Back to Journals » Nature and Science of Sleep » Volume 14
The Impact of Morning Surgery or Afternoon Surgery on Postoperative Sleep Quality and Melatonin Levels of Elderly Patients: A Prospective, Randomized Study
Authors Yang R, Xu XX, Liu H , Dai W, Zhang ZQ, Wang TT, Chen SS, Gu EW, Liu XS , Mei B
Received 2 June 2022
Accepted for publication 9 September 2022
Published 21 September 2022 Volume 2022:14 Pages 1677—1686
DOI https://doi.org/10.2147/NSS.S377209
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ahmed BaHammam
Rui Yang,* Xiao-Xia Xu,* Hu Liu, Wei Dai, Zheng-Qin Zhang, Ting-Ting Wang, Shi-Shou Chen, Er-Wei Gu, Xue-Sheng Liu, Bin Mei
Department of Anesthesiology, The First Affiliated Hospital of Anhui Medical University, Hefei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xue-Sheng Liu; Bin Mei, Department of Anesthesiology, The First Affiliated Hospital of Anhui Medical University, 218 Jixi Road, Hefei, Anhui, 230022, People’s Republic of China, Tel +86 551-62922344, Fax +86 551 62923704, Email [email protected]; [email protected]
Objective: Postoperative sleep disturbance after surgery is not conducive to the recovery of patients. The purpose of this study was to determine the influence of the timing of surgery (morning vs afternoon) on the postoperative sleep quality of elderly patients and to analyze the relationship between the timing of surgery and the change in the melatonin level.
Methods: Sixty patients who received hip surgery were randomly assigned to the Morning Group (Group M) or the Afternoon Group (Group A). The sleep quality was assessed by the Richards–Campbell Sleep Questionnaire. Before and after surgery, the nocturnal urine was collected over a 12-h period, and the 6-sulfatoxymelatonin concentration was measured. Also, the incidence of postoperative delirium (POD) was observed.
Results: On the first and second nights after surgery, the sleep quality scores of the patients in Group A were greater than those in Group M, and there was no difference in the sleep quality scores between the two groups on the third night after surgery (P=0.000, P=0.002, P> 0.05, respectively). In addition, the urine 6-sulphatoxymelatonin concentration was found to be greater in Group A than in Group M on the first night of surgery (P=0.00). Both the postoperative sleep quality scores and urine 6-sulphatoxymelatonin concentration were significantly less than those before surgery (P=0.00, P=0.00).
Conclusion: The postoperative sleep quality scores and melatonin levels of elderly patients who received hip surgery under general anesthesia were significantly less than those of the patients before surgery. Furthermore, the short-term sleep quality of the patients who received surgery in the afternoon was better than that of the patients who received surgery in the morning. This difference may be related to the short-term change of the melatonin level after surgery.
Keywords: sleep quality, melatonin, timing of surgery
Background
A regular circadian rhythm is critical to maintain a stable physiological status.1 For older adults, circadian rhythm is considered to play a crucial role to regulate sleep quality and duration, which is associated with cognitive function change.2 Several studies have demonstrated that surgery and anesthesia can disrupt the normal circadian rhythm and cause postoperative sleep disturbance,3,4 and the potential mechanism of this phenomenon still needs to be further clarified.
The central pacemaker in the suprachiasmatic nucleus (SCN) is associated with the organization of the circadian rhythm.5 Melatonin, a hormone released from the pineal gland after receiving the signal from SCN, plays a crucial role in regulating the sleep-awake cycle.6 Several studies have indicated that anesthesia and surgery have an impact on the perioperative melatonin level.7,8 It seems can be speculated that the change of melatonin is one of the potential mechanisms of perioperative circadian rhythm sleep-wake disorder. General anesthesia is also considered to be an independent risk factor for postoperative sleep disturbances, leading to a significant reduction in rapid eye movement sleep, which in turn causes circadian rhythm asynchrony.9 The unconsciousness induced by general anesthesia is a non-physiological process similar to natural sleep. Buxton et al have reported that taking a nap in the morning results in a delay of both the melatonin and thyroid-stimulating hormone peak levels, thereby impairing the normal circadian rhythm.10 Therefore, the timing of general anesthesia may also have an impact on postoperative sleep disturbance.
