Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
The Incidence of Metabolic Syndrome and the Valid Blood Pressure Cutoff Value for Predicting Metabolic Syndrome Within the Normal Blood Pressure Range in the Population Over 40 Years Old in Guiyang, China
Authors Ma L , Li H , Zhuang H, Zhang Q, Peng N , Hu Y, Han N, Yang Y, Shi L
Received 2 March 2021
Accepted for publication 20 May 2021
Published 30 June 2021 Volume 2021:14 Pages 2973—2983
DOI https://doi.org/10.2147/DMSO.S308923
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Li Ma,1 Hong Li,1,2 Huijun Zhuang,1 Qiao Zhang,1 Nianchun Peng,1 Ying Hu,1 Na Han,1 Yuxing Yang,1 Lixin Shi1
1Department of Endocrinology and Metabolism, Affiliated Hospital of Guizhou Medical University, Guiyang, Guizhou, People’s Republic of China; 2School Hospital, Shanghai Jiao Tong University, Shanghai, People’s Republic of China
Correspondence: Hong Li
Department of Endocrinology and Metabolism, Affiliated Hospital of Guizhou Medical University, No. 28 Guiyi Road, Guiyang, Guizhou, 550001, People’s Republic of China
Tel +8618685136016
Fax +86-851-86770523
Email [email protected]
Purpose: The study was conducted to investigate metabolic syndrome (MS) incidence within the normal blood pressure (BP) range in a population over 40 years old in an urban area of Guiyang, Guizhou Province, China, and to identify a valid BP cutoff value for predicting MS.
Materials and Methods: Data from this study are based on the Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal (REACTION) study. In total, 2935 subjects in the normal BP range and without MS (795 males, 2140 females) aged 40– 80 years were included in this study. Follow-up subjects were classified by baseline BP and grouped by age. After the 3-year follow-up, the MS incidence and valid BP cutoff value for predicting MS were calculated for subjects within the normal BP range.
Results: After the 3-year follow-up study, the crude and standardized MS incidences in the cohort were 19.83% and 16.89% for follow-up subjects, respectively, with incidences of 10.94% and 10.50% for males and 23.13% and 20.66% for females. The incidence of MS in normotensive subjects (15.53%) was lower than that in subjects with high-normal BP (29.08%). After adjusting for age, sex, BMI, smoking, and drinking, the risk of having MS in the high-normal BP group was 1.823-fold [HR 1.823 95% CI (1.538– 2.162)] higher than that in the normotensive group. The ROC curve showed that the BP cutoff values were more than 117/74 mmHg in males and 112/74 mmHg in females.
Conclusion: When BP was within the normal range, the incidence of MS in participants was very high. The MS incidence was higher among high-normal BP subjects than among normotensive subjects, as was the risk of having MS. The valid BP cutoff value for predicting MS in the population was 117/74 mmHg in males and 112/74 mmHg in females. Currently, epidemiological investigations are needed to determine whether a lower BP cutoff value is needed in diagnosing MS.
Keywords: metabolic syndrome, high-normal blood pressure, normotensive, incidence, cutoff value
Introduction
Metabolic syndrome (MS) is a series of clinical features characterized by central obesity, dyslipidemia, diabetes, hypertension, and other metabolic diseases.1 MS increases the possibility of having type 2 diabetes (T2D) and cardiovascular disease.2,3 Based on the recommendation of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) [USA] in 2003, the normal blood pressure (BP) range is divided into prehypertension (120–139/80–89 mmHg) and normotension (<120/80 mmHg).4 In China, BP is also defined using actual data from the Chinese population. Although the Chinese Guidelines for the Prevention and Treatment of Hypertension have been revised many times, the BP classifications have not changed.5–7 These guidelines define BP within the normal range as <140/90 mmHg; moreover, BP within the normal range is also divided into two classifications, normotension (<120/80 mmHg) and high-normal BP (120–139/80–89 mmHg). JNC7’s prehypertension category is equivalent to The Chinese GUIDELINes for the Management of Hypertension’s high-normal BP. Hypertension can increase the possibility of having MS and cardiovascular disease. Furthermore, these adverse effects even extend to the normal range of BP.8
A study showed that the risk of cardiovascular disease started to increase from BP 115/75 mmHg and an increasing trend was also applicable for the risk of MS.9 A study by Onat et al10 showed that the MS incidence in both males and females with prehypertension was higher than that in subjects with normotension. Jung et al’s study also showed that the incidence of MS gradually increased with the increasing BP level of the subjects.11 However, few studies have compared the MS incidence of high-normal BP subjects to normotensive subjects in China. The total incidence of MS in the normal BP range in the general population has not been reported in the literature worldwide.
The cutoff value for diagnosing MS in Chinese patients is 140/90 mmHg, which was proposed by the Chinese Diabetes Society (CDS) and that for the global population is 130/85 mmHg, which was proposed by the International Diabetes Federation (IDF).12,13 The value for Asian American patients is 130/85 mmHg, which was proposed by the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III).14 Although the BP cutoff value for the diagnosis of MS in China was established by the CDS, there are no epidemiological data to support this BP cutoff value.12 At present, there are few studies on BP cutoff values for diagnosing MS. To provide a theoretical basis for the prevention and earlier treatment of MS in the clinic, Romero-Saldaña et al in Spain proposed a BP cutoff value for diagnosing MS in the general population (without excluding hypertension).15 A Taiwanese study noted the BP cutoff value for diagnosing MS when BP was less than 120/80 mmHg without antihypertensive drug use.16 However, for subjects with BP less than 140/90 mmHg, there is no relevant literature at present from China or other countries reporting a valid BP cutoff value for diagnosing MS.
