Back to Journals » Clinical Interventions in Aging » Volume 17
The Impact of COVID-19 on SARSCoV-2-Negative Elderly Patients with Hip Fractures: A Single-Center Retrospective Study from Shanghai, China
Authors Zhao J , Cai Q, Jiang D, Wang L, He H, Chen S , Jia W , Zhang C
Received 10 May 2022
Accepted for publication 22 June 2022
Published 1 July 2022 Volume 2022:17 Pages 991—999
DOI https://doi.org/10.2147/CIA.S374083
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Jinhui Zhao,1,2,* Qianying Cai,2,* Dajun Jiang,1,2 Lingtian Wang,1,2 Haiyan He,2 Shengbao Chen,2 Weitao Jia,1,2 Changqing Zhang1,2
1Department of Orthopedic Surgery, Shanghai Jiaotong University Affiliated Sixth People’s Hospital, Shanghai, 200233, People’s Republic of China; 2Shanghai Institute of Microsurgery on Extremities, and Department of Orthopedic Surgery, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai, 200233, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Weitao Jia; Changqing Zhang, Department of Orthopedic Surgery, Shanghai Jiaotong University Affiliated Sixth People’s Hospital, Shanghai, 200233, People’s Republic of China, Tel +86-18930173388 ; +86-21-64701361, Email [email protected]; [email protected]
Purpose: Coronavirus disease 2019 (COVID-19) has brought an unprecedented change in wellbeing globally. The spread of the pandemic reportedly reduced the incidence of activity-related trauma, while that of fragility fractures remained stable. Here, we aimed to identify the risk factors associated with the prognosis of SARS-CoV-2 negative elderly patients with hip fractures.
Patients and Methods: This retrospective study included elderly patients with hip fractures between 1st January and 9th May during the COVID-19 pandemic (Experiment group) and the same period from 2017 to 2019 (Control group). Perioperative mortality, complications, and functional recovery were compared between two groups of different time frame in the total cohort and patients who received surgical treatment. Multiple linear regression was carried out to identify the risk factors influencing the prognosis of COVID-negative elderly patients with hip fractures.
Results: The proportion of patients with admission time less than 24 hours and the 6-month postoperative Parker score were significantly decreased during COVID-19 compared with the pre-COVID-19 period (p < 0.001). Multiple linear regression demonstrated that TTA (defined as time from injury to admission), rehabilitation after discharge and outpatient follow-up were associated with the 6-month Parker score in the total population (p < 0.001) and in patients who received surgical treatment (p < 0.001).
Conclusion: Elderly patients with hip fractures had a poorer prognosis in epidemic period despite being COVID-19 negative. Factors including timely admission, postoperative follow-up, and rehabilitation could optimize safety and significantly improve the prognosis of elderly COVID-19 negative patients with hip fractures, even during a pandemic.
Keywords: COVID-19, COVID-negative, elderly hip fracture, Parker score
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in Wuhan, China, on Dec 31, 2019.1 Immediately after Wuhan imposed an unprecedented cordon sanitaire, Shanghai launched a first-level response mechanism on January 24 2020, with measures including traffic control, home self-isolation, and restricted access to the community. On March 11, 2020, the World Health Organization (WHO) declared a pandemic. The leading clinical symptoms are fever and cough, usually combined with the ground-glass opacity found via computed tomography (CT), and abnormality in blood routine examination was associated with the severe cases.2–4 As of June 10, 2022, there are over 530 million cumulative confirmed cases and over 6.3 million cumulative deaths worldwide, of which China has a cumulative total of over 3.2 million confirmed cases and over 18 thousand deaths. The outbreak of COVID-19 has brought changes to people’s physical and psychological wellbeing.5
Elderly hip fracture patients, especially those with underlying comorbidities such as hypertension, diabetes, chronic lung disease, and cardiovascular and cerebrovascular diseases, are particularly vulnerable to developing complications from COVID-19 infection.6,7 The spread of the pandemic was reported to reduce the incidence of activity-related trauma, while that of fragility fractures remained stable.8,9 Considering the unsatisfactory outcomes of hip fractures in the elderly,10,11 their treatment should be prioritized even during COVID-19. A meta-analysis has found that a delay to surgery of more than 48 hours increases mortality,12 and in recent years, studies have increasingly shown that elderly patients with hip fractures could benefit from earlier treatment within 24 h, 12 h, and even 6 h after radiographic diagnosis if the patient’s physical condition allows.13–17 While all aforementioned researches have focused on in-hospital delays, those occurring before hospital admission have been neglected.
