Back to Journals » Clinical Epidemiology » Volume 14
The Global Burden of Appendicitis in 204 Countries and Territories from 1990 to 2019
Authors Yang Y, Guo C, Gu Z, Hua J, Zhang J, Qian S, Shi J
Received 30 June 2022
Accepted for publication 1 December 2022
Published 13 December 2022 Volume 2022:14 Pages 1487—1499
DOI https://doi.org/10.2147/CLEP.S376665
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eyal Cohen
Yongping Yang, Chengjun Guo, Zhaoxuan Gu, Junjie Hua, Jiaxuan Zhang, Siyu Qian, Jian Shi
Department of General Surgery, the Second Hospital of Jilin University, Changchun, People’s Republic of China
Correspondence: Jian Shi, Department of General Surgery, the Second Hospital of Jilin University, Changchun, People’s Republic of China, Email [email protected]
Objective: Appendicitis is a common surgical emergency. This study aimed to estimate the worldwide burden and trends of appendicitis from 1990 to 2019.
Methods: Data on appendicitis were derived from the Global Burden of Disease 2019. Incidence and disability-adjusted life-years (DALYs) data were analyzed at global, regional, and national levels and stratified by sex, age, and socio-demographic index. The estimated annual percentage change and relative change were used to assess changing trends. Pearson’s correlation test was used to assess the correlation between different measures.
Results: Global incidence grew by 63.55% between 1990 and 2019, age-standardized incidence rate climbed by an estimated percentage change of 0.58 per year, whereas the number of DALY declined by 31.93% during the same period, with an estimated annual percentage change of − 2.77. In 2019, the areas of Andean Latin America and the Caribbean had the highest age-standardized rates of incidence and DALYs. While South Asia saw the largest increase in age-standardized incidence rates, Andean Latin America saw the biggest decline in age-standardized rates of incidence and DALYs. At the national level, Bangladesh, Bhutan, and Peru were the top three countries in terms of age-standardized incidence rates in 2019, and Honduras, Haiti, and the Central African Republic held the highest age-standardized DALY rates. Ethiopia experienced the most age-standardized incidence rate increase, and Peru saw the largest decline in age-standardized rate of incidence and DALYs. Significant negative correlations between age-standardized DALY rates and socio-demographic index, between estimated annual percentage change and age-standardized incidence rates, were observed at the national level.
Conclusion: Appendicitis remains a major global health concern. Although the trends in DALYs decreased, the burden of incidence increased from 1990 to 2019. Policymakers should create health policies adapted to local conditions to manage the burden of appendicitis globally.
Keywords: appendicitis, global burden, incidence, disability-adjusted life-years, socio-demographic index
Introduction
Appendicitis is one of the most common surgical emergencies globally and imposes an important burden on modern health systems.1 Because it is very common among adults and children worldwide, previous studies of appendicitis epidemics have mainly focused on incident cases. Although the pooled incidence of the disease has been decreasing in high-income regions and countries since the 1990s, it has increased in newly industrialized countries.2–4 While appendicitis is also associated with the risk of morbidity and mortality, disability-adjusted life-years (DALYs), a comprehensive measurement of premature mortality and disability, is a meaningful measure that should be analyzed across geographical areas.
The Global Burden of Disease (GBD) study has estimated a variety of metrics for diseases annually since 1990 and provides a great opportunity for comparable assessments of disease burden and trends at the global, regional, and national levels; however, no study addressing these data on appendicitis has been published.5,6 A systematic review and meta-analysis reported the incidence of appendicitis in Western countries and several other industrialized countries; however, this study did not report data on mortality and morbidity rates. Additionally, the association between the burden of appendicitis and the socio-economic development of countries, age distribution, and sex differences were also not mentioned.4 Studies that have reported the association between socio-economic status and the incidence and severity of appendicitis, in which areas with a lower socio-economic status have much more incidence cases and perforation rates compared to areas with a high socio-economic status, have only used statewide or nationwide data sets.7–9 Other studies dealing with the epidemiology of appendicitis based on sex and age were also statewide or nationwide population-based studies.10–12 A study on appendicitis burden referring to the incidence and DALYs at the global level is needed.
