Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 11
The impact of ABCB1 (rs1045642 and rs4148738) and CES1 (rs2244613) gene polymorphisms on dabigatran equilibrium peak concentration in patients after total knee arthroplasty
Authors Sychev DA, Levanov AN , Shelekhova TV , Bochkov PO , Denisenko NP , Ryzhikova KA , Mirzaev KB, Grishina EA, Gavrilov MA, Ramenskaya GV, Kozlov AV, Bogoslovsky T
Received 28 March 2018
Accepted for publication 9 May 2018
Published 25 July 2018 Volume 2018:11 Pages 127—137
DOI https://doi.org/10.2147/PGPM.S169277
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin Bluth
Dmitriy Alekseevich Sychev,1 Alexander Nikolaevich Levanov,2 Tatiana Vladimirovna Shelekhova,2 Pavel Olegovich Bochkov,3 Natalia Pavlovna Denisenko,4 Kristina Anatolyevna Ryzhikova,4 Karin Badavievich Mirzaev,3 Elena Anatolyevna Grishina,4 Mikhail Alekseevich Gavrilov,5 Galina Vladislavovna Ramenskaya,6 Aleksei Vladimirovich Kozlov,6 Tanya Bogoslovsky7
1Department of Clinical Pharmacology and Therapy, Russian Medical Academy of Continuous Professional Education, Moscow, Russia; 2Department of Occupational Pathology, Haematology and Clinical Pharmacology, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia; 3Department of Personalized Medicine, Research Center, Russian Medical Academy of Continuous Professional Education, Moscow, Russia; 4Department of Molecular Medicine, Research Center, Russian Medical Academy of Continuous Professional Education, Moscow, Russia; 5Department of Traumatology and Orthopedics, Research Institute of Traumatology, Orthopedics and Neurosurgery, Saratov State Medical University named after V.I. Razumovsky, Saratov, Russia; 6Department of A.P. Arzamastsev Pharmaceutical and Toxicological Chemistry, Sechenov First Moscow Medical State University, Moscow, Russia; 7Department of Neurology, Division of Clinical Neurosciences, Turku University Hospital, Turku, Finland
Background: Non-vitamin K oral anticoagulants (NOACs) are commonly used for prophylaxis of venous thromboembolism (VTE) in orthopedic patients. Despite known safety and high potency of NOACs, potential interactions of NOACs with genetic polymorphisms are poorly understood. Dabigatran etexilate is one of the most commonly prescribed direct thrombin inhibitors for the prevention of VTE. The objectives of this study were to assess the effect of ABCB1 (rs1045642 and rs4148738) and CES1 (rs2244613) polymorphisms on dabigatran pharmacokinetics in patients after total knee arthroplasty.
Patients and methods: A total of 60 patients, aged 37–81 years, who underwent surgery for knee replacement have been included in the study. VTE prophylaxis was conducted via administration of dabigatran etexilate 220 mg once daily. Genotyping for carrier state of polymorphic variants such as rs1045642 and rs4148738 of the ABCB1 gene and rs2244613 of the CES1 gene was carried out using real-time polymerase chain reaction (PCR). We also measured the peak and trough concentrations of plasma dabigatran by using high-performance liquid chromatography (HPLC).
Results: Our study revealed that TT genotype of rs1045642 polymorphism of the ABCB1 gene was associated with higher dabigatran equilibrium peak concentrations and the higher risk of bleeding than the presence of CC genotype (p<0.008). There was no statistically significant genotype-dependent difference in the trough concentrations between rs1045642 and rs4148738 of the ABCB1 gene and rs2244613 of the CES1 gene.
Conclusion: Our findings indicate that the polymorphisms of ABCB1 rs1045642 may have a prominent contribution to the safety of dabigatran in patients after knee surgery. Moreover, TT genotype may be associated with the higher risk of hemorrhagic complications in this population. There were no influence of polymorphism of ABCB1 rs4148738 and CES1 rs2244613 on dabigatran peak and through concentrations. Larger studies are needed to confirm our observations.
