Back to Journals » Journal of Pain Research » Volume 10
The impact of anxiety and depressive symptoms on chronic pain in conservatively and operatively treated hand surgery patients
Authors Egloff N, Wegmann B, Juon B, Stauber S, von Känel R, Vögelin E
Received 7 July 2016
Accepted for publication 28 October 2016
Published 31 January 2017 Volume 2017:10 Pages 259—263
DOI https://doi.org/10.2147/JPR.S116674
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Niklaus Egloff,1,2 Barbara Wegmann,1 Bettina Juon,3 Stefanie Stauber,1 Roland von Känel,2,4 Esther Vögelin3
1Division of Psychosomatic Medicine, Department of General Internal Medicine, Inselspital Bern University Hospital, 2Department of Clinical Research, University of Bern, 3Department of Plastic and Hand Surgery, Inselspital Bern University Hospital, Bern, 4Department of Psychosomatic Medicine, Clinic Barmelweid, Barmelweid, Switzerland
Abstract: The aim of this prospective study was to examine to what extent anxiety and depressive symptoms predict the level of pain at 4-month follow-up in hand surgery patients. A total of 132 consecutive patients (mean age: 51.5±17.1 years, 51.9% female) of a tertiary center for hand surgery participated in this study. The patients underwent conservative or operative treatment, depending on the nature of their hand problem. The initial pain assessment included psychometric testing with the hospital anxiety and depression scale. Ninety-nine patients underwent operative treatment and 33 patients were conservatively treated. At 4-month follow-up, the amount of pain was measured with a visual analog scale (0–10). After controlling for age, sex, and pre-surgical pain intensity, depressive symptoms were a significant predictor for increased pain levels at follow-up in conservatively treated patients. In operatively treated patients, anxiety symptoms showed a trend for being a predictor of pain level at follow-up. The findings support the assumption that psychological factors may have an impact on pain outcome in patients presenting to hand surgery clinics.
Keywords: chronic pain, hand surgery, depressive symptoms, anxiety
Introduction
Chronic pain is defined as pain lasting over a period of at least 3 months.1 Patients with chronic pain are frequently seen in departments of hand surgery.2 Whereas a large proportion of patients benefit from surgical interventions, some continue to suffer from pain regardless of such therapeutic measures.3 Depending on the nature of the damaged anatomical structures, pain occurs postoperatively with different frequencies and for different durations. From research on complex regional pain syndrome (CRPS) type 1, it is, however, known that often there is no correlation between the type of initial lesion and the severity of subsequent pain and that psychological factors may be predictive for the course of pain.4
There is a large and well-established branch of pain research showing that in terms of the risk of post-surgical pain, psychological and social factors play a crucial role.5 In the case of patients undergoing spine surgery, Block et al have suggested that psychological factors may have a greater impact on outcome than medical ones, including type of surgery, chronicity, and previous spine surgery. The accuracy of pre-surgical psychological screening predicting overall outcome was 82%.6
An increasing number of studies also suggest an influence of psychological distress in hand surgery. A recent study of 66 patients with CRPS type 1 showed that anxiety is associated with poorer outcomes of this condition, including pain level, although patients with CRPS type 1 of the upper and lower limb were combined.4 A study of 121 patients with distal radius fractures reported that pain anxiety and pain catastrophizing were significantly associated with delayed functional recovery and increase in perceived disability, although the level of pain was not reported as a separate outcome.7 A further study of 120 patients with hand injuries showed that depressive symptoms were a significant predictor of pain intensity between 10 and 14 days after minor hand surgery (e.g., surgery for carpal tunnel syndrome, trigger finger, and benign hand tumor).3 One prospective and one retrospective study on 83 and 89 patients, respectively, who underwent decompression of carpal tunnel, found low mental health scores to be correlated with poorer response to surgery and higher level of scar pain.8,9 Taken together, it follows from the assessment of the currently available literature that more prospective studies are needed to gain more clarity about a potential association of anxiety and depressive symptoms with pain level as an outcome in hand surgery patients.
