Back to Journals » International Journal of General Medicine » Volume 14
The Impact on Blood Pressure of a Short-Term Change in Indoor Temperature
Authors Chen X, Tu P, Sun XL , Hu TY, Wan J, Hu YW, Zhou HL, Su H
Received 10 November 2020
Accepted for publication 23 March 2021
Published 22 April 2021 Volume 2021:14 Pages 1507—1511
DOI https://doi.org/10.2147/IJGM.S291431
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Xi Chen,1,* Ping Tu,2,* Xing-Lan Sun,1 Ting-Ying Hu,1 Jia Wan,1 Yi-Wei Hu,1 Hui-Ling Zhou,1 Hai Su1
1Department of Cardiovascular Medicine, The Second Affiliated Hospital of Nanchang University, Nanchang, 330006, People’s Republic of China; 2Department of Post Anesthesia Care Unit, The Second Affiliated Hospital of Nanchang University, Nanchang, 330006, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xing-Lan Sun
Department of Cardiovascular Medicine, The Second Affiliated Hospital of Nanchang University, No. 1 of Minde Road, Donghu District, Nanchang, 330006, People’s Republic of China
Tel +86 791-86312182
Fax +86 791-86312182
Email [email protected]
Objective: The aim of this study is to evaluate the impact on blood pressure (BP) of a 10°C change in room temperature (between 18°C and 28°C).
Methods: A total of 112 volunteers, 56 males and 56 females, 55 with and 57 without hypertension, were enrolled in the study. First, the participants were placed in a 25°C room. Second, they were randomly assigned to either a 28°C (group A) or an 18°C room (group B). Finally, they were moved from the 28°C to the 18°C room, or vice versa. They stayed in each room for 20 minutes. Seated BP was measured at the 17th and 19th minute in each room, and the average was used. The difference in the subject’s BP between the second two rooms was recorded as delta BP.
Results: The baseline systolic BP (SBP), age, gender distribution, and incidence of hypertension were similar between the two groups. In group A, the decrease in room temperature of 10°C induced a mean rise in SBP of 4.1 mmHg. In group B, the increase of 10°C caused SBP to decrease by 4.0 mmHg. When compared with the group without hypertension, the group with hypertension had a significantly higher rise in mean SBP (6.8 vs 1.2 mmHg) as a result of the decrease in temperature and a significantly higher drop in SBP (7.3 vs 1.2 mmHg) as a result of the increase in temperature. The participants in the group with hypertension were older.
Conclusion: A 10°C change in room temperature, from 18°C to 28°C, for 20 min can cause a significant change in SBP. The extent of this change is more obvious in the older group.
Keywords: room, temperature, BP, hypertension, change
Introduction
Blood pressure (BP) is generally higher in cold seasons than in warm seasons. Increased mortality from cardiovascular disease in winter is partly explained by the increased BP induced by exposure to the cold.
Generally, changes in outdoor temperatures have been considered as the reason for seasonal BP changes.1–4 A study showed that outdoor temperature was inversely associated with BP in 438,811 Chinese adults.2 In addition, a meta-analysis indicated that a 1°C decrease in mean daily outdoor temperature was associated with an increase in systolic BP (SBP) of 0.26 mmHg and diastolic BP (DBP) of 0.13 mmHg.4 Otsuki et al found that SBP during outdoor exercise was associated with the air temperature.5
Recently, the impact of indoor temperature on BP has attracted more attention.4,6,7 A study suggested that a change in indoor temperature has a more obvious impact on BP than a change in outdoor temperature. For example, the above-mentioned meta-analysis indicated that a 1°C decrease was associated with an increase of 0.38 mmHg in SBP.4 However, based on the data from 4659 community-dwelling adults, Zhao et al found that a 1°C decrease in indoor temperature was associated with a 0.48 mmHg increase in SBP and a 0.45 mmHg increase in DBP, after controlling for confounding variables.7
Some scholars consider that the relationship between BP and indoor temperature is not completely linear. When the indoor temperature is below 18°C, a decrease in indoor temperature may induce a more obvious increase in BP when compared with changes above 18°C. Therefore, an indoor temperature above 18°C is recommended for the prevention of high BP in humans.8
A change in room temperature in the range of 18°C–28°C is common at home or in hospital. Currently, the impact of this change on BP is unclear. If it were discovered that this change in room temperature could cause variation in BP, this information would be useful for the diagnosis of and research into hypertension. This study mainly evaluated the impact of a 10°C change in room temperature for 20 minutes on the BP of a group of volunteers.
