Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
The Effects of Serum Folic Acid and Vitamin B12 on the Risk of Gestational Diabetes Mellitus
Authors Cheng Y, Lu X, Zhao F, Sun G
Received 14 October 2022
Accepted for publication 6 December 2022
Published 14 December 2022 Volume 2022:15 Pages 3891—3899
DOI https://doi.org/10.2147/DMSO.S391888
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Yao Cheng,1 Xinfeng Lu,2 Feixia Zhao,3 Guoqiang Sun1
1Obstetrics Department, Maternal and Child Health Hospital of Hubei Province, Wuhan, People’s Republic of China; 2Medical Record Department, Maternal and Child Health Hospital of Hubei Province, Wuhan, People’s Republic of China; 3Medical College of Wuhan University of Science and Technology, Wuhan, People’s Republic of China
Correspondence: Guoqiang Sun, Obstetrics Department, Maternal and Child Health Hospital of Hubei Province, Tongji Medical College, Huazhong University of Science and Technology, Wuluo Road No. 745, Hongshan District, Wuhan, 430070, People’s Republic of China, Tel +86-15972153596, Email [email protected]
Purpose: In order to gain more knowledge on the risk of gestational diabetes mellitus (GDM), and to provide evidence for clinical guidance on the optimum level of serum folic acid and vitamin B12, this study aimed to clarify the relationship between serum folic acid and vitamin B12 and the risk of GDM.
Patients and Methods: This retrospective case−control study was conducted based on the clinical information system of the Maternal and Child Health Hospital of Hubei Province. Clinical data including maternal socio-demographical characteristics, serum folic acid, and vitamin B12 were collected. Logistic regression analyses and restricted cubic splines were performed to examine the impact of serum folic acid and vitamin B12 on the risk of GDM.
Results: Significantly elevated risks of GDM were observed in groups with high serum folic acid concentration (OR = 1.84, 95% CI: 1.07− 3.16), and in low vitamin B12 concentration (OR = 2.14, 95% CI: 1.26− 3.65). After stratified by age, the increased risk of GDM was still noticed in a low level of vitamin B12 among mothers aged < 30 years (OR = 4.76, 95% CI: 1.45− 15.61). In mothers with pre−pregnancy BMI < 24, elevated risk of GDM was significantly associated with a high folic acid (OR = 2.09, 95% CI: 1.11− 3.93) or a low vitamin B12 concentration (OR = 2.24, 95% CI: 1.22− 4.14). Moreover, the risk of GDM was on the decline with the increased level of folic acid in the beginning, and it started to manifest an upward trend when the serum folic acid reached 19.02 ng/mL.
Conclusion: This study demonstrated that serum folic acid excess or vitamin B12 deficiency could contribute to the increased risk of GDM, and revealed the potential side effect of serum folic acid overdose. As serum folic acid and vitamin B12 tests are widely applied in clinical practice, this finding could help clinicians to evaluate maternal risk from a new perspective.
Keywords: gestational diabetes mellitus, folic acid, vitamin B12, age, BMI
Introduction
Gestational diabetes mellitus (GDM) is a common endocrine disease during pregnancy, which is related to the elevated risk of adverse pregnancy outcomes including cesarean section, premature birth, dystocia, premature rupture of membranes, intrauterine infection, macrosomia, stillbirth, and fetal malformation.1 GDM patients also have higher life−span risks of hyperglycemia in both mothers and their offspring.2 The estimated prevalence of GDM was 14.0% in global, which was 12.7%, 9.2%, and 14.2% in low, middle, and high income countries, respectively.3 Although medical health-care technology has developed rapidly in recent years, the incidence of GDM is still on the rise and it has become a global problem.4,5 The prevention of GDM is of great significance to promote the health of mothers and their offspring worldwide.
