Back to Journals » International Journal of General Medicine » Volume 15
The Impact of COVID-19 on the Acute Stroke Care Pathway: Looking Beyond the Short Term
Authors Zhong M, Xiong H, Zhang K, Fu S
Received 15 December 2021
Accepted for publication 4 March 2022
Published 17 March 2022 Volume 2022:15 Pages 3069—3075
DOI https://doi.org/10.2147/IJGM.S349356
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mengqiu Zhong,* Hanlin Xiong,* Kebiao Zhang, Shimin Fu
Department of Emergency, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kebiao Zhang; Shimin Fu, Email [email protected]; [email protected]
Background: Early in the pandemic, coronavirus disease 2019 (COVID-19) had been reported with significant impact on the stroke care pathway. Meanwhile, the mid/long-term consequence of treatment efficiency and effectiveness of the acute stroke pathway still remains unknown.
Methods: A comprehensive retrospective analysis was conducted on the acute stroke care pathway parameters in a stroke unit in Chongqing, Southwest China. A total of 1492 patients were involved in this study, of whom 634 patients (42.5%) were included during the COVID-19 pandemic, 858 patients (57.5%) included during the similar period of 2019. We collected demographic and clinical characteristics, clinical outcome as the treatment efficiency and effectiveness indicators of the acute stroke pathway.
Results: Compared to the same period in 2019, there were 2.8% fewer transient ischemic attack (TIA) patients, while 9.9% more acute ischemic stroke patients in 2020. In addition, patients had significantly higher National Institutes of Health Stroke Scale (NIHSS) scores (P = 0.002) and hospital mortality (P = 0.004) during the pandemic. The median door-CT time (P < 0.001) and emergency stay (P < 0.001) of acute stroke were also remarkably increased during the pandemic. The proportion of patients with intravenous thrombolysis (IVT) was significantly lower (P < 0.001), while the mechanical thrombectomy (MET) was remarkably higher (P = 0.042) in the pandemic group. Moreover, the IVT was significantly delayed during the pandemic (door-needle time: P = 0.001).
Conclusion: The COVID-19 outbreak did not reduce the willingness of the acute stroke patient to seek medical help. Benefited from adjustments of stroke procedure in response to the COVID-19 pandemic, no significant reduction was observed in the reperfusion success of the acute stroke care pathway. However, more medical resources need to be invested into the acute stroke care pathway to prevent serious consequences of undiagnosed and untreated strokes.
Keywords: COVID-19, acute stroke care pathway, intravenous thrombolysis, mechanical thrombectomy
Introduction
Coronavirus disease 2019 (COVID-19) has posed unprecedented challenges for global healthcare systems and has forced restructuring of health services and reallocation of resources in many places.1 The impact of the pandemic on the management of acute stroke may be inevitable, and growing evidence indicates an increasing prevalence of neurological involvement during viral infection (eg, in the form of stroke).2 Thus, most studies have focused on the relationship between COVID-19 and stroke.
In fact, the pandemic has also had a great impact on the treatment efficiency and effectiveness of acute stroke patients without COVID-19. Studies have reported remarkable delays in CT scanning and thrombolytic therapy for stroke patients during the pandemic.3,4 However, previous studies have focused on the early stages of the pandemic (home isolation stage). Since the pandemic has been going on for a long period of time (almost two years), the acute stroke protocol adapted to COVID-19 screening has also been regularly updated. The medium and long-term impact of COVID-19 on the acute stroke care pathway is still unknown.
This study seeks to perform a detailed analysis of the impact of COVID-19 on treatment efficiency and effectiveness of the acute stroke pathway in Chongqing, one year since the outbreak, using the same time period from 2019 for comparison. We focused on major time intervals, reperfusion therapies, admissions and patient outcomes.
Materials and Methods
Study Design and Patients
This study was approved by the institutional ethical review board of the First Affiliated Hospital of Chongqing Medical University (reference 2021–057, 24 February 2021), and completed the clinical trial registration (ChiCTR2100053382). The data in this study are anonymous, and therefore the requirement for informed consent was waived.
