Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
The impact of exposure to biomass smoke versus cigarette smoke on inflammatory markers and pulmonary function parameters in patients with chronic respiratory failure
Authors Ocakli B , Acarturk E , Aksoy E , Gungor S , Ciyiltepe F , Oztas S, Ozmen I , Agca MC , Salturk C, Adiguzel N, Karakurt Z
Received 16 January 2018
Accepted for publication 4 March 2018
Published 18 April 2018 Volume 2018:13 Pages 1261—1267
DOI https://doi.org/10.2147/COPD.S162658
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Birsen Ocakli, Eylem Acarturk, Emine Aksoy, Sinem Gungor, Fulya Ciyiltepe, Selahattin Oztas, Ipek Ozmen, Meltem Coban Agca, Cuneyt Salturk, Nalan Adiguzel, Zuhal Karakurt
Department of Chest Diseases, Sureyyapasa Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul, Turkey
Purpose: The aim of this study was to evaluate the impact of exposure to biomass smoke vs cigarette smoke on serum inflammatory markers and pulmonary function parameters in patients with chronic respiratory failure (CRF).
Patients and methods: A total of 106 patients with CRF divided into age and gender-matched groups of cigarette-smoke exposure (n=55, mean [SD] age: 71.0 [12.0] years, 92.7% were females) and biomass smoke exposure (n=51, mean [SD] age: 73.0 [11.0] years, 94.1% were females) were included in this retrospective study. Data on patient demographics (age and gender), inflammatory markers, including neutrophil-to-lymphocyte ratio, C-reactive protein, platelet/mean platelet volume ratio, arterial blood gas analysis, and pulmonary function test findings, including forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC were obtained from medical records.
Results: Carbon dioxide partial pressure levels were significantly higher in the biomass smoke exposure than in the cigarette smoke exposure group (mean [SD] 51.0 [8.0] vs 47.0 [8.0] mmHg, p=0.026, respectively). Spirometry revealed similarly low levels for FEV1 (%) (38.0 [16.0] vs 40.0 [12.0]%) and FVC (%) (45.0 [19.0] vs 39.0 [19.0]%) in cigarette-smoke and biomass smoke exposure groups, whereas biomass smoke exposure was associated with significantly higher FEV1/FVC (75.0 [14.0] vs 58.0 [12.0]%, p=0.001), lower FVC (mL) (mean [SD] 744.0 [410.0] vs 1,063.0 [592.0] mL, p=0.035) and lower percentage of patients with FEV1/FVC <70% (36.8% vs 82.0%, p<0.001) than cigarette smoke exposure.
Conclusion: Our findings indicate similarly increased inflammatory markers and abnormally low pulmonary function test findings in both biomass smoke exposure and cigarette smoke exposure groups, emphasizing the adverse effects of biomass smoke exposure on lungs to be as significant as cigarette smoke exposure. Association of biomass smoke exposure with higher likelihood of FEV1/FVC ratio of >70% and more prominent loss of vital capacity than cigarette smoke exposure seems to indicate the likelihood of at least 18 years of biomass exposure to be sufficiently high to be responsible for both obstructive and restrictive pulmonary diseases.