Keywords: new oral anticoagulants, dabigatran, venous thromboembolism, ABCB1, CES1, pharmacogenetics
Corrigendum for this paper has been published
Introduction
The current demand for total knee replacement in the Russian Federation (RF) is high, more than 300,000 surgeries per year. The need to increase knee replacement procedures in RF is linked to the increased life expectancy. Furthermore, it is in alignment with the increased frequencies of primary knee replacement procedures worldwide.1
Venous thromboembolism (VTE) in the postoperative period is one of the major complications associated with knee replacement surgery.2 Due to the growing numbers of large joint arthroplasty procedures, the demand for the administration of oral non-vitamin K oral anticoagulants (NOACs), including dabigatran, is accelerating.3
Large joint arthroplasty is associated with massive injuries of muscles and bone tissues, which may facilitate the development of major adverse vascular events (MAVEs), from which VTE is the most prevalent adverse event (AE) after knee replacement.4 NOACs, recently approved in clinical practice for prophylaxis of thromboembolic complications, have the most favorable safety profile.3 The administration of NOACs after orthopedic surgery received a significant attention recently as a strategy for the prevention of aforementioned thromboembolic complications.5 NOACs do not require parenteral administration and careful laboratory monitoring of the hemostasis, which reduces the length of hospital stay and facilitates a quick transfer of patients to outpatient clinics in the early postoperative phase. Overall, the treatment costs due to the intervention of NOACs are significantly reduced, thus supporting the advantages of NOACs compared to unfractionated heparins (UFHs), low molecular weight heparins (LMWHs), and indirect anticoagulants (e.g., warfarin).6,7
Dabigatran is a competitive, selective, reversible, direct thrombin inhibitor. Its anticoagulant effect has a linear dose-dependent and reversible nature that allows use of the drug in the fixed dose over the whole treatment period. Pharmacokinetic studies of dabigatran showed that the peak plasma concentration can be reached within approximately 1–3 hours after oral administration.8 Dabigatran etexilate is a prodrug with low bioavailability. After being absorbed, ~6.5% of dabigatran etexilate is rapidly converted into the active form of dabigatran, which is the main active metabolite of the drug, via the liver enzymes such as carboxylesterases (CEs). The human carboxylesterase-1 (CES1) gene is located predominantly in the liver, and the carboxylesterase-2 (CES2) gene is found in the small intestine. The actions of two CEs significantly differ in response to the substrate specificity. Previous studies showed that dabigatran etexilate is predominantly hydrolyzed by CES1.9
The human CES1 gene is located in 16q13-q22.1 locus.10 The human CE genetic variants were discovered more recently following the advances in the methods of DNA analysis because the application of biochemical analysis of enzyme activity in human blood was previously challenged as the levels of CE in blood could not be determined.10
Dabigatran etexilate is a substrate of P-glycoprotein encoded by the ABCB1 gene.11 Emerging evidence indicates that different genotypes of polymorphic marker C3435T ABCB1 gene are associated with different P-glycoprotein activities that can influence the pharmacokinetics of dabigatran.11
The recently conducted RE-LY trial demonstrated that the ABCB1 and the CES1 genes may have influence on the concentrations of dabigatran. In this study, genotyping and determination of dabigatran concentration were performed in 1,490 patients with atrial fibrillation (AF) and other risk factors for the development of thromboembolic complications.12 The study showed that the minor allele of the ABCB1 gene SNP, rs4148738, is associated with a 12% increase in the equilibrium peak concentration of dabigatran. Furthermore, a number of other studies indicated that P-glycoprotein inhibitors have the potential to increase the bioavailability of dabigatran by 12–23%.12,13 A recent study substantiated the adjustment of the dose of dabigatran which may be necessary for those patients who take P-glycoprotein inhibitors (such as verapamil, clarithromycin, and amiodarone) together with dabigatran, as these medications may increase the exposure of dabigatran and enhance its anticoagulation effects and increase the risk of bleeding.14
Furthermore, the RE-LY study indicated that the carrier status of the CES1 polymorphism, rs2244613, was observed in 32.8% of patients (including 29.4% of heterozygotes and 3.4% of homozygotes), which was associated with the lower concentration of the active metabolite of dabigatran. The minimal trough concentrations of dabigatran were decreased by 15% which was equivalent to a decrease in relative risk of bleeding progression by 27%. These data were adjusted by the dabigatran dose, age, gender, risk of bleeding according to CHADS2, concomitant aspirin use, and the prespecified creatinine clearance.12 Therefore, the lower risk of bleeding identified in carriers of rs2244613 polymorphism corresponded to its impact on the trough steady-state concentration of the drug.12 Moreover, the number of studies indicated that CES1 can have mutations in different alleles, which may have resulted in the decreased clearance and high blood concentration of certain drugs.15–17
Most recent studies evaluated the impact of the CES1 polymorphisms, rs2244613 and rs8192935, on dabigatran pharmacokinetics in various pathologies. Dimatteo et al18 evaluated 92 AF patients who received dabigatran. This study of rs8192935 polymorphism showed a 3% decrease and an 11% decrease in trough steady-state dabigatran concentration in heterozygotes and homozygotes with AF, correspondingly. In addition, there was a 2% and 3% decrease in the trough steady-state concentration of dabigatran in heterozygotes and homozygotes for rs2244613 polymorphism, correspondingly.18 In conclusion, the current evidence indicates that ABCB1 and CES1 gene polymorphism may play a crucial role in the individual changes of concentrations of the active metabolite of dabigatran in subjects with various prothrombotic conditions. However, the information regarding the impact of rs8192935 polymorphism on the concentrations of dabigatran and the relationship to the rate of AEs after major knee surgery is currently incomplete.