In this study, using the data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2019 (GBD 2019), we analyzed the appendicitis burden of incidence and DALYs at the global, regional, and national levels stratified by sex, age, and SDI and in terms of numbers and age-standardized rates (ASRs) from 1990 to 2019. A burden and trend report for different countries and regions will help improve health care administration for appendicitis.
Materials and Methods
Data Source
Data on appendicitis burden were collected from the GBD 2019, which systematically analyzed 369 diseases and injuries, 87 risk factors for 204 countries and territories, and 21 regions from 1990 to 2019.5,6 In the GBD 2019, the countries or territories were classified into five regions, namely, low, low-middle, middle, high-middle, and high, in terms of the socio-demographic index (SDI), and the world was also geographically divided into 21 regions. In this study, data on appendicitis burden were mainly considered in terms of incidence and disability-adjusted life years (DALYs). Data on these appendicitis parameters were derived using the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool).13 Appendicitis burden data (rates, number of cases) on incidence and DALYs were extracted according to sex, age, SDI areas, geographic regions, and countries/territories from 1990 to 2019, without any inclusion or exclusion criteria. This study adhered to the guidelines for accurate and transparent health estimates reporting (GATHER) statements.14
Statistical Analysis
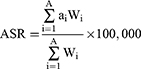
In this study, the incidence and DALYs number in 204 countries and territories with 95% uncertainty intervals (UIs) were used. To compare populations with different age structures or the same population with changing age structures in different time periods, data were standardized by applying age-specific rates. The age-standardized rate (ASR) did not reflect the actual case number, but was only used to compare the appendicitis burden in different countries, different regions, or different historical periods in the same region, so as to facilitate data comparisons. The method used to calculate ASR has been reported previously.15,16 Age-standardized rates of incidence and DALYs with 95% UIs were calculated using the following formulae:
Where ai is the age-specific rate in the ith age group, w is the number of people (or weight) in the ith age group from among the selected standard population, and A represents the number of age groups.
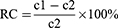
The relative changes (RC) and estimated annual percentage changes (EAPC) with 95% confidence intervals (CIs) were used to quantify the trends of appendicitis from 1990 to 2019. The relative changes are defined as follows:
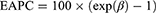
Where c1 represents the number or ASR in 2019 and c2 represents the number or ASR in 1990.17 The EAPC is a widely accepted index for quantifying and describing trends in ASR.18 EAPC was estimated using a linear regression model that was fitted to the natural logarithm of the ASR.19 The formulae are as follows:
Where y = ln (ASR), x is the calendar year, ε represents error term. These trends were assessed as follows: 1) ASR was considered to show an increasing trend with EAPC, and its 95% CI > 0; and 2) ASR was considered to have a decreasing trend with EAPC, and its 95% CI < 0.15
The Wilcoxon signed-rank test was used to compare sex differences in the global burden for different age groups.20 The Wilcoxon signed rank test is a non-parametric statistical hypothesis test used to determine if the population mean ranks of two related samples, matched samples, or repeated measurements on a single sample vary.21,22 The correlation between ASRs and SDI values and EAPC was assessed using a Pearson’s correlation test model. And An R of −1 indicates a perfect negative linear relationship, an R of 0 indicates no linear relationship, and an R of 1 indicates a perfect positive linear relationship between variables.21 In this study, data were analyzed using the R program (Version 3.6.3), and a p-value of < 0.05 was considered statistically significant.
Results
Appendicitis Burden at the Global Level
In 2019, there were 17.70 million (95% UI: 14.10–22.32) new cases of appendicitis globally, with an age-standardized incidence rate (ASIR) of 229.86 (95% UI: 180.88–291.0) per 100,000 population (Figures 1A and S1A, Table 1). The incidence increased by 63.55% (95% UI: 58.25–69.45%) and ASIRs increased with an EAPC of 0.58 (95% CI: 0.44–0.71) from 1990 to 2019. Globally, there were 1.50 million (95% UI: 1.24–1.71) DALYs attributed to appendicitis in 2019, representing a decrease of 31.93% (95% UI: –45.59 to –1.88%) from 1990 to 2019 (Figure S1B, Table 2). The global age-standardized DALY rate of appendicitis was 19.35 (95% UI: 15.92–21.98) per 100,000 population in 2019, which represents a decreasing EAPC of –0.77 (95% CI: –2.84 to –2.7) from 1990 to 2019 (Figure 1B and Table 2).