Besides the impact of surgery and anesthesia, the time of day of the surgery also has been reported to influence the recovery of patients.11,12 So, we hypothesize that postoperative sleep quality and melatonin levels would be greater in patients who underwent surgery in the afternoon than in those who underwent surgery in the morning.
We conducted the current study to investigate the influence of the timing of the surgery (morning vs afternoon) on the postoperative sleep quality of elderly patients who received hip surgery and to analyze the relationship between the timing of the surgery and the change in the melatonin level. Also, the incidence of postoperative delirium (POD) was observed.
Methods
Ethical Approval and Patient Eligibility Criteria
The Ethical Committee of our hospital approved this study (PJ2020-17-17) on December 17, 2020. Written informed consent was obtained from all patients prior to study enrolment. This study was also registered with the Chinese Clinical Trial Register (ChiCTR2100046773).
Patients undergoing hip surgery who were 65 years or older were included in this study. All of these patients were classified as American Society of Anesthesiologists (ASA) physical health class II to III. Patients were excluded from this study if they met any of the following criteria: Patients who refused to be included in this study, patients with mental or language barriers, patients with infections and renal insufficiency, patients who had been anesthetized within the past 30 days, patients who needed to receive surgeries for both hips, and patients with preoperative sleep disorders such as insomnia, obstructive sleep apnea, restless legs syndrome, etc. In addition, patients exhibiting cognitive impairment (ie, a Mini-Mental State Examination score <24) and/or preoperative delirium (ie, a positive Confusion Assessment Method result) were excluded.
Study Protocol
Demographic information, medications, and comorbidities were recorded for each patient. The cardiac function was assessed by the New York Heart Association classification (class I–IV), according to the patient’s activity tolerance. Class I is unrestricted physical activity, meaning that normal physical activity does not cause excessive fatigue, palpitations, or difficulty breathing in the patients. Class II is mild limitation of physical activity, meaning that the patient is comfortable at rest, but general physical activity can cause fatigue, palpitations, or difficulty breathing. Grade III is markedly limited physical activity, meaning that the patient is comfortable at rest, but less-than-usual activity can lead to fatigue, palpitations, or difficulty breathing. Class IV is the inability to perform any physical activity without discomfort, meaning that the patients experience symptoms of cardiac insufficiency at rest, and any physical activity will increase discomfort. The preoperative sleep quality was assessed by the Richards Campbell Sleep Questionnaire (RCSQ) and the Pittsburgh Sleep Quality Index (PSQI),13,14 In addition, the Mini-Mental State Examination and Confusion Assessment Method results were collected for all patients on the day before surgery.15 Moreover, to assess the risk of POD, the Inouye risk assessment was also performed for all patients.16 A total of 60 participants were randomly divided into the following two groups with computer-generated numbers placed in opaque, sealed envelopes: Patients whose surgeries started after 8:00 am and finished before 12:00 pm (Morning group, Group M); and patients whose surgeries started after 1:00 pm (Afternoon group, Group A). The randomization was done by the chief resident of the orthopedic surgery department who was blinded to this study.
On the day of surgery, after the patients arrived in the operating room, the patient characteristics, including invasive arterial pressure, pulse oximetry, and 5-lead electrocardiography, were monitored. All patients underwent bispectral index monitoring (BIS, Vista, Aspect Medical System Inc., USA) to determine the depth of sedation. To reduce the consumption of opioids and to provide sufficient postoperative analgesia, an ultrasound-guided iliac fascia block (30 mL of 0.375% ropivacaine) was applied to all patients. All patients received general anesthesia after the iliac fascia block, anesthesia induction was completed by an intravenous sufentanil bolus (0.2 μg/kg), a target-controlled infusion of propofol was carried out to keep the BIS between 40 and 60, and a bolus of rocuronium (0.6 mg/kg) was administered to facilitate tracheal intubation. Remifentanil was infused at a rate of 0.05–0.15 μg/kg/min to provide intraoperative analgesia. Then sufentanil at 0.3 μg/kg and 0.1 μg/kg was administered at 5 min before the onset of the operation and at 30 min before the end of the operation, respectively. During the operation, rocuronium was also used as needed. A laryngeal mask (LMA Supreme, Laryngeal Mask Company Limited, Malaysia) was used for airway management, and all patients tolerated the operation well as the muscle relaxant rocuronium was used. The consumption amounts of sufentanil and propofol during the operation were recorded. Intraoperative hypotension, defined as a decrease in systolic blood pressure greater than 30% from preoperative values and/or a systolic blood pressure less than 90 mmHg, was treated immediately by a bolus infusion of phenylephrine.
