Back to Journals » Clinical Ophthalmology » Volume 10
The emotional and physical impact of wet age-related macular degeneration: findings from the wAMD Patient and Caregiver Survey
Authors Varano M, Eter N, Winyard S, Wittrup-Jensen K, Navarro R, Heraghty J
Received 18 July 2015
Accepted for publication 21 October 2015
Published 3 February 2016 Volume 2016:10 Pages 257—267
DOI https://doi.org/10.2147/OPTH.S92616
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Monica Varano,1 Nicole Eter,2 Steve Winyard,3 Kim U Wittrup-Jensen,4 Rafael Navarro,5 Julie Heraghty6
On behalf of the wAMD Patient and Caregiver Survey Committee members
1Department of Ophthalmology, Fondazione GB Bietti-IRCCS, Rome, Italy; 2Department of Ophthalmology, University of Münster, Münster, Germany; 3Department of Policy and Campaigns, Royal National Institute of Blind People, London, UK; 4Bayer Pharma AG, Berlin, Germany; 5Instituto de Microcirugia Ocular, Barcelona, Spain; 6Macular Disease Foundation Australia, Sydney, NSW, Australia
Objectives: This was a cross-sectional survey to evaluate the physical and emotional impact of wet age-related macular degeneration (wAMD) on a global cohort of patients who were receiving (or had previously received) antivascular endothelial growth factor injections, and caregivers (paid and unpaid).
Methods: The survey was performed in nine countries using an ophthalmologist-devised questionnaire.
Results: A total of 910 patients and 890 caregivers completed the questionnaire. Most patients had been diagnosed and receiving antivascular endothelial growth factor injections for more than 1 year (74.7% and 63.8%, respectively), and many patients (82.1%) received support from a caregiver (usually a child/grandchild [47.3%] or partner [23.3%]). wAMD had a negative impact on most patients (71.6%); many rated fear (44.9%), sadness (39.9%), frustration (37.3%), and depression (34.0%) as common. It was linked to physical consequences, such as difficulty in reading (61.1%). Many effects were significantly greater in patients with a longer duration of disease or with wAMD in both eyes. Some caregivers (unpaid) also reported that caregiving had a negative impact on them (31.1%); many reported emotions such as sadness (34.9%) and depression (24.4%), but many also felt useful (48.4%). Overall, 27.2% of caregivers (unpaid) rated caregiving as inconvenient; this was linked to days of employment/personal obligations missed.
Conclusion: wAMD has a significant negative impact on the lives of patients, including vision-related depression, poor mobility, and limitations in day-to-day activities. The impact on nonprofessional caregivers may be underestimated in terms of emotional impact (such as depression) and loss of productivity.
Keywords: wet age-related macular degeneration, anti-vascular endothelial growth factor agents, wAMD Patient and Caregiver Survey, patient-reported outcomes
Introduction
It is estimated that there will be nearly 300 million people globally with age-related macular degeneration (AMD) by 2040.1 AMD is a progressive disease, and this growth level will be associated with a major economic burden, particularly in aging populations. From a societal perspective, AMD has been shown to adversely affect patient quality of life. Although much of the available evidence is based on small observational studies, these have clearly demonstrated an association between AMD and depression, poor mobility, and limited social functioning in older patients.2–7 There are fewer studies exploring the effects of wet age-related macular degeneration (wAMD) on caregivers. Surveys of caregivers of patients with chronic diseases indicate that inadequate income, lack of respite or support, and level of caregiving tasks were associated with more negative outcomes, but these associations were dependent on caregiver–recipient relationship and type of illness.8,9
A greater understanding of the emotional and physical impact of wAMD and the barriers to effective treatment from a patient and caregiver perspective may help to improve long-term management, improve treatment access and compliance, and address the wider quality-of-life issues associated with macular degeneration. At present, few studies have examined these factors on a more global scale and from the perspective of both the patient and caregiver.