Keywords: biomass exposure, cigarette smoke, inflammatory markers, spirometry, chronic respiratory failure
Introduction
Biomass fuels refer to any plant (eg, wood) or animal-based material (eg, dung and crop residues) deliberately burned by humans as their main source of domestic energy for cooking, home heating, and lightening.1–3 Among >200 different compounds in the biomass smoke, carbon monoxide, nitrous dioxides, sulfur oxides, formaldehyde, and polycyclic organic matter are considered to be the most hazardous ones.1,4–6
Accordingly, the combustion of biomass fuels has now been recognized as a relevant risk factor for respiratory disorders, such as chronic bronchitis and COPD, asthma, lung cancer, lung fibrosis, and tuberculosis.1–4
Being a cheaper and more attractive alternative to electricity and liquid petroleum gas, use of biomass fuels is a prevalent and a well-recognized cause of respiratory diseases, especially in developing countries.2,7,8 However, increasing trend toward use of indoor wood fires as a more “natural” alternative to electrical and gas heating and a more flavored option during cooking processes (eg, wood-fired pizza, smoked meats, and barbecues) is considered to increase the prevalence of biomass smoke exposure also in developed countries.8–10
More than 2,000,000 people worldwide, particularly in countries, such as China, India, and sub-Saharan Africa, rely on biomass fuels to supply their household energy needs.4,7 In many rural areas of Turkey, biomass fuels are widely used for heating and cooking, such as burning wood, dung, and crop residues in traditional fireplaces.11–13 Recent studies from rural areas in Turkey support the contributory role of exposure to biomass smoke in the development of chronic bronchitis and chronic airway obstruction in nonsmoking women.11–14
C-reactive protein (CRP) is a marker of inflammation and the acute-phase response,15 while platelet (PLT) count and mean platelet volume (MPV) are inflammatory markers reported to be associated with disease activity and efficacy of anti-inflammatory treatment in several chronic inflammatory disorders.16 Neutrophil-to-lymphocyte ratio (NLR) is considered to be a potential inflammatory marker in respiratory diseases as it is associated with severity and prognosis17,18 and correlates positively with serum CRP levels and negatively with MPV in patients with COPD.19
Previous studies have revealed differences between exposure to biomass smoke and cigarette smoke in terms of distribution of COPD phenotypes20–23 and type of systemic inflammatory response.24,25 However, limited data are available on comparison of biomass smoke- and cigarette smoke-induced pulmonary and inflammatory changes alongside inconsistent findings on the impact of acute biomass smoke exposure in healthy volunteers.26–29
This study was, therefore, designed to retrospectively evaluate the impact of exposure to biomass smoke vs cigarette smoke on serum inflammatory markers (NLR, CRP, MPV, and PLT/MPV ratio) and pulmonary function parameters in patients with chronic respiratory failure (CRF).
Patients and methods
Study population
A total of 106 patients with CRF were included in this retrospective study conducted in a respiratory intensive care clinic between 2014 and 2015. Patients were divided into 2 age and gender-matched groups, including cigarette smoke exposure (n=55, mean [SD] age: 71.0 [12.0] years, 92.7% were females) and biomass smoke exposure (n=51, mean [SD] age: 73.0 [11.0] years, 94.1% were females) groups. All patients in the biomass exposure group were non-smokers, with no exposure to cigarette smoke, while no biomass exposure was evident among patients in the cigarette smoke exposure group. Patients with lung cancer, rheumatic disease, collagen vascular disease, exposure to both biomass and tobacco smoke, and unknown history of biomass exposure were excluded from the study.
The study protocol was approved by the ethics committee (EC) of University of Health Sciences Sureyyapasa Chest Diseases and Thoracic Surgery Training and Research Hospital (date of approval/No: 24.05.2017/004). The study was conducted in full accordance with local Good Clinical Practice guideline and current legislations. Written informed consent was not obtained from the patients for the use of medical data for publication purposes since it was waived by the institution’s EC due to the retrospective nature of the study in line with the local legislations; and the patients’ ID information was strictly protected from the third parties.
Assessments
Data on patient demographics (age and gender), body mass index (BMI; kg/m2), hemogram (white blood cells [109/L], hematocrit [%], PLT [109/L], MPV [fL]), blood biochemistry (blood glucose [mg/dL], blood urea nitrogen [BUN; mg/dL], creatinine [mg/dL]), inflammatory markers (NLR, CRP, and PLT/MPV ratio), arterial blood gas (ABG) analysis (pH, partial pressure of carbon dioxide (PaCO2) [mmHg], partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) [mmHg], HCO3 [mmol] and oxygen saturation [SaO2, %]) and pulmonary function test (PFT, spirometry) findings within the past year, including forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC) and FEV1/FVC were obtained from medical records, and compared between biomass smoke and cigarette smoke exposure groups.
Years of exposure to biomass smoke was recorded based on exposure to fuel fumes for heating and cooking purposes (animal dung, wood, charcoal, and dried plant).
Amount of exposure to cigarette smoke was recorded based on smoking in pack/year.
Statistical analysis
Statistical analysis was made using IBM SPSS Statistics for Windows 2012 (version 22.0, IBM Corp., Armonk, NY, USA). Chi-square (χ2) test was used for the comparison of categorical data, while numerical data were analyzed using Students’ t-test for variables with normal distribution and with Mann–Whitney U for non-normally distributed variables. Data were expressed as “mean (SD)”, median (25–75 percentile), and percentage (%) where appropriate. p<0.05 was considered statistically significant.