 |
Table 1 The Burden and Trends on Incidence of Appendicitis from 1990 to 2019 |
 |
Table 2 The Burden and Trends on Disability-Adjusted Life-Years (DALYs) of Appendicitis from 1990 to 2019 |
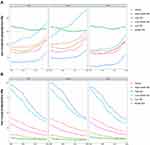 |
Figure 1 The age-standardized incidence (A) and disability-adjusted life-year (DALY) (B) rates of global appendicitis burden for sexes and socio-demographic index (SDI) quintiles, 1990–2019. |
Appendicitis Burden According to SDI Level
In 2019, the highest ASIR was observed in the low-middle SDI quintiles (283.10 [95% UI: 227.24–354.20] per 100,000 population) among all SDI regions, whereas the lowest ASIR was observed in the low SDI quintiles (168.76 [95% UI: 133.50–214.04] per 100,000 population). From 1990 to 2019, the number of incident cases increased across all SDI quintiles. Among them, the low SDI regions had the greatest increase in incident cases (1.75-fold). Analysis of ASIR according to SDI quintiles showed increasing trends in all SDI areas, except high SDI regions, over the study period. From 1990 to 2019, the sharpest increase in ASIR was also observed in the low-middle SD quintiles, which exhibited an EAPC of 1.05 (95% CI: 0.96–1.14), while the high SDI area had an EAPC of –0.15 (95% CI: –0.2 to –0.1) (Figure 1A and Table 1).
The highest rate of age-standardized DALYs in 2019 was observed in the low SDI quintiles (39.82 [95% UI: 28.82–51.56] per 100,000 population), and the lowest was observed in the high SDI quintiles (5.69 [95% UI: 4.45–7.14] per 100,000 population). The number of DALYs decreased in all SDI quintiles over the study period, with middle SDI regions holding the most pronounced decrease (0.34-fold). A decreasing trend in the age-standardized DALY rates over the study period was observed in all SDI quintiles, and the steepest decreasing trend was found in the low-middle SDI quintiles (EAPC: –3.37 [95% CI: –3.48 to –3.27]) (Figure 1B and Table 2).
Appendicitis Burden Affected by Sex and Age
In 2019, the burden of incidence and DALYs were higher for women globally (Figure 1, Tables 1 and 2). The Wilcoxon test showed significant differences between sexes in the global incidence burden of numbers and rates among different age groups (p < 0.05). Although the number of incident cases and incidence rate all peaked in the 15 to 19 age group for both females and males, the number of incident cases was higher for females in all groups except in the 1 to 4 and 30 to 39 age groups, and incidence rates were higher in females in the age groups younger than 70 years (Figure 2A and B). No statistically significant difference in DALYs between women and men according to age group was observed in 2019. The number of DALY for both sexes and the DALY rates for females also peaked in the 15–19 age group in 2019, while the DALY rate for males increased with age, peaking in the 90–94 age group (Figure 2C and D).
Appendicitis Burden at the Regional Level
In 2019, the highest ASIRs were observed in Andean Latin America (852.38 [95% UI: 697.66–1059.42] per 100,000 population), high-income Asia Pacific (448.09 [339.75–572.27] per 100,000 population), and Central Latin America (358.22 [271.11–460.12] per 100,000 population). Andean Latin America has a much higher ASIR than other regions throughout the past three decades. The lowest ASIRs were observed in Oceania (109.19 [85.02–140.31] per 100,000 population), Western Sub-Saharan Africa (120.12 [89.74–158.90] per 100,000 population), and Eastern Sub-Saharan Africa (127.0 [96.73–166.87] per 100,000 population). From 1990 to 2019, the number of incident cases increased across all regions except high-income Asia Pacific, Central Europe, and Eastern Europe. Western sub-Saharan Africa had the highest increase in incident cases (2.62-fold). Increasing trends of ASIR were also observed in most geographic regions from 1990 to 2019, of which the most pronounced was Southern Latin America (EAPC: 1.45 [95% CI: 1.32–1.57]). In contrast, only three regions exhibited downward trends in ASIR, including Andean Latin America (EAPC: –1.87 [95% CI: –2.27 to –1.47]), high-income North America (EAPC: –0.4 [95% CI: –0.51 to –0.3]), and high-income Asia Pacific (EAPC: –0.12 [95% CI: –0.2 to –0.04]) from 1990 to 2019 (Table 1).
