Back to Journals » Journal of Inflammation Research » Volume 14
The Impact of the Duration of Cardiac Troponin I Elevation on the Clinical Prognosis as Well as Incidence of New-Onset Atrial Fibrillation Respectively in Elderly Non-ST-Elevation Acute Myocardial Infarction Patients without PCI
Authors Wang Y, Wang XD, Yao JW, Shi BB, Gu QX, Zhang J, Cui XT, Wang Y
Received 21 October 2021
Accepted for publication 25 November 2021
Published 15 December 2021 Volume 2021:14 Pages 6907—6916
DOI https://doi.org/10.2147/JIR.S345576
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Yu Wang,1 Xue-Dong Wang,1 Ji-Wen Yao,1 Bei-Bei Shi,1 Qing-Xiang Gu,2 Jing Zhang,1 Xiao-Ting Cui,1 Yan Wang1
1Department of Cardiology, Beijing Hepingli Hospital, Beijing, 100013, People’s Republic of China; 2Department of Rheumatology, The First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, 300193, People’s Republic of China
Correspondence: Xue-Dong Wang
Department of Cardiology, Beijing Hepingli Hospital, No. 18 of Hepingli North Street, Dongcheng District, Beijing, 100013, People’s Republic of China
Tel +86 10 5804 3212
Fax +86 10 6429 5714
Email [email protected]
Objective: This study aimed to investigate the impact of the duration of cardiac troponin I (TnI) elevation on the prognosis and incidence of new-onset atrial fibrillation (NOAF) in elderly patients with non-ST-elevation acute myocardial infarction (NSTE-AMI).
Methods: A total of 383 NSTE-AMI patients ≥ 75 years old were enrolled in this study and divided into two groups: in 194 cases, the duration of TnI elevation was ≥ 14 days (group 1), and in 189 cases, the duration of TnI elevation was < 14 days (group 2). The patients were followed up for 60 months. The effect of TnI on prognosis was studied by cohort. The primary endpoint was a composite endpoint of cardiovascular death, reinfarction, ischemic stroke, and hospitalization for heart failure, and the secondary endpoint was all-cause death. A case–control study design was adopted to analyze the influencing factors of NOAF occurrence in Group 1 and Group 2.
Results: The median duration of follow-up was 26 months. Multivariate Cox’s regression analysis revealed that the duration of TnI elevation ≥ 14 days and diuretic use were independent variables of the major composite endpoint (p < 0.01 for both), and the left ventricular ejection fraction and the duration of TnI elevation ≥ 14 days were independent related variables of all-cause death (p < 0.05). The duration of TnI elevation ≥ 14 days was correlated with the occurrence of NOAF, but, in the multivariate logistic regression model, only uric acid and high-sensitivity C-reactive protein were independently associated with NOAF (p < 0.05).
Conclusion: The duration of TnI elevation ≥ 14 days was the independent correlation factor of the major composite endpoint and all-cause death; high sensitivity C-reactive protein and uric acid are independent risk factors for NOAF.
Keywords: duration of TnI elevation, the elderly, non-ST-segment acute elevation acute myocardial infarction, prognosis, new-onset atrial fibrillation
Introduction
Elderly patients with non-ST-segment elevation acute myocardial infarction (NSTE-AMI) aged ≥75 years often fail to receive percutaneous coronary intervention (PCI) or coronary artery bypass grafting due to weakness and multiple complications, and they only receive the standardized drug treatment recommended by the guidelines. In clinical practice, it has been observed that troponin I (TnI), a marker of myocardial necrosis, decreases slowly in a considerable proportion of such patients, and it takes a long time to return to normal levels. For such elderly patients with NSTE-AMI but without revascularization, in whom TnI level is delayed in returning to normal (≥14 days), the prognosis has not been reported yet.
There have been many studies on the relationship between myocardial ischemia and new atrial fibrillation, and the reported incidence of NOAF in acute myocardial infarction (AMI) ranged from 6% to 21%.1,2 However, similar studies have not been conducted on the occurrence and influencing factors of atrial fibrillation in elderly patients (≥75 years) without emergency PCI whose TnI delay is reduced to normal. Patients with AMI are prone to atrial fibrillation, its occurrence being related to many factors, such as neuroendocrine activation, left atrial pressure rise caused by decreased left ventricular contractility, and increased inflammatory response and oxidative stress.3,4 Moreover, once patients with AMI are combined with NOAF, it often means a worse prognosis, which deserves high attention and strengthened management.2,5,6 The latest literature reported that the incidence of NOAF in AMI patients undergoing emergency PCI was 7.9%,7,8 but, in elderly patients aged 75 years or older with NSTE-AMI without PCI, it remains unclear how the incidence of NOAF and whether the continuous increase in TnI increases the incidence of atrial fibrillation.