Results
Patient characteristics
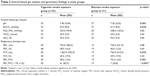
Both cigarette and biomass smoke exposure groups were homogenous in terms of age (mean [SD] 71.0 [12.0] vs 73.0 [11.0] years, respectively) and gender (92.7% vs 94.1%, respectively, were females) (Table 1).
Amount of cigarette consumption was median (25–75 percentile) 45.0 (30–50) package/year in the cigarette-smoke exposure group, while exposure to biomass-smoke was 18.0 (10.0–20.0) years in the biomass-smoke exposure group (Table 1).
Biomass fuels were used for the purpose of heating by 94.1% of patients and for cooking by 60.8% (Table 1).
Inflammatory markers
Cigarette smoke vs biomass smoke exposure groups were similar in terms of inflammatory markers, including PLT/MPV (mean [SD] 31.0 [10.0] vs 29.0 [11.0], p=0.41), CRP (median, min-max 7.3 [3.3–12.5] vs 8.7 [3.0–15.0] mg/L, p=0.46), and NLR (mean [SD] 3.5 [1.5] vs 3.4 [1.5], p=0.65; Table 1).
ABG analysis
Biomass smoke exposure was associated with significantly higher values for PaCO2 (mean [SD] 51.0 [8.0] vs 47.0 [8.0] mmHg, p=0.026) than cigarette smoke exposure (Table 2).
Other findings on ABG analysis were similar between groups, including PaO2/FiO2 (333.0 [99.0] and 338.0 [103.0] mmHg), HCO3 (30.0 [5.0] and 29.0 [4.0] mmol), and SaO2 (92.0 [5.0]% for each) (Table 2).
Spirometry findings
Spirometry revealed similarly low values of FEV1 (mean [SD] 38.0 [16] vs 40.0 [12.0]%) and FVC (45.0 [19.0] vs 39.0 [19.0]%), whereas biomass smoke exposure was associated with significantly higher FEV1/FVC (75.0 [14.0] vs 58.0 [12.0]%, p=0.001) and lower FVC (mL) (mean [SD] 744.0 [410.0] vs 1,063.0 [592.0] mL, p=0.035) than cigarette smoke exposure (Table 2).
Percentage of patients with FEV1/FVC <70% was significantly higher in cigarette smoke exposure than in biomass smoke exposure group (82.0% vs 36.8%, p<0.001).
Discussion
Our findings in a retrospective cohort of CRF patients with age and gender-matched groups of biomass smoke (for median 18.0 years) vs cigarette smoke (for median 45.0 package/year) exposure revealed similarly high serum levels of inflammatory markers and lower than normal spirometry findings in both groups. Biomass smoke exposure was associated with significantly higher values for PaCO2 and FEV1/FVC, lower FVC (mL) and less common identification of FEV1/FVC <70% compared with cigarette smoke exposure.
Abnormal PFT findings in our cohort, regardless of the type of smoke exposure, seem consistent with similarity of biomass fuels (300–5,000 μg/m3) and cigarettes (704 μg/m3) in terms of profile of average daily particulate matter (PM) production,2 exceeding the daily PM exposure threshold (50 μg/m3) stated in World Health Organization air quality guidelines.30
Although cigarette smoke exposure is the primary risk factor for development of COPD, biomass smoke exposure has been considered to be an additional risk factor for the development of COPD, leading to reduction in all lung function parameters (FEV1, FVC, and FEV1/FVC), similar to that observed in cigarette smoke exposure.31
In a past study among Turkish women with >17 years of biomass exposure, spirometry findings were reported to be consistent with obstructive pathology (FEV1/FVC <70%) in 19.1% of women, with small airway disease (FEF 25–75 <60%) in 23.4% and with restrictive pathology (FEV1/FVC >70%, FVC <80) in 17.3% of women.32 As calculated, based on daily and weekly exposure and years of exposure, biomass exposure index was shown to be negatively correlated with FVC and higher in females with pathological than normal PFT results, with a cutoff value of 34.7 for the existence of small airway disease, 42.7 for obstructive and 45.3 for restrictive pathology.32
In our cohort of patients with CRF, biomass exposure was associated with abnormally low average FEV1 (40.0%) and FVC (39.0%) values, while the average FEV1/FVC ratio was 75.0%. Accordingly, given the confirmed diagnosis of CRF in our cohort of patients after a median 18 years of biomass exposure, lower than normal FEV1 and FVC values in all patients and identification of FEV1/FVC <70% in 38% of patients with biomass exposure seem to indicate the likelihood of both obstructive and restrictive pathology in case of long-term biomass smoke exposure.
