Back to Journals » Risk Management and Healthcare Policy » Volume 13
The Impact of Air Pollution on Healthcare Expenditure for Respiratory Diseases: Evidence from the People’s Republic of China
Received 8 July 2020
Accepted for publication 3 September 2020
Published 24 September 2020 Volume 2020:13 Pages 1723—1738
DOI https://doi.org/10.2147/RMHP.S270587
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Marco Carotenuto
Lele Li,1,* Tiantian Du,2,* Chi Zhang3
1School of Public Policy and Management, Tsinghua University, Beijing 100084, People’s Republic of China; 2Institute for Hospital Management, Tsinghua University, Shenzhen 518055, People’s Republic of China; 3Chinese Academy of Fiscal Sciences, Beijing 100142, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Lele Li
School of Public Policy and Management, Tsinghua University, No.1 Tsinghua Yard, Haidian District, Beijing 10084, People’s Republic of China
Tel +86-010-6147-2626
Email [email protected]
Background: Air pollution is an important factor in health outcomes and health-care expenditure. It has become an important issue of global concern. The objective of this study was to explore the influence of air pollution on the economic burden of respiratory diseases using different levels of PM2.5.
Methods: Starting from the demand side, we took the 3,546 patients in the Respiratory and Critical Care Department of a tertiary hospital in Beijing between 2013 and 2015 as examples, combining daily air-quality data using a generalized linear regression–analysis model to explore the impact of air pollution on health-care expenditure on a microindividual level.
Results: We found that PM2.5 had a significant impact on health-care expenditure on respiratory diseases. It had a positive impact on total health-care expenditure, drug expenditure, and antibiotic expenditure. The impact of different levels of air pollution on the health care–expenditure burden of disease was heterogeneous. As the air-pollution index increased, health care–expenditure burden of respiratory diseases also gradually raised. The impact of PM10 and air-quality index had a positive impact on health-care expenditure for respiratory diseases. Air pollution had a significant impact on health care–expenditure burden of respiratory diseases. The effect of length of stay on various health-care expenditure was significantly positive.
Conclusion: The impact of mortality-risk classification on various health-care expenditure is significant. Therefore, policy-making must take into account both the supply side and the demand side of health-care services. Furthermore, the government should strengthen environmental governance, pay attention to the heterogeneity of the health care–expenditure burden affected by environmental pollution, improve the medical insurance system, and improve the health of residents to reduce the health care–expenditure burden.
Keywords: air pollution, PM2.5, respiratory diseases, health care–expenditure burden, individual health level
Introduction
Air pollution has become a major public concern around the world. It is caused mainly by the combustion of fuel and waste, industrial activities, and natural dust, including fine particles and harmful gases. According to a survey conducted by the World Health Organization, 90% of residents in the world live in areas that do not meet WHO air-quality standards.1 The Global Burden of Diseases, Injuries, and Risk Factor Study 2015 (GBD2015) showed that environmental pollution is the main factor affecting the global burden of disease, especially in low-and middle-income countries.2 The impact of exposure to PM2.5 on the global burden of disease continues to increase. The number of deaths resulting from PM2.5 increased from 3.5 million in 1990 to 4.2 million in 2015, accounting for 7.6% of total deaths all around the world. It is one of the five major risk factors for death.3 As is known to all, China’s economy has developed rapidly since its economic reform and opening up in 1978. However, with economic development, population growth, and urbanization acceleration, environmental problems, especially air pollution, are getting worse. According to the Report on the State of the Ecology and Environment in China in 2018, only 35.8% of a total 338 cities met national air-quality standards. Air-pollution improvement has become the top priority of China’s entire society. In 2018, the State Council issued and implemented the Three-Year Action Plan for Winning the Battle in Defense of Blue Skies, marking ecological environmental protection reaching a new stage. At the same time, some studies showed that air pollution not only damages residents’ physical health4 but also worsens mental health.5 Furthermore, Healthy China 2030 proposes that prosperity for all is impossible without health for all, and it is necessary to solve the environmental problems that affect the population’s health. Therefore, it is especially urgent and important to explore the relationship between air pollution and health in China.