In theory, general pain research offers sufficient grounds for a link of anxiety and depressive symptoms with chronic pain. Basically, pain perception is a function of the brain, which alerts the individual about potential tissue damage. This somatosensory function is always influenced by limbic-affective ones, coloring the experience of pain as emotionally aversive. This affective aspect is a function of brain structures that are also involved in anxiety and depressive disorders.10,11 Thus, it is not surprising that anxiety and depression along a spectrum of severity (i.e., yet at subsyndromal levels) are supposed to have an impact on pain experience.
In hand surgery clinics, a wide range of treatment options are available that can roughly be categorized according to operative and conservative interventions. Both these approaches have their clear indications and treatment standards.12 Regarding the treatment process, the operative procedure is perceived by patients as more severe and less controllable, but possibly more suggestible.13 To the extent that pain conditions differ between the two procedures, we distinguished in our analysis between operatively and conservatively treated patients. Accordingly, we hypothesized that anxiety and depressive symptoms would affect pain levels at 4-month follow-up in both the treatment groups, but with different effects.
Methods
Study design and patient population
This prospective investigation included 132 consecutive patients of a tertiary center for hand surgery. The study protocol was approved by the local ethics committee (KEK-Nr.117/12). All patients provided written informed consent for participating in the study.
Inclusion criteria was that participants must be at least 18 years of age. Regarding diagnoses, there were no selection criteria, that is, all patients were invited to participate in the study, regardless of their specific hand surgical problems. In particular, patients were not selected based on their pre-surgical pain level, so that patients with and without pre-surgical pain were included.
All patients included in the study underwent an initial, as well as a follow-up interview 4 months later. The interviews were conducted by one and the same investigator (BW). They took place in a separate room on the occasion of the consultation with the two hand surgeons (EV and BJ). The hand surgeons were blinded to the psychometric data of patients.
The decision regarding the necessary hand surgery intervention – operative or conservative – was taken by the two surgeons according to current Western standards.12 The chosen procedures were strictly based upon the type of lesion and anatomical circumstances of each patient. Therefore, a random allocation to the intervention groups was not intended, nor was it possible.
Conservative treatment included splinting of injured joints or soft tissues. Specific treatments to reduce pain were transcutaneous electrical nerve stimulation (TENS), lymph tapes, anti-inflammatory treatments by iontophoresis, laser, or sonography, and passive and active joint mobilization depending on the injury, stretching, and massaging of soft tissues and muscles.
Surgical treatment included procedures such as debridement of infected tissues, repair of skin, nerves, vessels, tendon, bones, joints, and reconstruction after trauma. In elective surgery, there were neurolyses of median and ulnar nerves; arthroplasties of carpometacarpal, metacarpophalangeal, or interphalangeal joints; arthrodeses and arthroscopies of radiocarpal joint, skin, and soft tissue tumor resections, as well as tendon transfers or reconstructions.
Psychometric assessment
During the initial consultation with the patient, a pain history was taken followed by the patient completing a self-rated psychometric questionnaire, namely, the Hospital Anxiety and Depression Scale (HADS).14 The HADS is a screening instrument for determining the level (i.e., the severity) of anxiety (HADS-A) and depression symptoms (HADS-D), but it cannot confirm a psychiatric diagnosis of an anxiety or depressive disorder. The HADS is a valid and reliable instrument to assess depressive and anxiety symptoms in populations with somatic diseases with a Cronbach’s alpha between .68 and .93 for HADS-A and between .67 and .90 for HADS-D.15 The anxiety and depressive symptom subscales each comprise seven items that are rated on a Likert scale from 0 to 3 total (scores 0–21).15 The test takes about 8 minutes to complete.
Our outcome measure (dependent variable) was the level of pain at a 4-month follow-up. All patients were asked to rate their pain level with a visual analog scale (VAS) ranging from 0 (no pain) to 10 (highest pain imaginable).16
Data analysis
We used independent t-test, Mann–Whitney U test, and chi-square test to compare the two patient groups on demographic and clinical characteristics. Multiple regression analyses were carried out controlling for age, sex, pain level at the initial assessment and HADS scores (independent variables).