Therefore, the present study, involving NSTE-AMI patients ≥75 years old without PCI, use a retrospective cohort study and a retrospective case control design, respectively, to observe the impact of the duration of TnI elevation (≥14 days) on the prognosis and incidence of NOAF.
Materials and Methods
Research Design
The study was divided into two parts. The first part was a retrospective cohort study and the second part was a retrospective case-control study. The research protocol was approved by the ethics review committee of Beijing Hepingli Hospital (No: BJSHPLYY-IRB-KYXM-2021-05). The experiment was carried out in accordance with the principles of the Declaration of Helsinki.
Subjects
The study population was elderly patients with NSTE-AMI hospitalized in the Department of Cardiology, Hepingli Hospital of Beijing between January 1, 2016 and December 31, 2019. The inclusion criteria were as follows: (1) age ≥75 years old; (2) elevated TnI; (3) the diagnosis of AMI met the standard of the Fourth Universal Definition of Myocardial Infarction;9 (4) the electrocardiogram (ECG) presented with no ST segment elevation; and (5) the drug therapy was as recommended by the guidelines. The exclusion criteria were as follows: (1) death within 14 days; (2) PCI given; (3) severe anemia; (4) acute attack of chronic obstructive pulmonary disease; (5) stage 5 chronic renal insufficiency; (6) acute infection; (7) severe heart failure (New York Heart Association classes III and IV); (8) malignant tumors; and (9) autoimmune disease. In line with the inclusion criteria, 449 patients were initially enrolled, but, as a result of the exclusion criteria, 66 of these patients had to be excluded; therefore, in the end, 383 patients, including 192 male patients (50.1%), were included in the analysis. The average age of these patients was 84.31 ± 5.98 years old (range, 75–107 years old). In this study, the diagnosis of NSTE-AMI was strictly in accordance with the criteria of the fourth Edition of the Global Unified Definition of Myocardial Infarction, and other conditions that could cause TnI, such as severe heart failure, myocarditis and other infectious diseases, were excluded according to the exclusion criteria. Although elderly patients ≥75 years old were included in this study, the average age of the patients after the final inclusion was around 85 years old, and frailness and multiple comorbidities were indeed the main reasons for patients not undergoing PCI at this age.
The patients were divided into two groups according to the duration of the TnI elevation. In group 1, there were 194 patients, and the duration of the TnI elevation was ≥14 days, while, in group 2, there were 189 patients, and the duration of the TnI elevation was <14 days (Figure 1).
 |
Figure 1 Study population. Among the 66 excluded patients, 12 were lost to follow-up. Abbreviation: TnI, Troponin I. |
A diagnosis of NOAF, based on the 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation,10 was made when there was no significant P wave in a standard 12-lead ECG or a single-lead ECG of ≥30 seconds, and the R-R interval was irregular.
Data Acquisition
The data were collected from the electronic medical records of inpatients in our hospital. Previous medical history, baseline clinical features, laboratory test results at admission, echocardiographic results, discharge diagnosis, and follow-up clinical results were included in the database. The data were collected by five trained independent investigators.
Follow-Up Times, Methods, and Endpoints
All the patients were followed up by telephone, and the longest follow-up time was 60 months. For patients with re-hospitalization records, the original hospitalization records and outpatient data were also obtained. The primary endpoint was a composite endpoint of cardiovascular death, reinfarction, ischemic stroke, and hospitalization for heart failure, while the secondary endpoint was all-cause death. In addition, it was recorded whether the patients had NOAF during the follow-up period.