In 2019, the Caribbean had the highest age-standardized DALYs rates (43.30 [95% UI: 30.29–61.73] per 100,000 population), whereas East Asia had the lowest age-standardized DALYs rate (4.37 [3.50–5.41] per 100,000 population). During the study period, the number of DALYs decreased in most of the geographic regions. Among them, Andean Latin America had the greatest decrease of 80.99% (95% UI: –86.59 to –71.48%). Downward trends in age-standardized DALYs rates were observed in all geographic regions from 1990 to 2019, especially in Andean Latin America (EAPC: –6.92 [95% CI: –7.73 to –6.1]), East Asia (EAPC: –4.84 [95% CI: –5.03 to –4.65]), and Central Asia (EAPC: –4.01 [95% CI: –4.39 to –3.63]) (Table 2).
Appendicitis Burden at the National Level
The top three countries in terms of appendicitis ASIR in 2019 were Bangladesh (1349.82 [95% UI: 1092.20–1673.12] per 100,000 population), Bhutan (1174.42 [942.11–1459.63] per 100,000 population), and Peru (879.70 [95% UI: 687.99–1137.55] per 100,000 population). In contrast, Ethiopia (53.78 [95% UI: 38.75–73.33] per 100,000 population), Kenya (65.41 [95% UI: 47.39–88.72] per 100,000 population), and Indonesia (92.53 [95% UI: 68.72–121.79] per 100,000 population) had the lowest ASIRs in 2019 (Figure 3A and Table S1). At the national level, the most pronounced changes in incident cases from 1990 to 2019 were observed in Qatar (increase, 904.21% [95% UI: 823.83–999.03%]) and Bosnia and Herzegovina (decrease, –39.75% [95% UI: –44.45 to –34.11%]) (Figure 3B and Table S1). The changes in ASIRs from 1990 to 2019 varied greatly between countries, with the highest increases in Ethiopia (EAPC: 3.74 [95% CI: 2.61–4.87]), Nigeria (EAPC: 2.72 [95% CI: 2.12–3.32)]), and India (EAPC: 2.44 [95% CI: 1.8–3.09)]; and greatest decreases in Peru (EAPC: –2.81 [95% CI: –3.37 to –2.24]), Guatemala (EAPC: –2.09 (95% CI: –2.72 to –1.46]), and El Salvador (EAPC: –1.72 [95% CI: –2.24 to –1.21]) (Figure 3C and Table S1).
The top three countries in terms of appendicitis-associated age-standardized DALY rates in 2019 were Honduras (80.91 [95% UI: 56.97–112.85] per 100,000 population), Haiti (80.82 [95% UI: 32.64–137.78] per 100,000 population), and the Central African Republic (78.82 [95% UI: 27.05–137.34] per 100,000 population). In contrast, the lowest age-standardized DALYs rates were in the Maldives (3.63 [95% UI: 2.48–5.25] per 100,000 population), Northern Mariana Islands (95% UI: 3.79 [3.01–4.82] per 100,000 population), and Cyprus (3.89 [95% UI: 2.91–5.19] per 100,000 population) (Figure S2A and Table S2). Similarly, the most pronounced changes in the number of DALYs from 1990 to 2019 were also observed in Qatar (increase, 489.18% [95% UI: 251.42–909.11%]) and Peru (decrease, –88.47% [95% UI: –92.62 to –80.74%]) (Figure S2B and Table S2). The age-standardized DALY rates showed a decreasing trend in all countries except Zimbabwe, Fiji, Georgia, Mexico, and Greenland over the study period. The DALY rates of Peru (EAPC: –8.7 [95% CI: –9.76 to –7.62]), El Salvador (EAPC: –6.48 [95% CI: –7.69 to –5.26]), and Guatemala (EAPC: –6.32 [95% CI: –7.03 to –5.61]) decreased most rapidly (Figure S2C and Table S2).