The aim of this noninterventional, cross-sectional survey was to evaluate the impact of wAMD on a global cohort of patients who were currently receiving (or had previously received) antivascular endothelial growth factor (anti-VEGF) injections. This population was chosen as the authors were most interested in improving the management and well-being of wAMD patients treated with anti-VEGF agents, and the burden of treatment for wAMD patients and their caregivers was greater than for atrophic AMD. The survey also identified caregivers (both paid and unpaid), and evaluated the effect that caring for someone with wAMD had on unpaid caregivers. The survey was conducted via an ophthalmologist-devised questionnaire. A study that used a reconfigured version of this questionnaire, which was completed by 500 caregivers from Australia, has already been published.10 This 29-item, self-administered questionnaire used logistic regression analysis to assess the impact of caregiving on several domains, including psychological well-being, social activities, and retirement plans. This study showed that if the wAMD patient was highly dependent on the caregiver, this increased the odds of caregiver distress (odds ratio =1.99). More than half of the caregivers reported a negative state of mind and had to make changes to everyday activities and retirement plans as a result of caregiving. Distress was linked to level of sight loss experienced by the care recipient and health of caregiver (69% of caregivers also reported health problems). However, this study did not focus on economic burden or loss of productivity associated with caregiving. These issues are assessed in this larger survey, which includes both caregivers and their patients. This survey will make an important contribution for assessing the impact of caring on caregivers.
Methods
Design
This was a global, noninterventional, cross-sectional survey (questionnaire) of patients with wAMD and their caregivers that was conducted in nine countries (Australia, Brazil, Canada, France, Germany, Italy, Japan, Spain, and the UK) from June 2012 to September 2012 (including data analysis from July 2012 to December 2012). The questionnaire was devised by an independent steering committee consisting of ophthalmologists and experts, and the research organizations (Blueprint Partnership, Manchester, UK, and Survey Sampling International [SSI], London, UK). The questionnaire was designed to evaluate the emotional and physical impact of wAMD in patients and caregivers and also to identify barriers to treatment from their perspectives. Approval was obtained from the British Healthcare Business Intelligence Association (BHBIA). All materials had to be compliant with BHBIA’s Legal and Ethical Guidelines for Healthcare Market Research. All participants provided informed consent.
The questionnaire was translated for each participating country, and was available via an online link. This link was soft-launched (ie, a small number of responders completed the questionnaire enabling a data check to ensure it was captured accurately). For those responders with poor eyesight, face-to-face and telephone collection methods were used, wherein a member of SSI or one of their online partners would read aloud the translated questions and collect and input the answers; all responses were anonymous.
Recruitment
Patients with an existing wAMD diagnosis (made by their own physician) and who received current or prior anti-VEGF injections (by their own physician) were included. Caregivers who provided care and support to a patient with wAMD (as described earlier) were also included. Support was defined as assisting with daily activities, being actively involved in clinical appointments, and/or influencing treatment decisions (eg, advising the patient). Patients and caregivers fulfilling the aforementioned criteria were enrolled using online recruitment via the SSI website, which was advertised through usual patient recruitment channels (eg, hospitals, clinics, care groups, etc). The research organization (SSI) also accessed physician databases, and those physicians who agreed to be involved referred patients (fulfilling the aforementioned criteria and with their consent) to the research organization. These patients also referred their caregivers.
Data collection and analysis
The questionnaire was divided into patient and caregiver sections. Each responder was asked to provide yes/no/not sure answers based on a number of available options, or to rate questions using impact scales (positive impact, no impact, negative impact), dependency scales (not dependent, neither dependent nor independent, dependent), or convenience scales (not inconvenient, neither convenient nor inconvenient, inconvenient). Professional caregivers did not participate in any questions related to the emotional impact of wAMD. It was assumed that if a caregiver was paid, then he or she will be less likely to be emotionally impacted by their client’s eye disease.