Statistical Analysis
Count data were expressed as percentage, and measurement data were expressed as mean ± standard deviation (x ± SD). The means of two samples were compared using a t-test, and the proportions of two samples were compared using a χ2 test. Kaplan–Meier survival analysis was used to analyze the correlation between the duration of the TnI elevation and the clinical endpoint events. The multivariate Cox stepwise regression risk model was used to analyze the independent related factors of the clinical endpoint events. The threshold value of variables included in the regression equation was set as p < 0.1, and the confounding factors to be corrected were as follows: age, digoxin use, diuretic use, smoking history, drinking history, uric acid, high sensitivity C-reactive protein (hs-CRP), N-terminal pro-B-type natriuretic peptide (NT-proBNP), TnI, total white blood cell (WBC) count, and left ventricular ejection fraction (LVEF).
As this study was not concerned with the onset time of NOAF, Spearman correlation analysis was used for the univariate analysis of NOAF, and a logistic binary stepwise regression model was used to analyze the independent related factors of NOAF. The threshold value of variables included in the regression equation was also set as p < 0.1. The confounding factors to be corrected for included age, digoxin use, diuretic use, smoking history, drinking history, uric acid, hs-CRP, NT-proBNP, TnI, total WBC count, LVEF, left atrial diameter, and the duration of the TnI elevation.
The median follow-up time was calculated using reverse Kaplan–Meier survival analysis. SPSS 19.0 and R language were used for statistical analysis. A p-value <0.05 was considered statistically significant.
Results
The Baseline Data of the Two Groups of Patients
Table 1 shows that in terms of general demographic data, laboratory tests, and cardiac ultrasound results, the age, uric acid, hs-CRP, NT-proBNP, and TnI levels were significantly higher in group 1 than in group 2 (p < 0.05 for all), while LVEF was significantly lower in group 1 than in group 2 (p < 0.05). In terms of the treatment and medication of patients, the utilization rates of digoxin and diuretics were significantly higher in group 1 than in group 2 (p < 0.05). In terms of other indexes, namely gender, smoking and drinking history, PCI history, systolic and diastolic blood pressure, heart rate, left atrial diameter, left ventricular end diastolic diameter, hypertension, diabetes, atrial fibrillation history, and use of aspirin/clopidogrel, ACEI/ARB/ARNI, β blockers, spironolactone, and statins, the differences between the two groups were not statistically significant (p > 0.05 for all).
 |
Table 1 Demographic and Clinical Characteristics of the Patients |
The Correlation Between the Duration of TnI Elevation and Clinical Endpoint Events
There were 182 cases (47.5%) of major composite endpoint events, among which there were 119 cases (65.4%) in group 1 and 63 cases (34.6%) in group 2, the former being significantly higher than the latter (hazard ratio [HR] 0.333; 95% confidence interval [CI]: 0.245–0.453, p < 0.001) (Figure 2A). In terms of the primary composite endpoint events, compared with group 2, cardiovascular death (88.7% vs 11.3%, HR 0.095, 95% CI: 0.043–0.210), re-infarction (54.7% vs 45.3%, HR 0.376, 95% CI: 0.225–0.627), ischemic stroke (47.5% vs 42.5%, HR 0.260, 95% CI: 0.132–0.511) and readmission due to heart failure (55.6% vs 44.4%, HR 0.279, 95% CI: 0.140–0.560) were significantly higher in group 1 (p < 0.001 for all). In terms of secondary endpoint events, there were 48 cases (12.5%) of all-cause death in the two groups, but there were significantly more cases in group 1 than in group 2 (38 vs 10; 58% vs 5.29%, HR 0.189, 95% CI: 0.093–0.376, p < 0.001) (Figure 2B).
Multivariate Cox Regression Model Analysis of the Clinical Endpoint Events
Multivariate Cox regression model analysis revealed that after controlling for age, digoxin use, uric acid, hs-CRP, NT-proBNP, total WBC count, smoking history, and drinking history, diuretic use (HR 1.570, 95% CI: 1.136–2.171, p = 0.006) and the duration of TnI elevation ≥14 days (HR 2.940, 95% CI: 2.126–4.064, p < 0.001) were independent risk factors for major composite endpoint events. LVEF (HR 1.034, 95% CI: 1.001–1.069, p = 0.042) and the duration of TnI elevation ≥14 days (HR 6.700, 95% CI: 3.203–14.014, p < 0.001) were independent risk factors for all-cause death (Table 2).