As individual modifiable factors, more and more attention has been paid to the effects of micronutrition supplements on GDM, including folic acid and vitamin B12. Folic acid and vitamin B12, classified as B−family water−soluble vitamins, are involved in one−carbon metabolism and important reactions for DNA methylation and nucleic acid, amino acid, and lipid metabolism.6 It is well established that dietary and supplemental intakes of folic acid are recommended for the prevention of neural tube defects. According to the latest clinical practice guideline by the Society of Obstetricians and Gynaecologists of Canada (SOGC), women with no history of neural tube defect were recommended to take 400μg or 1000μg folic acid supplement per day,7 while it was 400μg or 800μg recommended by the US Preventive Services Task Force (USPSTF).8 Additionally, total folic acid intake during pregnancy should reach 600μg dietary folic acid equivalent per day including 400μg folic acid supplements, which is suggested by the Chinese Nutrition Society.9
Folic acid and vitamin B12 closely interacted, and either of their deficiencies could lead to hyperhomocysteinemia and classical megaloblastic anemia.10 While the overdose of folic acid and vitamin B12 might have potential side effects on GDM. Previous studies showed controversial results on the relationship between folic acid and vitamin B12 and the risk of GDM. A study carried out in China by Li et al showed that continuous folic acid supplementation of more than 800μg per day before and during pregnancy could significantly increase the risk of GDM, as confirmed by Zhu et al.11,12 However, another longitudinal study based on the prospective data of the Nurses’ Health Study II showed a dose−response relationship of the higher the folic acid supplement and the lower the risk of GDM.13
Specifically, serum folic acid and vitamin B12 can indirectly reflect individual supplements consumption.14 The potential effects of serum folic acid and vitamin B12 on the risk of GDM could provide evidence for the clinical guidance of nutrition supplements. These blood tests were recommended to assist in clinical assessments, but their deficiency or excess has no clear standards.15,16 On this point, studies conducted by Li et al and Lai et al showed that higher folic acid concentrations and lower vitamin B12 concentrations contributed to higher risks of GDM.17,18 Whereas a meta−analysis conducted by Wang et al found no clear association between serum folic acid and vitamin B12 and GDM risk.19 These inconsistent results promote studies based on different populations to clarify the relationship between folic acid and vitamin B12 and GDM risk.
In summary, to gain more knowledge on the risk of GDM derived from folic acid and vitamin B12, and to provide evidence for clinical guidance on the optimum level of serum folic acid and vitamin B12, this study aimed to clarify the relationship between serum folic acid and vitamin B12 and the risk of GDM.
Materials and Methods
Study Population
This retrospective case−control study was conducted based on the clinical information system of the Maternal and Child Health Hospital of Hubei Province. Clinical data were obtained from pregnant women who visited the hospital from 2019 to 2021. The inclusion criteria of this study were participants with detailed clinical information including clinical diagnosis of GDM, the blood test result of serum folic acid and vitamin B12 (756 cases). After removing mothers with multiple pregnancies (7 cases) or with type 2 diabetes (5 cases), 744 eligible participants including 147 GDM patients and 597 controls were recruited.
Data Collection
Clinical data including maternal age, pre−pregnancy weight, height, gravidity, family history of diabetes, serum folic acid and vitamin B12, and GDM diagnostic information were collected from the electronic medical records. Among them, maternal age was classified into <30, 30−34, and ≥35 years; and gravidity was classified into three groups of 1, 2, and ≥3. The pre−pregnancy BMI was calculated by self−reported pre−pregnancy weight and height (kg/m2). According to the Chinese standard of obesity, the maternal pre−pregnancy BMI was classified into underweight (BMI <18.5), healthy weight (18.5−23.9), overweight (24−27.9), and obese (≥28). Self−reported family history of diabetes was defined as one or more clinically diagnosed diabetes patients within three generations of maternal participants. Serum folic acid and vitamin B12 were measured by the chemiluminescence method and tested by MAGLUMI 2000 (Shenzhen New Industries Biomedical Engineering Co., Ltd. (Snibe), Shenzhen, China) CLIA analyser. Data of serum folic acid and vitamin B12 were classified by four interquartile ranges (IQR) (<10.77, 10.77−14.10, 14.11−19.10, and ≥19.11 ng/mL; <265.40, 265.40−334.69, 334.70−405.79, and ≥405.80 pg/mL, respectively). Moreover, according to the recommendations of the International Association of the Diabetes and Pregnancy Study Groups Consensus Panel,20 GDM was diagnosed by 75g oral glucose tolerance test (OGTT) during 24−28 weeks of gestation on the following criteria: fasting blood glucose >5.1 mmol/L, and/or 1−hour blood glucose >10.0 mmol/L, and/or 2−hour blood glucose >8.5 mmol/L.