Objectives
The objectives of this study were to evaluate the influence of ABCB1 and CES1 gene polymorphisms on plasma dabigatran etexilate peak and residual concentrations in patients after total knee arthroplasty applicable to conditions of everyday clinical practice in a hospital setting.
Patients and methods
Research design and participants
This was a prospective cohort study. The study was conducted between September 2016 and November 2017 at the Saratov Scientific Research Institute of Traumatology and Orthopedics, Department of Occupational Pathology, Hematology and Clinical Pharmacology (Saratov) and the Scientific Research Centre of Russian Medical Academy of Continuous Professional Education (Moscow).
A total of 60 patients (two males and 58 females) aged 37–81 years were included in the study. Personal identifiable information (PII) about the participants in the study was not available for the research group. All the patients who underwent total knee arthroplasty (Day 1) received dabigatran etexilate at a dose of 220 mg once daily. It was initially given in the morning on the day after surgery (Day 2). Dabigatran was administered for 1 month to prevent VTE.5 A concomitant medication included 200 mg of ketoprofen once daily orally for the treatment of pain and 2.0 g of ceftriaxone once daily intravenously for the prevention of infection. None of the patients received P-glycoprotein or CE substrates. The inclusion and exclusion criteria for this study are mentioned in the following paragraphs.
Inclusion criteria were as follows: 1) male or female subjects aged 35–82 years; 2) scheduled for orthopedic surgery for total knee replacement; 3) signed informed consent.
Exclusion criteria were as follows: 1) treatment with inductors/inhibitors of P-glycoprotein within 2 weeks prior to enrollment; 2) cardiomyopathy and valvular heart disease; 3) myocardial infarction or ischemic stroke 6 months before enrollment; 4) contraindications to treatment with NOACs; 5) pregnancy and lactation; 6) known bleeding disorder; 7) concomitant systemic fibrinolytic, anticoagulant, or antiplatelet therapy; 8) other conditions, based on the investigator’s opinion, which may prevent the subject from adhering to procedures.
The duration of the hospital stay lasted up to 10 days. Subjects received physical therapy for 1 month following the surgery. The frequency of AEs was monitored for 10 weeks via phone calls conducted by personnel.
The concentration of dabigatran etexilate was determined in the plasma of all patients on Day 5 after the total knee arthroplasty. To determine the concentration of the drug, venous blood was sampled into vacuum tubes with an EDTA-K3 Improvacuter (Guangzhou Improve Medical Instruments Co., Ltd, Guangzhou, China) with a capacity of 6 mL. The first blood sample was collected from each patient before the administration of 220 mg of dabigatran etexilate. The second blood sample was collected 3 hours after the drug was administered. Plasma was obtained via centrifugation (Armed, Moscow, Russia) for 15 minutes at 4,000 rpm and was quickly cryopreserved at -40°C. The samples were stored until analysis.
Plasma concentration of dabigatran was measured by chromatography–mass spectrometric analysis using high-performance liquid chromatography (HPLC; Agilent G1978B Multimode Source for 6410 Triple Quad LC/MS; Agilent Technologies, Santa Clara, CA, USA). Quantitative determination of dabigatran in human plasma samples was performed by HPLC–tandem mass spectrometry. Sample preparation was carried out by the precipitation of plasma proteins with acetonitrile.19 Separation of the compounds was carried out using the Acquity UPLC BEN C18 (2.1 mm × 50 mm, 1.7 μm; Waters Corporation, Milford, MA, USA) chromatography column in a gradient elution mode at a flow rate of 0.4 mL/min.