A comprehensive retrospective analysis was conducted on the acute stroke care pathway parameters in a stroke unit in Chongqing, Southwest China, from 23 January to 30 December 2020 (Wuhan was locked down on January 23, and after that many cities entered a state of alert) and the same period from 2019. In accordance with guidelines from the National Health Commission, all patients in the stroke center underwent screening for COVID-19, which included body temperature measurement, travel history, chest CT scanning, real-time reverse transcriptase-polymerase chain reaction (RT-PCR), complete blood count test and even multidisciplinary consultation. None of the patients included in this study were diagnosed with COVID-19. This is because that all suspected and confirmed COVID-19 patients were transferred to designated hospitals in accordance with the guidelines of the National Health Commission.5
The Stroke code team in our center was composed of five attending physicians, five residents, six technicians, eight nurses (four professional stroke nurses and four senior emergency nurses) and four three anesthetists. Before the pandemic, all suspected stroke patients received symptom and medical history assessment immediately by professional physician when arrived at the hospital, and then prioritize the blood routine and coagulation examination, imageological diagnosis (cerebral CT, CTA and CTP), while there was no dedicated CT unit. Therapeutic interventions (intravenous thrombolysis/angiographic) were performed after the thrombus was identified. Finally, patients were transferred to a common ward. During the pandemic, we established three adjustments for stroke procedure: 1) A dedicated CT unit was set up (March/April); 2) A progressive stroke unit was created (May/June). Stroke patients were transferred to a progressive unit ahead of COVID-19 nucleic acid result. 3) Increased manpower was allocated for abroad cases screening (September/October).
Baseline Characteristics and Outcomes
We collected demographics and outcome data for all patients included in the stroke unit. The demographics included age, gender, final diagnosis in the stroke unit and medical history. Outcome data included the time from onset to hospital door (onset-door), the time from door to CT (door-CT), the National Institutes of Health Stroke Scale (NIHSS) score, admission rate, hospital mortality, emergency stay and length of stay. In addition, more detailed analyses on the major time intervals, acute revascularization treatments [intravenous thrombolysis (IVT) and mechanical thrombectomy (MET)] and successful recanalization rate of ischemic stroke patients were performed. Successful recanalization was defined as an mTICI grade 2b or 3 (mTICI≧2b) assessed on angiography. Finally, we also performed a monthly trend graph of major time intervals and patient volume for ischemic stroke, which was compared to data in 2019 to assess potential seasonal variations.
Statistical Analysis
Categorical variables were reported as absolute numbers and percentages, and differences between proportions were assessed using the χ2 test or Fisher’s exact tests. The distribution of continuous variables was not normal, and therefore, differences in variables were assessed with the Mann–Whitney U-test. Multivariate logistic regression analysis was used to determine risk factors for hospital mortality. All analyses were two-tailed, and the significance level was considered by p < 0.05. Data analyses were performed using the Statistical Package for Social Science (SPSS) statistical package version 25.0.
Results
From January 23, 2019 to December 30, 2020, a total of 1492 patients were involved in the First Affiliated Hospital of Chongqing Medical University with a clinical diagnosis of acute stroke, of whom 634 patients (42.5%) were included during the COVID-19 pandemic. Compared to the same period in 2019, there were 2.8% fewer TIA patients (3.4% vs 0.6%, P < 0.001) but 9.9% more acute ischemic stroke patients (57.1% vs 67%, P < 0.001 in 2020). In addition, patients had significantly higher NIHSS scores during the pandemic (6 vs 8, P = 0.002). No marked differences were observed between groups concerning age, gender and medical history. Baseline patient characteristics are outlined in Table 1.
 |
Table 1 Demographics Characteristics of Included Patients |
In general, compared with the pre-pandemic group, the median door-CT time (20 vs 22 (min), p < 0.001), median emergency stay time (64.7 vs 90 (min), p < 0.001) and hospital mortality (16.7% vs 23.3%, P = 0.004) were significantly higher in the pandemic group. Only a slight variation in median onset-door time (120 vs 120, min, P = 0.148), median length of stay (13 vs 13, days, P = 0.698) and admission rate (85.0% vs 83.9%, P = 0.578) were observed between groups (Table 2).