Data checks were undertaken to ensure that all responders met the screening criteria. Responders who clicked through the survey in less than 2.5 minutes were removed, and responders who clicked through and only gave limited feedback (eg, only selecting the top option) or gave contradictory responses were removed.
All data were presented as descriptive statistics based on absolute percentages and means. Where possible, data were stratified according to length of time since diagnosis and whether patients had wAMD in one or two eyes; these comparisons were analyzed using either a two-sided Student’s t-test (to compare mean values) or a two-tailed Z-test (to compare percentages). These analyses were based on the assumption of equal variance with a 5% significance level (P<0.05). Tests were adjusted using the Bonferroni correction to counteract the problem of multiple and pairwise comparisons. Data analyses were performed in SPSS version 21 (IBM Corporation, Armonk, NY, USA), and all analyses were documented in syntax files.
Results
Participants
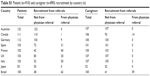
A total of 910 patients and 890 caregivers completed the questionnaire (Table 1); 25.6% (n=233/910) of patients and 8.7% (n=77/890) of caregivers (n=77/890) were recruited by physician referral. The complete breakdown by country is shown in Table S1. The majority of patients had been diagnosed (74.7%; n=680/910) and had been receiving anti-VEGF injections (63.8%; n=581/910) for more than 1 year, and many patients (82.1%) also received support from a caregiver (Table 1). Most caregivers were nonprofessional (93.5%; n=832/890) (Table 1). Many were related to the patient being a partner (23.3%), child/grandchild (47.3%), or sibling (6.0%) (Table 1).
General impact of wAMD on patients and caregivers
Figure 1 shows a snapshot of the overall effect of wAMD. The majority of patients (71.6%) reported that wAMD had a negative impact on their life. The effect on the caregiver (unpaid/nonprofessional) was mixed, with 31.1% rating the impact of the patient’s diagnosis as negative and 34.7% reporting that it had a positive impact (Figure 1A). The level of dependency of patients on caregivers after the wAMD diagnosis was rated as comparable between patients (54.2%) and caregivers (57.2%) (Figure 1B). Most patients required support for daily tasks 7 days per week (28.0%) or on an “as-needed” basis (30.1%) (Figure 1C). Patients with wAMD in one eye were significantly more likely to require support on an “as-needed” basis (38.2% vs 21.5%; P<0.05). Overall, 57.6% of patients and 77.2% of caregivers rated patient vision as very poor or quite poor (Figure 1D).
Emotional impact of wAMD on patients
wAMD was associated with a range of negative emotions in patients, including fear (44.9%), sadness (39.9%), frustration (37.3%), and depression (34.0%) (Figure 2A). Several negative emotions also increased with the time since diagnosis, including fear, frustration, and depression (Figure 2A). However, some patients also reported positive emotions such as hope (27.8%), determination (23.5%), and relief that it was not more serious (20.1%), which did not change with time since diagnosis (Figure 2A). Despite 82.1% of patients receiving caregiver support, only 24.6% felt supported.
A number of negative emotions were greater in patients with wAMD in two eyes compared with one eye, including depression (37.1% vs 31.4%; P= not significant, respectively), desperation/helplessness (24.1% vs 15.0%; P<0.05), and isolation (20.5% vs 14.6%; P<0.05). Positive emotions were significantly greater in patients with wAMD in one eye, including relief that it was not more serious (22.8% vs 16.8%; P<0.05), hope (32.6% vs 22.0%; P<0.05), and determination (28.4% vs 17.6%; P<0.05). In patients who reported feeling fearful about their diagnosis, the greatest fear was permanent loss of vision (60.0%; n=244/407).