COVID-19 has taken extensive public medical resources, affecting the emergency treatment of hip fractures in the elderly. During COVID-19, as a result of the lockdown policy, hip fractures in elderly patients exhibited changes in their incidence (including ratio of male to female incidence), type, severity, and patient age.5,18–20 More importantly, elderly patients with hip fractures may face a treatment delay due to lack of space in hospital, reduced access due to quarantine measures, and additional screening before admission. Usually, an operative delay is defined as an interval between the time of radiographic diagnosis and the operation. An additional delay from the injury to the hospital presentation (pre-hospital delay) is usually neglected but should be acknowledged.21 The influence of COVID-19 on elderly hip fracture patients infected with SARS-CoV-2 has been well studied.22–24 However, to our knowledge, research on elderly patients with hip fractures and without SARS-CoV-2 during the COVID-19 period is limited, but is important since it could enable planning of hip fracture treatment for elderly patients in future public health emergencies. Besides, the present study could also provide evidence of the relationship between some overlooked risk factors and the prognosis of elderly hip fractures. The aims of the present study were to analyze whether time from injury to admission (TTA) or time from diagnosis to surgery (TTS) increases 6-month mortality rates and affects postoperative functional recovery for elderly patients with hip fractures and to identify other potentially modifiable factors that affect prognosis in such patients diagnosed as COVID-19-negative.
Materials and Methods
Subject
This retrospective study included elderly patients with hip fractures (femoral neck fractures and intertrochanteric fractures) between 1st January and 9th May from 2017 to 2020 in Shanghai Sixth People’s Hospital, China. Patients in 2020 between 1st January and 9th May were recruited to the Experiment group, while those in 2017–2019 of the same periods were considered the Control group. The inclusion criteria were as follows: (i) participants aged ≥65 years old; (ii) confirmed diagnosis of a first hip fracture; (iii) COVID-19 negative during the study. The exclusion criteria were: (i) Multiple fractures; (ii) history of previous hip fracture; (iii) hip fractures caused by high-energy injury; (iv) pathological fracture. After admission, the operation was arranged as soon as possible if the patient’s physical condition permits. If the patient has surgical contraindications or refuses the operation for other reasons, traction or brace fixation and discharge conservative treatment. All participants were aware of the purpose of the study and provided signed informed consent. The study was reviewed by the ethics committee of Shanghai Sixth People’s Hospital (approval number: 2017–152) and registered with the China Clinical Trial Center (registration number: “ChiCTR-ONC-17,013,389”). The study protocol followed the principles of the Declaration of Helsinki (as revised in Brazil 2013).
Assays
Patient information, including demographic characteristics, imaging data, laboratory examinations, treatments, complications, outcomes, interviews and follow-up visits were all obtained from electronic medical records of the hospital information system. Baseline data collected from each patient included: TTA, TTS, pre-existing medical conditions, type of hip fracture, treatment methods. Follow-up data included: perioperative complications, mortality, postoperative complications, six-month mobility after discharge, postoperative rehabilitation site and follow-up way (outpatient follow-up or other). TTA was defined as the time in hours from injury to the admission, and TTS was defined as that from the radiographic diagnosis of the fracture until the start of the surgical procedure. TTA > 24 hours was defined as a pre-hospital delay (Admission delay), while TTS > 48 hours was considered as an in-hospital delay (Surgical delay). Surgical duration is defined as the time from the start of the skin incision to the end of the operation. The Parker Mobility Scale consists of three questions based on the sum of the mobility assessment in three different situations. Each question valued 0–3 points, the total score is between 0 and 9. All participants enrolled in the present study were free of COVID-19. The Parker mobility score25 was used to evaluate the prognosis of hip fractures in this cohort.