The nexus of air pollution and health has received widespread attention from scholars. At present, there are two main types of research on the relationship between air pollution and health. The first type explores the impact of air pollution on residents’ health outcomes from a medical or public health perspective. Air pollution is the biggest environmental risk to health, mainly causing cardiovascular and respiratory diseases. As such, there have been a large amount of studies using cardiovascular or respiratory diseases as examples to study the impact of air pollution on health. Studies have shown that compared with other causes of death, the impact of air pollution on cardiovascular disease is the largest.6 Both developed and developing countries have confirmed that air pollution increases the rate of cardiovascular and respiratory diseases, hospital admissions,7–13 and mortality.13–18 Air pollution can also affect birth outcomes, such as low birth weight xx,19–21 preterm birth (PTB),22–24 and births small for gestational age (SGA).25,26 In addition, air pollution also affects diabetes mellitus,27–32 cognitive functioning and impairment,33–38 and metabolic syndrome.39
The second type of research is the study of the impact of air pollution on health-care expenditure from social and economic perspectives. Narayan and Narayan40 used 1980–1999 data from eight OECD countries to study the effect of air pollution on health-care expenditure. Short-term elasticity indicates that CO1 emissions have a positive impact on health expenditure, while long-term elasticity indicates that apart from CO1, SO emissions also have an impact on health expenditure. Apergis et al41 used panel data from 178 countries during 1995–2017 to evaluate the relationship between health-care expenditure and air pollution among different income groups. In general, a 1% increase in CO2 emissions increased health-care expenditure by 2.5%. Specifically, health-care expenditure in the low-income, low–middle income, high–middle income, and high-income groups increased by 2.9%, 1.2%, 2.312%, and 2.6% respectively. Scholars have focused not only on cross-country studies but also single country studies to explore the relationship between air pollution and health-care expenditure. Apergis et al42 used panel data from 50 states in the US spanning the period 1966–2009 to evaluate the short- and long-term effects of CO2 emissions on health-care expenditure. Quantile regression results showed that the impact of CO2 emissions on health-care expenditure was more significant in states with higher health-care expenditure. In detail, CO2 emissions increased by 1% and health-care expenditure of states within the 10th and 90th percentiles increased by 0.13% and 0.16%, respectively. Romley et al used data from California to investigate how air pollution affected private and public insurer spending. The results showed that there were 30,000 hospital admissions and emergency visits due to California’s poor air quality during 2005–2007.43
Jerrett et al44 used data from 49 counties in Ontario, Canada to explore the relationship between health-care expenditure and pollution. Regression results showed that toxic-pollutant emission was significantly linked to health expenditure. Counties with higher toxic-pollutant emissions had higher health-care expenditure per capita, while those with higher expenditure on environmental protection had lower health-care expenditure. Based on data from 16 provinces and cities in South Korea in the period 2010–2017, An and Heshmati45 took four diseases caused by environmental pollution — vascular mobility and allergic rhinitis, atopic dermatitis, asthma, and asthma-persistence status — as examples to explore the influence of air pollution on health-care expenditure. Effects of air pollution on health-care expenditure were analyzed using a fixed-effect model and a random-effect model. The results showed that air pollutants had a positive impact on health-care expenditure. In 2016, health-care expenditure related to environmental pollution reached ₩438 billion. If the environment quality met WHO standards, it would save ₩120.4 billion. Low- and middle-income countries suffer a greater disease burden from air pollution.1 Therefore, research taking developing countries as an example have also begun. Raeissi et al46 analyzed the impact of air pollution on private and public health expenditure using Iranian panel data from 1972 to 2014. The results showed that for a 1% increase in CO2 emissions, public and private health expenditure would increase by 3.32% and 1.16%, respectively.
In summary, many scholars have focused on the effect of environment pollution on health issues and conducted detailed studies on the impact of air pollution on health outcomes and expenditure. In this paper, we attempt to explore the impact of air pollution on burden of disease from the demand side. Combining microdata from the Department of Respiratory and Critical Care Medicine of a tertiary hospital and daily air-quality data in Beijing, we performed multiple regression in order to fill the gap in existing research and provide empirical evidence for policy development. The objective of this study was to explore the influence of air pollution on the economic burden of respiratory diseases using different levels of PM2.5. In the following sections, we describe our data sources and statistical analysis,followed by a description of our descriptive and multivariate findings. The findings are then discussed.
Methods
Data Sources and Variable Selection
We collected 3,546 samples of data from Beijing for 2013–2015. The 3,546 samples were patients hospitalized in the Department of Respiratory and Critical Care Medicine of a tertiary hospital in Beijing between 2013 and 2015. The data are in two parts. One part are individual health care–expenditure dataprovided by the Department of Respiratory and Critical Care Medicine of the tertiary hospital. Health-care expenditure is money spent on respiratory disease treatment. The other part is air-pollution data obtained from the website http://beijingair.sinaapp.com. The Beijing Municipal Environmental Monitoring Center is one of the earliest professional environmental monitoring agencies in China, and it is also a national environmental monitoring primary station. The main responsibility of the center is to monitor atmospheric elements, water, noise, soil, ecology, and other environmental elements within Beijing. The center publishes hourly air-pollutant data on their official website, publishing hourly monitoring data from 35 measurement stations for air pollutants in Beijing. It also includes data from the official website of the Beijing Municipal Environmental Monitoring Center. Weselected the 24-hour average from the measurement station nearest the tertiary hospital. Missing values were replaced by closes values.
The dependent variable was health-care expenditure, which falls into total health-care expenditure, drug expenditure, diagnostic test expenditure, medical consumable expenditure, nursing expenditure, bed expenditure, blood expenditure, and antibiotic-consumption expenditure. The independent variable was the degree of air pollution, measured by three parameters: PM2.5, PM10, and air-quality index(AQI). Among these, PM2.5 is particles in the air with a diameter <2.5 µm, and PM10 particles in the air with a diameter <10 µm. According to the air-pollution index PM2.5 classification standard, the degree of air pollution is divided into excellent (0–50), good (50–100), light pollution (100–150), medium pollution (150–200), heavy pollution (200–300), and serious pollution (>300). The control variables mainly refer to the relevant indicators of diagnosis-related groups (DRGs): length of stay, weight, mortality-risk classification, reference average health-care expenditure, and reference average length of hospital stay.