Emotional impact of wAMD on caregivers
Similar to patients, caregivers commonly experienced sadness (34.9%), fear (27.6%), frustration (26.8%), and depression (24.4%) (Figure 2B). However, nearly half of all unpaid caregivers also felt useful (48.4%). When caregivers were stratified according to length of time since patient diagnosis of wAMD (≤1 year, >1–<3 years, ≥3–6 years), a number of negative emotions were highlighted, which included frustration: 17.8%, 29.1%*, and 26.6%; depression about diagnosis: 18.4%, 27.4%, and 22.9%; loss/hopelessness: 8.6%, 14.9%, and 17.6%*; and desperation/helplessness: 9.2%, 19.6%*, and 13.8% (*P<0.05 vs ≤1 year), respectively. Positive emotions, such as feeling useful, decreased over the same timeframe (Figure 2B). In caregivers, negative (but not positive) emotions were also linked to whether the patient had wAMD in both eyes compared with one eye.
Physical impact of wAMD on patients
Day-to-day activities
In patients, wAMD was associated with a number of negative disease consequences (Figure 3A). The most commonly reported disease consequences were difficulty reading (61.1%), inability to drive (38.5%), not engaging in the same activities as before (34.9%), being uncomfortable leaving the house alone (34.8%), and becoming less active (34.7%). Many of the negative consequences of wAMD also increased with time since diagnosis. Patients with wAMD for ≥3–6 years were significantly more likely to report difficulty reading compared with patients diagnosed for ≤1 year (67.5% vs 54.8%; P<0.05, respectively) (Figure 3A). Patients diagnosed for ≥3–6 years were also significantly (P<0.05) more likely to report a greater physical impact of wAMD, including an inability to engage in the same activities as before, having difficulty with stairs, cooking and facial recognition, and were uncomfortable leaving the house alone, when compared with patients diagnosed for ≤1 year. The physical impact of wAMD was also greater in patients with both eyes affected compared with one eye; this was particularly notable for inability to drive (44.4% vs 33.6%; P<0.05, respectively), lack of facial recognition (37.1% vs 20.4%; P<0.05), difficulty using stairs (34.1% vs 28.0%; P<0.05), reduced travel on public transportation (33.9% vs 25.4%; P<0.05), reduction in holidays (30.0% vs 22.2%; P<0.05), limited social life (27.8% vs 22.0%; P<0.05), feeling clumsy (27.6% vs 20.6%; P<0.05), and inability to play with grandchildren (12.9% vs 6.0%; P<0.05).
Falls and accidents
A number of patients reported a fall (25.7%) or accident (7.3%) in the previous 2 years due to vision impairment associated with wAMD, and 34.2% of these patients had been hospitalized as a result of a fall. The number of falls increased with time since diagnosis: 22.2% (≤1 year since diagnosis), 25.0% (>1–<3 years), and 28.1% (≥3–6 years). However, the number of accidents (such as car accidents) was higher in those with a more recent diagnosis: 8.3% (≤1 year), 8.3% (>1–<3 years), and 3.0% (≥3–6 years). The number of falls and accidents was significantly greater in patients with wAMD in two eyes compared with one eye (32.2% vs 20.4%; P<0.05 [falls] and 11.5% vs 3.8%; P<0.05 [accidents]).
Troublesome symptoms
The main symptoms of wAMD reported by patients are summarized in Figure 3B. These include blurring of central vision (69.7%), difficulty seeing fine detail (64.1%), and distortion of lines and shapes (58.2%). Many symptoms increased with time since diagnosis, and blind spots in center of vision, difficulty seeing fine detail and faces, and distortion of lines and shapes were all significantly (P<0.05) greater in patients diagnosed between ≥3 and 6 years compared with ≤1 year (Figure 3B). A number of symptoms were also reported with significantly more frequency in patients with wAMD in both eyes compared with one eye, including blurring of central vision (74.4% vs 65.8%; P<0.05), constant object in vision (35.6% vs 26.4%; P<0.05), difficulty seeing faces (53.7% vs 42.0%; P<0.05), and visual hallucinations (9.8% vs 3.0%; P<0.05).