Statistical Analysis
Baseline data were compared between the Experiment and Control group. Continuous variables were expressed as means ± standard deviation, and categorical variables as percentages. The normality of continuous variables was tested to determine the statistical method used in further analysis. Baseline variables were tested between two groups using the independent samples t-test or Mann–Whitney test, and qualitative data were compared using the Pearson’s chi-squared test or Fisher’s exact test (when appropriate) for proportions. Multiple linear regression was performed to adjust the identified confounding factors (based on P-value from the univariate analysis, combined with clinical expertise and previous studies) and calculate the effect values (odds ratios (OR) or beta) with 95% confidence intervals (CI). Data analysis was performed using SPSS software (version 25) and SAS software (version 9.4). The p-values were two-sided, and a value <0.05 was considered statistically significant.
Results
A total of 1622 elderly patients with hip fractures were recruited during the study periods. Table 1 describes the demographics of the study groups. The number of elderly patients with hip fractures from 1st January to 9th May in 2020 was slightly higher than the average number from 1st January to 9th May in 2017–2019 (average of 397). The groups were similar in terms of age, sex, height, treatment type, fracture type, hypertension, diabetes, heart failure or hyperlipidemia on admission, perioperative pulmonary embolism or pneumonia, 6-month postoperative mortality and baseline Parker scores (p > 0.05). Admission was delayed for a higher proportion of patients during the COVID-19 period (Experiment group) than prior to this period (Control group). During the COVID-19 period, patients also had higher weight, higher incidence of perioperative deep venous thrombosis (DVT), lower 6-month Parker score post-fracture, lower rehabilitation hospital occupancy rate and outpatient follow-up rate (p < 0.001).
 |
Table 1 Comparison of Characteristics Between Patients Recruited During COVID-19 and in the Same Period of 2017–2019 Admitted to Hospital with a Diagnosis of Elderly Hip Fracture |
Table 2 presents demographics of patients who chose operative treatment. Compared with patients in the control group, patients in the COVID-19 period had longer surgery duration (p < 0.001), the proportion of TTA < 24 h and TTS < 48 h were significantly decreased (p < 0.001). Similar to the total population, patients who chose surgical treatment also showed differences in weight, incidence of perioperative DVT, 6-month postoperative Parker score, rehabilitation hospital occupancy rate and outpatient follow-up rate between Experiment and Control groups (p < 0.05).
 |
Table 2 Characteristics of Elderly Patients with Hip Fractures Who Received Operative Treatment Between Experiment and Control Group |
In the multiple linear regression model test for normality, a quantile-quantile plot showed a normal distribution of residuals (Figures 1 and 2). Multiple linear regression analysis was performed to examine the association between various potential indicators and 6-month postoperative Parker scores for the total population (Table 3). This model indicated that better 6-month postoperative Parker scores were associated with age, baseline Parker scores, TTA < 24 h, diabetes, hospital rehabilitation, and outpatient follow-up (p < 0.05).
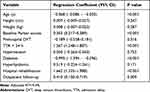 |
Table 3 Results of Multiple Linear Regression Analysis on 6-Month Parker Score Postoperatively |
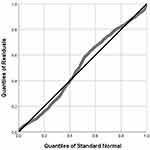 |
Figure 1 Quantile-Quantile plot of residuals in the multiple linear regression model for the total population. |
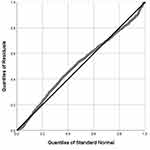 |
Figure 2 Quantile-Quantile plot of residuals in the multiple linear regression model for patients who received surgical treatment. |
For patients who received surgical treatment, the multiple linear regression model revealed that 6-month postoperative Parker score was significantly related to age, baseline Parker scores, TTA < 24 h, TTS < 48 h, diabetes, and hospital rehabilitation (p < 0.001) (Table 4).
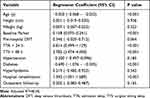 |
Table 4 Results of Multiple Linear Regression Analysis for Patients Who Received Operative Treatment on 6-Month Parker Score Postoperatively |
Discussion
The present study focused on the risk factors associated with the prognosis of elderly patients with hip fractures, providing several key insights into such patients without SARS-CoV-2 during the COVID-19 pandemic. Firstly, TTA, which has been neglected in previous research, was found to be significantly associated with postoperative prognosis (6-month postoperative Parker scores). Secondly, the prognosis is significantly affected by the patient’s location after discharge and outpatient follow-up. Specifically, for all elderly hip fracture patients included in the present study, hospital rehabilitation and outpatient follow-up significantly improved 6-month postoperative Parker scores, while for patients who underwent surgery, hospital rehabilitation was beneficial for prognosis but outpatient follow-up had no significant impact. Thirdly, the impact of delay from injury to operation in elderly hip fracture patients deserves more attention, to increase the scientific basis for effective disease management outside of hospital, and because the overall delay might partly explain disagreement about the need for surgery to be conducted as soon as possible after admission.