Model Construction
The empirical research method of this paper was logistic regression, which is a generalized linear regression–analysis model. Logistic regression is often used in data mining, automatic disease diagnosis, economic prediction, and other fields, eg, discussing influencing factors that cause a certain variable and predicting the probability of the occurrence of such variable according to the influencing factors.52 The essence of logistic regression is the probability of occurrence divided by the probability of no occurrence, and then the logarithm is taken. All empirical analysis of data was performed with Stata software.
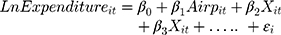
In order to analyze the effects of air pollution on health-care expenditure, we used the data from 2013 to 2015 from Beijing in China and built the logistic regression model(Equation 1):
Equation (1) is composed of four subequations, where  refers to the time period and here refers to 2013–2015,
refers to the time period and here refers to 2013–2015, the model coefficient and,
the model coefficient and,  different patients in the sample. The dependent variables represented the different types of health-care expenditure on patients (including total health-care expenditure, drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure). The independent variables (
different patients in the sample. The dependent variables represented the different types of health-care expenditure on patients (including total health-care expenditure, drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure). The independent variables ( ) mainly included air-pollution status (PM2.5, PM10, and AQI) when different patients were admitted to hospital in the sample. All variables were subjected to log transformation before empirical analysis to reduce dimensional effects.
) mainly included air-pollution status (PM2.5, PM10, and AQI) when different patients were admitted to hospital in the sample. All variables were subjected to log transformation before empirical analysis to reduce dimensional effects.  represented a group of observable control variables. The control variables mainly refer to the relevant indicators of DRGs, including length of stay, weight, mortality-risk classification, reference average health-care expenditure, and reference average length of hospital stay.
represented a group of observable control variables. The control variables mainly refer to the relevant indicators of DRGs, including length of stay, weight, mortality-risk classification, reference average health-care expenditure, and reference average length of hospital stay.
Statistical Characteristics
Descriptive statistics of all variables are shown in Table 1. average total health-care expenditure on respiratory diseases was CN¥15,839.45. The average medical expenditure, average diagnostic test expenditure, average nursing expenditure, average management expenditure, average drug expenditure, average medical consumable expenditure, average antibiotic consumption expenditure, and average blood expenditure was ¥624.75, ¥5,772.01, ¥210.40, ¥1,114.40, ¥6,049.32, ¥2,017.61, ¥3,328.59, and ¥16.97, respectively. Drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure were the main factors in total expenditure: 38.2%, 36.4%, and 20.8%, respectively. This indicated that drug expenditure and diagnostic test expenditure were still the main sources of increased total health-care expenditure. According to relevant calculations of the DRGs, average length of stay for respiratory diseases was 10.66 days, average weight 1.28, mortality-risk classification 2.59, reference average expenditure ¥16,237.38, and reference average length of hospital stays 13.32 days. Descriptive statistics of health-care expenditure in DRGs for respiratory diseases are in Table 2. According to the DRG codes, we divided the samples into 39 DRG groups.
 |
Table 1 Variable Definitions and Descriptive Statistics |
 |
Table 2 Descriptive statistics of health-care expenditure in DRGs for respiratory diseases |
Results
Empirical Analysis
In order to evaluate the impact of air pollution on health-care expenditure, we used 2013–2015 individual health care–expenditure data provided by the Department of Respiratory and Critical Care Medicine of the hospital and air-quality data from http://beijingair.sinaapp.com for the multiple regression analysis. The results are shown in Table 3.
 |
Table 3 Effect of air pollution on Health-Care expenditure |
From the results, PM2.5 had a significant impact on health-care expenditure on respiratory diseases. PM2.5 had a positive impact on total health-care expenditure, drug expenditure, and antibiotic-consumption expenditure, ie, the higher the PM2.5, the higher the expenditure. This showed that the more severe the air pollution is, the higher the total health-care expenditure, drug expenditure, and antibiotic-consumption expenditure will be. The incidence of respiratory diseases was higher because Beijing is a city with severe air pollution. When air pollution is more serious, the incidence of respiratory diseases increases. Air pollution increases the incidence of respiratory diseases and worsens the health of residents, and thus increases health-care expenditure.47 This is the mechanism by which air pollution affects the burden of disease. Length of stay had a significant positive impact on health-care expenditure. The longer the length of stay, the higher the health-care expenditure, which is consistent with reality.