In this work, a cohort follow-up study was performed on the incidence of MS in subjects within the normal BP range, and we found a valid cutoff value of BP for predicting MS, which was based on the clinical epidemiological study of residents over 40 years old in the urban area of Guiyang, Guizhou Province, China.
Materials and Methods
Study Participants
The present work was one part of the baseline survey from the REACTION study, which involved 259,657 adults over 40 years old in 25 communities in mainland China from 2011 to 2012.17–20
This study adopted a cluster sampling method. A total of 10,140 urban residents who had been living in Guiyang for more than 5 years were identified in the REACTION study, and follow up was completed from May 2011 to July 2014. We excluded 137 participants with incomplete data and 3203 participants with a history of hypertension, diabetes, hyperlipidemia, or use of related medications. We excluded 91 subjects with myocardial infarction or stroke and 1296 participants with BP ≥ 140/90 mmHg or < 90/60 mmHg. Furthermore, we excluded 1535 participants whose baseline was MS, 16 subjects who died during follow up, and 927 participants who were lost to follow up. Finally, 2935 participants remained, among whom 795 were males (age 62.51±7.71 years), and 2140 were females (age 58.69±7.28 years). Then, a cohort follow-up study with 76% follow-up rate was conducted based on data on these subjects.
According to the Chinese Guidelines for the Prevention and Treatment of Hypertension, the normal BP range is defined as <140/90 mmHg and divided into two classifications: normotension and high-normal BP.5–7 The subjects in the normal BP range were further divided into four age groups: 40–49, 50–59, 60–69, and over 70 years. This study was conducted by stratifying the subjects based on sex. The flow chart is displayed in Figure 1. Informed consent had already been given by all participants, and this study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University.
 |
Figure 1 Flow chart of the study subjects. Abbreviation: BP, blood pressure. |
Anthropometric Measurements
The health questionnaire was administered by professionally trained medical personnel and included data such as name, sex, age, medication use, smoking, drinking, medical history. Height, weight, hip circumference (HP), and waist circumference (WC) were measured with inelastic tape by professionals. WC measured the horizontal circumference of the midpoint of the line between the anterior superior iliac spine and the 12th subcostal margin at 1 cm above the umbilicus when subjects were in the standing position with their abdomen relaxed and breathing calmly. HP measured the most prominent horizontal circumference of the subject’s buttock while standing. The subjects’ WC and HP were measured twice, and the averaged value of two measurements was recorded. Body mass index (BMI) was calculated by the formula: weight/height2 (kg/m2). BP was measured by professionally trained medical personnel with a correlated OMRON mercury sphygmomanometer (Dalian OMRON Company). Before being measured, the subjects were not allowed to smoke or have coffee. Participants needed to empty their bladders and sit quietly for at least 5 minutes. When being measured, the subjects sat quietly and with exposed arms and placed their elbows at the same level as the heart. When measuring the BP, the medical personnel exhausted the air of the sphygmomanometer cuff and wrapped it around the middle of the right upper arm of the participants. The cuff was uniformly attached to the skin and wound around the upper arm of the subjects with its center located on the surface of the brachial artery with its lower edge 2.5 cm away from the elbow fossa. The width of the cuff was selected according to the upper arm circumference of the subjects, so that at least 80% of the upper arm was covered. After finding the brachial artery pulsation, the auscultation device was placed in a fluctuating position to prepare the auscultation. Then medical personnel inflated the cuff and auscultated the brachial artery pulsation until the sound disappeared. They continued to inflate the cuff to a sphygmomanometer value 30 mmHg higher than the value when sound of auscultation disappeared. They then deflated the cuff slowly. The Korotkoff 5-staging method was used here, that is, the first stage of Korotkoff is systolic blood pressure (SBP), and the fifth stage of Korotkoff is diastolic blood pressure (DBP). After the measurement, the subjects were asked to move their arms slightly, then measured a second time after 1-minute interval, then measured a third time. The mean values of SBP and DBP were obtained as mmHg.21
Biochemical Measurements
Subjects fasted after 8:00 p.m. the day before the beginning of the investigation, and all blood samples were collected at 8:00 a.m. Each subject consumed 75 g anhydrous glucose, and blood glucose was measured 2 hours later. An enzymatic method was used to measure total cholesterol (TC). The range of TC was 0.17 to 18.26 mmol/L. The coefficients of variation of intra-assay and inter-assay were <3%. The glycerol phosphate oxidase method was to measure triglycerides (TGs). The detection range of TG was 0.08 to 16.05 mmol/L. The coefficients of variation of intra-assay and interassay were <5%. A direct homogeneous enzymatic method was used to measure low-density lipoprotein cholesterol (LDL-C). The detection range of LDL-C was 0.03–20.69 mmol/L. The coefficients of variation of intra-assay and inter-assay were <4%. Accelerator selective detergent was used to measure high-density lipoprotein cholesterol (HDL-C). The coefficients of variation of intra-assay and inter-assay were <4%. Fasting plasma glucose (FPG) and 2-hour plasma glucose in the oral glucose tolerance test (OGTT2hPG) were evaluated by using the hexokinase method. The detection range of plasma glucose was 0.28–44.40 mmol/L.