Determination of ABCB1 and CES1 polymorphisms
Venous blood in the volume of 4 mL was collected with vacuum system Vacuette (Greiner Bio-One, Kremsmünster, Austria) into test tubes with K3 EDTA and was used for the molecular genetic analysis. DNA extraction was performed using the kit of DNA – EKSTRAN-1 for genomic DNA extraction from the whole blood (ZAO Sintol, Moscow, Russia). CES1 gene polymorphic marker (rs2244613) carrier status was determined by real-time polymerase chain reaction (PCR) using the commercial kit GenTest CES1 (OOO Nomotek, Moscow, Russia). Amplification program included incubation at 95°C for 3 minutes, then denaturation at 95°C for 10 seconds and annealing at 60°C – for 30 seconds repeating 50 cycles in the same manner. The determination of the fluorescent signal was conducted using the predetermined channels: carboxyfluorescein (FAM), hexachloro-fluorescein (HEX) separately or FAM and HEX simultaneously. As per the manufacturer’s instructions, genotyping was performed utilizing the amplifier Real-Time CFX96 Touch (Bio-Rad Laboratories Inc., Hercules, CA, USA) as described elsewhere.
Genotyping of the patients for the presence of ABCB1 gene polymorphic variant rs1045642 and rs4148738 carrier status was also carried out with the application of real-time PCR. The carriership of gene ABCB1 (rs4148738) was determined by real-time PCR using commercial kits TaqMan®SNP Genotyping Assays of Thermo Fisher Scientific (Waltham, MA, USA) and Q5® HF DNA Polymerase of New England Biolabs (Ipswich, MA, USA). The program included preliminary denaturation at 95°C, which lasted 2 minutes, 39 cycles of 15 seconds, denaturation at 95°C, and then annealing at 56°C for 1 minute.
Statistical analyses
Statistical analysis was conducted using the program StatSoft, Inc. (2011), Statistica (data analysis software system), version 10 (www.statsoft.com). To assess the differences between the groups, Mann–Whitney criteria were used. The results were considered statistically significant at p<0.05. The risk analysis has been conducted using MedCalc® version 12.5.0.0.
Data are represented as the median and range of 25–75% unless indicated otherwise.
Ethics
The study protocol was approved by the local ethics committee affiliated with Saratov State Medical University named after V.I. Razumovsky of Ministry of Health of the Russian Federation. We enrolled the patients after they provided signed patient informed consent. We carried out all the procedures with respect to the local legislation (national standard of the RF GOST R 52379-2005 [Good Clinical Practice, GCP]) and international ethics standards (World Medical Association’s [WMA] Declaration of Helsinki, the latest modifications were made on the 64th WMA General Assembly, Fortaleza, Brazil, October 2013).
Opinions regarding the minimum number of participants included in a pharmacokinetic study differ (US Food and Drug Administration Guidance for Industry: Statistical Approaches to Establishing Bioequivalence, 2001;20 Guidelines for the Evaluation of Bioequivalence of Medicines, 2011;21 and EMEA [Europe, the Middle East and Africa] Guidelines on the Investigation of Bioequivalence, 2010).22
Results
Demographics and clinical characteristics of the patients
A total of 60 patients (two males and 58 females) aged 37–81 years were enrolled in the study (Table 1). All the patients underwent total knee replacement due to the medical condition of deforming osteoarthritis.
Allele frequencies in the subjects after knee surgery who received dabigatran
Pharmacogenetic testing showed that the allele frequencies by loci for the ABCB1 rs4148738 gene were as follows: GG – 20 patients (33.3%), GA – 25 patients (41.7%), and AA – 15 patients (25%). The ABCB1 allele frequencies of the polymorphism marker, rs1045642, were as follows: CC genotype – 15 patients (25%), CT genotype – 29 patients (48.3%), and TT genotype – 16 patients (26.7%). On the other hand, the frequencies for the CES1 gene were identified as follows: 33 patients (55%) had CC genotype, 21 patients (35%) had CA genotype, and six patients (10%) had AA genotype. The distribution of all the genotypes was in agreement with the Hardy–Weinberg equilibrium (Table 2).
Influence of dabigatran concentrations of ABCB1 and CES1 polymorphisms on clinical outcomes
There were no cases of major bleeding or major thromboembolism. The AEs included minor bleedings (second degree of bleeding as per the World Health Organization [WHO] scale), including transient hematuria (n=1) and small hematomas in the surgical area (n=3). These AEs were mild and short in the duration and did not require blood transfusion to correct hemostasis. In the case of the hematuria, the drug was discontinued for 1 day and was later reintroduced without reappearance of AEs. Among thromboembolic AEs, one patient experienced deep vein thrombosis (DVT; determined by Day 3 after the surgery). Other AEs included pain and swelling in lower extremities (n=3). AE of DVT was considered a serious AE (SAE) and resulted in prolonged hospitalization. The SAE fully resolved in 6 months after the onset and required treatment with LMWH subcutaneously.