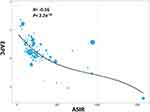
Correlation Between ASRs and Both SDI and EAPC
Overall, a slightly positive correlation was found between ASIR and SDI in global regions from 1990 to 2019, while a prominent negative correlation was observed between age-standardized DALY rates and SDI (Figure 4A and B). Andean Latin America, High-income Asia Pacific, Central Latin America, and Central Sub-Saharan Africa showed higher than expected levels of ASIR during the study period, while Andean Latin America and the Caribbean showed higher than expected levels of age-standardized DALY rates. Similarly, a slightly positive correlation between ASIR and SDI and a significant negative correlation between age-standardized DALY rates and the SDI were observed at the national level, suggesting a higher incidence burden but a lower DALY burden with higher socio-economic development (Figure 4C and D). In addition, a negative correlation between EAPC and ASIR was found, which indicated that appendicitis cases increased more rapidly in lower-incidence countries than in higher-incidence countries (Figure 5).
Discussion
This study analyzed the substantial burden of appendicitis worldwide over the past three decades. We reported the overall and age-standardized appendicitis incidence and DALY burden at the global, regional, and national levels from 1990 to 2019. Although DALYs decreased over the study period, the burden of incidence increased. Globally, the incidence of new cases was 17.70 million, and the ASIR was 229.86 per 100,000 population in 2019, both increasing from 1990. The number of DALYs was 1.50 million and the ASR of DALYs was 19.35 per 100,000 population in 2019, both decreasing from 1990.
The increased burden of incidence from 1990 to 2019 may be related to population growth, whereas the decreased number and rate of DALYs reflected an improvement in medical management and treatment, especially in diagnosis and operation. In recent years, the use of imaging and scoring systems has improved the efficiency of clinical diagnosis, which will not delay treatment and add the risk of perforation.23 As phlegmonous and gangrenous appendicitis seem to be separate entities, one of which may resolve spontaneously and another that progresses to gangrene and perforation, diagnostic improvements in CT and the application of artificial intelligence and advanced combinatorial tools for distinguishing these two entities, especially in middle-income countries, helped in choosing treatment and reduced the perforation rate and adverse events.24–27 Surgical advances have begun to reduce complications, and the promoted laparoscopic appendectomy is reported to be associated with a lower incidence of wound infection and post-intervention morbidity, shorter hospital stay, and better quality of life scores than open appendectomy.28–30 In addition, endoscopic retrograde appendicitis therapy, which is a new and minimally invasive technique, has emerged as a promising non-invasive treatment for acute uncomplicated appendicitis.31 Compared to laparoscopic appendectomy, endoscopic retrograde appendicitis therapy holds the advantages of rapid postoperative abdominal pain relief, preservation of the appendix, fast recovery, and a lower rate of adverse events for acute uncomplicated appendicitis patients.32
Differences were found between different age groups and sexes. We found that the incidence rate was significantly higher in the 15–19 year age group, which is similar to that reported in previous studies that appendicitis is most common between the ages of 10 and 20 years.33,34 In addition, the burden for females was heavier than that of males, and ASIRs were higher for females under 70 years of age. As previous studies reported that the appendicitis incidence rate was higher in males even with a male to female ratio of 1.4:1, they all drew conclusions from data from the United States, while this study made the analysis at the global level.10,33 We found that older individuals, especially older males, have increasing DALY rates with increasing age. As appendicitis in the elderly is associated with higher rates of complicated appendicitis, morbidity, and mortality, the DALY rate has increased.35–37