Results
Within a period of 6 months, 132 consecutive patients could be included in the study. Table 1 summarizes the sociodemographic and clinical data of the cohort. Table 2 gives an overview of the diagnoses and treatments of the patients. Between the first interview and the 4-month follow-up, 33 patients were provided conservative treatment and 99 underwent operative treatment. Compared to the operatively treated patients, those in the conservatively treated group were significantly older, reported greater pain intensity at the 4-month follow-up, and had greater levels of anxiety symptoms. Degenerative disorders were significantly more frequent, whereas injuries and compression neuropathy were less frequent in conservatively treated patients, who, moreover, used less paracetamol compared with operatively treated patients.
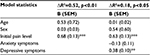
After controlling for age and sex, pretreatment pain level was found to be a significant predictor for an increased level of pain at the 4-month follow-up (p≤0.001) in both the patient groups. Controlling for age, sex, and initial pain level in patients who were conservatively treated, depressive symptoms were found to be a significant predictor for an increased pain level at the 4-month follow-up (B=0.38, p=0.001; Table 3). For every point increase in the HADS-D score, there was a 0.38-point higher level of pain intensity at the 4-month follow-up. Accordingly, a 3-point increase in the HADS-D score corresponded to a 1.14-point increase on the pain VAS. Usually, a one- or two-point change/difference on the pain VAS is considered to be clinically relevant. To better illustrate this: the difference in pain scores between a patient with a normal level of depressive symptoms (HADS-D score=7) and a patient with moderate depressive symptoms (HADS-D score=13) would exceed two units on the VAS, indicating clinical relevance.
Depression accounted for 1.8% of the unique variance in pain intensity at the 4-month follow-up.
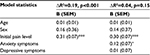
In patients who were operatively treated, anxiety symptoms showed a trend for being a predictor of the level of pain (B=0.12, p=0.09; Table 4), explaining 0.4% of the unique variance in pain intensity at the 4-month follow-up. For every point increase in the HADS-A score, there was a 0.12-point higher level of pain intensity at the 4-month follow-up.
Discussion
In concordance with our hypothesis, this prospective study of 132 subjects showed that symptoms of anxiety and depression may predict the level of pain in patients undergoing hand surgery treatment. In conservatively treated patients, depressive symptoms were a significant predictor of elevated pain levels at the 4-month follow-up. In operatively treated patients, anxiety symptoms showed a trend towards statistical significance. These results are in agreement with other recent studies in hand surgery patients, although prospective studies are still few in number.4,7–9
The differing patterns of correlations in conservatively and operatively treated patients suggest different pain conditions in the two patient groups. As expected, this is also reflected by differences in some patient characteristics that suggest two distinct diagnostic populations (Table 1).
As shown in Table 2, we included a broad spectrum of hand surgical diagnoses. We are aware that this heterogeneity across hand surgical diagnoses represents a certain limitation in terms of the generalization of our results. To determine the association of anxiety and depressive symptoms with the outcome of specific hand surgery diagnoses, future cohort studies with larger sample sizes are clearly needed.
As a whole, the currently available literature draws attention to the relevance of psychosocial factors as predictors of pain persistence, pointing out at the same time that the development of chronic pain is always multicausal. Accordingly, in recent years, the bio-psychosocial model has established its firm role in understanding the pathogenesis of chronic pain.17 This multicausal model assigns the relevance of biological aspects, as well as psychosocial aspects, and analyzes their inherent pathophysiological relationships. Furthermore, modern experiments in animal models provide physiological evidence in support of the hypothesis that psychological stressors intensify and prolong pain responses in the peripheral and central nervous system via alterations in neuroendocrine pathways and substrates.18–21
We mention several limitations of our study. Due to the rather small effects, our results are to be interpreted carefully. However, as illustrated, the association between depressive symptoms and pain levels may be considered clinically meaningful. The rather small variance in pain scores explained by depressive and anxiety symptoms implies that there must be additional, perhaps even more important factors explaining the pain levels at 4-month follow-up. We only measured depressive and anxiety symptoms due to feasibility issues. However, other important concepts such as quality of life, self-esteem, allostatic stress load, positive affects, or well-being would be predictors of interest to be investigated in future studies. Furthermore, we did not assess anxiety and depressive symptoms at follow-up, so we cannot draw any conclusions based on the course of psychological symptoms.
