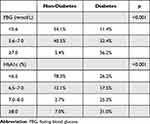 |
Table 3 BG Management in Patients with Hypertension |
The average BMI was 24.68±4.40 in females and 25.05±3.72 in males. 59.8% of the females and 54.4% of the males attained the BMI targets. The average abdominal circumference was 82.28±13.34 cm in females and 87.96±14.31 cm in males. Only 38.7% of the female and 57.9% of the males achieved the target of the abdominal circumference (Table 4).
 |
Table 4 Body Weight Management in Patients with Hypertension |
Characteristics of Patients from General and Community Hospitals
Patients of general hospitals were much younger than those of community hospitals (63.0±13.3 vs 67.0±12.3, p<0.01). Males accounted for more in general hospitals than in community hospitals (61.8% vs 53.6%, p<0.01).
The average BP in general hospitals was higher than that in community hospitals (144.6±20.5/85.6±13.6 mmHg vs 140.0±16.4/82.9±11.9 mmHg, p<0.01). Fewer patients had their BP controlled under 140/90 mmHg in general hospitals than in community hospitals (34.5% vs 46.6%, p<0.01). ABPM was not frequently used in general or community hospitals (4.2% vs 4.9%, p=0.34).
The plasma lipid levels were much more well-controlled in general hospitals than in community hospitals. In patients with CAD, more patients achieved LDL-C lower than 1.8 mmol/L in general hospitals than in community hospitals (39.7% vs 16.7%, p<0.01).
However, blood glucose was still poorly managed and the average HbA1c was higher in general hospitals than in community hospitals (8.2±2.5 vs 7.4±1.9, p<0.01).
The average BMI was also higher in general hospitals than in community hospitals (25.3±3.7 vs 24.7±4.2, p<0.01) (Table 5).
 |
Table 5 Integrated Management of Hypertension in General and Community Hospitals |
After adjusting for age, gender, anti-hypertensive therapy, statin therapy, and anti-diabetes therapy, general hospitals turned out to have worse control of BP < 140/90 mmHg (OR 0.63, 95% CI 0.55–0.73, p<0.001) and similar control of BP<130/80 mmHg (OR 0.85,95% CI 0.68–1.06, p=0.138), comparing to community hospitals (Table 6).
 |
Table 6 The Achievement of BP, LDL-C, HbA1c and BMI in General Hospitals Compared to Those in Community Hospitals |
Patients in general hospitals had better control of LDL-C <1.8 mmol/L in CAD (OR 3.25, 95% CI 2.02–5.24, p<0.001), better control of LDL-C <2.6 mmol/L in DM (OR 1.57, 95% CI 1.05–2.34, p=0.026) and better control of LDL-C < 2.6 mmol/L in CKD (OR 3.13, 95% CI 1.72–5.71, p<0.001) (Table 6).
The control of HbA1c in patients with DM was similar in general and community hospitals at the target of 6.5% (OR 0.77, 95% CI 0.47–1.25, p=0.292), the goal of<7.0% (OR 0.83, 95% CI 0.54–1.27, p=0.393) and the target of 8% (OR 0.64, 95% CI 0.41–1.00, p=0.052) (Table 6).
The control of BMI was worse in general hospitals comparing to community hospitals (OR 0.72, 95% CI 0.63–0.83, p<0.001) (Table 6).
Discussion
Our study illustrated the inadequate integrated management of BP and other risk factors in patients with hypertension. Although 92.5% of hypertension were on antihypertensive treatment, only 43.2% of them controlled BP below 140/90 mmHg and 11.5% controlled BP below 130/90 mmHg. BP control in younger patients was poorer than average. Approximately half of the patients were taking statins, but LDL-C control was around 24.7–49.4% in very high-risk and high-risk patients. In patients with self-reported diabetes, 31% had HbA1c greater than 8.0%. In patients without self-reported diabetes, 40.5% had impaired fasting glucose and 21.8% had HbA1c greater than 6.5%. BMI control was around 54.4%-59.8%. Waist circumference was particularly poorly managed in females. Smoking rate was 14.3% in total and 24.3% in males, which did not tend to decrease in patients with concomitant CAD, diabetes, and CKD.
Compared to the community hospitals, the general hospitals achieved much lower LDL-C levels in very high-risk and high-risk patients. However, the control of BP and BMI were worse in general hospitals while the control of HbA1c was similar in the two settings of hospitals.
Besides LDL-C, the management of BP, BG, and BMI should also be strengthened not only in community hospitals but also in general hospitals. The achievement in general hospitals was not superior as expected. Three possible reasons were considered. The first being that patients in general hospitals might be more seriously ill, usually having more comorbidities. The second reason being that patients were treated in a more specialized model in general hospitals rather than an interdisciplinary model in community hospitals. The last reason that was considered was that LDL-C lowering therapy had always been emphasized over other risk factors particularly in cardiologists from general hospitals.
The integrated management of BP and other risk factors has been demonstrated to be critically important to improve the prognosis of hypertensive patients. BP, BG, lipid, weight, and lifestyle management are the integrated strategies that will reduce the risk of cardiovascular disease far more than BP management alone.