This paper divides air pollution into several levels according to PM2.5: excellent (0–50), good (50–100), light pollution (100–150), medium pollution (150–200), heavy pollution (200–300), and serious pollution (>300). We used the 2013–2015 health care–expenditure data of inpatients from the Department of Respiratory and Critical Care Medicine of the hospital and daily air-quality data in Beijing to further examine the impact of air pollution on health-care expenditure. Results are shown in Tables 4–9. It was found that air-pollution index PM2.5 (0–50) affected total health-care expenditure (significant at 10% level), diagnostic test expenditure (significant at 1% level), and antibiotic-consumption expenditure (not significant) negatively and affected drug expenditure positively (not significant). This indicated that when air quality is excellent, the incidence of respiratory diseases is low and health-care expenditure, such as drug expenditure and diagnostic test expenditure, is lower. However, some patients with chronic respiratory diseases, such as asthma, need medicine for a long time. Therefore, drug expenditure is also high even when the air quality is excellent. Air-pollution index PM2.5 (50–100) had a positive (not significant) impact on total health-care expenditure (significant at 10% level), drug expenditure, diagnostic test expenditure (significant at 1% level), and antibiotic-consumption expenditure, indicating that when air quality is good, the incidence of respiratory diseases began to increase, as did health-care expenditure. Air-pollution index PM2.5 (100–150) had a positive impact on total health-care expenditure (significant at level of 5%), drug expenditure (significant at 10% level), and diagnostic test expenditure (significant at level of 5%) and a negative impact on antibiotic-consumption expenditure (not significant). This showed that when air quality was lightly polluted, the incidence of respiratory diseases increased, and total health-care expenditure, drug expenditure, and diagnostic test expenditure increased. While antibiotic use is affected by disease inflammation, antibiotic consumption expenditure was not affected by air quality significantly. Air-pollution index PM2.5 (150–200) had a positive impact on total health-care expenditure (significant at 1% level), drug expenditure, and diagnostic test expenditure (significant at 10% level) and a negative (not significant) impact on antibiotic-consumption expenditure. As such, the effect of air pollution on health-care expenditure when air pollution was medium-polluted was consistent with that when lightly polluted. They were different significantly (just). Air-pollution index PM2.5 (200–300) had a positive impact on total health-care expenditure (significant at 5% level), drug expenditure (significant at 10% level) and a negative (not significant) impact on diagnostic test expenditure and antibiotic-consumption expenditure. This showed that when the air was heavily polluted, total health-care expenditure and drug expenditure increased, but diagnostic test expenditure and antibiotic-consumption expenditure decreased. This may be due to the fact that when air pollution is more severe, most patients with respiratory diseases do not rely on diagnostic tests, as they have a disease history. The impact of air pollution index PM2.5 (>300) on total health-care expenditure was positive (significant at 1% level) and drug expenditure (significant at 5% level), diagnostic test expenditure, and antibiotic- consumption expenditure (significant at the 10% level) were negative. This shows that when air is seriously polluted, total health-care expenditure increases and drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure reduces. Most patients with respiratory diseases are severely ill when air pollution is serious, and the use of drugs, diagnostic tests, and antibiotics are all reduced. Length of stay had a significant positive impact on various health-care expenditure (significant at 1% level). The longer the length of stay, the higher the expenditure. The impact of mortality-risk classification on various expenditure was more significant, which indicates that the impact of air pollution on the economic burden of respiratory diseases is greatly affected by individual health status.
 |
Table 4 Effect of PM2.5 (0–50) on Health-Care Expenditure on Respiratory Diseases |
 |
Table 5 Effect of PM2.5 (50–100) on Health-Care Expenditure on Respiratory Diseases |
 |
Table 6 Effect of PM2.5 (100–150) on Health-Care Expenditure on Respiratory Diseases |
 |
Table 7 Effect of PM2.5 (150–200) on Health-Care Expenditure on Respiratory Diseases |
 |
Table 8 Effect of PM2.5 (200–300) on Health-Care Expenditure on Respiratory Diseases |
 |
Table 9 Effect of PM2.5 (>300) on Health-Care Expenditure on Respiratory Diseases |
Robustness Check
In order to verify the robustness of the regression results, we replaced key variables. This paper evaluated the effect of PM10 and AQI on health-care expenditure, instead of different levels of PM2.5, comprising excellent (0–50), good (50–100), light pollution (100–150), medium pollution (150–200), heavy pollution (200–300), and serious pollution (>300). We also conducted a separate set of analyses that included PM10 and AQI on health-care expenditure for respiratory diseases. Regression results are shown in Tables 10 and 11, and were basically consistent with the previous regression results. Air-pollution index PM10 and AQI had a positive impact on total health-care expenditure, drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure. Among these, direct and significant levels of explanatory variables were consistent with previous regression results, including different levels of PM2.5, length of stay, weight, mortalit- risk classification, reference health-care expenditure, and reference length of stay.