 |
Table 2 Univariate and Multivariate Cox Regression Analysis of Clinical Endpoints |
Univariate Analysis of the Variables Related to NOAF
Because this study was not concerned about the time of NOAF, Spearman correlation analysis was used to analyze the variables related to NOAF. The results revealed that the total WBC count (odds ratio [OR] 0.115; p = 0.025), uric acid (OR 0.128, p = 0.012), hs-CRP (OR 0.113, p = 0.027) and the duration of TnI elevation ≥14 days (OR 0.105, p = 0.040) were significantly related to the occurrence of NOAF. Other variables such as age, gender, smoking and drinking history, systolic blood pressure level, heart rate, NT-proBNP, TnI, left atrial diameter, left ventricular end diastolic diameter, LVEF, and the use of diuretics and digoxin were not correlated with the occurrence of NOAF (p > 0.05 for all) (Table 3).
 |
Table 3 Univariate Analysis of NOAF (Spearman Correlation) |
Multivariate Analysis of the Variables Related to NOAF
Binary multivariate logistic regression analysis revealed that after controlling for confounding factors such as age, NT-proBNP, left atrial diameter, LVEF, administration of digoxin and diuretics, TnI, and the duration of TnI elevation ≥14 days, only uric acid (OR 0.997, 95% CI: 0.995–1.000, p = 0.018) and hs-CRP (OR 0.994, 95% CI: 0.988–0.999, p = 0.015) were independent risk factors for NOAF (Table 4).
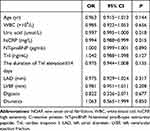 |
Table 4 Binary Logistic Regression Analysis of NOAF |
Discussion
The Duration of TnI Elevation and the Prognosis of Elderly Patients with NSTE-AMI
TnI is a regulatory protein of myocardial contraction that only exists in human cardiac muscle cells, and the content in skeletal muscle cells is very low.11 After myocardial cell injury and necrosis, TnI is released into the blood, and, therefore, the detection of TnI in the blood is a highly specific and sensitive method for the diagnosis of AMI.12 In AMI, TnI can be detected in the blood within 4–6 hours, lasts for about 7–10 days, and then decreases to a normal level.13 One study has confirmed that the increase in TnI is proportional to the size of the myocardial infarction;14 the higher the TnI value, the larger the infarct, and the poorer the prognosis of the patient. However, the correlation between the duration of TnI elevation and the prognosis remains unclear. In view of the fact that TnI elevation is often detected in elderly patients with NSTE-AMI, this study investigated the correlation between the duration of TnI elevation ≥14 days and the prognosis of elderly patients with NSTE-AMI.
A total of 383 elderly patients aged ≥75 years old who met the inclusion and exclusion criteria were enrolled in this study. Among them, 194 cases (50.7%) had a duration of TnI elevation ≥14 days, which accounted for half of the total cases. This suggested that, in elderly patients, the delayed reduction of elevated TnI to normal was very common, and, thus, it was necessary to study the effect of this phenomenon on the prognosis of elderly patients with NSTE-AMI.
The baseline data characteristics and laboratory and auxiliary examination results of the two groups were analyzed, and the results revealed that the patients in group 1 were older, had higher serum levels of uric acid, hsCRP, NT-proBNP, and TnI, had lower cardiac ejection fraction, and took more digoxin and diuretics, suggesting that for patients with a duration of TnI elevation ≥14 days, it often means poorer cardiac function and stronger inflammatory response, and the size of myocardial necrosis is larger. Moreover, the delayed reduction of elevated TnI to a normal level may be an aging phenomenon; that is to say, the older the person, the longer the duration of TnI elevation.
The median follow-up time was 26.00 ± 1.31 months (95% CI: 23.433–28.567, reverse Kaplan–Meier method), the duration of TnI elevation was closely related to the main composite endpoint (cardiovascular death, reinfarction, ischemic stroke, and hospitalization for heart failure) and all-cause death (Figure 2A and B). Univariate analysis revealed that diuretic use, TnI level, and the duration of TnI elevation ≥14 days were variables associated with the primary composite endpoint, while drinking history and the duration of TnI elevation ≥14 days were variables associated with all-cause death. Multivariate Cox regression model analysis revealed that after controlling for age, NT-proBNP, and other confounding factors, diuretic use and the duration of TnI elevation ≥14 days were independent risk factors of the primary composite endpoints, while LVEF and the duration of TnI elevation ≥14 days were independent risk factors of all-cause death.