The AE of hematuria (determined on Day 3 after the surgery) was associated with the high dabigatran trough and maximum equilibrium peak concentrations (95.03 ng/mL measured before dabigatran administration) and 612.17 ng/mL (measured on Day 5). These were the highest among the concentrations determined in the patients included in this study. Most importantly, the pharmacogenetic analysis revealed that the subject with hematuria had ABCB1 rs1045642 – TT genotype. On the other hand, three cases of small hematomas were associated with average dabigatran equilibrium peak concentrations which were within the range of dabigatran concentrations of other study participants. It is essential to note that one of the patients with small hematoma had a TT genotype, and two patients with small hematomas had CT genotype of ABCB1 rs1045642 polymorphism.
Influence of ABCB1 and CES1 polymorphisms on dabigatran concentration
The pharmacokinetic study with the respect to ABCB1 rs4148738 polymorphism equilibrium peak concentrations showed that the median of equilibrium peak concentration was 218.7 (143.4–310.7) ng/mL for GG genotype, 152.6 (114.7–227.1) ng/mL for AA genotype, and 130.7 (102.2–249.1) ng/mL for GA genotype (Figure 1). The dabigatran equilibrium peak concentration did not show statistically significant differences with the respect to the ABCB1 rs4148738 polymorphism marker.
  | Figure 1 Peak plasma concentrations of dabigatran in patients after knee surgery with respect to the genotype ABCB1 rs4148738. Abbreviations: Max, maximum; Min, minimum. |
The following Cmax data were obtained when comparing the results of ABCB1 rs1045642 polymorphism dabigatran equilibrium peak concentrations: CC genotype – 124.1 (79.9–177.7) ng/mL, CT genotype – 198.4 (103.9–269.3) ng/mL, TT genotype – 291.8 (193.6–345.0) ng/mL (Figure 2). It is vital to note the importance of our findings, which indicated a statistically significant difference between CC and TT genotypes, with respect to Cmax of dabigatran (CC vs. TT, p=0.008). The analysis of sensitivity on the effect of ABCB1 rs1045642 on dabigatran concentrations remained significant after excluding the individual who had hematuria. The following Cmax data were obtained when comparing the results of ABCB1 rs1045642 polymorphism dabigatran equilibrium peak plasma concentrations (the results are calculated after exclusion of the subject who experienced AE hematuria and had the highest concentration of dabigatran): CC genotype – 124.1 (79.9–177.7) ng/mL, CT genotype – 198.4 (103.9–269.3) ng/mL, TT genotype – 243.7 (193.6–339.9) ng/mL (CC vs. TT, p=0.016).
  | Figure 2 Peak plasma concentrations of dabigatran in patients after knee surgery with respect to genotype ABCB1 rs1045642. Abbreviations: Max, maximum; Min, minimum. |
Of the 60 subjects included in our analysis, only one subject with genotype TT (out of 16 subjects with this genotype in total) had a major hemorrhage. The relative risk of major hemorrhages associated with TT genotype was 2.903 (95% CI 1.17–7.19), p=0.0214. At the same time, subjects with genotype TT experienced one major and one minor hemorrhage. Therefore, the odds ratio of major and minor hemorrhages in the subjects with genotype TT was 3.0 (95% CI 0.38–23.33), although this was insignificant (p=0.29). On the other hand, subjects with genotype CC (n=15) did not experience any hemorrhages. The relative risk of hemorrhages in the group with TT genotype vs. subjects with CC genotype was 1.72 (95% CI 0.92–3.22), which was not significant (p=0.088).
It is imperative to acknowledge that rs2244613 polymorphism of the CES1 gene is statistically significant and differences were obtained in patients under 60 years of age. Previous studies indicated that the activity of CES1 is related to aging rather than gender.17,23 Therefore, this analysis was conducted on a subset of subjects aged below 60 years (n=20). In this cohort, 10 subjects were identified as heterozygotes by allele A (CA+AA) and 10 subjects were homozygotes on allele C (CC). Peak concentration of dabigatran was found to be significantly higher (p=0.025) in subjects who were heterozygotes by allele A (118.2 [74.5–152.6] ng/mL) compared to concentrations in subjects with phenotype CC (361.3 [155–528] ng/mL).