 |
Table 10 Robustness of Effects of PM10 on Health-Care Expenditure on Respiratory Diseases |
 |
Table 11 Robustness of effects of AQI on Health-Care Expenditure on Respiratory Diseases |
Discussion
With environment protection gradually gaining attention in China, an increasing number of Chinese studies have focused on the impact of air pollution on health-care expenditure. Based on 5-year panel data from 161 cities in China, Chen and Chen48 used three-stage least squares to estimate the impact of SO2 emissions on medical spending. Their results showed that health-care expenditure attributed to SO2 emissions exceeded ¥300 billion. In order to analyze the impact of air pollution on health-care expenditure, Cui et al49 used panel data from 31 provinces and cities during 2006–2012. Regression results showed that air pollution was positively related to health-care expenditure per capita. Hao et al50 used provincial panel data of 1998–2015 and first-order difference generalized method of moments to estimate the impact of environmental pollution on health expenditure on residents. Environmental pollution had a significant impact on health expenditure. For a 1% increase in SO2 and soot emissions, public health expenditure increased by 0.15% and 0.79%, respectively. Based on a spatial econometric model, Zeng and He51 used panel data covering 31 provinces and cities in China from 2002 to 2014 to explore the relationship between industrial air pollution and health-care expenditure. Their results showed that at the provincial level, industrial air pollution had a significant positive impact on health-care expenditure. A 1% increase in industrial air pollution in a province increased health-care expenditure of that and neighboring provinces by 0.032% and 0.0072%, respectively. Yang and Zhang52 used data from the China Urban Household Survey to estimate the impact of environmental pollution on expenditure. They found that with every 1% increase in PM2.5 concentration, household medical expenditure increased by 2.942%. According to data from the China Health and Retirement Longitudinal Survey, Pi et al47 studied the impact of environmental pollution on health-care expenditure of the elderly using ordinary least squares. The regression results showed that environmental pollution (PM10, S02, NO2) affected elderly health status and health status also affected medical insurance costs, which will indirectly affect health-care expenditure. Xu et al used Bayesian quantile regression to estimate the impact of industrial waste–gas emission on health expenditure based on panel data of 30 Chinese provinces during 2005–2016. The results showed that industrial waste–gas emission did affect health expenditure. Furthermore, people in different-income regions have different understanding of environment and health issues. People in low-income regions were likely to ignore this issue.53
Although the relationship between air pollution, PM2.5, and respiratory diseases has attracted great attention from scholars all over the world, there are few studies that have used different levels of PM2.5 to measure air pollution, especially using microdata to evaluate its impact on the economic burden of respiratory diseases. This paper focused on the demand side of disease burden. Combining health care–expenditure data and air-quality data, we evaluated the effect of air pollution on health-care expenditure at the individual level. This paper attempts to introduce different levels of PM2.5 to the research on the influence of air pollution on the economic burden of respiratory diseases, and revealed some important findings.
First, PM2.5 had a significant impact on health-care expenditure for respiratory diseases (Table 3). Because Beijing is a severely polluted city, the incidence of respiratory diseases was higher and total health-care expenditure, drug expenditure, diagnostic test expenditure, and antibiotic-consumption expenditure increased significantly. This was consistent with the conclusions of Zeng and He51 and Yang and Zhang.52 Air pollution is one of the main reasons for increased health-care expenditure on respiratory diseases. In the process of reducing the burden of disease, the government should not only start from the supply side of health-care services, such as reforming medical insurance payments, new technologies, and equipment, but should also focus on solving the demand side, such as by improving air quality, reducing environmental pollution, and improving residents’ health. Therefore, the formulation of policies must take into account both the supply and the demand side of health-care services.
Second, impacts of different levels of air pollution on disease burden were heterogeneous. As the air-pollution index increased, the burden of respiratory diseases gradually rose as well (Tables 4–9). The reason was that the more serious the air pollution, the higher the incidence of respiratory diseases and thus the higher the health-care expenditure. Air pollution increased the incidence of respiratory diseases and worsened residents’ health status, increasing health-care expenditure.47 The impact of PM10 and AQI on disease was basically consistent with the impact of PM2.5 (Tables 10 and 11). Air pollution had a significant impact on health-care expenditure on respiratory diseases. That was the mechanism by which air pollution affected the burden of disease. The impact of different levels of air pollution on health-care expenditure burden is heterogeneous. The government must strengthen air-pollution control to ensure air quality is better, which can effectively reduce the impact of air pollution on health-care expenditure. At the same time, the impact of air pollution on health-care expenditure is different. The medical insurance system must play a key role. Differentiated reimbursement policies can be adopted to reduce the burden of disease on patients.
Finally, the effects of length of stay on various health-care expenditure was significantly positive. The longer the length of stay, the higher the health-care expenditure. The impact of mortality risk on various health-care expenditure was more significant, which indicated that the impact of air pollution on the health-care expenditure for respiratory diseases was greatly affected by individuals’ health status. Individual health status is one of the main factors affecting the burden of disease caused by air pollution.54 In order to improve residents’ health, on the one hand the government should increase the construction of public sports facilities to improve the whole population’s health, and on the other it should focus on environmental governance and ensure decent air quality. In summary, in the process of reducing the impact of air pollution on the burden of disease, a variety of measures must be taken to ensure air quality and good health of residents so as to effectively reduce the burden of disease and ultimately achieve the grand goal of Healthy China 2030.