Although the current literature indicate that >20 years of biomass exposure is needed for the risk of developing obstructive airway disease,20,33,34 our findings emphasize the quantity and intensity of biomass exposure (median 18 years) in our cohort of patients with CRF to be sufficiently high to induce the appearance of both obstructive and restrictive lung disease.
The exact chemical composition of biomass smoke is considered to be dependent upon the fuel type, the temperature of burning, use of an open fire or incinerator, and local conditions.2 Studies from rural areas of Turkey revealed that heating and domestic cooking with biomass fuel via burning wood, dung, and crop residues in traditional fireplaces located in a small room resulted in an intensive exposure of household members to biomass fuel smoke and particles.11–13 Hence, our findings support the likelihood of exposure to more concentrated smoke because of the poor indoor ventilation conditions to accelerate the appearance of pathological PFT findings in Turkish women with biomass exposure.13,32
Given that obstructive lung disease was the main pathology in CRF patients who were exposed to cigarette smoke (FEV1/FVC <70 in 82%) in our cohort, our findings emphasize that respiratory impact of biomass and cigarette smoke exposures in patients with CRF differs in terms of likelihood of restrictive pattern of PFT abnormality in addition to obstructive pathology in patients with biomass smoke exposure.
In fact, biomass smoke-induced COPD per se was also reported to be distinct from cigarette smoke-induced COPD in terms of slower decline of FEV1, a different distribution of phenotypes,20–23 higher pigment deposition and fibrosis in lungs and thicker pulmonary arterial intima and reduced emphysema.35 This seems consistent with higher rates of hypercapnia with biomass smoke than cigarette smoke in our cohort.
A restrictive pattern in biomass exposure was also confirmed in past studies from Turkey based on radio-imaging findings consistent with restrictive pathology and histopathological findings, such as septal enlargements, goblet cell metaplasia, glandular hyperplasia, and fibrosis demonstrated in patients who were exposed to biomass smoke.36–38
The source of energy was also suggested to be associated with likelihood of restrictive pathology, with higher likelihood of burning organic material (animal waste) to induce chemical reactions responsible for restrictive lung disease.32 Besides, FVC is considered to be the PFT parameter that is particularly affected by indoor air pollution due to domestic cooking with biomass fuel.39 Use of biomass fuels for cooking by 60% of patients in the biomass smoke exposure group in our cohort seems notable in this regard, given that organic wastes (eg, dry animal dung) rather than wood or charcoal has been used as a primary fuel source in rural areas of Turkey.32
Nonetheless, it should be noted that unlike to homogenous distribution of cigarette smoke, biomass exposure is considered to exhibit a more heterogeneous distribution.32 Thus, calculation of biomass exposure based on an index with inclusion of hours per day, days per week, and total years is considered to reveal higher values that provide for greater probability of altered PFT results.12,32,40
Serum levels of inflammatory markers did not differ with respect to cigarette smoke vs biomass smoke exposure in our patients with CRF. Similarly, in a past study, comparing the inflammatory profile in biomass smoke vs cigarette smoke-exposed patients with COPD who were matched for gender, age, and FEV1, both biomass smoke and cigarette smoke exposure were found to be associated with high levels of systemic inflammation biomarkers.24 Nonetheless, differences in the type of systemic inflammatory response were reported between biomass smoke and cigarette smoke exposure with higher interleukin (IL)-6, IL-8, and IL-5 in cigarette smoke exposure24,25 and higher IL-4-producing T helper cells (Th2) in case of biomass exposure.25