After the outbreak of COVID-19 in China, the Chinese government implemented multifactorial prevention measures to restrict people’s movement and avoid their contact with suspected cases; for example, patients diagnosed as SARS-CoV-2 positive were admitted to specialized hospitals. These measures proved highly effective in restricting the spread of COVID-19. During the pandemic, our hospital received only patients free of SARS-CoV-2, confirmed via nucleic acid detection and chest computerized tomography. Compared with the non-pandemic period, the injury mechanism and epidemiology of traumatic fractures have changed dramatically in China, while the incidence of fragility fractures, such as hip fractures in the elderly, remains stable.8 In the present study, the number of elderly hip fracture patients at the height of the epidemic was similar to that in the same periods in 2017–2019. During a pandemic such as COVID-19, knowledge of these trends is of great importance, because of the high morbidity and mortality of elderly patients with hip fractures. Both for the total population and patients who received operations, the percentage of patients with TTA < 24 h, in rehabilitation hospital, and with outpatient follow-up were significantly decreased in experiment group when compared with the control group. In addition, surgical duration was increased and the percentage of patients with TTS < 48 was decreased during COVID-19, which might be affected by COVID-19, such as traffic control or the fear of the epidemic. However, there were no significant differences in 6-month mortality postoperatively between experiment and control group. And, for those who chose surgical treatment, the perioperative mortality in experiment group (O) was similar with that in control group (O). The same mortality rate between groups might be attributed to advances in medical technology or relatively low sample size.
During COVID-19, TTA and TTS were both delayed to some extent, providing an opportunity to investigate the relationship between TTA/TTS and the postoperative prognosis of elderly hip fracture patients more objectively. For hip fractures in the elderly, accelerated surgery has generated increasing attention17 and the issue is controversial since proponents of a delay believe it provides the opportunity to optimize patients’ medical status, thereby decreasing the risk of perioperative complications.26 It is neither logical nor ethical to study a delay to surgery, particularly since patients with more severe illness are most likely to suffer a delay, meaning that groups in such a study would be heterogeneous. Previous research has attempted to address this by retrospectively stratifying patients by health status to control for illness severity, but has been limited by low statistical power.21,27–29 Previous studies have often neglected TTA, which may present risk for elderly hip fracture patients due to a lack of medical care. In the present study, TTA > 24 h (but not TTS > 24 h) was an independent risk factor for six-month DVT, which may have resulted from the delay to in-hospital care. Earlier admission after fracture may benefit elderly hip fracture patients even if surgery is delayed after admission. In this study, compared with patients during the period from 2017 to 2019, the percentage of patients who chose conservative treatment in a period during COVID-19 pandemic was significantly higher. One important reason could be patients’ concern that long-term medical care could make them susceptible to nosocomial COVID-19 infection.30–33 These patients should be observed carefully in the recovery period.
Although surgical treatment can reduce the patient’s pain duration and improve function associated with hip fracture in elderly patients, long-term rehabilitation is required for functional independence.34 Under normal circumstances, elderly patients with hip fractures have been recommended to rehabilitate in hospital for further recovery and to attend for follow-up visits 1.5, 3, 6, 12 and 24 months after discharge. However, both rehabilitation and follow-up were impacted by the pandemic, with negative outcomes. In recent years, home-based rehabilitation has generated increasing interest for its positive effect on the physical and mental functions of patients with various ailments.35–37 Home-based rehabilitation with proper guidelines could aid in the recovery of elderly hip fracture patients during COVID-19. In addition, the Internet healthcare based on 5G communication technology should be widely applied to guide patients online with no face-to-face contact, and may be particularly meaningful during COVID-19 and other similar periods.