Our research has several advantages. We used different levels ofPM2.5 to measure air pollution and microdata to evaluate the impact on the economic burden of respiratory diseases. Our results suggest that the impact of different levels of air pollution on disease burden was heterogeneous. As the air-pollution index increased, the burden of respiratory diseases gradually rose as well. In addition, we used health-care expenditure data of inpatients from third-class hospitals in Beijing combined with the daily air-quality data of Beijing to further examine the impact of air pollution on health-care expenditure at an individual level, which can better reflect the mechanism by which different levels of air pollution impacts on the economic burden of respiratory diseases. Finally, our results relied on multiple robustness tests with different standards of air pollution. Our results apply to different logistic regression methods as well as to match different levels of PM2.5 to add to the research on the influence of air pollution on the economic burden of respiratory diseases.
Our study also has some limitations. Firstly, the data were from the tertiary hospital, where patients go for more serious care or treatment. Therefore, the results likely overestimate the health impacts of health-care spending. Secondly, the different levels of PM2.5 had different observations of respiratory diseases at the individual level. For example, the PM2.5 (>300) group had nearly 90 observations, but the PM2.5 (<500) group had about 1,400 observations, which may impact the results for the study. Therefore, we should use big data to ensure the accuracy of empirical results in the future. Thirdly, since our data was taken from hospitals and government websites, we could not control its quality.Last but not least, due to data limitations, we could not control for some variables, such as time trends, temperature, and day of week, which may influence our results.
Conclusion
In summary, this study measured the impact different levels of air pollution on the economic burden of respiratory diseases using the health care–expenditure data of inpatients from tertiary hospitals and daily air-quality data in Beijing. Our findings may contribute some useful information on the impact of air pollution on the economic burden of respiratory diseases in China. For example, the impact of different levels of air pollution on the disease burden was heterogeneous. As the air-pollution index increased, the burden of respiratory diseases gradually rose as well. In the process of reducing the burden of disease, the government should start from the supply side of health-care services, such as reforming medical insurance payments, new technologies, and equipment. Meanwhile, it should also focus on solving the demand side, such as by improving air quality, solving environmental pollution, and improving the health of residents. Therefore, the formulation of policies must take into account both the supply and the demand side of health-care services. All these conclusions enrich and expand our discussion space.
Data-Sharing Statement
Data and materials are free from the hospital.
Ethics Approval and Consent to Participate
The study was exempt from the need to obtain approval (deidentifid data, not human subjects).
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. WHO. Ambient (outdoor) air pollution. Published May 2, 2018. Available from: https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health.
2. Forouzanfar MH, Afshin A, Alexander LT, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659–1724. doi:10.1016/S0140-6736(16)31679-8
3. Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi:10.1016/S0140-6736(17)30505-6
4. Gu HJ, Cao YX, Elahi E, Jha SK. Human health damages related to air pollution in China. Environ Sci Pollut Res. 2019;26(13):13115–13125. doi:10.1007/s11356-019-04708-y
5. Gu HJ, Yan WR, Elahi E, Cao YX. Air pollution risks human mental health: an implication of two-stages least squares estimation of interaction effects. Environ Sci Pollut Res. 2020;27(2):2036–2043. doi:10.1007/s11356-019-06612-x
6. Hoek G, Krishnan RM, Beelen R, et al. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health. 2013;12:16. doi:10.1186/1476-069X-12-43
7. Chang CC, Tsai SS, Ho SC, Yang CY. Air pollution and hospital admissions for cardiovascular disease in Taipei, Taiwan. Environ Res. 2005;98(1):114–119. doi:10.1016/j.envres.2004.07.005
8. Ye F, Piver WT, Ando M, Portier CJ. Effects of temperature and air pollutants on cardiovascular and respiratory diseases for males and females older than 65 years of age in Tokyo, July and August 1980–1995. Environ Health Perspect. 2001;109(4):355–359. doi:10.1289/ehp.01109355
9. Wong CM, Atkinson RW, Anderson HR, et al. A tale of two cities: effects of air pollution on hospital admissions in Hong Kong and London compared. Environ Health Perspect. 2002;110(1):67–77. doi:10.1289/ehp.0211067