Serum levels of inflammatory markers (NLR, CRP, MPV, and PLT/MPV ratio) in the biomass exposure group of CRF patients in our cohort support the consideration of biomass smoke exposure either from the combustion of wood or animal dung to be pro-inflammatory.2,35,41–45 Altered gene expression and synergistic interaction between biomass smoke components and other pro-inflammatory agents have also been suggested to play a role in biomass smoke-induced COPD.2,35,46
Moreover, in animal models of biomass exposure, sub-chronic exposure to wood smoke was reported to be associated primarily with eosinophilic inflammation and destruction of alveoli tissue, whereas predominant increase was noted in neutrophil and macrophage chemokine with sub-chronic exposure to cow dung.47
Notably, studies in otherwise healthy volunteers revealed inconsistent findings regarding pro-inflammatory effects of acute biomass smoke exposure.27–29,48 Peripheral and lung neutrophilia27 with variable T cell proliferation and cytokine production28 as well as reduced levels of inflammatory cells and mediators in bronchoalveolar lavage48 were reported after 1–6 hours of exposure to wood smoke (up to 500 μg/m3). Additionally, 1-week exposure to wood smoke (0.41 mg/m3) was reported to be not associated with alterations related to inflammatory markers (serum CRP, IL6, IL8, and tumor necrosis factor).29
Accordingly, our findings indicate that exposure to biomass adversely affects the lungs at least as much as cigarette smoking,35 alongside a more remarkable vital capacity loss. This supports that while cigarette smoking is the main risk factor for COPD in developed countries,8 indoor air pollution associated with biomass burning is also a significant risk factor in developing countries, not only for obstructive but also for restrictive lung diseases. This seems notable given that mainly women, and also young children accompanying their mothers, are considered to be the at-risk population for biomass exposure during cooking and other household activities.1
It should also be noted that cigarette or biomass smoke may induce not only inflammatory markers but also innate immunity regulators, such as G-protein-coupled receptor 15 (GPR-15), and the altered expression and epigenetic regulation of GPR-15 has been suggested to have a significant role in the health impact of smoking and biomass exposure.49–52
Certain limitations to this study should be considered. First, due to retrospective single-center design of the present study, establishing the temporality between cause and effect as well as generalizing our findings to overall diabetic population seems difficult. Second, the inability to perform more precise calculation of the cumulative exposure to biomass smoke as well as to assess serum levels of inflammatory cytokines, such as ILs, due to retrospective nature of the study is another limitation, which otherwise would extend the knowledge achieved in the current study. Nevertheless, despite these limitations, given the limited data available on direct comparison of the impact of biomass smoke vs cigarette smoke exposure on respiratory functions, our findings represent a valuable contribution to the literature.
Conclusion
Our findings in a retrospective cohort of CRF patients indicate similarly increased inflammatory markers and abnormally low PFT findings in both biomass smoke exposure and cigarette smoke exposure groups, emphasizing the adverse effects of biomass smoke exposure on lungs to be as significant as cigarette smoke exposure. Association of biomass smoke exposure with higher likelihood of FEV1/FVC ratio of >70% and more prominent loss of vital capacity than cigarette smoke exposure seems to indicate the likelihood of at least 18 years of biomass exposure to be sufficiently high to be responsible for causing both obstructive and restrictive pulmonary diseases. Accordingly, implementation of awareness-increasing measures and education of populations at risk for biomass exposure, such as women and children living in rural areas of developing countries, seem crucial to prevent this important public health problem.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization Protection of the Human Environment. The Health Effects of Indoor Air Pollution Exposure in Developing Countries. Geneva, 2002. | ||