MS Diagnostic Criteria
This study was included in a series of studies22–24 that were conducted based on the 2005 standard of the IDF.13 In patients meeting the central obesity standard (WC: male ≥ 90 cm, female ≥ 80 cm), any two of the following four indexes were combined: 1) TG ≥ 1.7 mmol/l or undergoing current treatment; 2) HDL-C < 1.03 mmol/l (male) or < 1.29 mmol/l (female) or undergoing current treatment; 3) blood pressure rise: SBP ≥ 130 mmHg or DBP ≥ 85 mmHg or undergoing current corresponding treatment or having a diagnosis of hypertension; and 4) FPG ≥ 5.6 mmol/l or undergoing current treatment or having a diagnosis of T2D.
Statistical Analysis
IBM SPSS 19.0 for Windows (IBM, Armonk, NY, USA) was used for data processing. The normal distribution of continuous variables was evaluated by the Kolmogorov–Smirnov test, and homogeneity of variances was evaluated by using the Levene test. The mean ± standard deviation ( ± s) was used to express continuous variables with a normal distribution of the data. The variables with abnormal distribution were log-transformed before analysis; if, after transformation, the variables still did not conform to a normal distribution, they were statistically described with median and quartile intervals M (P25 - P75). Then, in the statistical analysis, when compared within groups, the Wilcoxon test was used for two groups and the Kruskal–Wallis H-test for three or more groups. For qualitative variables, statistical descriptions were made by rate, and statistical analysis was performed by the Cochran Armitage Trend test or Chi-square test (χ2). Age and sex were standardized using data from the sixth national census of China in 2010. Cox regression was performed to assess the risk of MS after 3 years of follow up. The area under the curve (AUC) of the diagnosis of MS with different BPs was drawn and calculated by receiver operator characteristic (ROC) curves. Then, the one with the largest Jordan index was screened out as the best diagnostic cutoff value. P-values of less than 0.05 were indicative of statistical significance.
± s) was used to express continuous variables with a normal distribution of the data. The variables with abnormal distribution were log-transformed before analysis; if, after transformation, the variables still did not conform to a normal distribution, they were statistically described with median and quartile intervals M (P25 - P75). Then, in the statistical analysis, when compared within groups, the Wilcoxon test was used for two groups and the Kruskal–Wallis H-test for three or more groups. For qualitative variables, statistical descriptions were made by rate, and statistical analysis was performed by the Cochran Armitage Trend test or Chi-square test (χ2). Age and sex were standardized using data from the sixth national census of China in 2010. Cox regression was performed to assess the risk of MS after 3 years of follow up. The area under the curve (AUC) of the diagnosis of MS with different BPs was drawn and calculated by receiver operator characteristic (ROC) curves. Then, the one with the largest Jordan index was screened out as the best diagnostic cutoff value. P-values of less than 0.05 were indicative of statistical significance.
Results
Comparison Between Basic Characteristics of Subjects Within the Normal BP Range with or without MS After a 3-Year Follow Up
After a 3-year follow-up of the subjects whose BP was in the normal range, there were 582 new MS patients, an incidence of 19.83%. After sex standardization according to data from the 2010 national census in China, the incidence of MS was 16.89%. Among the new MS patients, 87 were male, and the incidence of MS was 10.94%; after age standardization, the incidence was 10.5%. A total of 495 patients were females, and the incidence of MS was 23.13%; after age standardization, the incidence was 20.66%. The incidence was obviously lower in males than in females (χ2 =54.159, P < 0.001). All indexes were statistically significant in both the MS and non-MS groups (P < 0.05). Among these subjects, age, BMI, WC, FPG, OGTT2hPG, SBP, DBP, LDL-C, TC, TG, T2D, smoking, and drinking were higher in MS group than that in non-MS group, except for HDL-C (Table 1).
 |
Table 1 Comparison of Related Indexes Between the MS and Non-MS Groups in the Follow-Up Population with Baseline Normal BP Range |
The Incidence of MS Among Subjects Within the Normal BP Range in Different Age Groups
Among the different age groups within the normal BP range, the incidence of MS in subjects age 40–49, 50–59, 60–69, and over 70 years was 13.23%, 18.58%, 22.71%, and 19.69%, respectively (χ2 = 14.188, P = 0.003). After stratification of the groups by sex, the incidence of MS in male subjects age 40–49, 50–59, 60–69, and over 70 years was 9.09%, 13.66%, 11.08%, and 7.14%, respectively (P > 0.05). Furthermore, the MS incidence in female subjects age 40–49, 50–59, 60–69, and over 70 years was 14.08%, 19.70%, 28.33%, and 31.33%, respectively (P < 0.05). There were significant differences in MS incidence between males and females in the same age groups (P < 0.05), except for the group in which subjects were age 40–49 years (P > 0.05). The MS incidence in males was lower than that in females (P <0.05). Comparison of the MS incidence among subjects of different ages showed that among females, MS incidence increased significantly with increasing age (P < 0.05), but it was not significantly different among males (P > 0.05) (Table 2).