At the regional level, Andean Latin America had the highest ASIRs and the steepest decrease in ASIR from 1990 to 2019. The ASIR in this region was far higher than those of other regions across the three decades. The three countries in this region, Peru, Ecuador, and Bolivia, all had high ASIRs. Other Latin American regions, such as Central and Southern Latin America, also had high ASIRs. Geographic and ethnic variations in appendicitis incidence have been reported in previous studies.33,38,39 Appendicitis was less common in non-white groups than in white and Hispanic individuals.40 A Swedish cohort study on immigrant populations and international adoptees reported that individuals of South American origin have the highest appendicitis incidence rate compared to individuals from other regions, which is in accordance with our findings.41 Although the reasons for the geographical and ethnic differences are not known, environmental and genetic differences may partially explain this. Studies have reported a predominantly seasonal incidence rate of acute appendicitis during the summer, which may be statistically associated with ambient temperature.42 Individuals with a family history of appendicitis tend to have an increased risk for appendicitis.43 A multi-institutional genome-wide association study identified SNVs within the NEDD4L gene as being associated with acute appendicitis, which presented individuals with a genetic predisposition.44
This study provides several novel insights. First, we conducted a comprehensive analysis of the appendicitis burden and global trends. While there have been nationwide studies on appendicitis epidemics, worldwide reports are lacking. Although there has been a systematic review of population-based studies reporting the incidence of appendicitis across the world, it only mentioned several regions and could not evaluate the burden in 204 countries and territories.4 Moreover, it only analyzed incidence. Second, we investigated the association between the burden of appendicitis and SDI using regression modeling instead of just presenting estimates separately for each SDI quintile. A positive association between ASIR and SDI quintiles was found, which differs from previous reports.7–9 As this study dealt with global data, it may be influenced by environmental and ethnic factors compared to previous reports that only dealt with statewide or nationwide burdens. Our findings of a negative association between SDI and DALYs, in accordance with the analysis that the highest age-standardized DALYs were observed in the low SDI quintiles and the lowest age-standardized DALYs were observed in the high SDI quintiles, which reflected great variation in the presentation, severity of disease, diagnosis, and surgical management of patients related to country socio-economic status.45 This result may be due to better healthcare and treatment conditions in high SDI regions and countries. Although the highest age-standardized DALY rates occurred in the low-middle and low SDI regions during this study period, there was still an improvement in the management and treatment of appendicitis, leading to the steepest decrease in these regions.
This study has some limitations. First, the quality and quantity of the input data used in the DisMod-MR 2.1 model may have influenced the GBD 2019 estimates. As data were absent or sparse in many regions and countries, and only a few countries or territories provided actual national data globally, the burden estimates were heavily dependent on the modeled data instead of typical data. Second, in the GBD 2019, acute and chronic appendicitis data were combined, and there was no differentiation between the subtypes of perforated appendicitis and non-perforated appendicitis, which differed in DALYs. To clarify the burden of appendicitis, stratification of appendicitis subtypes is needed in the future.
Conclusion
Appendicitis remains a major public health problem worldwide with a large burden of incidence. The number and rate of incidence have increased, while the number and rate of DALYs have decreased globally. Our findings may be valuable for policymakers to establish effective prevention and management strategies that are adaptable to local conditions.
Data Sharing Statement
Data used in this study were derived from the Global Burden of Diseases, Injuries, and Risk Factors Study 2019 (GBD 2019).
Ethics Approval and Informed Consent
This study did not contain identifiable data of living individual, and animal subjects were not involved in the study. An ethics-approval waiver was consented to by the ethics committee of the Second Hospital of Jilin University.
Acknowledgments
We thank the Institute for Health Metrics and Evaluation (IHME) and the Global Burden of Disease study collaborations. We thank professor Zhenxing Mao from College of Public Health, Zhengzhou University for his help in checking the statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: a review. JAMA. 2021;326(22):2299–2311. doi:10.1001/jama.2021.20502
2. Sulu B, Günerhan Y, Palanci Y, Işler B, Cağlayan K. Epidemiological and demographic features of appendicitis and influences of several environmental factors. J Trauma Emerg Surg TJTES. 2010;16(1):38–42.
3. Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010;20(2):97–105. doi:10.2188/jea.je20090011
4. Ferris M, Quan S, Kaplan BS, et al. The global incidence of appendicitis: a systematic review of population-based studies. Ann Surg. 2017;266(2):237–241. doi:10.1097/SLA.0000000000002188
5. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Lond Engl. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
6. GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Lond Engl. 2020;396(10258):1223–1249. doi:10.1016/S0140-6736(20)30752-2
7. Golz RA, Flum DR, Sanchez SE, Liu X, Donovan C, Drake FT. Geographic association between incidence of acute appendicitis and socioeconomic status. JAMA Surg. 2020;155(4):330–338. doi:10.1001/jamasurg.2019.6030
8. Akhtar-Danesh GG, Doumouras AG, Flageole H, Hong D. Geographic and socioeconomic predictors of perforated appendicitis: a national Canadian cohort study. J Pediatr Surg. 2019;54(9):1804–1808. doi:10.1016/j.jpedsurg.2018.10.065
9. Lin KB, Chan CL, Yang NP, et al. Epidemiology of appendicitis and appendectomy for the low-income population in Taiwan, 2003-2011. BMC Gastroenterol. 2015;15:18. doi:10.1186/s12876-015-0242-1
10. Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res. 2012;175(2):185–190. doi:10.1016/j.jss.2011.07.017
11. Oguntola AS, Adeoti ML, Oyemolade TA. Appendicitis: trends in incidence, age, sex, and seasonal variations in South-Western Nigeria. Ann Afr Med. 2010;9(4):213–217. doi:10.4103/1596-3519.70956
12. Stein GY, Rath-Wolfson L, Zeidman A, et al. Sex differences in the epidemiology, seasonal variation, and trends in the management of patients with acute appendicitis. Langenbecks Arch Surg. 2012;397(7):1087–1092. doi:10.1007/s00423-012-0958-0
13. Wang R, Jing W, Liu M, Liu J. Trends of the Global, Regional, and National Incidence of Measles, Vaccine Coverage, and Risk Factors in 204 Countries From 1990 to 2019. Front Med. 2021;8:798031. doi:10.3389/fmed.2021.798031
14. Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet Lond Engl. 2016;388(10062):e19–e23. doi:10.1016/S0140-6736(16)30388-9
15. Liu Z, Jiang Y, Yuan H, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–683. doi:10.1016/j.jhep.2018.12.001
16. Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the Global Burden of Disease study. J Psychiatr Res. 2020;126:134–140. doi:10.1016/j.jpsychires.2019.08.002
17. Jing W, Liu J, Liu M. The global trends and regional differences in incidence of HEV infection from 1990 to 2017 and implications for HEV prevention. Liver Int off J Int Assoc Study Liver. 2021;41(1):58–69. doi:10.1111/liv.14686
18. Hankey BF, Ries LA, Kosary CL, et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control CCC. 2000;11(1):31–35. doi:10.1023/a:1008953201688
19. Gao S, Yang WS, Bray F, et al. Declining rates of hepatocellular carcinoma in urban Shanghai: incidence trends in 1976–2005. Eur J Epidemiol. 2012;27(1):39–46. doi:10.1007/s10654-011-9636-8
20. Rosner B, Glynn RJ, Lee MLT. The Wilcoxon signed rank test for paired comparisons of clustered data. Biometrics. 2006;62(1):185–192. doi:10.1111/j.1541-0420.2005.00389.x
21. Hu Y, Shan Y, Du Q, et al. Gender and socioeconomic disparities in global burden of epilepsy: an analysis of time trends from 1990 to 2017. Front Neurol. 2021;12:643450. doi:10.3389/fneur.2021.643450
22. Li HY, Liu YM, Dong L, et al. Global, regional, and national prevalence, disability adjusted life years, and time trends for refraction disorders, 1990–2019: findings from the global burden of disease study 2019. BMC Public Health. 2021;21(1):1619. doi:10.1186/s12889-021-11648-1
23. Teng TZJ, Thong XR, Lau KY, Balasubramaniam S, Shelat VG. Acute appendicitis-advances and controversies. World J Gastrointest Surg. 2021;13(11):1293–1314. doi:10.4240/wjgs.v13.i11.1293
24. Kiss N, Minderjahn M, Reismann J, et al. Use of gene expression profiling to identify candidate genes for pretherapeutic patient classification in acute appendicitis. BJS Open. 2021;5(1):zraa045. doi:10.1093/bjsopen/zraa045