 |
Table 2 Stroke Time Interval and Clinical Outcomes Before and During the Pandemic |
Similarly, more detailed analyses for ischemic stroke also found that the median door-CT time (19 vs 20 (min), p < 0.001) and emergency stay time (62 vs 91 (min), p < 0.001) significantly increased during the pandemic. In addition, the proportion of patients with IVT was significantly lower (29.8% vs 19.3%, P < 0.001) while with MET significantly higher (3.5% vs 6.4%, P = 0.042) in the pandemic group compared to the pre-pandemic group. Moreover, the door-needle time also increased during the pandemic (43 vs 52.5, P = 0.001). There were no significant variations in onset-door time, door-groin time, length of stay or reperfusion success rate between groups (Table 3). Furthermore, we performed logistic regression to clarify the hospital mortality risk factors. The following variables were investigated: age, pre-NIHSS revascularization treatments, COVID-19 pandemic and classification of stroke. We found that age (OR: 1.017, 95% CI: 1.001–1.033), pre-NIHSS (OR: 1.154, 95% CI: 1.123–1.185) and COVID-19 pandemic (OR: 1.670, 95% CI: 1.107–2.519) were independently associated with a greater risk of hospital mortality (Table 4).
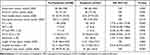 |
Table 3 Stroke Time Interval and Clinical Outcomes Before and During the Pandemic (Ischemic Stroke) |
 |
Table 4 Multivariable Logistic Regression Analysis of Hospital Death Risk |
In general, the visual representation for ischemic stroke indicated a significant reduction in patients and a marked prolongation of door-CT and door-needle time due to the COVID-19 pandemic. However, monthly fluctuations in these data are similar to those in the pre-pandemic period, reflecting the seasonal variation of ischemic stroke. Emergency stays were also generally prolonged after the pandemic, showing three prolongation peaks (23 February to 22 March 2020, 23 April to 22 May 2020, and 23 August to 22 September 2020) (Figure 1).
Discussion
We evaluated the impact of COVID-19 on treatment efficiency and effectiveness of the acute stroke care pathway in a regional stroke center. Overall, the COVID-19 outbreak did not reduce the willingness of acute stroke patients to seek medical help, as there was no significant prolongation in the time from onset to hospital door, which is inconsistent with previous research.6 However, compared with pre-pandemic, patients who came to the hospital during the outbreak were more seriously ill. Similarly to a previous short-term study,4 we also found a remarkably increased baseline NIHSS score for acute stroke patients, a lower proportion of TIA patients, while a higher proportion of ischemic stroke patients during the pandemic. According to the results of logistic regression analysis, COVID-19 pandemic and baseline NIHSS score were independently associated with a greater risk of hospital mortality, which explains the higher hospital mortality observed during the pandemic. One of the reasons for this phenomenon may be that people were isolated at home, and some with chronic diseases (eg, atrial fibrillation and hypertension) did not take medication regularly or were followed up regularly. These chronic diseases played an important role in the development of acute stroke. Normally, primary healthcare services play an important role in the management of these chronic diseases, which include scheduled follow-up, health education and drug intervention. However, most of these primary healthcare resources were allocated to epidemic prevention during the pandemic. This would increase the incidence and severity of cerebrovascular diseases. As a previous study reported,7 we indeed need to increase publicity about the relationship between these chronic diseases and stroke through social media and encourage regular exercise at home.
The treatment efficiency of the acute stroke care pathway was indeed reduced to a certain extent after the outbreak. Thorough assistance for ischemic stroke patients with door-to-needle usually takes more than 50 min (43 min in 2019), which directly results in the delay of thrombolytic therapy, thus the proportion of patients with IVT was lower after the outbreak. In addition, the median emergency stay time was obviously prolonged, and the admission rate also significantly decreased. This could be attributed to the increased time required to perform personal protection measures during the COVID-19 pandemic, which led to delays in symptom identification, neurological assessment, communication, transport, imaging and treatments, ultimately prolonging the emergency stay. While these delays did not significantly affect the effectiveness of the acute stroke care pathway, and there were no significant variations in the reperfusion success rate or length of stay before and after the pandemic.