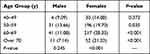 |
Table 2 Incidence of MS in Males and Females with Baseline Normal BP Range in Different Age Groups (n, %) |
The MS Incidence in Subjects with Different BP Levels Within the Normal Range
After the 3-year follow up, the MS incidence in subjects with normotension was 15.53%, and it was 29.08% in subjects with high-normal BP (χ2 =73.464, P <0.001). Among males, the incidence of MS was 8.33% with normotension and 14.05% with high-normal BP (χ2 =6.613, P =0.010). Among females, the incidence of MS was 17.5% with normotension and 38.66% with high-normal BP (χ2=105.183, P <0.001). Above all, the incidence of MS in subjects with high-normal BP was higher than that in subjects with normotension (Figure 2).
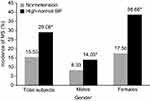 |
Figure 2 The incidence of MS in subjects with different BP levels within the normal BP range. Note: *Compared to normotension P<0.05. |
Cox Regression Analysis of BP Level of MS Incidence in Subjects in the Normal BP Range
The risk of MS in subjects with high-normal BP without adjustment was 1.873-fold [HR 1.873; 95% CI (1.591–2.204)] higher than that of subjects with normotension. After the sex, age, BMI, smoking, and drinking were adjusted, this risk was still higher than that in normotension (P <0.05), and the risk of having MS among subjects with high-normal BP was 1.823-fold higher [HR 1.823; 95% CI (1.538–2.162)] than among subjects with normotension (Table 3).
 |
Table 3 Cox Regression Analysis of Baseline BP Group Follow Up of MS Incidence in Subjects with Baseline Normal BP Range |
ROC Curves and the Valid Cutoff Value of BP for Predicting MS in Subjects in the Normal BP Range
Figure 3 shows that the AUCs of SBP and DBP were greater than 0.5 in all subjects (P < 0.05), and when SBP and DBP were greater than 113 mmHg and 74 mmHg, the corresponding sensitivities were 61.2% and 58.9%, respectively, and the specificities were 55.6% and 61.4%, respectively, indicating that MS was present. The AUCs of SBP and DBP were greater than 0.5 in males (P < 0.05), and when SBP and DBP were greater than 117 mmHg and 74 mmHg, the corresponding sensitivity was 67.8% and 73.6%, and the specificity was 50.3% and 47.7%, respectively, indicating that MS was possibly present. The AUCs of SBP and DBP were greater than 0.5 in females (P < 0.05), and when SBP and DBP were over 112 mmHg and 74 mmHg, the corresponding sensitivities were 61.6% and 56.4%, and the specificities were 60.1% and 67.3%, respectively, indicating that MS may have been present.
Discussion
In recent years, health problems in middle-aged and senior people have attracted worldwide attention. MS is one of these important public health concerns. Moreover, MS can lead to the rise of the risk of cardiovascular disease and T2D.25 There is an obvious correlation between MS and mortality in cardiovascular disease, and early prevention and treatment of MS is an effective way to prevent cardiovascular disease.26 This study was conducted to study the MS incidence in subjects in the normal BP range among residents over 40 years old in the urban area of Guiyang, Guizhou Province, China and to find valid BP cutoff values for predicting MS.
A previous study conducted by our group on subjects over 40 years old in Guiyang showed that the MS incidence was 23.57% and that the incidence after standardization was 23.23%.24 Based on that study and excluding subjects with BP ≥ 140/90 mmHg or ≤ 90/60 mmHg, this study showed that the MS incidence was 19.83% and that the incidence after standardization was 16.89% for subjects within the normal BP range. The total incidence of MS in subjects in Guiyang24 was 23.57%, which was higher than the 12.7% reported in a 5-year follow-up study (1999–2004, 25–64 years old, NCEP-ATP III14) in Beijing27 and the 9% reported in a 10-year follow-up study (2001–2010, 40–70 years old, NCEP-ATP III14) in South Korea.28 Furthermore, when considering the incidence of MS in subjects within a normal BP range in the urban area of Guiyang for comparison, the incidence was still higher in Beijing27 and South Korea.28 There might be two reasons for this disparity. First, Guiyang is located in southwestern China, its economy is underdeveloped, and people may lack an understanding of the importance of exercise. People in Guiyang like to eat pickled food and food that is high in fat and calories. A study has shown that there are insulin receptors in the liver, skeletal muscle, and adipose tissue, and exercise increases the number of insulin receptors.29 As a result, exercise could increase the number of insulin receptors so that the sensitivity of these tissues to insulin and the affinity to insulin receptors will increase and reduce insulin resistance (IR).29 In addition, physical activity prevents fat accumulation. Therefore, a lack of exercise might lead to MS. Furthermore, marinated foods contain more sodium. With an increase in sodium intake, BP levels gradually increase, resulting in abnormal BP in the general population.30 A high-calorie, high-fat diet could easily lead to obesity; moreover, it can produce more fat cells and release a number of fat-related factors. Fat-related factors can then release a number of inflammatory substances, leptin, resistin, and other substances, leading to abnormal lipid metabolism and resulting in MS.31–34 Second, MS may be related to the time of follow up, age composition, diagnostic criteria, climatic factors and so on. Therefore, for residents over 40 years of age, even if BP is within the normal range, it is still necessary to guard against the occurrence of MS.