Statistical Analysis
In this study, serum folic acid and vitamin B12 were regarded as the key independent variables, and GDM as a dependent variable. Additionally, maternal demographic characteristics including age, pre−pregnancy BMI, gravidity, and family history of diabetes were applied as the covariates. All of the participants were classified into GDM patient group and the control group. The Shapiro–Wilk tests were applied to the normality examination of continuous variables. Non-normal continuous variables were presented as median (IQR) and categorical variables were summarized as count (percentages). The differences in the prevalence of GDM among subgroups stratified by maternal demographic characteristics and folic acid and vitamin B12 concentrations were compared by Chi−square tests for categorical variables and/or Wilcoxon–Mann–Whitney tests for continuous variables. Logistic regression analyses were performed to examine the impact of serum folic acid and vitamin B12 on the risk of GDM, and the corresponding odds ratios (ORs) and 95% confidence intervals (CIs) were obtained. The third quartile of folic acid and vitamin B12 were used as references in the logistic regression models. First, the risks of GDM were evaluated by an unadjusted logistic regression model (model 1) and a logistic regression model adjusted for age, BMI, gravidity, and family history of diabetes (model 2). Second, the risks of GDM were further explored by logistic regression models stratified by age with two categories of <30 years (model 3) and ≥30 years (model 4) which adjusted for BMI, gravidity, and family history of diabetes. Third, age, gravidity, and family history of diabetes were adjusted in logistic regression models according to pre−pregnancy BMI of <24 (model 5) and ≥24 (model 6). Shapiro–Wilk tests, Chi−square tests, Wilcoxon–Mann–Whitney tests, and logistic regressions were performed by SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Moreover, potential nonlinear relationships between serum folic acid/vitamin B12 and the risk of GDM were examined by the restricted cubic splines (RCS). We adopted RCS with 4 knots, and the medium of folic acid and vitamin B12 were used as references to obtain the ORs. The RCS regression analysis was performed by R 4.2.1 (The R Foundation for Statistical Computing, Vienna, Austria). Two-sided P<0.05 was regarded as statistically significant.
Results
The prevalence of GDM was 19.76% in this study (Table 1). Mothers aged 30−34 were observed to have the highest prevalence of GDM (25.51% vs 13.13%, P=0.0005). The median age of GDM patients was significantly higher than the control group (P=0.0002). Notably, the results showed that a higher prevalence of GDM was observed in mothers with higher pre−pregnancy BMI (7.94% vs 36.36%, P < 0.0001). The median BMI of GDM patients was significantly higher than the control group (P < 0.0001). Mothers who have a family history of diabetes presented a higher prevalence of GDM (41.38% vs 18.88%, P=0.0029).
 |
Table 1 Demographic Characteristics and Clinical Outcomes of Maternal with GDM and Control Group |
The serum folic acid and vitamin B12 were categorized into four groups according to the median and interquartile concentrations, and the prevalence of GDM among the subgroups is shown in Table 2. There was no significant difference in the prevalence of GDM among the four folic acid levels. Specifically, mothers with higher levels of serum vitamin B12 concentrations presented a lower prevalence of GDM (29.79% vs 14.52%, P=0.0004). The median vitamin B12 concentration of GDM patients was significantly lower than the control group (P=0.0015).
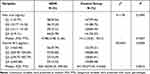 |
Table 2 The Interquartile Ranges of Serum Folic Acid/Vitamin B12 in GDM and Control Group |
The effects of serum folic acid and vitamin B12 on the risk of GDM are shown in Table 3. Model 1 showed the unadjusted results of logistic regression analysis, and model 2 was adjusted for age, BMI, gravidity, and family history of diabetes. Both model 1 and model 2 showed significantly elevated risks of GDM in the Q4 group of folic acid compared to the Q3 group (OR = 1.70, 95% CI: 1.01−2.86; OR = 1.84, 95% CI: 1.07−3.16, respectively). For vitamin B12, the Q1 group showed increased risks of GDM in model 1 and model 2 (OR = 2.48, 95% CI: 1.49−4.15; OR = 2.14, 95% CI: 1.26−3.65, respectively). And a decreasing trend in the risk of GDM was observed among mothers with higher vitamin B12 concentration (P for trend <0.05). After stratified by age, the increased risk of GDM was still noticed in the Q1 level of vitamin B12 among mothers aged <30 years (OR = 4.76, 95% CI: 1.45−15.61), but there were no significant associations between folic acid/vitamin B12 and the risk of GDM among mothers aged ≥30 years. Furthermore, among mothers with a pre−pregnancy BMI <24, the Q4 group of folic acid (OR = 2.09, 95% CI: 1.11−3.93) and the Q1 group of vitamin B12 (OR = 2.24, 95% CI: 1.22−4.14) had higher risks of GDM. Moreover, multivariable analyses on the associations between serum folic acid/vitamin B12 and fasting blood glucose/1−hour blood glucose/2−hour blood glucose were presented in Table S1.