The overall visual representation for ischemic stroke reflected the impact of the pandemic, including a significant reduction in patient volume and marked delay in imaging and reperfusion therapy. While monthly trend representation of these data reflected the seasonal variation of ischemic stroke, it is worth noting that there were three emergency stay peaks, which were associated with changes during the pandemic. The first peak (2.23.2020–3.23.2020) reflected the increased pressure in the emergency department in the early days of the outbreak. All patients in the emergency department, regardless of etiology, underwent immediate screening for signs, symptoms, and risk factors for COVID-19 exposure before admission to the inpatient ward, prolonging the stay in the emergency unit. In response to this situation, we set up a dedicated CT unit for suspected stroke patients (Figure 1A). Consequently, the door-CT time and emergency stay of ischemic stroke patients were largely decreased in the next period of time. In April 2020, the closure of temporary treatment centers in two major hospitals (Huoshenshan hospital and Leishenshan hospital) in Wuhan marked the domestic epidemic being under effective control, and most cities across the country lifted the lockdown. With an increase in outpatients and emergency patients, the number of patients waiting for hospitalization kept rising, and the emergency stay of ischemic stroke was significantly prolonged again (4.23.2020–5.22.2020). We adapted quickly to the pandemic and created a progressive stroke unit (Figure 1B). Patients were transferred to a progressive unit ahead of COVID-19 nucleic acid result, thus reducing treatment delays and protecting patients and healthcare workers from potential exposures. Finally, the third emergency stay peak (8.23.2020–9.22.2020) was related to the increase in cases from abroad. To deal with this situation, we increased manpower for the screening of cases from abroad, and the further revised pandemic prevention efforts (Figure 1C).
Some limitations are still raised in this study. Firstly, our stroke center did not receive any COVID positive case during the epidemic period, we could not provide this part of data for readers to compare it with their experience. In addition, data on the patient’s mRS scores were unavailable, thus we evaluated the treatment effectiveness of the acute stroke care pathway by using TICI scores, it may affect the conclusion to some extent, more studies are needed in the future.
At present, the global COVID-19 pandemic is continuing, and the incidence is increasing. We should constantly optimize the acute stroke care pathway protocol according to current changes during the pandemic so as to provide complete medical assistance for acute stroke as quickly as possible, while implementing COVID-19 prevention measures.
Data Sharing Statement
As the data from this study are also part of a follow-up study, we could not share the original data immediately. We will share the data on the Clinical Trial Management Public Platform (www.medresman.org.cn) as soon as the study is completed. The data will be free for all to see, but the author’s consent ([email protected]) is required before it can be obtained.
Funding
Shimin Fu received a cultivation fund of the First Affiliated Hospital of Chongqing Medical University (grant number, PYJJ2019-10); Kebiao Zhang received funding from Chongqing Medical University, for the Emergency Specific Clinical Research Projects for COVID-19 (grant number, 20200704).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fauci AS, Lane HC, Redfield RR. Covid-19 - navigating the uncharted. N Engl J Med. 2020;382:1268–1269. doi:10.1056/NEJMe2002387
2. Vogrig A, Gigli GL, Bna C, Morassi M. Stroke in patients with covid-19: clinical and neuroimaging characteristics. Neurosci Lett. 2021;743:135564. doi:10.1016/j.neulet.2020.135564
3. Zini A, Romoli M, Gentile M, et al. The stroke mothership model survived during covid-19 era: an observational single-center study in emilia-romagna, Italy. Neurol Sci. 2020;41(12):3395–3399. doi:10.1007/s10072-020-04754-2
4. John S, Hussain SI, Piechowski-Jozwiak B, et al. Clinical characteristics and admission patterns of stroke patients during the covid 19 pandemic: a single center retrospective, observational study from the Abu Dhabi, United Arab Emirates. Clin Neurol Neurosurg. 2020;199:106227. doi:10.1016/j.clineuro.2020.106227
5. National Health Commission of the People s Republic of China. Protocol for diagnosis and treatment of COVID-19; 2020. Available from: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=0a7bdf12bd4b46e5bd28ca7f9a7f5e5a.
6. Teo K-C, Leung WCY, Wong Y-K, et al. Delays in stroke onset to hospital arrival time during covid-19. Stroke. 2020;51(7):2228–2231. doi:10.1161/strokeaha.120.030105
7. Hoyer C, Ebert A, Huttner HB, et al. Acute stroke in times of the covid-19 pandemic a multicenter study. Stroke. 2020;51:2224–2227. doi:10.1161/strokeaha.120.030395
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