This study stratified males and females into different age groups and found that when BP was in the normal range, the incidence of MS in females increased with age, although there was no significant difference in males. The results were consistent with a 5-year follow-up study of 762 Korean subjects with an average age of 58 years (332 males, 430 females) in South Korea.35 In addition, this study also compared the MS incidence between males and females in the same age groups, and except for the group aged 40 to 49 years, the difference in the MS incidence in the other age groups was significant, with females having a higher incidence than males. The reason might be the average menopausal age of women was approximately 50 years old.36,37 Postmenopausal women are affected by levels of estrogen, androgen, and other hormones, resulting in increased body fat, abdominal fat accumulation, and ultimately, MS.38 As a result, we should focus on the health problems of postmenopausal women in Guiyang and regularly screen for and manage MS.
According to this study, the incidence of MS in normotension and high-normal BP was 8.33% and 14.05% in males and 17.5% and 38.66% in females, respectively. A study conducted by Turkish researchers showed that the incidence of MS was 21.2% for normotensive men, 27.7% for men with high-normal BP, 16.5% for normotensive women, and 26.4% for women with high-normal BP.10 This indicates that the MS incidence in high-normal BP was higher than that in normotensive individuals among both males and females, which was consistent with the outcomes of our study. The reason is that increasing BP levels lead to a decline in islet β-cell function and IR,39 vascular endothelial dysfunction, abnormal arterial elasticity, and multiple metabolic disorders, resulting in MS.40 Thus, this study and the Turkish study10 show that there is a high risk of MS in subjects when the BP is over 120/80 mmHg. Therefore, the prevention and treatment of chronic diseases should be a public health priority. Reasonable changes to lifestyle such as in eating habits and more sports activity could be used to control BP under 120/80 mmHg in subjects aged over 40. Moreover, the public health sector should establish relevant health institutions to educate and screen for chronic diseases (including MS and T2D) in people over 40 years old with BP ≥ 120/80 mmHg. The goal is to diagnose and prevent MS earlier, lower the incidence of T2D and cardiovascular and cerebrovascular diseases, and lower the economic burden of T2D and cardiovascular disease prevention and treatment for the public health sector.
This study showed that the risk of MS in subjects with high-normal BP was higher than that in normotensive subjects after a 3-year follow-up study in residents over 40 years in Guiyang city. The results were consistent with a study in Turkey.10 In summary, after 3 years of follow up, the risk of MS in subjects was quite high. Therefore, when BP ≥ 120/80 mmHg, the risk of MS increases in residents over 40 years of age in Guiyang city, and intervention and screening measures should be carried out at this time. However, when BP was < 120/80 mmHg, BP levels were also associated with the risk of MS. Taiwanese researchers have studied normotension (< 120/80 mmHg) in older men and menopausal women and suggested that MS risk also increases with increasing BP levels.41,42 However, these studies did not indicate the specific BP values. Therefore, to study the relationship between normotension and MS, we will need to study subjects with BP < 120/80 mmHg.
The criteria commonly used to diagnose MS are those of the CDS, IDF, and NCEP-ATPIII, and the defined BP cutoff values are 140/90, 130/85, and 130/85 mmHg, respectively. Among these diagnostic criteria, those of the CDS are more suitable for Chinese people, but there are no epidemiological data. There are few studies on BP cutoff values for diagnosing MS. This study was a 3-year cohort follow-up study; therefore, when subjects were in the normal BP range, the cutoff values of BP for all subjects were 117/74 mmHg for males and 112/74 mmHg for females, which was of diagnostic significance in MS. A study of diagnostic testing in 550 Spanish workers (without excluding hypertension) proposed that there was high sensitivity and specificity for diagnosis of MS when blood pressure was 128/85 mmHg.15 A 10-year follow-up study investigated 2782 residents over 60 years of age with normotension (BP < 120/80 mmHg) who were not taking antihypertensive drugs and found that the cutoff values of BP for MS were 112/71 mmHg in males and 113/66 mmHg in females.16 The BP cutoff value of this study was lower than that of the Caucasian population in the Spanish study,15 although there were no differences between the subjects in this study and the participants in the Taiwanese study,16 because both groups were from similar Asian populations. These results were closely related to race, diagnostic criteria, characteristics of subjects, lifestyle, and so on.
This study was a cohort follow-up study of subjects with BP in the normal range, excluding a large number of risk factors that affect the occurrence of MS at baseline. When the cutoff value of BP was 117/74 mmHg for males and 112/74 mmHg for females, for which the AUCs were > 0.5, the sensitivity and specificity were high. Therefore, when BP was in the normal range, the cutoff value of BP was 117/74 mmHg for males and 112/74 mmHg for females, which might be considered a valid cutoff value for predicting MS. The BP cutoff value obtained in this study was much lower than that defined by the CDS and IDF, which are commonly used as diagnostic MS criteria in China. As a result, among these commonly used diagnostic criteria, regardless of whether the cutoff value of BP for diagnosing MS should be lowered, more regional and larger epidemiological surveys should be conducted in China.