Physical impact of wAMD on caregivers
Day-to-day activities
The role of the caregiver (as rated by the caregiver and patient) is summarized in Figure 4A. The most frequent support provided by the caregiver was associated with arranging travel (85.5% [caregiver]). The provision of support was rated as greater by the caregiver than the patient; this was greatest for help with health care professional (HCP) discussions (including treatment plan) (65.5% [caregivers] vs 40.4% [patients]). The level of support provided by caregivers tended to increase with duration of diagnosis. Help with treatment aftercare was provided by 54.9% of caregivers for patients diagnosed within ≤1 year and by 64.8% of caregivers for patients diagnosed between ≥3 and 6 years. Help with shopping increased from 53.7% to 64.8%, and help with reading increased from 39.4% to 57.8%.
Productivity
Overall, 27.2% (n=242/890) of caregivers rated the patient’s current treatment (ie, caregiving) as inconvenient. The level of inconvenience was associated with the number of days of employment/personal obligations missed (Figure 4B). In total, 57.2% (n=377/659) of caregivers missed days of employment/personal obligations during the previous 12 months as a result of helping the patient; 14.4% (n=95/659) missed 10–20 days of employment/personal obligations, with 41.0% of these caregivers rating the patient’s treatment (ie, caregiving) as inconvenient.
Discussion
This global survey showed that wAMD has a major emotional and physical impact on the lives of patients and caregivers, and may be associated with an economic burden (ie, lost caregiver productivity due to missed workdays). The majority of patients had been diagnosed for more than 1 year, and most patients experienced a range of problems. Many of these impairments were significantly worse in patients who had wAMD in both eyes, and in those with a longer duration of disease (notably depression).
The high rate of depressive symptoms observed in patients in our survey is consistent with other published estimates, which range from 30% to 42%,2,11 and is two to three times higher than estimates in an elderly community-dwelling population without wAMD (which was approximately 8%–20%).12 wAMD has also been shown to double the fall rate (from 8% to 16%) and quadruple the need for daily assistance (from 7% to 29%) compared with controls.11 Other reports also highlight that emotional problems increase in patients with bilateral wAMD.13 However, a major impact on day-to-day activities was also observed for patients with wAMD in one eye alone in our survey. Another study in 86 elderly adults found that emotional distress was significantly greater in patients with wAMD blindness in one eye only.5 A possible explanation for this may be related to uncertainty surrounding further vision loss.14
The current survey also showed that wAMD had a major impact on nonprofessional (unpaid) caregivers. Despite 48.4% of caregivers having reported feeling useful, many also reported feeling sad, fearful, and frustrated, with these emotions increasing with duration of the patient’s diagnosis and their disease severity (two eyes vs one eye). It was interesting to note that 24.4% of caregivers (33.6% of caregivers supporting a patient with wAMD in both eyes) experienced depression about the diagnosis. In general, the emotional impact on caregivers was comparable with that experienced by the patient. Although the support provided by the caregiver was mostly practical help with day-to-day activities, around one-quarter expressed that the patient’s treatment (ie, caregiving) was inconvenient. Many caregivers had missed days of employment/personal obligations as a result of supporting the patient. In the survey of 500 caregivers in Australia, which used a reconfigured version of this questionnaire, one-third of caregivers reported high dependence by patients, 53.3% of caregivers provided daily care to patients who were blind, but 80.6% still provided “as-needed” support to those patients whose vision was rated as good.10
The findings show that despite receiving anti-VEGF agents, which can improve or stabilize vision, many patients with wAMD continue to suffer adverse affective and functional consequences. It is possible that a number of other factors, which were not explored in detail in this survey, could be considered for reducing the negative impact on patients and caregivers, including tailoring of treatment and follow-up visits. The survey also reports that 42.3% of patients attended clinic visits every 4–6 weeks, with 42.5% having treatment at every visit (data not shown). This suggests that many patients may have been undertreated. A number of observational studies have found that the frequency of actual anti-VEGF injections (such as monthly ranibizumab or bevacizumab) is lower than that recommended in large-scale studies, and according to the label.15,16 In the AURA (a retrospective non-interventional study to assess the effectiveness of existing anti-VEGF treatment regimens in patients with wet age-related macular degeneration) study, 2,227 wAMD patients were followed-up for a 2-year period.17 During this time, patients received a mean of 5.0 anti-VEGF injections (mainly ranibizumab) in year 1 and a mean of 2.2 injections in year 2; this was coupled with a gradual decline in visual acuity. Unfortunately, no studies have explored the effect of different dosing regimens and follow-up schedules on patient and caregiver outcomes, including depression.