After surgery, all patients recovered in the Postanesthesia Unit and were transferred to the Inpatient Ward when they achieved a Steward score greater than 4. An oral analgesic (tramadol hydrochloride sustained-release tablet) was also provided to patients who required extra analgesia.
Postoperative Sleep Quality and POD Assessment
The postoperative sleep quality was assessed by the RCSQ assessment, and the score obtained on the first day after surgery was set as the primary endpoint investigated in this study. One trained nurse in our department who was blinded to this study conducted the RCSQ on the first three days after surgery. The incidence of POD within three days after surgery was also recorded by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition;17 this evaluation was performed by another trained nurse who was also blinded to this study. Postoperative complications within 30 days were also recorded.
Nocturnal Urine Collection and 6-Sulphatoxymelatonin (6-SMT) Measurement
Nocturnal urine was collected by the duty nurses who were blinded to this study. The collections were between 8:00 pm and 8:00 am during the night before surgery and the first and second nights after surgery. To protect the urine from light, the uric bags were covered with black plastic bags. After the total volume in 12 h was recorded, one tube containing a 2-mL sample was collected and frozen at −20℃ for later analysis. The concentrations of 6-SMT, the stable metabolite of melatonin, was measured by an enzyme-linked immunosorbent assay (IBL, Hamburg, Germany), in duplicate.18 Effect size (ES) calculations were used to compare the degree of melatonin changes in each group after and before surgery.19 The larger the ES value, the greater the degree of change.
Sample Size and Statistical Analyses
A pilot study in which 20 patients were randomly assigned to Group A or Group M was conducted. The mean RCSQ average scores of Group A on the first postoperative day were 50.2, and the mean RCSQ average scores of Group M on the first postoperative day were 34.8, with a standard deviation of 16.5. It was determined that a sample size of 28 patients in each group would provide 95% power with a two-sided α of 5% to detect differences in the mean scores between the two groups, as calculated with PASS 11.0 software (NCSS, LLC, Kaysville, UT, USA). Therefore, we increased the sample size to 30 patients per group in the current study to account for the possibility that patients might be lost to follow up.
Continuous variables were presented as the mean and variance or median and inter-quartile range. Categorical variables were expressed as frequencies. The distribution of continuous variables was analyzed by the Kolmogorov–Smirnov normality test. Continuous data were compared using an independent-samples t-test and Manne Whitney U-test as appropriate. Categorical data were compared using Pearson’s chi-square tests or Fisher’s exact test as appropriate. The independent t-test was used to compare RCSQ scores between the groups, and the Mann–Whitney Rank Sum Test was used to compare the concentration of urine 6-SMT between the groups. Based on the two-tailed probability, significance was considered when P <0.05. A post hoc analysis of the differences between Group A and Group M was performed using a multivariable linear regression analysis for potential confounders. All statistical analyses were done using SPSS version 16 software (IBM Corp., Armonk, NY, U.S.A.).
Results
From June 2021 to December 2021, of the 95 patients who were screened for the study, 35 patients were excluded: 28 failed to meet the inclusion criteria, 5 refused to participate, and 2 were unable to consent. During the postoperative follow-up period, no patients were lost to follow-up. A total of 60 patients were included in the final analysis (Figure 1). Demographic characteristics did not differ between the two groups (Table 1).