 |
Table 3 Multivariable Analyses on the Relationships Between Serum Folic Acid/Vitamin B12 and the Risk of GDM |
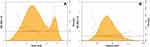
The results of RCS regression analysis are presented in Figure 1 to examine the nonlinear relationships between serum folic acid/vitamin B12 and the risk of GDM. Serum folic acid showed a bimodal distribution, while vitamin B12 showed a unimodal distribution. In Figure 1A, folic acid and the risk of GDM showed a significant nonlinear relationship (χ2=7.41, P=0.0246), and linear relationship between vitamin B12 and the risk of GDM is observed in Figure 1B (χ2=4.85, P=0.0885). The predicted ORs were on the decline with the increased level of folic acid in the beginning, and it started to manifest an upward trend when the folic acid reached 19.02 ng/mL. Furthermore, the risk of GDM was decreased in parallel with the increase of vitamin B12 concentration.
Discussion
This study showed that serum folic acid excess or vitamin B12 deficiency could contribute to the increased risk of GDM. Specifically, serum folic acid and GDM risk presented a significant “J” shape nonlinear relationship, and the optimum level was below 19.02 ng/mL. This result was double confirmed by the result of logistic regression analysis that the highest folic acid quartile was related to the significantly elevated risk of GDM. This threshold value was close to what was recommended for the general population by the WHO based on the Third National Health and Nutrition Examination Survey (NHANES III) (20 ng/mL).21 Moreover, the relationship between folic acid and the risk of GDM was emphasized among pregnant women with BMI <24, and the results also pointed out that women aged <30 years with low serum vitamin B12 should be alert to the elevated risk of GDM.
Most of previous studies documented that higher serum folic acid or lower vitamin B12 levels were detected in GDM patients. Jankovic-Karasoulos et al reported significantly higher serum folic acid levels in GDM patients,22 and Krishnaveni et al also reported an increased incidence of GDM among B12−deficient women with elevated serum folic acid.23 After adjusted for age, parity, smoking status, ethnicity, family history, household income and B12 status, Saravanan et al reported a 11% higher risk of GDM among women with higher serum folic acid concentration.24 Xie et al further confirmed the trend effects between serum folic acid concentration and the risk of GDM by both logistic regressions and RCS regressions.25 Moreover, Li et al and Lai et al conducted the joint analysis of serum folic acid and vitamin B12 and found higher folic acid and lower vitamin B12 might have contributed to the elevated risk of GDM.17,18
A few studies declared different viewpoints on the associations between serum folic acid and vitamin B12 and the risk of GDM. A cross−sectional study performed by Guven et al based on 223 mothers found no significant difference in folic acid and vitamin B12 concentrations among gestational diabetes and other groups.26 A cohort study conducted by Chen et al showed significant positive dose−response relationships of higher vitamin B12 concentration and increased GDM risk.27
The results of this study could partly agree with the above studies that folic acid excess and vitamin B12 deficiency are hazard factors for GDM. But inconsistent with these studies, this study showed no trend effect on the relationship between serum folic acid and the risk of GDM overall. Moreover, to reduce the vitamin B12 and folic acid interaction and to further elucidate the relationships, the results stratified by vitamin B12 and folic acid showed that the trend effect of folic acid on the risk of GDM might exist on the circumstances of serum vitamin B12 ≥334.70 pg/mL, while no trend effect of vitamin B12 was observed among pregnant women with serum folic acid ≥14.11 ng/mL (Tables S2 and S3). These biases on the above results might lie in the differences on study design, population, adjusted variables, and stratification factors.