Capistrano SJ, van Reyk D, Chen H, Oliver BG. Evidence of biomass smoke exposure as a causative factor for the development of COPD. Toxics. 2017;5(4):pii:E36. | ||
Babalik A, Bakirci N, Taylan M, et al. Biomass smoke exposure as a serious health hazard for women. Tuberk Toraks. 2013;61:115–121. | ||
Viegi G, Simoni M, Scognamiglio A, et al. Indoor air pollution and airway disease. Int J Tuberc Lung Dis. 2004;8:1401–1415. | ||
Gordon SB, Bruce NG, Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2:823–860. | ||
Naeher LP, Brauer M, Lipsett M, et al. Woodsmoke health effects: a review. Inhal Toxicol. 2007;19:67–106. | ||
Trevor J, Antony V, Jindal SK. The effect of biomass fuel exposure on the prevalence of asthma in adults in India – review of current evidence. J Asthma. 2014;51:136–141. | ||
Salvi S, Barnes PJ. Is exposure to biomass smoke the biggest risk factor for COPD globally? Chest. 2010;138:3–6. | ||
Reisen F, Brown SK. Australian firefighters’ exposure to air toxics during bushfire burns of autumn 2005 and 2006. Environ Int. 2009;35:342–352. | ||
Orozco-Levi M, García Aymerich J, Villar J, Ramírez-Sarmiento A, Antó JM, Gea J. Wood smoke exposure and risk of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:542–546. | ||
Baris YI, Hoskins JA, Seyfikli Z, Demir A. Biomass lung: primitive biomass combustion and lung disease. Indoor Built Environ. 2002;11:351–358. | ||
Ekici A, Ekici M, Kurtipek E, et al. Obstructive airway diseases in women exposed to biomass smoke. Environ Res. 2005;99:93–98. | ||
Torun T, Gungor G, Ozmen I, Maden E, Bolukbasi Y, Tahaoglu K. Bronchial anthracostenosis in patients exposed to biomass smoke. Turkish Resp J. 2007;8:48–51. | ||
Ozbay B, Uzun K, Arslan H, Zehir I. Functional and radiological impairment in women highly exposed to indoor biomass fuels. Respirology. 2001;6:255–258. | ||
Di Napoli M, Elkind MS, Godoy DA, et al. Role of C-reactive protein in cerebrovascular disease: a critical review. Expert Rev Cardiovasc Ther. 2011;9:1565–1584. | ||
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17:47–58. | ||
Lee JH, Song S, Yoon SY, Lim CS, Song JW, Kim HS. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as diagnostic markers for pneumonia severity. Br J Biomed Sci. 2016;73:140–142. | ||
Acartürk Tunçay E, Karakurt Z, Aksoy E, et al. Eosinophilic and non-eosinophilic COPD patients with chronic respiratory failure: neutrophil-to-lymphocyte ratio as an exacerbation marker. Int J Chron Obstruct Pulmon Dis. 2017;12:3361–3370. | ||
Günay E, Sarinç Ulaşli S, Akar O, et al. Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. Inflammation. 2014;37:374–380. | ||
Ramírez-Venegas A, Sansores RH, Quintana-Carrillo RH, et al. FEV1decline in patients with chronic obstructive pulmonary disease associated with biomass exposure. Am J Respir Crit Care Med. 2014;190:996–1002. | ||
Camp PG, Ramírez-Venegas A, Sansores RH, et al. COPD phenotypes in biomass smoke- versus tobacco smoke-exposed Mexican women. Eur Respir J. 2014;43:725–734. | ||
Golpe R, Sanjuán-López P, Cano-Jiménez E, Castro-Añón O, Pérez-de-Llano LA. Distribution of clinical phenotypes in patients with chronic obstructive pulmonary disease caused by biomass and tobacco smoke. Arch Bronconeumol. 2014;50:318–324. | ||
Golpe R, Martín-Robles I, Sanjuán-López P, et al. Prevalence of major comorbidities in chronic obstructive pulmonary disease caused by biomass smoke or tobacco. Respiration. 2017;94:38–44. | ||
Golpe R, Martín-Robles I, Sanjuán-López P, et al. Differences in systemic inflammation between cigarette and biomass smoke-induced COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2639–2646. | ||
Solleiro-Villavicencio H, Quintana-Carrillo R, Falfán-Valencia R, Vargas-Rojas MI. Chronic obstructive pulmonary disease induced by exposure to biomass smoke is associated with a Th2 cytokine production profile. Clin Immunol. 2015;161:150–155. | ||
Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109. | ||
Ghio AJ, Soukup JM, Case M, et al. Exposure to wood smoke particles produces inflammation in healthy volunteers. Occup Environ Med. 2012;69:170–175. | ||
Burchiel SW, Lauer FT, MacKenzie D, et al. Changes in HPBMC markers of immune function following controlled short-term inhalation exposures of humans to hardwood smoke. Inhal Toxicol. 2016;28:61–70. | ||