The SPRINT study showed that intensive treatment of systolic blood pressure (SBP) lower than 120 mmHg could significantly reduce the primary outcome compared to the standard treatment (SBP<140mmHg) in patients with hypertension.12 The 2017 ACC guidelines have already lowered the definition of hypertension and BP target from 140/90 mmHg to 130/80 mmHg.4 The 2018 ESC guidelines have defined 130–139/85–89 mmHg as high normal and treated BP should be targeted to < 130/80 mmHg if tolerated.3 The recently published 2020 ISH guidelines also defined 130–139/85–89 mmHg as high normal, the essential target should be 140/90mmHg and the optimal target should be 130/80 mmHg in patients < 65 years.13
Similarly, the 2019 ESC guidelines for the management of dyslipidemia have lowered the target of LDL-C level from 1.8 mmol/L to 1.4 mmol/L in patients with very high risks.14 The gap between the guideline implementation and the clinical practice seems to be widening rather than narrowing.
The prevalence of diabetes has always been increasing due to population growth, aging, economic development, and lifestyle change. The worldwide prevalence of diabetes increased from 4.3–5.0% to 7.9–9.0% from 1980 to 2014.15 In China, the prevalence of diabetes increased from 9.7% in 2007 to 10.4% in 2013 and 11.2% in 2017 and the prevalence of prediabetes was 35.7% in 2013.16–18 In our study, the prevalence of diabetes was 22.3% in hypertensive patients. In the recently published 2019 ESC guidelines on diabetes, prediabetes and cardiovascular disease, the management of BG in cardiovascular disease has been highlighted which indicated the brand-new concept of preventive cardiology.19 The ISH guidelines have also recommended FBG <7 mmol/l or HbA1c <7% in hypertension.13 A lot of effort is required in the integrated management to improve the primary and secondary prevention of cardiovascular diseases.
The prevalence of obesity has also been rising in the past ten years from 5.7% to 6.3%.17 In our study, obese patients accounted for 6.4% whereas overweight patients accounted for 36.8%, which remained as a large population to be managed to achieve further fitness. The prevalence of obesity (BMI≥30 kg/m2) and central obesity (waist circumference≥80cm) was found to be higher in females.
There are several ways to improve the integrated management of hypertension. Great effort should be made to follow up with the patients to optimize the medical therapy. The guidelines should be implemented during daily clinical practice for better achievement of the targets. Patients should be screened and risk assessment should be done for better evaluation in primary and secondary prevention. The knowledge of lifestyle management should be further strengthened during patient education. On the other side, patients should be treated as a whole rather than from a single aspect. The integrated management and whole disease course management of hypertension should be adopted in not only community hospitals but also general hospitals.
The weakness of our study was the relatively small sample size. Moreover, patients were recruited using convenience sampling which could have caused bias. However, the strength of our study was that it was a multi-center cross-sectional study with 15 cities all over the country which made it possible for the results to be generalized to all patients in China. Furthermore, to our knowledge, it was the first study to compare the integrated management and guidelines implementation in general and community hospitals. More effort should be made in not only community hospitals but also general hospitals to reduce cardiovascular morbidity and mortality.
Conclusions
There was a huge gap between guideline implementation and clinical practice concerning the integrated management of hypertensive patients. A lot more effort is required in both general and community hospitals to reduce the risk of cardiovascular diseases in patients with hypertension.
Data Sharing Statement
The datasets are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The research protocols were approved by the Ethics Committee of Huashan Hospital, Fudan University (2017-282-1). All participants provided written informed consent and approved the information to be published.
Consent for Publication
Consent for publication has been provided by patients.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Shanghai Health Committee (grant number ZY (2018–2020)-ZWB-1001-CPJS16).
Disclosure
The authors declare that there is no conflict of interest.
References
1. World Health Organization. 65th World Health Assembly closes with new global health measures. Cent Eur J Public Health. 2012;20(2):163–164.
2. Authors/Task Force M, Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts): developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur J Prev Cardiol. 2016;23(11):NP1–NP96. doi:10.1177/2047487316653709
3. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104.
4. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71(6):1269–1324. doi:10.1161/HYP.0000000000000066
5. Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–835. doi:10.1177/2047487318825350
6. Xie K, Bao L, Jiang X, et al. The association of metabolic syndrome components and chronic kidney disease in patients with hypertension. Lipids Health Dis. 2019;18(1):229. doi:10.1186/s12944-019-1121-5
7. Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016;23(6):636–648. doi:10.1177/2047487315569401
8. American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S61–S70. doi:10.2337/dc19-S006
9. World Health Organization. Obesity: preventing and managing the global epidemic. report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:
10. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005;112(17):2735–2752. doi:10.1161/CIRCULATIONAHA.105.169404
11. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S13–S28. doi:10.2337/dc19-S002
12. Group SR, Wright JT
13. Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38(6):982–1004. doi:10.1097/HJH.0000000000002453
14. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2019;40(32):2700–2709. doi:10.1093/eurheartj/ehz259
15. Collaboration NCDRF. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530.
16. Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090–1101. doi:10.1056/NEJMoa0908292
17. Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi:10.1001/jama.2013.168118
18. Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi:10.1001/jama.2017.7596
19. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2019.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