What is more, this study showed a declined trend in the risk of GDM in serum folic acid below 19.02 ng/mL. It was in line with a double−blind randomized controlled clinical trial which showed an effective co−treatment of folic acid for patients of type 2 diabetes under metformin treatment.28 The potential explanation is that folic acid improves endothelial dysfunction induced by high homocysteine and helps to improve insulin resistance.29 However, folic acid excess and vitamin B12 deficiency might have side effects on GDM. A previous study has summarized the potential mechanisms of the elevated risk of GDM derived from folic acid excess and vitamin B12 deficiency.30 High folic acid and low vitamin B12 could block the folate cycle, and inhibit the conversion of tetrahydrofolate from 5−methyltetrahydrofolate and methionine from homocysteine, which affects the production of de novo purine and thymidine and impedes DNA synthesis in association with insulin resistance.31 Additionally, the accumulated homocysteine and the unmetabolized folic acid might result in an elevated risk of GDM as well.32,33 Interestingly, the associations mentioned above were only observed among mothers with BMI <24, and the negative association between vitamin B12 and GDM was observed in pregnant women aged <30 years. In line with this study, van Weelden et al found no associations between folic acid/vitamin B12 and the risk of GDM among mothers with BMI ≥30.34 Sufficient studies affirmed that obesity and advanced maternal age were hazard factors for GDM, and these factors might interfere with the impacts of folic acid/vitamin B12 on the risk of GDM.35,36
As numerous studies presented inconsistent results, this study applied both linear and nonlinear regression analysis to explore the relationships between folic acid and vitamin B12 and the risk of GDM in depth. Additionally, few studies focused on the subgroups stratified by age and BMI, and this study identified that folic acid excess or vitamin B12 deficiency in pregnant women with BMI <24, or vitamin B12 deficiency in pregnant women aged <30 years were at high risks of GDM. However, this study has several limitations. Firstly, the data of this study was obtained from a single hospital, therefore it should be cautious when generalizing the results to other populations. Secondly, this study was based on hospital information system and only considered the serum folic acid and vitamin B12, and the folic acid and vitamin B12 supplements were failed to obtain. Thirdly, other confounding factors might be associated with GDM were neither considered in this study, such as physical exercise, dietary energy intake, and desserts intake et al. Fourthly, this study only considered only one test results of serum folic acid and vitamin B12, future studies to explore the pathogeny of GDM based on the dynamic surveillances of serum folic acid and vitamin B12 during the pregnancy period were promoted.
Conclusion
This study provided strengthened evidence on the relationships between folic acid, vitamin B12, and the risk of GDM, and revealed the potential side effect of serum folic acid overdose (>19.02 ng/mL). As serum folic acid and vitamin B12 tests are widely applied in clinical practice, this finding could help clinicians to evaluate maternal risk from a new perspective. Specifically, in pregnant women with BMI <24, an increased risk of GDM was observed in the group of folic acid excess or vitamin B12 deficiency; and in pregnant women aged <30 years, elevated risk of GDM was also associated to lower vitamin B12 concentration. Longitudinal studies are warranted to explore the underlying mechanism of the occurrence of GDM caused by folic acid and vitamin B12 among different populations.
Abbreviations
CI, Confidence Interval; GDM, gestational diabetes mellitus; IQR, interquartile range; OR, Odds Ratios; RCS, restricted cubic spline.
Data Sharing Statement
The dataset used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Maternal and Child Health Hospital of Hubei Province (2021IECXM047).
Patient Informed Consent
Patient informed consents were not collected in this study because the data was obtained retrospectively from the clinical information system without any individual patient identifiers. The patient informed consent has been exempted by the Ethics Committee of Maternal and Child Health Hospital of Hubei Province.
Author Contributions
All authors have made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, and they have drafted, or written, or substantially revised or critically reviewed the article. All authors agreed on the journal to which the article submitted, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding
This study was funded by the Maternal and Child Health Hospital of Hubei Province Research Project [grant No. 2021SFYM007].
Disclosure
The authors have no potential conflicts of interest and confirm that this study has not been previously been published elsewhere by any of the authors.