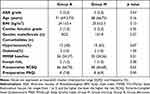 |
Table 1 Demographic Characteristics of Patients |
 |
Figure 1 The CONSORT flowchart. Notes: Adapted from: Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010;7(3):e1000251.37 Copyright: © 2010 Schulz et al. Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/legalcode). https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000251. |
The sleep quality scores of the patients in Group A were lower on the first night after surgery than before surgery, and there was no difference in the sleep quality scores on the second and third days after surgery compared with those before surgery (P=0.003). Meanwhile, the sleep quality scores of the patients in Group M were lower on the first three nights after surgery than those before surgery (P=0.000, P=0.000, P=0.003, respectively). As shown in Figure 2, on the first and second nights after surgery, the sleep quality scores of the patients in Group A were greater than those in Group M, and there was no difference in the sleep quality scores between the two groups on the third night after surgery (P=0.033, P=0.011, P>0.05). After adjusting for the consumption of propofol, postoperative pain score, and duration of surgery by multiple linear regression, the patients undergoing surgery in the afternoon were independently associated with a higher sleep quality score on the first postoperative night (beta coefficient=−0.29, P=0.03). The five parts of the RCSQ were calculated separately to discover differences between the groups. On the first night after surgery, the sleep latency score in Group A was greater than that in Group M, and there was no difference in the other four items between the two groups (P=0.002). On the second night after surgery, the scores of sleep depth, sleep latency, and awakenings in Group A were greater than those in Group M, and there was no difference between the two groups for the other two items (P=0.016, P=0.004, P=0.041, respectively). On the third night after surgery, the scores of sleep depth and sleep latency in Group A were greater than those in Group M, and there was no difference for the other three items between the two groups (P=0.049, P=0.028, respectively). There was no difference in the noise intensity score between the two groups in the first three nights after surgery (all P>0.05).
As shown in Table 2, there were no differences in intraoperative consumption of propofol or remifentanil, or duration of surgery or anesthesia between the two groups (all P>0.05). The times of eye-opening, extubation, and Postanesthesia Unit stay did not differ between the two groups (all P>0.05). In addition, there were no differences in the pain scores within 24, 48, or 72 h after surgery or in the consumption of opioids within 72 h after surgery between the two groups (all P>0.05). Moreover, there was no difference in the incidence of POD or postoperative complications within 30 days between the two groups (P>0.05).
 |
Table 2 Intraoperative and Postoperative Data for the 2 Anesthetic Groups |
The preoperative and postoperative total nocturnal excretion levels of urinary 6-SMT over 12 h in patients are shown in Figure 3 and Table 3. The postoperative total urinary excretion of 6-SMT for the two groups of patients was significantly less than that before surgery (all P<0.05). For the night before surgery and the second night after surgery, no significant differences were found in the total urinary excretion of 6-SMT between Group M and Group A. However, the total urinary excretion of 6-SMT was found to be greater in Group A than in Group M on the first night after surgery (P=0.00). ES calculation showed that the 6-SMT concentration of both groups on the first and second day after surgery was significantly lower than that before surgery. The decrease in melatonin concentration in Group A was lower than that in Group M on the second day after surgery (Table 4). After adjusting for the consumption of propofol, postoperative pain score, and duration of surgery by multiple linear regression, the patients who underwent surgery in the afternoon were independently associated with a greater total urinary excretion of 6-SMT on the first postoperative night (beta coefficient=−0.33, P=0.01).