Although the survey is valuable in providing an overview of the impact of wAMD on patients and caregivers, it does have a number of limitations inherent to the observational design. The questionnaire was devised by experts to cover all aspects of wAMD, but it is not validated and is still subjective, and some questions (including the definition of depression) may be perceived differently by responders from different countries. We did not correlate the severity of visual acuity impairment at baseline on emotional and physical outcomes addressed by the questionnaire. The impact of other baseline characteristics was were also not assessed, and this could have influenced some of the participants’ answers, especially for patients suffering with depression or anxiety before the wAMD diagnosis, resulting in bias. It is also not possible to distinguish the severity of the outcomes reported, or to gauge the level of symptoms such as depression. Furthermore, the results are based on pooled findings from nine countries, and the impact of wAMD varied between countries (Table S2). Notably, patients who reported difficulty reading ranged from 38.8% (UK) to 79.0% (Brazil), and patients who could not drive anymore ranged from 10.9% (Japan) to 48.4% (Australia). The level of support for day-to-day tasks also varied between countries (Table S3). Help with reading (caregiver perspective) ranged from 23.1% (Japan) to 79.2% (Spain). It was interesting to note that the level of support provided was, in general, rated as higher by caregivers than patients across all countries.
Conclusion
In summary, the findings from this survey indicate that there is a range of emotional and physical problems associated with wAMD in patients, including vision-related depression, mobility, and limitations in day-to-day activities. The impact on nonprofessional caregivers may also be underestimated in terms of emotional impact (such as depression) and loss of productivity. However, it is interesting to note that 82.1% of patients received caregiver support, but only 24.6% felt supported – this highlights a key issue. Previous reports suggest that HCPs may underestimate the impact of wAMD.18 These findings also highlight the need for a more holistic approach to the problems encountered by wAMD patients. In a previous study of 477 patients with moderate-to-severe vision loss (43% had wAMD), visual acuity, presence of comorbidities, and dependence on family and friends emerged as the strongest independent predictors of greater rehabilitation needs.19 Depending on the health care system, the treating HCP could address some of these issues in more detail, ensuring adequate diagnosis and treatment of comorbidities, including depression, other eye disorders, and age-related disorders, or referral to other HCPs where necessary, and this wider approach may help to reduce the burden of wAMD in the longer term. The burden on the caregiver also highlights the need for a wider approach to service provision, support, and psychological resources, which is consistent with a previous meta-synthesis of qualitative research in this area.6
Acknowledgment
These data have been presented at the Royal College of Ophthalmologists’ Congress (May 20–22, 2014, Birmingham, UK), the German Retina Society Congress (June 13–14, 2014, Düsseldorf, Germany), and the International Society for Pharmacoeconomics and Outcomes Research (November 8–12, 2014, Amsterdam, the Netherlands). The contribution of the Fondazione GB Bietti-IRCCS to this paper was supported by the Italian Ministry of Health and by Fondazione Roma. The survey was sponsored by Bayer HealthCare Pharmaceuticals. Medical writing assistance was provided by PAREXEL and was funded by Bayer HealthCare Pharmaceuticals.