10. Capraz O, Deniz A, Dogan N. Effects of air pollution on respiratory hospital admissions in Istanbul, Turkey, 2013 to 2015. Chemosphere. 2017;181:544–550. doi:10.1016/j.chemosphere.2017.04.105
11. Makra L, Matyasovszky I, Balint B. Association of allergic asthma emergency room visits with the main biological and chemical air pollutants. Sci Total Environ. 2012;432:288–296. doi:10.1016/j.scitotenv.2012.05.088
12. Zhang Y, Ding Z, Xiang Q, Wang W, Huang L, Mao F. Short-term effects of ambient PM1 and PM2.5 air pollution on hospital admission for respiratory diseases: case-crossover evidence from Shenzhen, China. Int J Hyg Environ Health. 2020;224:113418. doi:10.1016/j.ijheh.2019.11.001
13. Chen H, Lin Y, Su Q, Cheng L. Spatial variation of multiple air pollutants and their potential contributions to all-cause, respiratory, and cardiovascular mortality across China in 2015–2016. Atmos Environ. 2017;168:23–35. doi:10.1016/j.atmosenv.2017.09.006
14. Kim H, Kim Y, Hong YC. The lag-effect pattern in the relationship of particulate air pollution to daily mortality in Seoul, Korea. Int J Biometeorol. 2003;48(1):25–30. doi:10.1007/s00484-003-0176-0
15. Omori T, Fujimoto G, Yoshimura I, Nitta H, Ono M. Effects of particulate matter on daily mortality in 13 Japanese cities. J Epidemiol. 2003;13(6):314–322. doi:10.2188/jea.13.314
16. Iwai K, Mizuno S, Miyasaka Y, Mori T. Correlation between suspended particles in the environmental air and causes of disease among inhabitants: cross-sectional studies using the vital statistics and air pollution data in Japan. Environ Res. 2005;99(1):106–117. doi:10.1016/j.envres.2004.11.004
17. Yang CX, Peng XW, Huang W, et al. A time-stratified case-crossover study of fine particulate matter air pollution and mortality in Guangzhou, China. Int Arch Occup Environ Health. 2012;85(5):579–585. doi:10.1007/s00420-011-0707-7
18. Zhu FR, Ding R, Lei RQ, et al. The short-term effects of air pollution on respiratory diseases and lung cancer mortality in Hefei: a time-series analysis. Respir Med. 2019;146:57–65. doi:10.1016/j.rmed.2018.11.019
19. Rogers JF, Thompson SJ, Addy CL, McKeown RE, Cowen DJ, Decoufle P. Association of very low birth weight with exposures to environmental sulfur dioxide and total suspended particulates. Am J Epidemiol. 2000;151(6):602–613. doi:10.1093/oxfordjournals.aje.a010248
20. Hyder A, Lee HJ, Ebisu K, Koutrakis P, Belanger K, Bell ML. PM2.5 exposure and birth outcomes use of satellite- and monitor-based data. Epidemiology. 2014;25(1):58–67. doi:10.1097/EDE.0000000000000027
21. Kumar N. The exposure uncertainty analysis: the association between birth weight and trimester specific exposure to particulate matter (PM2.5 vs. PM10). Int J Environ Res Public Health. 2016;13(9):15. doi:10.3390/ijerph13090906
22. Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JKC. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol. 2007;166(9):1045–1052. doi:10.1093/aje/kwm181
23. Lavigne E, Yasseen AS, Stieb DM, et al. Ambient air pollution and adverse birth outcomes: differences by maternal comorbidities. Environ Res. 2016;148:457–466. doi:10.1016/j.envres.2016.04.026
24. Yuan L, Zhang Y, Wang WD, et al. Critical windows for maternal fine particulate matter exposure and adverse birth outcomes: the Shanghai birth cohort study. Chemosphere. 2020;240:9. doi:10.1016/j.chemosphere.2019.124904
25. Ballester F, Estarlich M, Iniguez C, et al. Air pollution exposure during pregnancy and reduced birth size: a prospective birth cohort study in Valencia, Spain. Environ Health. 2010;9:11. doi:10.1186/1476-069X-9-6
26. Hannam K, McNamee R, Baker P, Sibley C, Agius R. Air pollution exposure and adverse pregnancy outcomes in a large UK birth cohort: use of a novel spatio-temporal modelling technique. Scand J Work Environ Health. 2014;40(5):518–530. doi:10.5271/sjweh.3423
27. Eze IC, Hemkens LG, Bucher HC, et al. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect. 2015;123(5):381–389. doi:10.1289/ehp.1307823
28. Thiering E, Heinrich J. Epidemiology of air pollution and diabetes. Trends Endocrinol Metab. 2015;26(7):384–394. doi:10.1016/j.tem.2015.05.002
29. Janghorbani M, Momeni F, Mansourian M. Systematic review and meta-analysis of air pollution exposure and risk of diabetes. Eur J Epidemiol. 2014;29(4):231–242. doi:10.1007/s10654-014-9907-2
30. Eze IC, Foraster M, Schaffner E, et al. Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol. 2017;46(4):1115–1125. doi:10.1093/ije/dyx020
31. Thiering E, Markevych I, Bruske I, et al. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ Health Perspect. 2016;124(8):1291–1298. doi:10.1289/ehp.1509967
32. Yang B-Y, Qian ZM, Li S, et al. Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 communities Chinese Health Study. Lancet Planet Health. 2018;2(2):e64–e73. doi:10.1016/S2542-5196(18)30001-9