Methods
Subjects
A total of 112 volunteers, 56 males and 56 females, were enrolled in this study (age: 18–80 years old). According to their disease history, 55 had hypertension and 57 did not. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Second Affiliated Hospital of Nanchang University, and all participants gave informed consent. Hypertensives patients took Annezen (Amlozepin Benzylate Tablets 5 mg-10 mg/day), Annexide (Losartan Potassium 50 mg/Hydrochlorothiazide Tablets 12.5 mg, 1 tablet/day).
Study Design
The participants were asked to abstain from caffeine and alcohol and to avoid intense physical activity. In this study, three rooms were maintained using central air conditioning at 25°C, 28°C, and 18°C, respectively. Room humidity was 50–60%. The experiment was carried out in winter and spring from 08:00 to 12:00 and 14:00 to 17:30.
First, all the participants were placed in the 25°C room. Second, they were randomly assigned to the 28°C (group A) or the 18°C (group B) room. Finally, the participants in group A moved to the 18°C room, ie, from 25°C to 28°C to 18°C, and those in group B moved to the 28°C room, ie, from 25°C to 18°C to 28°C. This means that in the last stage, group A experienced a decrease in room temperature of 10°C, while group B experienced an increase of 10°C. The participants stayed in each room for 20 minutes, and they could put on or remove items of clothing according to how they were feeling (Figure 1).
 |
Figure 1 The scheme of the study proposal. |
BP Measurement
Blood pressure testers: research nurses;
Participants: The blood pressure was measured in a sitting position to protect and relax. The thickness of the jacket was no more than 0.5 cm. The lower edge of the cuff was 2~3 cm above the elbow socket, and it was considered to be moderately tight if two fingers could fit into it.
Cuff: the cuff for ordinary people to use the electronic blood pressure monitor is 22–32 cm, and the cuff for obese people to use the electronic blood pressure monitor is 32–45 cm.
First, a cuff was carefully placed on the right arm of the participant. In this study, seated BP was measured using an electronic (oscillometric) BP device (Omron HEM-7201) in each room at the 17th and 19th minute. The average of these two measurements was recorded as the final value for each participant. The BP was measured with the same BP device for each participant.
The BP measured in the 25°C room was recorded as the baseline BP (BP-25). The BPs measured in the 28°C and 18°C rooms were recorded as BP-28 and BP-18, respectively. The difference in BP between the 28°C and 18°C rooms was recorded as delta BP, and the difference in temperature was recorded as delta T. The BP change rate was calculated using the following formula: Delta BP ÷ Delta T (mmHg/°C).
Statistical Analysis
All data were presented as mean ± standard deviation, and the SPSS 21.0 statistical package was used for the analysis. A t-test was performed for the comparison of continuous variables, and a paired t-test was performed for the comparison of paired data. Categorical variables presented as a percentage were analyzed using the Pearson Chi-square test. P < 0.05 was considered statistically significant.
Results
The baseline BP, age, distribution of gender, and incidence of hypertension were similar between the two groups (Table 1).
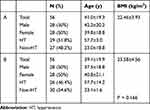 |
Table 1 The Age and Gender of the A and B Groups |
When the participants in group A moved from the 28°C to the 18°C room (10°C decrease), their mean SBP increased by 4.1 mmHg, a rate of increase of 0.41 mmHg/°C, and their mean DBP increased by 3.6 mmHg, a rate of increase of 0.36 mmHg/°C. When the participants in group B moved from the 25°C to the 18°C room (7°C decrease), their mean SBP increased by 2.7 mmHg, a rate of increase of 0.39 mmHg/°C, and their mean DBP increased by 3 mmHg, a rate of increase of 0.43 mmHg/°C.