 |
Table 3 The Concentration of 6-SMT Before and Two Days After Surgery for the 2 Anesthetic Groups |
 |
Table 4 The 6-SMT Concentration of Patients in Each Group Changes Over Time |
Discussion
High-quality sleep is essential for maintaining the physical and mental health of normal people, and the incidence of postoperative sleep disturbance is very high in major surgery and elderly patients.20 Postoperative sleep disturbance could seriously affect the neurocognitive function of patients, and even worsen the outcomes of patients.21 A study on knee surgery demonstrated that patients developed sleep disturbance for up to a month after surgery, which seriously affected the recovery of motor function.22 In our study, patients in both groups exhibited postoperative sleep disturbance, which is consistent with the previous studies. Existing evidence indicated aging is a potential factor associated with postoperative sleep disturbance, as for elderly patients, it could be difficult to adjust their sleep habits as the environment changed.23 Anesthesia is also considered a factor leading to postoperative sleep disturbance, and the large use of opioids during general anesthesia may be one of the important reasons.24 For the patients included in this study, an iliac fascia block was performed to reduce opioid use; however, this effort is not considered to be sufficient to improve the postoperative sleep quality of patients, as surgical trauma is an important and unavoidable risk factor of postoperative sleep disturbance.25
Melatonin is the crucial hormone involved in regulating sleep rhythm.6 The secretion of melatonin exhibited an obvious circadian rhythm feature.26 Under the influence of light, the secretion was inhibited during the day and increased significantly at night. And regulating the impulse and firing frequency of SCN through the MT1 and MT2, which are high-affinity G protein coupled receptors and widely distributed in the suprachiasmatic nucleus of hypothalamus, is the biological mechanism of melatonin participating in the regulation of sleep.27 6-SMT, the metabolite of melatonin, has been demonstrated to be a reliable humoral index to reflect the change of endogenous melatonin.18 Surgery can lead to changes in melatonin level.7,8 In a study of patients who received non-cardiac surgery, it was found that 6-SMT in urine decreased significantly after surgery.18 And the effect of surgery on melatonin is mainly manifested in the decrease of night/day secretion ratio.28 In our study, whether the patients underwent surgery in the morning or afternoon, the level of 6-SMT in nocturnal urine decreased significantly after surgery. Based on this evidence, the change in melatonin level induced by surgery might be a potential neuroendocrine mechanism causing postoperative sleep disturbance. Some factors might have an influence on the secretion of melatonin after surgery in the two groups of patients. In terms of external factors, both strong light and β-blockers can reduce the secretion of endogenous melatonin. The patients in this study spent their evenings under artificial light in the hospital, so the influence of external environmental factors related to the hospital can be ignored. On the other hand, neither group of patients took β-blockers. Propofol dose, duration of surgery, and postoperative pain score also had potential effects on postoperative melatonin secretion in patients.29–31 In our study, the propofol dose, and duration of surgery were balanced between the two groups, so the influence of the above-mentioned factors was negligible for our conclusions. Postoperative pain and circadian rhythm are bidirectionally affected. Poor postoperative pain control can promote postoperative sleep disturbance in patients. However, Cronin et al reported that the occurrence of postoperative sleep disturbances in patients undergoing abdominal surgery was not associated with well-controlled pain. In our study, postoperative pain was effectively controlled in both groups. Therefore, the effect of postoperative pain on postoperative melatonin secretion in our study was subtle.
The impact of circadian rhythm on surgical outcomes has been investigated in previous studies. For example, Montaigne et al performed a single-center propensity matched cohort study and a randomized study at the same time to determine the influence of the timing of surgery on the incidence of perioperative myocardial injury. The results of both two studies indicated afternoon surgery might provide perioperative myocardial protection and lead to improved patient outcomes compared with morning surgery.11 It seems that the timing of surgery can influence the outcomes of surgical patients. In our study, we compared the influence of surgical procedures performed at different times of the day (morning vs afternoon) on the postoperative sleep quality of patients who received hip surgery. Our study suggested that elderly patients undergoing hip surgery in the afternoon had a better postoperative sleep quality than those undergoing surgery in the morning. For healthy people who do not undergo surgery, a daytime nap potentially affects their circadian rhythm and melatonin secretion. A previous study has found that taking a nap in the morning results in a delay of both peak melatonin and thyroid-stimulating hormone levels, thereby impairing the normal circadian rhythm. By contrast, taking a nap in the afternoon had no influence on the melatonin secretion.10 In our study, the total