In this study, we did not find statistically significant differences in dabigatran equilibrium peak concentration with the respect to gene CES1 rs 2244613 polymorphism (Figure 3).
  | Figure 3 Peak plasma concentrations of dabigatran in patients after knee surgery with respect to genotype CES1 rs2244613. Abbreviations: Max, maximum; Min, minimum. |
Conversely, we detected a statistically significant decrease in dabigatran equilibrium peak concentration in the group of patients under the age of 60 years in minor A allele homozygote (p<0.05). This observation can potentially contribute to the weak effect of dabigatran in minor A allele homozygotes.
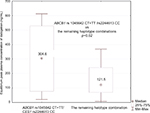
Analysis of haplotype combinations of the both polymorphisms revealed that the most abundant haplotype combination (n=23, 38.3%) ABCB1 (rs1045642 CT+TT)/CES1 (rs2244613 CC) is significantly associated with higher dabigatran equilibrium peak concentration – 304.6 (76.5–612.2) ng/mL compared to the set of the remaining haplotype combinations (n=37, 61.7%) – 121.5 (69.1–241.0) ng/mL (p=0.02; Figure 4).
Likewise, we did not discover statistically significant differences in dabigatran trough concentrations pertaining to polymorphisms, rs1045642 and rs4148738, of the ABCB1 gene and rs2244613 of the CES1 gene. The highest trough concentration was found in patients with AA genotype of the CES1 rs2244613 – 34.6 (32.2–36.9) ng/mL and TT genotype of the ABCB1 rs1045642 – 25.3 (13.0–76.4) ng/mL. On the other hand, the lowest trough concentration was detected in patients with CC genotype of the CES1 rs2244613 – 17.1 (12.0–25.4) ng/mL and CC genotype of the ABCB1 rs1045642 – 18.9 (11.8–25.4) ng/mL (Figure 5).
  | Figure 5 Trough plasma concentrations of dabigatran with respect to genotype ABCB1: (A) rs1045642; (B) rs4148738; (C) CES1 rs2244613. Abbreviations: Max, maximum; Min, minimum. |
Discussion
Our study showed that TT genotype of rs1045642 polymorphism of the ABCB1 gene is associated with higher dabigatran equilibrium peak concentration and higher risks of bleeding than in the cases of CC genotype. This important observation was obtained in everyday clinical practices pertaining to orthopedic surgery in subjects who received dabigatran for the prevention of DVT. The major finding of the study highlights the significant influence of rs1045642 polymorphism of the ABCB1 gene on dabigatran concentrations in these subjects. Furthermore, rs2244613 polymorphism of the CES1 gene displays significant differences obtained in patients under 60 years of age.
We studied the pharmacogenetics and the pharmacokinetic properties of an NOAC dabigatran in the clinical practice of patients after knee surgery, which were compared to the outcomes of the other pharmacogenetic trials conducted using dabigatran for other indications. Our data verified and validated the previous findings of gene polymorphisms associated with dabigatran pharmacokinetic properties found in the RE-LY trial.12
It is widely accepted in the scientific community that CES gene encodes enzyme CE-1 in the liver which is responsible for the biotransformation of dabigatran etexilate into the active metabolite dabigatran.9 Previous studies have shown that SNPs, rs2244613, of the CES1 gene, rs2244613 and rs8192935, of the ABCB1 gene have an impact on dabigatran trough and equilibrium peak concentrations.12
Previous studies indicated that P-glycoprotein, ATP-dependent drug efflux pump for xenobiotic compounds with wide substrate specificity is also encoded by the ABCB1 gene.24 On the other hand, dabigatran etexilate is the substrate of P-glycoprotein. Earlier studies indicated that the presence of ABCB1 SNPs, rs4148738 and rs1045642, may influence dabigatran equilibrium peak concentration.11
Different haplotype combinations of both polymorphisms of ABCB1 (rs1045642) and CES1 (rs2244613), can lead to augmentation of their effects on the concentration of dabigatran in the blood. Thus, certain haplotype combinations can be of great importance for the clinical practice. Likewise, the ABCB1 (rs1045642 CC)/CES1 (rs2244613 AA) and ABCB1 (rs1045642 TT)/CES1 (rs2244613 CC) P-glycoprotein may also require additional attention, as they may influence the peak and the trough concentrations of dabigatran. It is plausible that combinations of polymorphisms of ABCB1 (rs1045642 CC)/CES1 (rs2244613 AA) and ABCB1 (rs1045642 TT)/CES1 (rs2244613 CC) may influence how dabigatran activates from the prodrug and how it is absorbed in the small intestine. These gene polymorphisms have the potential to influence the pharmacological effect of the drug; however, this hypothesis remains to be confirmed in the future studies.