This study had some advantages. First, the sample was large and the objective data obtained by trained professionals were based on accurate physical examination and laboratory results, so the research results were reliable. Second, this study was a 3-year follow-up cohort study, which excluded a large number of factors that affect MS, therefore its findings are reliable. However, there were also limitations to this study. First, we did not address the relevant family history, lifestyle, and education level; therefore, the possible effects of these factors could not be eliminated. Second, the sample we studied in this article was limited to the urban area of Guiyang, Guizhou Province, China, in 2011, which involved the regional and environmental factors, lifestyles, cultural levels, and other factors that might have effects on the results of this study so the results may not be highly generalizable. Therefore, the incidence of MS in subjects with a normal BP range and the valid cutoff value of BP for predicting MS need to be further explored.
Conclusions
After the 3-year cohort follow-up study, the crude and standardized MS incidences among the population over 40 years old in the Guiyang urban area who were in the normal BP range were 19.83% and 16.89%, respectively, which were 10.94% and 10.50% for males and 23.13% and 20.66% for females. The incidence in females was higher than in males. The MS incidence was higher among high-normal BP subjects than among normotensive subjects. The incidence of MS in subjects was closely related to sex and age. After the age, sex, BMI, smoking, and drinking were adjusted, the MS risk in subjects with high-normal BP was obviously higher than that in normotensive subjects. The valid BP cutoff value for predicting MS in the population was 117/74 mmHg in males and 112/74 mmHg in females. Currently, further epidemiological investigations are needed to determine whether a lower BP cutoff value is needed for diagnosing MS.
Abbreviations
AUC, area under the curve; BMI, body mass index; BP, blood pressure; CDS, Chinese Diabetes Society; CI, confidence interval; DBP, diastolic blood pressure; FPG, fasting plasma glucose; IDF, International Diabetes Federation; HC, hip circumference; HDL-C, high-density lipoprotein cholesterol; HR, hazard ratio; IR, insulin resistance; JNC 7, the Seventh report of the Joint National Committee; LDL-C, low-density lipoprotein cholesterol; MS, metabolic syndrome; NCEP-ATP III, National Cholesterol Education Program Adult Treatment Panel III; OGTT2hPG, oral glucose tolerance test 2-hour plasma glucose; REACTION, the Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal; ROC, receiver operator characteristic; SBP, systolic blood pressure; TC, total cholesterol; T2D, type 2 diabetes; TG, triglycerides; WC, waist circumference.
Data Sharing Statement
Data for the current study can be obtained from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University and was in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent had already been given by all the subjects.
Consent for Publication
This paper can be published with the consent of the study subjects.
Acknowledgments
We thank the participants for participating in the study. We appreciate the REACTION Study Group’s and the Steering Committee of the REACTION Study Group’s help in this study.
REACTION Study Group: Weiqing Wang, Yufang Bi, Jieli Lu, National Clinical Research Center for Metabolic Diseases, Rui Jin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China; Yiming Mu, Chinese People’s Liberation Army General Hospital, Beijing, China; Jiajun Zhao, Shandong Provincial Hospital affiliated with Shandong University, Jinan, China; Chao Liu, Jiangsu Province Hospital on the Integration of Chinese and Western Medicine, Nanjing, China; Lulu Chen, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China; Lixin Shi, Affiliated Hospital of Guiyang Medical College, Guiyang, China; Qiang Li, The Second Affiliated Hospital of Harbin Medical University, Harbin, China; Tao Yang, The First Affiliated Hospital of Nanjing Medical University, Jiangsu Province Hospital, Nanjing, China; Li Yan, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China; Qin Wan, The Affiliated Hospital of Luzhou Medical College, Luzhou, China; Shengli Wu, Karamay Municipal People’s Hospital, Xinjiang, China; Guixia Wang, The First Hospital of Jilin University, Changchun, China; Zuojie Luo, The First Affiliated Hospital of Guangxi Medical University, Nanning, China; Xulei Tang, The First Hospital of Lanzhou University, Lanzhou, China; Gang Chen, Fujian Provincial Hospital, Fujian Medical University, Fuzhou, China; Yanan Huo, Jiangxi People’s Hospital, Nanchang, China; Zhengnan Gao, Dalian Municipal Central Hospital, Dalian, China; Qing Su, Xinhua Hospital Affiliated with Shanghai Jiaotong University School of Medicine, Shanghai, China; Zhen Ye, Zhejiang Provincial Center for Disease Control and Prevention, China; Youmin Wang, The First Affiliated Hospital of Anhui Medical University, Hefei, China; Guijun Qin, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China; Huacong Deng, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China; Xuefeng Yu, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China; Feixia Shen, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China; and Li Chen, Qilu Hospital of Shandong University, Jinan, China.