urinary excretion of 6-SMT during the first postoperative night was found to be greater in patients who received surgery in the afternoon, indicating that the short time of general anesthesia performed in the patients in our study potentially had a similar influence on the circadian rhythm as a daytime nap. The change in endogenous melatonin level, which is reflected by the urinary excretion of 6-SMT, could be the reason why elderly patients undergoing hip surgery in the afternoon obtained better postoperative sleep quality than patients undergoing hip surgery in the morning. A previously published study also compared the effects of the timing of surgery under general anesthesia on postoperative sleep quality in patients; the results demonstrated that the patients who received surgery in the morning (8 am to noon) had a better postoperative sleep quality than those who underwent surgery in the night (6 pm to 10 pm).12 This study mainly compared surgeries performed in the morning and evening, while our study compared the effect of morning or afternoon surgery on postoperative sleep quality. In addition, different from our results, their results suggest that night surgery can lead to differences in intraoperative anesthetics consumption and postoperative pain and may contribute to the difference in postoperative sleep quality. In our study, the decreased endogenous melatonin secretion level might be the mechanism of the decreased postoperative sleep quality scores. Several studies have also confirmed that the use of exogenous melatonin can improve sleep quality.32 Therefore, according to the results of the current study, the addition of exogenous melatonin to patients who are expected to undergo surgery in the morning may help improve their postoperative sleep quality. Future studies of the effect of adding exogenous melatonin to patients undergoing morning surgery may be needed.
Sleep-wake cycle and circadian rhythm disorder are the typical characteristics of POD, and a lack of synchronization between the sleep-wake cycle and melatonin secretion can impair postoperative neurocognitive function.33 The results from a study of noncardiac surgical patients have demonstrated that the proportion of nocturnal sleep awakening in the total sleep time of patients with POD was significantly greater than that of patients without POD.34 In addition, another study has reported that the melatonin levels in patients with POD are significantly less than those in patients without delirium.35 Moreover, the exogenous application of melatonin has been proven to improve the neurocognitive function of surgical patients and patients hospitalized in the Intensive Care Unit.36 Our results also suggest that postoperative melatonin level and/or sleep quality may influent postoperative cognitive function, although it did not reach a significant difference. In our study, five patients who received surgery in the morning developed POD, while only three patients who received surgery in the afternoon developed POD.
There are some limitations in our study. We failed to observe the change of postoperative sleep quality in the long term as the sleep quality of the patients was only monitored for three days after surgery. The difference in postoperative sleep quality disappeared on the third day after surgery, and the difference in the level of 6-SMT only exist on the first night after surgery, which indicated the influence of daytime variation on the postoperative sleep quality and melatonin level was transient. The change of postoperative sleep quality was the primary outcome we want to observe in the current study, which lead to the small sample size, and is probably the reason for the failure to obtain significant differences in postoperative neurocognitive function. In the future, a multicenter randomized study with a large sample size needs to be conducted to investigate the impact of the timing of surgery on postoperative neurocognitive function in elderly patients.
In conclusion, the postoperative sleep quality scores and melatonin levels of elderly patients who received hip surgery under general anesthesia were significantly less than those of the patients before surgery. Furthermore, the short-term sleep quality of the patients who received surgery in the afternoon was better than that of the patients who received surgery in the morning. This difference may be related to the short-term change of the melatonin level after surgery.
Registration
This work was registered at the Chinese Clinical Trial Register (ChiCTR2100046773).
Data Sharing Statement
Individual deidentified participant data can be obtained from the corresponding author with approval from the corresponding author within three years of publication, as can the published main results as well as the study protocol.
Ethical Adherence
Ethical approval (PJ2020-17-17) was provided by the Ethical Committee Anhui Medical University, Hefei, Anhui, China. All patients provided informed consent and all procedures were conducted according to the Declaration of Helsinki.
Acknowledgment
The authors would like to thank Panpan Fang, MD, Ph.D., from the Department of Anesthesiology, The First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China for her work on statistical analysis.
Funding
This work was supported by the National Nature Science Foundation of China (Grant No. 82172136) and the Innovation and entrepreneurship project for returned overseas students in Anhui Province (Grant No. 2022LCX023).