The possible mechanism of prolonged duration of TnI elevation is that in elderly NSTE-AMI patients, the degree of coronary artery disease is more severe, and such patients have more multivessel disease, calcification disease, and chronic vascular occlusion disease,15 and the collateral circulation between the diseased vessels is complicated. After the acute occlusion of one vessel, the myocardial cells in the corresponding blood supply range are necrotic, and the level of TnI in the blood increases.16 Meanwhile, the perfusion pressure of the recipient vessel decreases,17 and the corresponding blood supply myocardial region is also in a state of ischemia. As a result, myocardial injury and necrosis occur slowly, causing the level of TnI in the blood to gradually increase. Similar to the increase in TnI, the duration of TnI elevation may also reflect the size of the myocardial infarction area to a certain extent. The longer the duration of TnI elevation, the larger the size of myocardial infarction, and patients are more likely to have various end-point events.
The use of diuretics reflects the volume load state of patients,18 and the increase in volume load is not only the cause of heart failure with decreased ejection fraction, but also the cause of heart failure with preserved ejection fraction.19 Therefore, the use of diuretics in elderly patients with NSTE-AMI suggests two problems, one being the heavy volume load and the other the poor cardiac function. The use of diuretics increases blood concentration, which increases the incidence of reinfarction and ischemic stroke,20 while poor cardiac function leads to increased hospitalization and cardiovascular death due to heart failure.21
LVEF is an independent risk factor of all-cause death, which is understandable since a decrease in LVEF often means a serious decrease in cardiac reserve function.22,23 In this state, in elderly patients with any disease, because the heart cannot provide strong and effective circulatory support, the death rate of such patients increases significantly.24,25
The Impact of the Duration of TnI Elevation on NOAF in Elderly Patients with NSTE-AMI
Of the 383 patients who were enrolled in this study, by the end of the follow-up period, 56 patients had NOAF, an incidence of 14.62%, which is significantly higher than that (7.9%) reported in the literature. The main reason for the difference in the incidence of NOAF may be related to the older age of the patients in this study. Age is one of the important risk factors for NOAF, and, with the increase in age, the incidence of atrial fibrillation increases significantly.26,27
There were 36 cases (18.56%) of NOAF in group 1 and 20 cases (10.58%) in group 2. This means that the incidence of NOAF in the two groups was not only higher than the average level reported in the literature but the difference in the incidence of NOAF between the two groups was also statistically significant. The incidence of NOAF in group 1 was higher than that in group 2. The above results suggest that age and the duration of TnI elevation are closely related to the occurrence of NOAF.
It is important to note that Spearman’s univariate correlation analysis revealed that the variables related to the occurrence of NOAF were the total WBC count, hs-CRP, uric acid, and duration of TnI elevation ≥14 days. The above factors were imported into a binary logistic regression model, and the confounding factors such as age, NT-proBNP, left atrial diameter, and LVEF were controlled. The results showed that only hs-CRP and uric acid were independently associated with NOAF, which is consistent with the conclusions of many previous studies.28 This explains, on the one hand, that the effect of hs-CRP and uric acid in promoting NOAF was stronger than that of age and the duration of TnI elevation ≥14 days, and, on the other hand, that the effect of the duration of TnI elevation ≥14 days on the occurrence of NOAF was gradually weakened. The reason for the latter may be that with the extension of follow-up time (the longest follow-up time was 60 months), the damaged and necrotic myocardium gradually healed, heart function was gradually compensated for, and the promoting effect of TnI elevation on NOAF was gradually weakened. However, inflammation secondary to myocardial infarction or other causes continued, and it eventually become an independent related factor for NOAF.
Atrial electrical remodeling and structural remodeling are the basis of the electrophysiology and anatomy of atrial fibrillation.29 Studies have confirmed that uric acid can induce and aggravate atrial remodeling by enhancing inflammation and oxidative stress, and thereby triggering the occurrence of atrial fibrillation.30,31
Uric acid is the end product of purine metabolism, and xanthine oxidase is the rate limiting enzyme of its synthesis. A physiological concentration of uric acid has antioxidant properties, but when uric acid enters the cell or is in the acidic/hydrophobic environment of atherosclerotic plaque, the antioxidant properties will change, and it becomes a pro-oxidant.32 Due to the decline of the metabolic function of the body, elderly patients often have hyperuricemia. A high concentration of uric acid, together with its rate limiting enzyme xanthine oxidase, is likely to cause the generation of oxygen-free radicals such as superoxide anion and hydrogen peroxide in the body.33 Both the increase of oxidative stress and the activation of inflammation result in the occurrence and development of NOAF.