References
1. Ana Y, Prafulla S, Deepa R, Babu GR. Emerging and public health challenges existing in gestational diabetes mellitus and diabetes in pregnancy. Endocrinol Metab Clin North Am. 2021;50:513–530. doi:10.1016/j.ecl.2021.05.008
2. Kennelly MA, McAuliffe FM. Prediction and prevention of Gestational Diabetes: an update of recent literature. Eur J Obstet Gynecol Reprod Biol. 2016;202:92–98. doi:10.1016/j.ejogrb.2016.03.032
3. Wang H, Li N, Chivese T, et al. IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by International Association of Diabetes in Pregnancy Study Group’s criteria. Diabetes Res Clin Pract. 2022;183:109050. doi:10.1016/j.diabres.2021.109050
4. Su FL, Lu MC, Yu SC, et al. Increasing trend in the prevalence of gestational diabetes mellitus in Taiwan. J Diabetes Investig. 2021;12:2080–2088. doi:10.1111/jdi.13595
5. Huy C, Loerbroks A, Hornemann A, Röhrig S, Schneider S. Prevalence, trend and determining factors of gestational diabetes in Germany. Geburtshilfe Frauenheilkd. 2012;72:311–315.
6. Furness D, Fenech M, Dekker G, Khong TY, Roberts C, Hague W. Folate, vitamin B12, vitamin B6 and homocysteine: impact on pregnancy outcome. Matern Child Nutr. 2013;9:155–166.
7. Wilson RD, O’Connor DL. Guideline No. 427: folic acid and multivitamin supplementation for prevention of folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can. 2022;44:707–719.e701. doi:10.1016/j.jogc.2022.04.004
8. Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Folic acid supplementation for the prevention of neural tube defects: US Preventive Services Task Force recommendation statement. JAMA. 2017;317:183–189. doi:10.1001/jama.2016.19438
9. Chinese Nutrition Society. Dietary guidelines for pregnant women. Chin J Perinat Med. 2016;19:641–648. In Chinese.
10. Cook S, Hess OM. Homocysteine and B vitamins. Handb Exp Pharmacol. 2005;2005:325–338.
11. Li Q, Zhang Y, Huang L, et al. High-dose folic acid supplement use from prepregnancy through midpregnancy is associated with increased risk of gestational diabetes mellitus: a prospective cohort study. Diabetes Care. 2019;42:e113–e115. doi:10.2337/dc18-2572
12. Zhu B, Ge X, Huang K, et al. Folic acid supplement intake in early pregnancy increases risk of gestational diabetes mellitus: evidence from a prospective cohort study. Diabetes Care. 2016;39:e36–37. doi:10.2337/dc15-2389
13. Li M, Li S, Chavarro JE, et al. Prepregnancy habitual intakes of total, supplemental, and food folate and risk of gestational diabetes mellitus: a prospective cohort study. Diabetes Care. 2019;42:1034–1041. doi:10.2337/dc18-2198
14. Bailey RL, Mills JL, Yetley EA, et al. Unmetabolized serum folic acid and its relation to folic acid intake from diet and supplements in a nationally representative sample of adults aged > or =60 y in the United States. Am J Clin Nutr. 2010;92:383–389. doi:10.3945/ajcn.2010.29499
15. Devalia V, Hamilton MS, Molloy AM. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol. 2014;166:496–513. doi:10.1111/bjh.12959
16. Cordero AM, Crider KS, Rogers LM, Cannon MJ, Berry RJ. Optimal serum and red blood cell folate concentrations in women of reproductive age for prevention of neural tube defects: World Health Organization guidelines. MMWR Morb Mortal Wkly Rep. 2015;64:421–423.
17. Li S, Hou Y, Yan X, et al. Joint effects of folate and vitamin B(12) imbalance with maternal characteristics on gestational diabetes mellitus. J Diabetes. 2019;11:744–751. doi:10.1111/1753-0407.12899
18. Lai JS, Pang WW, Cai S, et al. High folate and low vitamin B12 status during pregnancy is associated with gestational diabetes mellitus. Clin Nutr. 2018;37:940–947. doi:10.1016/j.clnu.2017.03.022
19. Wang L, Hou Y, Meng D, Yang L, Meng X, Liu F. Vitamin B12 and folate levels during pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Front Nutr. 2021;8:670289. doi:10.3389/fnut.2021.670289
20. Metzger BE, Gabbe SG, Persson B, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–682. doi:10.2337/dc10-0719
21. World Health Organization. Serum and red blood cell folate concentrations for assessing folate status in populations. Vitamin and Mineral Nutrition Information System. [WHO website]; 2012. Available from: http://www.who.int/iris/bitstream/10665/75584/3/WHO_NMH_NHD_EPG_12.1_chi.pdf.