Nevertheless, all together, this study motivates to take more care about patient’s psychological conditions in hand surgery. Obviously, future studies will have to examine the extent to which concomitant treatment of psychological symptoms can improve the outcome of hand surgical treatments. Findings of interdisciplinary pain centers offering multimodal therapeutic approaches suggest that such an effect can be expected.22
Disclosure
The authors report no conflicts of interest in this work.
References
Treede RD, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. | ||
Eiche J, Krimmer H, Lanz U, Müller-Zimmermann A, Reichl M. Treatment of hand surgery patients in chronic pain. Orthopade. 2003;32(5):413–417. German. | ||
Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010;35(6):956–960. | ||
Bean DJ, Johnson MH, Heiss-Dunlop W, Lee AC, Kydd RR. Do psychological factors influence recovery from complex regional pain syndrome type-1? A prospective study. Pain. 2015;156(11):2310–2318. | ||
Hinrichs-Rocker A, Schulz K, Järvinen I, Lefering R, Simanski C, Neugebauer EA. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) – a systematic review. Eur J Pain. 2009;13(7):719–730. | ||
Block AR, Ohnmeiss DD, Guyer RD, Rashbaum RF, Hochschuler SH. The use of presurgical psychological screening to predict the outcome of spine surgery. Spine J. 2001;1(4):274 –282. | ||
Roh YH, Lee BK, Noh JH, Oh JH, Gong HS, Baek GH. Effect of anxiety and catastrophic pain ideation on early recovery after surgery for distal radius fractures. J Hand Surg Am. 2014;39(11):2258–2264. | ||
Kim JK, Kim YK. Predictors of scar pain after open carpal tunnel release. J Hand Surg Am. 2011;36(6):1042–1046. | ||
Nanavati N, Walker-Bone K, Stanworth H, Williams C. Outcomes of open carpal tunnel decompression. N Z Med J. 2013;126(1369):60–67. | ||
Eisenberger NI. Social pain and the brain: controversies, questions, and where to go from here. Annu Rev Psychol. 2015;66:601–629. | ||
Franklin G, Carson AJ, Welch KA. Cognitive behavioural therapy for depression: systematic review of imaging studies. Acta Neuropsychiatr. 2016;28(2):61–74. | ||
Wolfe S, Pederson W, Hotchkiss R, Kozin S, Cohen M. Green’s Operative Hand Surgery. 6th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2011. | ||
Sihvonen R, Paavola M, Malmivaara A, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–2524. | ||
Herrmann C, Buss U, Snaith RP. HADS-D. Hospital Anxiety and Depression Scale. Deutsche Version. Bern, Switzerland: Hans Huber; 1995. | ||
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. | ||
Sindhu BS, Shechtman O, Tuckey L. Validity, reliability, and responsiveness of a digital version of the visual analog scale. J Hand Ther. 2011;24(4):356–363. | ||
Egle UT, Hofmann SO, Lehmann KA, Nix WA, editors. Das bio-psycho-soziale Krankheitsmodell. In: Handbuch chronischer Schmerz. Stuttgart, Germany: Schattauer; 2003:1–9. | ||
Alvarez P, Green PG, Levine JD. Stress in the adult rat exacerbates muscle pain induced by early-life stress. Biol Psychiatry. 2013;74(9):688–695. | ||
Green PG, Chen X, Alvarez P, Ferrari LF, Levine JD. Early-life stress produces muscle hyperalgesia and nociceptor sensitization in the adult rat. Pain. 2011;152(11):2549–2556. | ||
Jennings EM, Okine BN, Roche M, Finn DP. Stress-induced hyperalgesia. Prog Neurobiol. 2014;121:1–18. | ||
Khasar SG, Burkham J, Dina OA, et al. Stress induces a switch of intracellular signaling in sensory neurons in a model of generalized pain. J Neurosci. 2008;28(22):5721–5730. | ||
Deckert S, Kaiser U, Kopkow C, Trautmann F, Sabatowski R, Schmitt J. A systematic review of the outcomes reported in multimodal pain therapy for chronic pain. Eur J Pain. 2016;20(1):51–63. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.