When the participants in group B moved from the 18°C to the 28°C room, their mean SBP decreased by 4.0 mmHg, a rate of decline of 0.40 mmHg/°C, and their mean DBP decreased by 1.3 mmHg, a rate of decline of 0.13 mmHg/°C. When group A moved from the 25°C to the 28°C room (3°C increase), their mean SBP decreased by 0.8 mmHg, a rate of decline of 0.26 mmHg/°C, and their mean DBP decreased by 0.6 mmHg, a rate of decline of 0.20 mm Hg/°C (no statistical significance) (Table 2).
 |
Table 2 The BP Change Between the A and B Groups in the Rooms with Different Temperatures |
The participants in the group with hypertension, who were significantly older, had higher BP-25 levels than those in the group without hypertension, but the gender distribution was similar between the two groups (Table 3).
 |
Table 3 The Age and BP Levels of the Groups with and without Hypertension |
Figure 2 compares the change in SBP and DBP between the group with and the group without hypertension when the room temperature changed by 10°C. The group with hypertension had a significantly higher increase in mean SBP (6.8 mmHg vs 1.2 mmHg, p = 0.014) when the room temperature decreased by 10°C and a significantly higher decrease in SBP (7.3 mmHg vs 1.2 mmHg, p = 0.021) when the room temperature increased by 10°C. However, for DBP the values were 4.8 mmHg vs 2.4 mmHg (p = 0.206) and 2.7 mmHg vs 0.03 mmHg (p = 0.208), respectively, but there is no statistical significance (Figure 2).
Discussion
A previous study found that when the room temperature was above 18°C, the temperature change had a relatively weak impact on BP.8 Therefore, this study set the lowest room temperature at 18°C.
Our results demonstrated that an increase or decrease in temperature of 10°C, between 18°C and 28°C, may induce a significant decrease or increase in both SBP and DBP. When the room temperature decreased by 10 °C, the rate of increase was 0.41 mmHg/°C for SBP and 0.36 mmHg/°C for DBP. Interestingly, a decrease in room temperature of 7°C induced a similar rate of increase of 0.39 mmHg/°C for SBP and 0.43 mmHg/°C for DBP. Previously, a study4 indicated that a 1°C decrease in indoor temperature was associated with a 0.38 mmHg increase in SBP. In addition, Zhao et al found that a 1°C decrease in indoor temperature was associated with a rise of 0.48 mmHg in SBP and 0.45 mmHg in DBP.7 These values indicate that a 1°C decrease in indoor temperature is associated with an increase of 0.4–0.5 mmHg in SBP and of 0.35–0.45 mmHg in DBP.
Our results demonstrated that an increase in room temperature of 10°C could decrease SBP, with a rate of 0.40 mmHg/°C, and that the absolute value of this decrease is very close to that of the rate of increase induced by a 10°C decrease in room temperature. However, this change in room temperature did not induce a significant decrease in DBP (a rate of decline of only 0.13 mmHg/°C). These results indicated that the DBP response to the change in temperature may be different to the SBP response. Although the exact mechanism is unclear, a possible reason is that cold exposure could rapidly increase the sympathetic activity, while warm exposure could not rapidly decrease the sympathetic activity.2,9–14
In addition, we found that an increase in room temperature of 3°C did not induce a significant decrease in SBP or DBP. However, a previous study found that a rise in room temperature of 2.09°C could significantly decrease SBP and DBP by 4.43 mmHg and 2.33 mmHg, respectively.6 This difference may be due to the short length of time (20 min) that the participants spent in each room in our study.
Our study also found that the group with hypertension, who were older, had a larger change in BP when the room temperature changed by 10°C than the younger group without hypertension. As both the age and the baseline BP levels in the group with hypertension were higher, these two factors may also be related to the excessive change in BP.15,16 Based on our results, more attention should be paid to older patients and patients with hypertension when the room temperature changes, especially when the room temperature decreases.
Clinical Implications
Our study showed that even though the participants could freely put on or remove items of clothing, a 10°C change in room temperature for only 20 min can induce a change in SBP of about 4 mmHg. However, this change was about 7 mmHg in the older group with hypertension. Therefore, this finding should be considered in clinical diagnosis and management of hypertension and in hypertension research, especially for the elderly and those with hypertension.
Limitations
Potential limitations may have affected this study. First, this study involved only a small population. Therefore, the findings must be treated with caution. Second, the participants with hypertension in this study were older than those without hypertension. Therefore, we could not fully explain the impact of hypertension on the change in BP induced by changes in room temperature. Third, the impact of anti-hypertensive treatment on the relationship between BP and room temperature was not analyzed in depth, since the sample was small. Also, The sample is restricted and of young age. The main limitation is the selection of participants (no report), the restricted sample size, and the fact that we did not use a cross-over design for all participants which would increase study power.