Our findings suggest that the age of elderly patients with hip fractures in the epidemic period was significantly higher than that in the non-epidemic period, consistent with previous research.5 During the epidemic period, most industries stopped production, besides, outdoor activities, unnecessary travel and transportation were canceled, affecting mostly young and middle-aged adults. However, the elderly people who ordinarily stay at home, especially those with hip fractures, were more likely to have low-energy fractures due to a decrease in exercise and change to sedentary lifestyle during the epidemic period.18 In patients who chose surgical treatment, TTA was significantly longer during COVID-19 than in the non-pandemic period, with resulting significant increases in preoperative complications such as DVT, indicating a link between TTA and DVT.
To our knowledge, this is the first research to focus on identifying risk factors associated with hip fractures in SARS-CoV-2-negative elderly patients during COVID-19. We believe the present study may provide a guideline for countries and regions still affected by the pandemic. However, some potential limitations should be considered. Firstly, this is single-center study with a relatively small sample size; secondly, the results may only apply to hospitals handling patients who are COVID-19 negative; thirdly, follow up extended to only six months, which is insufficient to investigate long-term outcomes in COVID-19-negative elderly hip fracture patients. Further study should be conducted addressing these limitations.
Conclusion
To summarize, elderly patients with hip fractures tend to have worse outcomes during COVID-19, despite being free of the disease. TTA, which has been neglected in previous research, is a risk factor for the incidence of perioperative DVT and postoperative functional recovery, while TTS was not associated with perioperative complications in the present study. This means that delays in admission to hospital may be much more dangerous than those after admission, and TTA should be minimized in elderly patients with hip fractures. Furthermore, postoperative follow-up and postoperative rehabilitation are independent risk factors associated with prognosis, which should be implemented during the pandemic.
Funding
W.-T.J. received funding from the National Key Research and Development Program of China (NO.2018YFC1106300), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (Grant NO.20172026), and Shanghai Talents Development Fund (Grant NO.2017035).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Phelan AL, Katz R, Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020;323(8):709–710. doi:10.1001/jama.2020.1097
2. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
3. Popov GT, Baymakova M, Vaseva V, Kundurzhiev T, Mutafchiyski V. Clinical characteristics of hospitalized patients with COVID-19 in Sofia, Bulgaria. Vector Borne Zoonotic Dis. 2020;20(12):910–915. doi:10.1089/vbz.2020.2679
4. Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi:10.1136/bmj.m1985
5. Lv H, Zhang Q, Yin Y, et al. Epidemiologic characteristics of traumatic fractures during the outbreak of coronavirus disease 2019 (COVID-19) in China: a retrospective & comparative multi-center study. Injury. 2020;51(8):1698–1704. doi:10.1016/j.injury.2020.06.022
6. Pranata R, Lim MA, Huang I, Raharjo SB, Lukito AA. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression. JRAAS. 2020;21(2):1470320320926899. doi:10.1177/1470320320926899
7. Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia – a systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2020;14(4):395–403. doi:10.1016/j.dsx.2020.04.018
8. Nuñez JH, Sallent A, Lakhani K, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51(7):1414–1418. doi:10.1016/j.injury.2020.05.016
9. Scott CEH, Holland G, Powell-Bowns MFR, et al. Population mobility and adult orthopaedic trauma services during the COVID-19 pandemic: fragility fracture provision remains a priority. Bone Joint Open. 2020;1(6):182–189. doi:10.1302/2633-1462.16.Bjo-2020-0043.R1
10. Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519–1525. doi:10.1056/nejm199606063342307
11. Yombi JC, Putineanu DC, Cornu O, Lavand’homme P, Cornette P, Castanares-Zapatero D. Low haemoglobin at admission is associated with mortality after Hip fractures in elderly patients. Bone Joint J. 2019;101-b(9):1122–1128. doi:10.1302/0301-620x.101b9.Bjj-2019-0526.R1
12. Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of Hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55(3):146–154. doi:10.1007/bf03016088
13. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after Hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(15):1609–1616. doi:10.1503/cmaj.092220
14. Nyholm AM, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish fracture database collaborators. J Bone Joint Surg Am. 2015;97(16):1333–1339. doi:10.2106/jbjs.O.00029
15. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in Hip fracture patients improves survival. Injury. 2013;44(6):726–729. doi:10.1016/j.injury.2012.08.025
16. Bretherton CP, Parker MJ. Early surgery for patients with a fracture of the Hip decreases 30-day mortality. Bone Joint J. 2015;97-b(1):104–108. doi:10.1302/0301-620x.97b1.35041
17. Borges FK, Bhandari M, Guerra-Farfan E, et al. Accelerated surgery versus standard care in Hip fracture (Hip ATTACK): an international, randomised, controlled trial. Lancet. 2020;395(10225):698–708. doi:10.1016/s0140-6736(20)30058-1
18. Malik-Tabassum K, Crooks M, Robertson A, To C, Maling L, Selmon G. Management of Hip fractures during the COVID-19 pandemic at a high-volume Hip fracture unit in the United Kingdom. J Orthop. 2020;20:332–337. doi:10.1016/j.jor.2020.06.018
19. Slullitel PA, Lucero CM, Soruco ML, et al. Prolonged social lockdown during COVID-19 pandemic and Hip fracture epidemiology. Int Orthop. 2020;44(10):1887–1895. doi:10.1007/s00264-020-04769-6
20. Yu P, Wu C, Zhuang C, et al. The patterns and management of fracture patients under COVID-19 outbreak in China. Ann Transl Med. 2020;8(15):932. doi:10.21037/atm-20-4174
21. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after Hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. doi:10.2106/jbjs.D.01796
22. Pluskiewicz W, Wilk R, Adamczyk P, et al. The incidence of arm, forearm, and Hip osteoporotic fractures during early stage of COVID-19 pandemic. Osteoporos Int. 2021:1–5. doi:10.1007/s00198-020-05811-4.
23. Clement ND, Hall AJ, Makaram NS, et al. IMPACT-Restart: the influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Joint J. 2020;102-b(12):1774–1781. doi:10.1302/0301-620x.102b12.Bjj-2020-1395.R2
24. Dizdarevic A, Farah F. Perioperative management of elderly patients presenting with Hip fracture during COVID-19 pandemic surge. J Clin Anesth. 2020;67:110014. doi:10.1016/j.jclinane.2020.110014
25. Parker MJ, Palmer CR. A new mobility score for predicting mortality after Hip fracture. J Bone Joint Surg Br. 1993;75(5):797–798. doi:10.1302/0301-620x.75b5.8376443
26. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for Hip fracture and patient outcomes. JAMA. 2004;291(14):1738–1743. doi:10.1001/jama.291.14.1738
27. Eiskjaer S, Ostgård SE. Risk factors influencing mortality after bipolar hemiarthroplasty in the treatment of fracture of the femoral neck. Clin Orthop Relat Res. 1991;270:295–300. doi:10.1097/00003086-199109000-00039
28. White BL, Fisher WD, Laurin CA. Rate of mortality for elderly patients after fracture of the Hip in the 1980ʹs. J Bone Joint Surg Am. 1987;69(9):1335–1340.
29. Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the Hip. J Bone Joint Surg Am. 1995;77(10):1551–1556. doi:10.2106/00004623-199510000-00010
30. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–882. doi:10.1016/s0140-6736(98)09075-8
31. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi:10.1016/s0140-6736(02)08657-9
32. Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. doi:10.1001/jama.2009.50
33. Borgström F, Zethraeus N, Johnell O, et al. Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int. 2006;17(5):637–650. doi:10.1007/s00198-005-0015-8
34. Okamoto T, Ridley RJ, Edmondston SJ, Visser M, Headford J, Yates PJ. Day-of-surgery mobilization reduces the length of stay after elective hip arthroplasty. J Arthroplasty. 2016;31(10):2227–2230. doi:10.1016/j.arth.2016.03.066
35. Karlsson Å, Lindelöf N, Olofsson B, et al. Effects of geriatric interdisciplinary home rehabilitation on independence in activities of daily living in older people with hip fracture: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(4):571–578. doi:10.1016/j.apmr.2019.12.007
36. Wong JJ, Shearer HM, Mior S, et al. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? An update of the bone and joint decade task force on neck pain and its associated disorders by the OPTIMa collaboration. Spine J. 2016;16(12):1598–1630. doi:10.1016/j.spinee.2015.08.024
37. Buhagiar MA, Naylor JM, Harris IA, Xuan W, Adie S, Lewin A. Assessment of outcomes of inpatient or clinic-based vs home-based rehabilitation after total knee arthroplasty: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(4):e192810. doi:10.1001/jamanetworkopen.2019.2810
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