Steering Committee of the REACTION Study Group: Guang Ning (Principal Investigator), National Clinical Research Center for Metabolic Diseases, Rui Jin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. Yiming Mu, Chinese People’s Liberation Army General Hospital, Beijing, China. Jiajun Zhao, Shandong Provincial Hospital affiliated with Shandong University, Jinan, China. Weiqing Wang, National Clinical Research Center for Metabolic Diseases, Rui Jin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. Chao Liu, Jiangsu Province Hospital on the Integration of Chinese and Western Medicine, Nanjing, China. Yufang Bi, National Clinical Research Center for Metabolic Diseases, Rui Jin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. Donghui Li, Department of Gastrointestinal Medical Oncology, the University of Texas MD Anderson Cancer Center, Houston, Texas, USA. Shenghan Lai, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA. Zachary T. Bloomgarden, Mount Sinai School of Medicine, New York, USA.
Author Contributions
All authors made a significant contribution to study conception, study design, questionnaire, data analysis, drafting the paper, revising the paper and all other aspects. The manuscript was reviewed and the final draft for publication was approved by all authors, who agree to be accountable for all aspects of the work. The authors declare that there is no conflict of interest.
Funding
This work was supported by grants from the National Key R&D Program of China (2017YFC1310700), the National Clinical Research Center for Metabolic Diseases (2013BAI09B13), the National Key New Drug Creation and Manufacturing Program of Ministry of Science and Technology (2012ZX09303006-001), and the Special Scientific Research Fund of Public Welfare Profession from the National Health and Family Planning Commission of the PRC (201502007).
Disclosure
The authors report that there is no conflict of interest in this work.
References
1. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415–1428. doi:10.1016/S0140-6736(05)66378-7
2. Lee MK, Han K, Kim MK, et al. Changes in metabolic syndrome and its components and the risk of type 2 diabetes: a nationwide cohort study. Sci Rep. 2020;10(1):2313. doi:10.1038/s41598-020-59203-z
3. Watanabe J, Kotani K. Metabolic syndrome for cardiovascular disease morbidity and mortality among general Japanese people: a mini review. Vasc Health Risk Manag. 2020;16:149–155. doi:10.2147/VHRM.S245829
4. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2571. doi:10.1001/jama.289.19.2560
5. Writing Group of 2004 Chinese Guidelines for the Management of Hypertension. 2004 Chinese guidelines for the management of hypertension (practical edition). Chin J Cardiol. 2004;32(12):1060–1064.
6. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Chin J Cardiol. 2010;39(7):579–617.
7. Writing Group of 2018 Chinese Guidelines for the Management of Hypertension. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2018;24(1):24–56.
8. Franklin SS, Barboza MG, Pio JR, Wong ND. Blood pressure categories, hypertensive subtypes, and the metabolic syndrome. J Hypertens. 2006;24(10):2009–2016. doi:10.1097/01.hjh.0000244950.72664.02
9. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913.
10. Onat A, Yazici M, Can G, Kaya Z, Bulur S, Hergenc G. Predictive value of prehypertension for metabolic syndrome, diabetes, and coronary heart disease among Turks. Am J Hypertens. 2008;21(8):890–895. doi:10.1038/ajh.2008.212
11. Jung JY, Oh CM, Choi JM, et al. Levels of systolic and diastolic blood pressure and their relation to incident metabolic syndrome. Cardiology. 2019;142(4):224–231. doi:10.1159/000499867
12. Chinese Diabetes Society Metabolic Syndrome Research Collaboration Group. Chinese Diabetes Society recommendations on metabolic syndrome. Chin J Diabetes. 2004;12(3):156.
13. Alberti KGMM, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi:10.1016/S0140-6736(05)67402-8
14. National Cholesterol Education Program (NCEP) Expert Panel on Detection E, III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143. doi:10.1161/circ.106.25.3143
15. Romero-Saldaña M, Fuentes-Jiménez FJ, Vaquero-Abellán M, Álvarez-fernández C, Molina-Recio G, López-Miranda J. New non-invasive method for early detection of metabolic syndrome in the working population. Eur J Cardiovasc Nurs. 2016;15(7):549–558. doi:10.1177/1474515115626622
16. Hsu CH, Chang JB, Liu IC, et al. Mean arterial pressure is better at predicting future metabolic syndrome in the normotensive elderly: a prospective cohort study in Taiwan. Prev Med. 2015;72:76–82. doi:10.1016/j.ypmed.2014.12.036
17. Ning G, Reaction Study Group. Risk evaluation of cancers in Chinese diabetic individuals: a longitudinal (REACTION) study. J Diabetes. 2012;4(2):172–173. doi:10.1111/j.1753-0407.2012.00182.x
18. Bi Y, Lu J, Wang W, et al. Cohort profile: risk evaluation of cancers in Chinese diabetic individuals: a longitudinal (REACTION) study. J Diabetes. 2014;6(2):147–157. doi:10.1111/1753-0407.12108
19. Lu J, Bi Y, Wang T, et al. The relationship between insulin-sensitive obesity and cardiovascular diseases in a Chinese population. Int J Cardiol. 2014;172(2):388–394. doi:10.1016/j.ijcard.2014.01.073
20. Ning G, Bloomgarden Z. Diabetes and cancer: findings from the REACTION study. J Diabetes. 2015;7(2):143–144. doi:10.1111/1753-0407.12240
21. Wang W, Zhang WZ, Sun NL, et al. Guidelines to blood pressure measurement in China. Chin J Hypertens. 2011;19(12):1101–1115.