33. Perera FP, Rauh V, Whyatt RM, et al. Effect of prenatal exposure to airborne polycyclic aromatic hydrocarbons on neurodevelopment in the first 3 years of life among inner-city children. Environ Health Perspect. 2006;114(8):1287–1292. doi:10.1289/ehp.9084
34. Sun RJ, Gu DN. Air pollution, economic development of communities, and health status among the elderly in urban China. Am J Epidemiol. 2008;168(11):1311–1318. doi:10.1093/aje/kwn260
35. Power MC, Weisskopf MG, Alexeeff SE, Coull BA, Spiro A, Schwartz J. Traffic-related air pollution and cognitive function in a cohort of older men. Environ Health Perspect. 2011;119(5):682–687. doi:10.1289/ehp.1002767
36. Weuve J, Puett RC, Schwartz J, Yanosky JD, Laden F, Grodstein F. Exposure to particulate air pollution and cognitive decline in older women. Arch Intern Med. 2012;172(3):219–227. doi:10.1001/archinternmed.2011.683
37. Lertxundi A, Baccini M, Lertxundi N, et al. Exposure to fine particle matter, nitrogen dioxide and benzene during pregnancy and cognitive and psychomotor developments in children at 15 months of age. Environ Int. 2015;80:33–40. doi:10.1016/j.envint.2015.03.007
38. Clifford A, Lang LD, Chen RL, Anstey KJ, Seaton A. Exposure to air pollution and cognitive functioning across the life course - a systematic literature review. Environ Res. 2016;147:383–398. doi:10.1016/j.envres.2016.01.018
39. Hou J, Liu X, Tu R, et al. Long-term exposure to ambient air pollution attenuated the association of physical activity with metabolic syndrome in rural Chinese adults: a cross-sectional study. Environ Int. 2020;136:105459. doi:10.1016/j.envint.2020.105459
40. Narayan PK, Narayan S. Does environmental quality influence health expenditures? Empirical evidence from a panel of selected OECD countries. Ecol Econ. 2008;65(2):367–374. doi:10.1016/j.ecolecon.2007.07.005
41. Apergis N, Bhattacharya M, Hadhri W. Health care expenditure and environmental pollution: a cross-country comparison across different income groups. Environ Sci Pollut Res. 2020;27:8142–8156. doi:10.1007/s11356-019-07457-0
42. Apergis N, Gupta R, Lau CKM, Mukherjee Z. US state-level carbon dioxide emissions: does it affect health care expenditure? Renew Sust Energ Rev. 2018;91:521–530. doi:10.1016/j.rser.2018.03.035
43. Romley JA, Hackbarth A, Goldman DP. Cost and health consequences of air pollution in California. RAND Corporation; Published 2010. Available from: https://www.rand.org/pubs/research_briefs/RB9501.html.
44. Jerrett M, Eyles J, Dufournaud C, Birch S. Environmental influences on healthcare expenditures: an exploratory analysis from Ontario, Canada. J Epidemiol Community Health. 2003;57(5):334–338. doi:10.1136/jech.57.5.334
45. An J, Heshmati A. The relationship between air pollutants and healthcare expenditure: empirical evidence from South Korea. Environ Sci Pollut Res. 2019;26(31):31730–31751. doi:10.1007/s11356-019-06145-3
46. Raeissi P, Harati-Khalilabad T, Rezapour A, Hashemi SY, Mousavi A, Khodabakhshzadeh S. Effects of air pollution on public and private health expenditures in Iran: a time series study (1972–2014). J Prev Med Public Health. 2018;51(3):140–147. doi:10.3961/jpmph.17.153
47. Pi TL, Wu HY, Li XT. Does Air pollution affect health and medical insurance cost in the elderly: an empirical evidence from China. Sustainability. 2019;11(6):49. doi:10.3390/su11061526
48. Shuo C, Ting C. Air pollution and public health: evidence from sulfur dioxide emission of coal-fires power stations in China. Economic Res J. 2014;49(8):158–169.
49. Ciu E, Jiang S, Jia S. Research on the impact of environmental pollution, commercial health insurance to health costs: based on the empirical analysis of provincial panel data. Nankai econ. Stud. 2016;6:140–150.
50. Hao Y, Liu S, Lu ZN, Huang JB, Zhao MY. The impact of environmental pollution on public health expenditure: dynamic panel analysis based on Chinese provincial data. Environ Sci Pollut Res. 2018;25(19):18853–18865. doi:10.1007/s11356-018-2095-y
51. Zeng JY, He QQ. Does industrial air pollution drive health care expenditures? Spatial evidence from China. J Clean Prod. 2019;218:400–408. doi:10.1016/j.jclepro.2019.01.288
52. Yang J, Zhang B. Air pollution and healthcare expenditure: implication for the benefit of air pollution control in China. Environ Int. 2018;120:443–455. doi:10.1016/j.envint.2018.08.011
53. Xu XC, Xu ZM, Chen LH, Li C. How does industrial waste gas emission affect health care expenditure in different regions of China: an application of bayesian quantile regression. Int J Environ Res Public Health. 2019;16(15):12.
54. Chen LH, Zhang X, Xu X. Health insurance and long-term care services for the disabled elderly in China: based on CHARLS data. Risk Manag Healthc Policy. 2020;13:155–162. doi:10.2147/RMHP.S233949
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.