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Huang W, Ramsey KM, Marcheva B, et al. Circadian rhythms, sleep, and metabolism. J Clin Invest. 2011;121(6):2133–2141. doi:10.1172/JCI46043
2. Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017–1028. doi:10.1016/S1474-4422(14)70172-3
3. Song Y, Liu Y, Yuan Y, et al. Effects of general versus subarachnoid anaesthesia on circadian melatonin rhythm and postoperative delirium in elderly patients undergoing Hip fracture surgery: a prospective cohort clinical trial. EBioMed. 2021;70:103490. doi:10.1016/j.ebiom.2021.103490
4. O’Gara BP, Gao L, Marcantonio ER, et al. Sleep, pain, and cognition: modifiable targets for optimal perioperative brain health. Anesthesiology. 2021;135(6):1132–1135. doi:10.1097/ALN.0000000000004046
5. Levi F. Circadian rhythms: mechanisms and therapeutic implications. Annu Rev Pharmacol Toxicol. 2007;47:593–628. doi:10.1146/annurev.pharmtox.47.120505.105208
6. RJ Reiter. Pineal melatonin: cell biology of its synthesis and of its physiological interactions. Endocr Rev. 1991;12(2):151–180. doi:10.1210/edrv-12-2-151
7. Nishi T, Saeki K, Miyata K, et al. Effects of cataract surgery on melatonin secretion in adults 60 years and older: a randomized clinical trial. JAMA Ophthalmol. 2020;138(4):405–411. doi:10.1001/jamaophthalmol.2020.0206
8. Scholtens RM, van Munster BC, van Faassen M, et al. Plasma melatonin levels in Hip fracture patients with and without delirium: a confirmation study. Mech Ageing Dev. 2017;167:1–4. doi:10.1016/j.mad.2017.08.016
9. Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track Hip and knee arthroplasty. Br J Anaesth. 2012;109(5):769–775. doi:10.1093/bja/aes252
10. Buxton OM, L’Hermite-Balériaux M, Turek FW, et al. Daytime naps in darkness phase shift the human circadian rhythms of melatonin and thyrotropin secretion. Am J Physiol Regul Integr Comp Physiol. 2000;278(2):R373–R382. doi:10.1152/ajpregu.2000.278.2.R373
11. Montaigne D, Marechal X, Modine T, et al. Daytime variation of perioperative myocardial injury in cardiac surgery and its prevention by Rev-Erbα antagonism: a single-centre propensity-matched cohort study and a randomised study. Lancet. 2018;391(10115):59–69. doi:10.1016/S0140-6736(17)32132-3
12. Song B, Li Y, Teng X, et al. Comparison of morning and evening operation under general anesthesia on intraoperative anesthetic requirement, postoperative sleep quality, and pain: a randomized controlled trial. Nat Sci Sleep. 2020;12:467–475. doi:10.2147/NSS.S257896
13. Chen LX, Ji DH, Zhang F. Richards-Campbell sleep questionnaire: psychometric properties of Chinese critically ill patients. Nurs Crit Care. 2019;24(6):362–368. doi:10.1111/nicc.12357
14. Chang Q, Xia Y, Bai S, et al. Association between Pittsburgh sleep quality index and depressive symptoms in Chinese resident physicians. Front Psychiatry. 2021;12:564815. doi:10.3389/fpsyt.2021.564815
15. Mei B, Xu G, Han W, et al. The benefit of dexmedetomidine on postoperative cognitive function is unrelated to the modulation on peripheral inflammation: a single-center, prospective, randomized study. Clin J Pain. 2020;36(2):88–95. doi:10.1097/AJP.0000000000000779
16. Inouye SK, Viscoli CM, Horwitz RI, et al. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993;119(6):474–481. doi:10.7326/0003-4819-119-6-199309150-00005
17. Sachdev PS, Blacker D, Blazer DG, et al. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol. 2014;10(11):634–642. doi:10.1038/nrneurol.2014.181
18. Hu RF, Jiang XY, Hegadoren KM, et al. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care. 2015;19(1):115. doi:10.1186/s13054-015-0855-3
19. Kazis LE, Anderson JJ, RF Meenan. Effect sizes for interpreting changes in health status. Med Care. 1989;27(3 Suppl):S178–S189.