Our findings support the importance of assessments associated with genetic factors on dabigatran concentration. The added value of this study is rooted in the administration of dabigatran, and assessments of the genetic polymorphisms were conducted in the orthopedic surgical patients in real clinics. Limitations include the selection of specific study populations, such as excluding the subjects with known bleeding disorders and those who received systemic fibrinolytic therapy or anticoagulants or antiplatelets. Consequently, the conclusions of our study do not apply to the abovementioned populations which were excluded due to limitations of the study. Additional limitations include a restricted number of polymorphisms evaluated, small sample size, and variability of pharmacokinetic parameters. The most likely cause in the variability of aforementioned parameters is the difference in characteristics of patient population. The sample size was too small to evaluate the relationship between ABCB1 and CES1 polymorphism and the risk of bleeding after the use of dabigatran. Subgroup analysis in subjects under the age of 60 years is justified by the known influence of age on the activity of CES1. Likewise, the study was not randomized and was a single-center study, which may have introduced a selection bias. On the other hand, the study was conducted on a group of subjects admitted from broad areas of rural and city settlements which may prove to enrich the study population and therefore may be used as a reference for clinicians who are using dabigatran in the clinical practice.
Only few studies are currently underway which are looking further into NOAC therapies and pharmacogenetic markers that could be associated with them. Our search on www.clinicaltrials.gov resulted in two small completed and one ongoing clinical trials. One of the studies investigated a relationship between seven polymorphisms of ABCB1 (rs4148738, rs2235046, rs1128503, rs10276036, rs1202169, rs1202168, rs1202167) and the drug plasma concentrations in a prospective single-center study on subjects with major bleeding or thromboembolic event occurring under treatment with NOACs (rivaroxaban, apixaban, or dabigatran) with the total sample size of 90 subjects (NCT02103101). Another single-center study examined the influence of genetic factors on area under the curve (AUC) of NOACs (dabigatran and rivaroxaban) separately and after coadministration of antibiotic clarithromycin in 64 healthy volunteers (NCT01627665). The results of both of the completed studies are not yet available. One ongoing single-center study is investigating the influence of CYP3A4, CYP3A5, CYP3A7, and ABCB1 single nucleotide polymorphism in subjects with AF, DVT, and pulmonary embolism who are receiving rivaroxaban and apixaban (n=350). The search did not reveal any pharmacogenomic studies analyzing polymorphisms of gene CES1 in subjects with NOAC therapy.
In the future, an increase in the number of patients in need of knee arthroplasty will lead to an increase in the quality and effectiveness of prevention of thromboembolic complications. Therefore, the continuation of studies has the potential to optimize anticoagulant therapy with an NOAC, ensuring safety and lowering bleeding risks in different groups of patients, especially in the elderly.
In the future, when prescribing dabigatran, physicians may need to consider not only the age, gender and kidney function, but also the genetic traits which may prominently influence dabigatran pharmacokinetics and pharmacodynamics. Polymorphisms of the ABCB1 and CES1 genes are among the candidates which may be utilized in future pharmacogenetic testing while prescribing dabigatran for DVT prophylaxis.