22. Jankovic-Karasoulos T, Furness DL, Leemaqz SY, et al. Maternal folate, one-carbon metabolism and pregnancy outcomes. Matern Child Nutr. 2021;17:e13064. doi:10.1111/mcn.13064
23. Krishnaveni GV, Hill JC, Veena SR, et al. Low plasma vitamin B12 in pregnancy is associated with gestational ‘diabesity’ and later diabetes. Diabetologia. 2009;52:2350–2358. doi:10.1007/s00125-009-1499-0
24. Saravanan P, Sukumar N, Adaikalakoteswari A, et al. Association of maternal vitamin B(12) and folate levels in early pregnancy with gestational diabetes: a prospective UK cohort study (PRiDE study). Diabetologia. 2021;64:2170–2182. doi:10.1007/s00125-021-05510-7
25. Xie K, Xu P, Fu Z, et al. Association of maternal folate status in the second trimester of pregnancy with the risk of gestational diabetes mellitus. Food Sci Nutr. 2019;7:3759–3765. doi:10.1002/fsn3.1235
26. Guven MA, Kilinc M, Batukan C, Ekerbicer HC, Aksu T. Elevated second trimester serum homocysteine levels in women with gestational diabetes mellitus. Arch Gynecol Obstet. 2006;274:333–337. doi:10.1007/s00404-006-0191-6
27. Chen X, Zhang Y, Chen H, et al. Association of maternal folate and vitamin B(12) in early pregnancy with gestational diabetes mellitus: a prospective cohort study. Diabetes Care. 2021;44:217–223. doi:10.2337/dc20-1607
28. El-Khodary NM, Dabees H, Werida RH. Folic acid effect on homocysteine, sortilin levels and glycemic control in type 2 diabetes mellitus patients. Nutr Diabetes. 2022;12:33. doi:10.1038/s41387-022-00210-6
29. Gargari BP, Aghamohammadi V, Aliasgharzadeh A. Effect of folic acid supplementation on biochemical indices in overweight and obese men with type 2 diabetes. Diabetes Res Clin Pract. 2011;94:33–38. doi:10.1016/j.diabres.2011.07.003
30. Maher A, Sobczyńska-Malefora A. The relationship between folate, vitamin B12 and gestational diabetes mellitus with proposed mechanisms and foetal implications. J Family Reprod Health. 2021;15:141–149. doi:10.18502/jfrh.v15i3.7131
31. Crovetto F, Lattuada D, Rossi G, et al. A role for mitochondria in gestational diabetes mellitus? Gynecol Endocrinol. 2013;29:259–262. doi:10.3109/09513590.2012.736556
32. Zheng Y, Deng HY, Qiao ZY, Gong FX. Homocysteine level and gestational diabetes mellitus: a systematic review and meta-analysis. Gynecol Endocrinol. 2021;37:987–994. doi:10.1080/09513590.2021.1967314
33. Obeid R, Herrmann W. The emerging role of unmetabolized folic acid in human diseases: myth or reality? Curr Drug Metab. 2012;13:1184–1195. doi:10.2174/138920012802850137
34. van Weelden W, Seed PT, Antoun E, et al. Folate and vitamin B12 status: associations with maternal glucose and neonatal DNA methylation sites related to dysglycaemia, in pregnant women with obesity. J Dev Orig Health Dis. 2022;13:168–176. doi:10.1017/S2040174421000246
35. Elçi G, Çakmak A, Elçi E, Sayan S. The effect of advanced maternal age on perinatal outcomes in nulliparous pregnancies. J Perinat Med. 2022;50:1087–1095. doi:10.1515/jpm-2021-0298
36. Mi C, Liu H, Peng H, et al. Relationships among pre-pregnancy BMI, gestational, and postpartum oral glucose tolerance results in women with gestational diabetes mellitus. Front Nutr. 2021;8:714690. doi:10.3389/fnut.2021.714690
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.