25. Iamwat J, Teerasamit W, Apisarnthanarak P, Noppakunsomboon N, Kaewlai R. Predictive ability of CT findings in the differentiation of complicated and uncomplicated appendicitis: a retrospective investigation of 201 patients undergone appendectomy at initial admission. Insights Imaging. 2021;12(1):143. doi:10.1186/s13244-021-01086-3
26. Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic Review and Meta-Analysis of CT Features for Differentiating Complicated and Uncomplicated Appendicitis. Radiology. 2018;287(1):104–115. doi:10.1148/radiol.2017171260
27. Pogorelić Z, Mihanović J, Ninčević S, Lukšić B, Elezović Baloević S, Polašek O. Validity of Appendicitis Inflammatory Response Score in Distinguishing Perforated from Non-Perforated Appendicitis in Children. Child Basel Switz. 2021;8(4):309. doi:10.3390/children8040309
28. Poprom N, Wilasrusmee C, Attia J, McEvoy M, Thakkinstian A, Rattanasiri S. Comparison of postoperative complications between open and laparoscopic appendectomy: an umbrella review of systematic reviews and meta-analyses. J Trauma Acute Care Surg. 2020;89(4):813–820. doi:10.1097/TA.0000000000002878
29. Cao J, Tao F, Xing H, et al. Laparoscopic Procedure is Not Independently Associated With the Development of Intra-Abdominal Abscess After Appendectomy: a Multicenter Cohort Study With Propensity Score Matching Analysis. Surg Laparosc Endosc Percutan Tech. 2017;27(5):409–414. doi:10.1097/SLE.0000000000000460
30. Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11:CD001546. doi:10.1002/14651858.CD001546.pub4
31. Liu BR, Song JT, Han FY, Li H, Yin JB. Endoscopic retrograde appendicitis therapy: a pilot minimally invasive technique (with videos). Gastrointest Endosc. 2012;76(4):862–866. doi:10.1016/j.gie.2012.05.029
32. Yang B, Kong L, Ullah S, et al. Endoscopic retrograde appendicitis therapy versus laparoscopic appendectomy for uncomplicated acute appendicitis. Endoscopy. 2022;54(8):747–754. doi:10.1055/a-1737-6381
33. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925. doi:10.1093/oxfordjournals.aje.a115734
34. Baird DLH, Simillis C, Kontovounisios C, Rasheed S, Tekkis PP. Acute appendicitis. BMJ. 2017;357:j1703. doi:10.1136/bmj.j1703
35. Yamini D, Vargas H, Bongard F, Klein S, Stamos MJ. Perforated appendicitis: is it truly a surgical urgency? Am Surg. 1998;64(10):970–975.
36. Franz MG, Norman J, Fabri PJ. Increased morbidity of appendicitis with advancing age. Am Surg. 1995;61(1):40–44.
37. Weinandt M, Godiris-Petit G, Menegaux F, Chereau N, Lupinacci RM. Appendicitis is a severe disease in elderly patients: a twenty-year audit. JSLS. 2020;24(3):
38. Petroianu A, Oliveira-Neto JE, Alberti LR. Comparative incidence of acute appendicitis in a mixed population, related to skin color. Arq Gastroenterol. 2004;41(1):24–26. doi:10.1590/s0004-28032004000100005
39. Luckmann R, Davis P. The epidemiology of acute appendicitis in California: racial, gender, and seasonal variation. Epidemiol Camb Mass. 1991;2(5):323–330. doi:10.1097/00001648-199109000-00003
40. Anderson JE, Bickler SW, Chang DC, Talamini MA. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995–2009. World J Surg. 2012;36(12):2787–2794. doi:10.1007/s00268-012-1749-z
41. Terlinder J, Andersson RE. Incidence of appendicitis according to region of origin in first- and second-generation immigrants and adoptees in Sweden. A cohort follow-up study. Scand J Gastroenterol. 2016;51(1):111–120. doi:10.3109/00365521.2015.1030688
42. Wei PL, Chen CS, Keller JJ, Lin HC. Monthly variation in acute appendicitis incidence: a 10-year nationwide population-based study. J Surg Res. 2012;178(2):670–676. doi:10.1016/j.jss.2012.06.034
43. Li HM, Yeh LR, Huang YK, Hsieh MY, Yu KH, Kuo CF. Familial Risk of Appendicitis: a Nationwide Population Study. J Pediatr. 2018;203:330–335.e3. doi:10.1016/j.jpeds.2018.07.071
44. Gaitanidis A, Kaafarani HMA, Christensen MA, et al. Association Between NEDD4L Variation and the Genetic Risk of Acute Appendicitis: a Multi-institutional Genome-Wide Association Study. JAMA Surg. 2021;156(10):917–923. doi:10.1001/jamasurg.2021.3303
45. Gomes CA, Abu-Zidan FM, Sartelli M, et al. Management of Appendicitis Globally Based on Income of Countries (MAGIC) Study. World J Surg. 2018;42(12):3903–3910. doi:10.1007/s00268-018-4736-1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.