Conclusion
Bleeding remains a serious undesirable problem when using oral anticoagulants. Our study indicates that polymorphisms of ABCB1 SNP, rs1045642, may have a prominent contribution to the safety of dabigatran in patients after knee surgery. Our findings have confirmed the need to continue exploring new genetic traits which may impact pharmacokinetic and pharmacodynamic properties of NOACs.7
Acknowledgments
This study was supported by Russian Science Foundation, project 16-15-00227 “Conducting fundamental scientific research and exploratory research on priority thematic research areas”. The funding organization played no role in the study design, collection, analysis and interpretation of data, writing of the report, or decision to submit the report for publication.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Borisov DB, Kirov MY. Endoprosthesis replacement of hip and knee joints: epidemiological aspects and effect on quality of life. Hum Ecol. 2013;(8):52–57. | ||
Shevchenko YL, Stoyko YM, Zamyatin MN, et al. Multimodal prevention of venous thromboembolic complications after total hip and knee joint endoprosthesis. Meditsinskiy Sov. 2014;2:8–12. | ||
Diacov I. New oral anticoagulants – a place in the domestic pharmaceutical market. Remedium Period Pharm Med Equip Mark. 2014;(11):42–43. | ||
Kouzmin II, Akhtiamov IF, Sorokin VA. Thromboembolic complications in the hip endoprosthetics. Orthop Genius. 2004;(4):63–68. | ||
Bokeria LA, Zatevachin II, Kirienko AI, et al. Russian clinical guidelines for the diagnosis, treatment and prevention of venous thromboembolic complications (VTEC). Flebologia. 2015;4(2):1–52. | ||
Zhirova TA, Zubkov EA, Reino EV, Bogatkin AA, Kuznetsova OA, Mashinskaya TM. Venous thromboses prevention in orthopedics. Recommendations and real practice. 2012;3:142–144. | ||
Bozhkova SA. Specificity of anticoagulant choice for VTE prophylaxes after major orthopedic surgery – the view of clinical pharmacologists. Traumatol Orthop Russ. 2011;1(59):1–6. | ||
Instructions on Medical Use of a Medicinal Product PRADAXA. 2016. Available from: https://www.boehringer-ingelheim.ru/file/27473/download?token=VfNA1RPy. Accessed May 31, 2018. | ||
Kurdyukov ID, Shmurak VI, Nadeyev AD, Voitenko NG, Prokofyeva DS, Goncharov NV. «Esterase status» of the organism at exposure to toxic substances and pharmaceutical preparations. Toxicol Rev. 2012;(6):6–12. | ||
Lockridge O, Quinn DM. 4.14 – Esterases. In: McQueen CA, ed. Comprehensive Toxicology (Second Edition). Kidlington, UK: Elsevier Ltd; 2010:243–273. | ||
Sychev DA, Kryukov AV, Tereshchenko OV. Pharmacogenetic aspects of new oral anticoagulants application. Ration Pharmacother Cardiol. 2017;13(3):416–421. | ||
Paré G, Eriksson N, Lehr T, et al. Genetic determinants of dabigatran plasma levels and their relation to bleeding. Circulation. 2013;127(13):1404–1412. | ||
Liesenfeld KH, Lehr T, Dansirikul C, et al. Population pharmacokinetic analysis of the oral thrombin inhibitor dabigatran etexilate in patients with non-valvular atrial fibrillation from the RE-LY trial. J Thromb Haemost. 2011;9(11):2168–2175. | ||
Gilyarov MY. Dabigatran: how to select an optimal dose in clinical practice? J Arrhythmol. 2012;(69):77–80. | ||
Shi J, Wang X, Nguyen JH, et al. Dabigatran etexilate activation is affected by the CES1 genetic polymorphism G143E (rs71647871) and gender. Biochem Pharmacol. 2016;119:76–84. | ||
Zhu HJ, Appel DI, Johnson JA, Chavin KD, Markowitz JS. Role of carboxylesterase 1 and impact of natural genetic variants on the hydrolysis of trandolapril. Biochem Pharmacol. 2009;77(7):1266–1272. | ||
Zhu HJ, Markowitz JS. Activation of the antiviral prodrug oseltamivir is impaired by two newly identified carboxylesterase 1 variants. Drug Metab Dispos. 2009;37(2):264–267. | ||
Dimatteo C, D’Andrea G, Vecchione G, et al. Pharmacogenetics of dabigatran etexilate interindividual variability. Thromb Res. 2016;144:1–5. | ||
Biophen® Dabigatran Calibrator Low; 2014. Available from: https://www.aniara.com/mm5/PDFs/IFU/INS-A222901-RUO.pdf. Accessed May 31, 2018. | ||
U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER). Guidance for Industry Establishing Bioequivalence Guidance for Industry Statistical Approaches to. Vol. 4. Rockville, MD; 2001. | ||
Vasilenko GF, Davydova KS, Krasnykh LM, Savchenko YA, Shohin IE. Methodological Recommendations for Drug Manufacturers on in Vitro Equivalence Test for Generic Drug Products according to Biowaiver Procedure (DRAFT). Moscow: Federal Service on Surveillance in Healthcare and Social Development; 2010. | ||
European Medicines Agency. Guideline on the Investigation of Bioequivalence. EMEA, ed. London: 2018. | ||
Zhu H, Appel DI, Jiang Y, Markowitz JS. Age- and sex-related expression and activity of carboxylesterase 1 and 2 in mouse and human liver. Drug Metab Dispos. 2009;37(9):1819–1825. | ||
Shulkin AV, Yakusheva EN, Popova NM. The role of P-glycoprotein in rational pharmacotherapy in cardiology. Ration Pharmacother Cardiol. 2013;9(6):701–707. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.