Disclosure
Monica Varano has served on advisory boards for Bayer, Novartis, and Allergan. Nicole Eter, Steve Winyard, and Rafael Navarro report no conflicts of interest in this study. Kim U Wittrup-Jensen is an employee of Bayer Pharma AG. Julie Heraghty is a CEO of Macular Disease Foundation Australia, which receives funding from Bayer and Novartis. The authors resport no other conflicts of interest in this work.
References
Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–e116. | ||
Casten RJ, Rovner BW, Tasman W. Age-related macular degeneration and depression: a review of recent research. Curr Opin Ophthalmol. 2004;15(3):181–183. | ||
Casten RJ, Rovner BW. Update on depression and age-related macular degeneration. Curr Opin Ophthalmol. 2013;24(3):239–243. | ||
Hassell JB, Lamoureux EL, Keeffe JE. Impact of age related macular degeneration on quality of life. Br J Ophthalmol. 2006;90(5):593–596. | ||
Williams RA, Brody BL, Thomas RG, Kaplan RM, Brown SI. The psychosocial impact of macular degeneration. Arch Ophthalmol. 1998;116(4):514–520. | ||
Bennion AE, Shaw RL, Gibson JM. What do we know about the experience of age related macular degeneration? A systematic review and meta-synthesis of qualitative research. Social Sci Med. 2012;75(6):976–985. | ||
Bandello F, Lafuma A, Berdeaux G. Public health impact of neovascular age-related macular degeneration treatments extrapolated from visual acuity. Investig Ophthalmol Visual Sci. 2007;48(1):96–103. | ||
Pinquart M, Sorensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):112–128. | ||
Robison J, Fortinsky R, Kleppinger A, Shugrue N, Porter M. A broader view of family caregiving: effects of caregiving and caregiver conditions on depressive symptoms, health, work, and social isolation. J Gerontol B Psychol Sci Soc Sci. 2009;64(6):788–798. | ||
Gopinath B, Kifley A, Cummins R, Heraghty J, Mitchell P. Predictors of psychological distress in caregivers of older persons with wet age-related macular degeneration. Aging Ment Health. 2015;19(3):239–246. | ||
Soubrane G, Cruess A, Lotery A, et al. Burden and health care resource utilization in neovascular age-related macular degeneration: findings of a multicountry study. Arch Ophthalmol. 2007;125(9):1249–1254. | ||
World Health Organization. World Health Report: Mental Health: New Understanding, New Hope. Geneva: World Health Organization; 2001. Available from: http://www.who.int/whr/2001/en/whr01_en.pdf. Accessed October 7, 2014. | ||
Berman K, Brodaty H. Psychosocial effects of age-related macular degeneration. Int Psychogeriatr. 2006;18(3):415–428. | ||
Slakter JS, Stur M. Quality of life in patients with age-related macular degeneration: impact of the condition and benefits of treatment. Surv Ophthalmol. 2005;50(3):263–273. | ||
Holekamp NM, Liu Y, Yeh WS, et al. Clinical utilization of anti-VEGF agents and disease monitoring in neovascular age-related macular degeneration. Am J Ophthalmol. 2014;157(4):825–833. | ||
Lad EM, Hammill BG, Qualls LG, Wang F, Cousins SW, Curtis LH. Anti-VEGF treatment patterns for neovascular age-related macular degeneration among medicare beneficiaries. Am J Ophthalmol. 2014;158(3):537–543. | ||
Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–226. | ||
Stein JD, Brown MM, Brown GC, Hollands H, Sharma S. Quality of life with macular degeneration: perceptions of patients, clinicians, and community members. Br J Ophthalmol. 2003;87(1):8–12. | ||
O’Connor PM, Lamoureux EL, Keeffe JE. Predicting the need for low vision rehabilitation services. Br J Ophthalmol. 2008;92(2):252–255. |
Supplementary materials
  | Table S1 Patient (n=910) and caregiver (n=890) recruitment by country (n) |
  | Table S2 The impact (%) of wAMD on a patient’s ability to read or drive as rated by patients (n=910) and caregivers (n=890) in each country |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