20. Su X, DX Wang. Improve postoperative sleep: what can we do? Curr Opin Anaesthesiol. 2018;31(1):83–88. doi:10.1097/ACO.0000000000000538
21. Rampes S, Ma K, Divecha YA, et al. Postoperative sleep disorders and their potential impacts on surgical outcomes. J Biomed Res. 2019;34(4):271–280. doi:10.7555/JBR.33.20190054
22. Cremeans-Smith JK, Millington K, Sledjeski E, et al. Sleep disruptions mediate the relationship between early postoperative pain and later functioning following total knee replacement surgery. J Behav Med. 2006;29(2):215–222. doi:10.1007/s10865-005-9045-0
23. Sterniczuk R, Rusak B, Rockwood K. Sleep disturbance in older ICU patients. Clin Interv Aging. 2014;9:969–977. doi:10.2147/CIA.S59927
24. Chung F, Liao P, Elsaid H, et al. Factors associated with postoperative exacerbation of sleep-disordered breathing. Anesthesiology. 2014;120(2):299–311. doi:10.1097/ALN.0000000000000041
25. Raymond I, Ancoli-Israel S. Sleep disturbances, pain and analgesia in adults hospitalized for burn injuries. Sleep Med. 2004;5(6):551–559. doi:10.1016/j.sleep.2004.07.007
26. Amaral FGD, C-N J. A brief review about melatonin, a pineal hormone. Arch Endocrinol Metab. 2018;62(4):472–479. doi:10.20945/2359-3997000000066
27. Boguszewska A, Pasternak K. Melatonina i jej biologiczne znaczenie [Melatonin and its biological significance]. Pol Merkur Lekarski. 2004;17(101):523–527. Polish.
28. Gögenur I, Middleton B, Burgdorf S, et al. Impact of sleep and circadian disturbances in urinary 6-sulphatoxymelatonin levels, on cognitive function after major surgery. J Pineal Res. 2007;43(2):179–184. doi:10.1111/j.1600-079X.2007.00460.x
29. Reber A, Huber PR, Ummenhofer W, et al. General anaesthesia for surgery can influence circulating melatonin during daylight hours. Acta Anaesthesiol Scand. 1998;42(9):1050–1056. doi:10.1111/j.1399-6576.1998.tb05375.x
30. Ding F, Wang X, Zhang L, et al. Effect of propofol-based total intravenous anaesthesia on postoperative cognitive function and sleep quality in elderly patients. Int J Clin Pract. 2021;75(7):e14266. doi:10.1111/ijcp.14266
31. Gögenur I. Postoperative circadian disturbances. Dan Med Bull. 2010;57(12):B4205.
32. Fatemeh G, Sajjad M, Niloufar R, et al. Effect of melatonin supplementation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. J Neurol. 2022;269(1):205–216. doi:10.1007/s00415-020-10381-w
33. Brainard J, Gobel M, Bartels K, et al. Circadian rhythms in anesthesia and critical care medicine: potential importance of circadian disruptions. Semin Cardiothorac Vasc Anesth. 2015;19(1):49–60. doi:10.1177/1089253214553066
34. Leung JM, Sands LP, Newman S, et al. Preoperative sleep disruption and postoperative delirium. J Clin Sleep Med. 2015;11(8):907–913. doi:10.5664/jcsm.4944
35. Yoshitaka S, Egi M, Morimatsu H, et al. Perioperative plasma melatonin concentration in postoperative critically ill patients: its association with delirium. J Crit Care. 2013;28(3):236–242. doi:10.1016/j.jcrc.2012.11.004
36. Fan Y, Yuan L, Ji M, et al. The effect of melatonin on early postoperative cognitive decline in elderly patients undergoing Hip arthroplasty: a randomized controlled trial. J Clin Anesth. 2017;39:77–81. doi:10.1016/j.jclinane.2017.03.023
37. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7(3):e1000251. doi:10.1371/journal.pmed.1000251
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