Jensen A, Karottki DG, Christensen JM, et al. Biomarkers of oxidative stress and inflammation after wood smoke exposure in a reconstructed viking age house. Environ Mol Mutagen. 2014;55:652–661. | ||
World Health Organization. Joint United Nations Programme on HIV/AIDS. Air Quality Guidelines: Global Update 2005. Geneva, Switzerland: World Health Organization; 2006. | ||
Montaño M, Cisneros J, Ramírez-Venegas A, et al. Malondialdehyde and superoxide dismutase correlate with FEV(1) in patients with COPD associated with wood smoke exposure and tobacco smoking. Inhal Toxicol. 2010;22:868–874. | ||
Balcan B, Akan S, Ugurlu AO, Handemir BO, Ceyhan BB, Ozkaya S. Effects of biomass smoke on pulmonary functions: a case control study. Int J Chron Obstruct Pulmon Dis. 2016;11:1615–1622. | ||
Regalado J, Pérez-Padilla R, Sansores R, et al. The effect of biomass burning on respiratory symptoms and lung function in rural Mexican women. Am J Respir Crit Care Med. 2006;174:901–905. | ||
Døssing M, Khan J, al-Rabiah F. Risk factors for chronic obstructive lung disease in Saudi Arabia. Respir Med. 1994;88:519–522. | ||
Rivera RM, Cosio MG, Ghezzo H, Salazar M, Pérez-Padilla R. Comparison of lung morphology in COPD secondary to cigarette and biomass smoke. Int J Tuberc Lung Dis. 2008;12:972–977. | ||
Kara M, Bulut S, Tas F, Akkurt I, Seyfikli Z. Evaluation of pulmonary changes due to biomass fuels using high-resolution computed tomography. Eur Radiol. 2003;13:2372–2377. | ||
Arslan M, Akkurt I, Egilmez H, Atalar M, Salk I. Biomass exposure and the high resolution computed tomographic and spirometric findings. Eur J Radiol. 2004;52:192–199. | ||
Mena MA, Woll F, Cok J, Ferrufino JC, Accinelli RA. Histopathological lung changes in children due to biomass fuel. Am J Respir Crit Care Med. 2012;185:687–688. | ||
Behera D, Jindal SK, Malhotra HS. Ventilatory function in nonsmoking rural Indian women using different cooking fuels. Respiration. 1994;61:89–92. | ||
Pérez-Padilla R, Regalado J, Vedal S, et al. Exposure to biomass smoke and chronic airway disease in Mexican women. A case-control study. Am J Respir Crit Care Med. 1996;154:701–706. | ||
Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, Ran P. Risk of COPD from exposure to biomass smoke: a metaanalysis. Chest. 2010;138:20–31. | ||
Balmes JR. When smoke gets in your lungs. Proc Am Thorac Soc. 2010;7:98–101. | ||
Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: a systematic review and meta-analysis. Bull World Health Organ. 2008;86:390–398. | ||
Venkataraman C, Rao GU. Emission factors of carbon monoxide and size-resolved aerosols from biofuel combustion. Environ Sci Technol. 2001;35:2100–2107. | ||
Togo S, Holz O, Liu X, et al. Lung fibroblast repair functions in patients with chronic obstructive pulmonary disease are altered by multiple mechanisms. Am J Respir Crit Care Med. 2008;178:248–260. | ||
Perez-Padilla R, Schilmann A, Riojas-Rodriguez H. Respiratory health effects of indoor air pollution. Int J Tuberc Lung Dis. 2010;14:1079–1086. | ||
Sussan TE, Ingole V, Kim JH, et al. Source of biomass cooking fuel determines pulmonary response to household air pollution. Am J Respir Cell Mol Biol. 2014;50:538–548. | ||
Muala A, Rankin G, Sehlstedt M, et al. Acute exposure to wood smoke from incomplete combustion–indications of cytotoxicity. Part Fibre Toxicol. 2015;12:33. | ||
Kõks G, Uudelepp ML, Limbach M, Peterson P, Reimann E, Kõks S. Smoking-induced expression of the GPR15 gene indicates its potential role in chronic inflammatory pathologies. Am J Pathol. 2015;185:2898–2906. | ||
Kõks S, Kõks G. Activation of GPR15 and its involvement in the biological effects of smoking. Exp Biol Med (Maywood). 2017;242:1207–1212. | ||
Olloquequi J, Silva OR. Biomass smoke as a risk factor for chronic obstructive pulmonary disease: effects on innate immunity. Innate Immun. 2016;22:373–381. | ||
Lee A, Kinney P, Chillrud S, Jack D. A systematic review of innate immunomodulatory effects of household air pollution secondary to the burning of biomass fuels. Ann Glob Health. 2015;81:368–374. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.