Conclusions
A change in room temperature of 10°C, between 18°C and 28°C, for 20 min induced a mean change of 4 mmHg in the SBP of 112 volunteers. However, the change was about 7 mmHg in the older group with hypertension.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Giaconi S, Ghione S, Palombo C, et al. Seasonal influences on blood pressure in high normal to mild hypertensive range. Hypertension. 1989;14(1):22–27. doi:10.1161/01.hyp.14.1.22
2. Wang S, Li M, Hua Z, et al. Outdoor temperature and temperature maintenance associated with blood pressure in 438,811 Chinese adults. Blood Press. 2017;26(4):246–254. doi:10.1080/08037051.2017.1297676
3. Yatabe J, Yatabe MS, Morimoto S, Watanabe T, Ichihara A. Effects of room temperature on home blood pressure variations: findings from a long-term observational study in Aizumisato Town. Hypertens Res. 2017;40(8):785–787. doi:10.1038/hr.2017.18
4. Wang Q, Li C, Guo Y, et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–286. doi:10.1016/j.scitotenv.2016.10.019
5. Otsuki T, Ishii N. Association between blood pressure changes during self-paced outdoor walking and air temperature. Clin Physiol Funct Imaging. 2017;37(2):155–161. doi:10.1111/cpf.12280
6. Saeki K, Obayashi K, Kurumatani N. Short-term effects of instruction in home heating on indoor temperature and blood pressure in elderly people: a randomized controlled trial. J Hypertens. 2015;33(11):2338–2343. doi:10.1097/HJH.0000000000000729
7. Zhao H, Jivraj S, Moody A. ‘My blood pressure is low today, do you have the heating on?’ The association between indoor temperature and blood pressure. J Hypertens. 2019;37(3):504–512. doi:10.1097/HJH.0000000000001924
8. Shiue I, Shiue M. Indoor temperature below 18°C accounts for 9% population attributable risk for high blood pressure in Scotland. Int J Cardiol. 2014;171(1):e1–e2. doi:10.1016/j.ijcard.2013.11.040
9. Xu D, Zhang Y, Wang B, et al. Acute effects of temperature exposure on blood pressure: an hourly level panel study. Environ Int. 2019;124:493–500. doi:10.1016/j.envint.2019.01.045
10. Brook RD, Weder AB, Rajagopalan S. “Environmental hypertensionology” the effects of environmental factors on blood pressure in clinical practice and research. J Clin Hypertens (Greenwich). 2011;13(11):836–842. doi:10.1111/j.1751-7176.2011.00543.x
11. Cui J, Muller MD, Blaha C, Kunselman AR, Sinoway LI. Seasonal variation in muscle sympathetic nerve activity. Physiol Rep. 2015;3(8):e12492. doi:10.14814/phy2.12492
12. Ushigome E, Kitagawa N, Kitae A, et al. Seasonal variation in home blood pressure and its relationship with room temperature in patients with type 2 diabetes. Diab Vasc Dis Res. 2020;17(1):1479164119883986. doi:10.1177/1479164119883986
13. Huang CC, Chen YH, Hung CS, et al. Assessment of the relationship between ambient temperature and home blood pressure in patients from a web-based synchronous telehealth care program: retrospective Study. J Med Internet Res. 2019;21(3):e12369. doi:10.2196/12369
14. Umishio W, Ikaga T, Kario K, et al.; SWH Survey Group. Cross-sectional analysis of the relationship between home blood pressure and indoor temperature in winter: a nationwide smart wellness housing survey in Japan. Hypertension. 2019;74(4):756–766. doi:10.1161/HYPERTENSIONAHA.119.12914
15. Stergiou GS, Palatini P, Modesti PA, et al. Seasonal variation in blood pressure: evidence, consensus and recommendations for clinical practice. Consensus statement by the European society of hypertension working group on blood pressure monitoring and cardiovascular variability. J Hypertens. 2020;38(7):1235–1243. doi:10.1097/HJH.0000000000002341
16. Kollias A, Kyriakoulis KG, Stambolliu E, Ntineri A, Anagnostopoulos I, Stergiou GS. Seasonal blood pressure variation assessed by different measurement methods: systematic review and meta-analysis. J Hypertens. 2020;38(5):791–798. doi:10.1097/HJH.0000000000002355
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