There are some limitations to this study: (1) It is a single-center retrospective cohort study, and the sample size is limited to a certain extent; (2) The patients were weak on admission, most patients being admitted to the hospital in a supine position, and so body mass index could not be calculated; (3) All the patients were elderly, and some auxiliary tests were not carried out, so the sample data were incomplete, and some patients were excluded from the study. In the future, a prospective cohort design with a larger sample size is needed to verify the conclusions of this study.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Beijing Hepingli Hospital (BJSHPLYY-IRB-KYXM-2021-05). Written informed consent was obtained from all participants.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Schmitt J, Duray G, Gersh BJ, et al. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30(9):1038–1045. doi:10.1093/eurheartj/ehn579
2. Jabre P, Roger VL, Murad MH, et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta⁃analysis. Circulation. 2011;123(15):1587–1593. doi:10.1161/CIRCULATIONAHA.110.986661
3. Bas HA, Aksoy F, Icli A, et al. The association of plasma oxidative status and inflammation with the development of atrial fibrillation in patients presenting with ST elevation myocardial infarction. Scand J Clin Lab Invest. 2017;77(2):77–82. doi:10.1080/00365513.2016.1244857
4. Bağcı A, Aksoy F. Systemic immune-inflammation index predicts new-onset atrial fibrillation after ST elevation myocardial infarction. Biomark Med. 2021;15(10):731–739. doi:10.2217/bmm-2020-0838
5. Garg L, Agrawal S, Agarwal M, et al. Influence of atrial fibrillation on outcomes in patients who underwent primary percutaneous coronary intervention for ST‐segment elevation myocardial infarction. Am J Cardiol. 2018;121:684–689. doi:10.1016/j.amjcard.2017.12.003
6. Zeymer U, Annemans L, Danchin N, et al. Impact of known or new‐onset atrial fibrillation on 2‐year cardiovascular event rate in patients with acute coronary syndromes: results from the prospective EPICOR registry. Eur Heart J Acute Cardiovasc Care. 2019;8:121–129. doi:10.1177/2048872618769057
7. Jin YY, Bai R, Ye M, et al. [Risk factors and prognoses analysis of new-onset atrial fibrillation in patients with acute myocardial infarction]. Zhonghua Nei Ke Za Zhi. 2019;58(2):133–138. Chinese. doi:10.3760/cma.j.issn.0578-1426.2019.02.010
8. Obayashi Y, Shiomi H, Morimoto T, et al. Newly diagnosed atrial fibrillation in acute myocardial infarction. J Am Heart Assoc. 2021;10(18):e021417. doi:10.1161/JAHA.121.021417
9. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–2264. doi:10.1016/j.jacc.2018.08.1038
10. Hindricks G. Corrigendum to: 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):546–547. doi:10.1093/eurheartj/ehaa798
11. Aydin S, Ugur K, Aydin S, et al. Biomarkers in acute myocardial infarction: current perspectives. Vasc Health Risk Manag. 2019;15:1–10. doi:10.2147/VHRM.S166157
12. Eggers KM, Oldgren J, Nordenskjöld A, et al. Diagnostic value of serial measurement of cardiac markers in patients with chest pain: limited value of adding myoglobin to troponin I for exclusion of myocardial infarction. Am Heart J. 2004;148(4):574–581. doi:10.1016/j.ahj.2004.04.030
13. Ramasamy I. Biochemical markers in acute coronary syndrome. Clin Chim Acta. 2011;412(15–16):1279–1296. doi:10.1016/j.cca.2011.04.003
14. Park KC, Gaze DC, Collinson PO, et al. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res. 2017;113(14):1708–1718. doi:10.1093/cvr/cvx183