22. Li H, Shi LX, Zhang Q, et al. Prevalence of metabolic syndrome in Chinese population aged over 40 in Guiyang. Chin J Endocrinol Metab. 2013;29(5):410–413.
23. Yuan X, Li H, Shi LX, et al. Relationship between weight change and incidence of metabolic syndrome in Guiyang urban residents aged 40 or over: a 3-year follow-up study. Chin Gen Pract. 2017;20(17):2106–2110.
24. Wang XY, Li H, Shi LX, Zhang Q, Peng N, Hu Y. Relationship between sleep duration, TV watching time and the incidence of metabolic syndrome in adults aged 40 or older in Guiyang city: a prospective cohort study. Chin J Endocrinol Metab. 2016;32(6):488–493.
25. Zafar U, Khaliq S, Ahmad HU, Manzoor S, Lone KP. Metabolic syndrome: an update on diagnostic criteria, pathogenesis, and genetic links. Hormones. 2018;17(3):299–313. doi:10.1007/s42000-018-0051-3
26. van Herpt TTW, Dehghan A, van Hoek M, et al. The clinical value of metabolic syndrome and risks of cardiometabolic events and mortality in the elderly: the Rotterdam study. Cardiovasc Diabetol. 2016;15:69. doi:10.1186/s12933-016-0387-4
27. Liu J, Zhao D, Wang W, Liu J, Sun J, Wu Z. Incidence of the metabolic syndrome and its risk factors. J Cardiovasc Pulm Dis. 2007;26(2):65–68.
28. Huh JH, Ahn SG, Kim YI, et al. Impact of longitudinal changes in metabolic syndrome status over 2 years on 10-year incident diabetes mellitus. Diabetes Metab J. 2019;43(4):530–538. doi:10.4093/dmj.2018.0111
29. Perry RJ, Samuel VT, Petersen KF, Shulman GI. The role of hepatic lipids in hepatic insulin resistance and type 2 diabetes. Nature. 2014;510(7503):84–91. doi:10.1038/nature13478
30. Nomura K, Hiyama TY, Sakuta H, et al. [Na+] increases in body fluids sensed by central NAX induce sympathetically mediated blood pressure elevations via h+-dependent activation of ASIC1a. Neuron. 2019;101(1):60–75.e6. doi:10.1016/j.neuron.2018.11.017
31. Rosen ED, Spiegelman BM. Adipocytes as regulators of energy balance and glucose homeostasis. Nature. 2006;444(7121):847–853. doi:10.1038/nature05483
32. Choi JR, Kim JY, Huh JH, Kim SH, Koh SB. Contribution of obesity as an effect regulator to an association between serum leptin and incident metabolic syndrome. Clin Chim Acta. 2018;487:275–280. doi:10.1016/j.cca.2018.09.038
33. Pan F, Cui J, Zhou C. Correlation study of serum adiponectin, resistin and liver fibrosis in patients with nonalcoholic fatty liver disease. Shaanxi Med J. 2008;11:1500–1503.
34. Shen ZH, Lu Y, Li F, Wang L, Yu YW, Feng YB. Association between diet style and metabolic syndrome in old people. Chin J Geriatr. 2011;30(3):245–247.
35. Hwang JH, Kam S, Shin JY, et al. Incidence of metabolic syndrome and relative importance of five components as a predictor of metabolic syndrome: 5-year follow-up study in Korea. J Korean Med Sci. 2013;28(12):1768–1773. doi:10.3346/jkms.2013.28.12.1768
36. Shen TY, Chen HJ, Pan WH, et al. Secular trends and associated factors of age at natural menopause in Taiwanese women. Menopause. 2019;26(5):499–505. doi:10.1097/GME.0000000000001307. PMID: 30672884.
37. Zhu D, Chung HF, Pandeya N, et al. Body mass index and age at natural menopause: an international pooled analysis of 11 prospective studies. Eur J Epidemiol. 2018;33(8):699–710. doi:10.1007/s10654-018-0367-y
38. Zhao L, Fan X, Zuo L, et al. Estrogen receptor 1 gene polymorphisms are associated with metabolic syndrome in postmenopausal women in China. BMC Endocr Disord. 2018;18(1):65. doi:10.1186/s12902-018-0289-4
39. Xu LL, Xiang HD, Zhang LH. Changes of insulin resistance and islet β-cell function in subjects with high normal blood pressure. Acta Acad Med Sin. 2009;31(4):494–497.
40. Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–1297. doi:10.1056/NEJMoa003417
41. Er LK, Chen YL, Pei D, Lau SC, Kuo SW, Hsu CH. Increased incidence of metabolic syndrome in older men with high normotension. Aging Male. 2012;15(4):227–232. doi:10.3109/13685538.2012.720742
42. Hsu CH, Lin JD, Wu CZ, et al. High normotension is associated with higher metabolic syndrome risk in postmenopausal women. Geriatr Gerontol Int. 2014;14(2):293–300. doi:10.1111/ggi.12097
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