15. Varghese T, Wenger NK. Non-ST elevation acute coronary syndrome in women and the elderly: recent updates and stones still left unturned. F1000Res. 2018;7:F1000Faculty Rev–1865. doi:10.12688/f1000research.16492.1
16. Al-Otaiby MA, Al-Amri HS, Al-Moghairi AM. The clinical significance of cardiac troponins in medical practice. J Saudi Heart Assoc. 2011;23(1):3–11. doi:10.1016/j.jsha.2010.10.001
17. Stoller M, Seiler C. Pathophysiology of coronary collaterals. Curr Cardiol Rev. 2014;10(1):38–56. doi:10.2174/1573403x113099990005
18. Mullens W, Damman K, Harjola VP, et al. The use of diuretics in heart failure with congestion - a position statement from the heart failure association of the European society of cardiology. Eur J Heart Fail. 2019;21(2):137–155. doi:10.1002/ejhf.1369
19. van der Meer P, Gaggin HK, Dec GW. ACC/AHA versus ESC guidelines on heart failure: JACC guideline comparison. J Am Coll Cardiol. 2019;73(21):2756–2768. doi:10.1016/j.jacc.2019.03.478
20. Felker GM, Ellison DH, Mullens W, et al. Diuretic therapy for patients with heart failure: JACC state-of-The-art review. J Am Coll Cardiol. 2020;75(10):1178–1195. doi:10.1016/j.jacc.2019.12.059
21. Murphy SP, Ibrahim NE, Januzzi JL. Heart failure with reduced ejection fraction: a review. JAMA. 2020;324(5):488–504. doi:10.1001/jama.2020.10262
22. Hayıroğlu Mİ, Keskin M, Uzun AO, et al. Predictors of in-hospital mortality in patients with ST-segment elevation myocardial infarction complicated with cardiogenic shock. Heart Lung Circ. 2019;28(2):237–244. doi:10.1016/j.hlc.2017.10.023
23. Hayıroğlu Mİ, Çınar T, Çinier G, et al. Comparison of mortality prediction scores in elderly patients with ICD for heart failure with reduced ejection fraction. Aging Clin Exp Res. 2021. doi:10.1007/s40520-021-01960-6
24. Zheng PP, Yao SM, Guo D, et al. Prevalence and prognostic value of heart failure stages: an elderly inpatient based cohort study. Front Med (Lausanne). 2021;8:639453. doi:10.3389/fmed.2021.639453
25. Sakata Y, Tsuji K, Nochioka K, et al. Transition of left ventricular ejection fraction in heart failure. Adv Exp Med Biol. 2018;1067:5–15. doi:10.1007/5584_2018_178
26. Gutierrez C, Blanchard DG. Diagnosis and treatment of atrial fibrillation. Am Fam Physician. 2016;94(6):442–452.
27. Aksoy F, Baş HA, Bağcı A, et al. The CHA2DS2-VASc score for predicting atrial fibrillation in patients presenting with ST elevation myocardial infarction: prospective observational study. Sao Paulo Med J. 2019;137(3):248–254. doi:10.1590/1516-3180.2018.0431140319
28. Oikonomou E, Zografos T, Papamikroulis GA, et al. Biomarkers in atrial fibrillation and heart failure. Curr Med Chem. 2019;26(5):873–887. doi:10.2174/0929867324666170830100424
29. Arslan A, Ozaydin M, Aksoy F, et al. Association between the use of renin-angiotensin system blockers and development of in-hospital atrial fibrillation in patients with ST-segment elevation myocardial infarction. Medicina (Kaunas). 2016;52(2):104–109. doi:10.1016/j.medici.2016.02.006
30. Tamariz L, Hernandez F, Bush A, et al. Association between serum uric acid and atrial fibrillation: a systematic review and meta-analysis. Heart Rhythm. 2014;11(7):1102–1108. doi:10.1016/j.hrthm.2014.04.003
31. Pak S, Yatsynovich Y, Valencia D, et al. Serum uric acid and atrial fibrillation: meta-analysis. Crit Pathw Cardiol. 2018;17(3):161–166. doi:10.1097/HPC.0000000000000150
32. Ndrepepa G. Uric acid and cardiovascular disease. Clin Chim Acta. 2018;484:150–163. doi:10.1016/j.cca.2018.05.046
33. Yu W, Cheng JD. Uric acid and cardiovascular disease: an update from molecular mechanism to clinical perspective. Front Pharmacol. 2020;11:582680. doi:10.3389/fphar.2020.582680
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

