Back to Journals » Psychology Research and Behavior Management » Volume 15
The Effects of Long Working Hours on Mental Health Among Resident Physicians in Saudi Arabia
Authors Bondagji D , Fakeerh M , Alwafi H , Khan AA
Received 13 April 2022
Accepted for publication 14 June 2022
Published 20 June 2022 Volume 2022:15 Pages 1545—1557
DOI https://doi.org/10.2147/PRBM.S370642
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Daniah Bondagji,1 Mutaz Fakeerh,1 Hassan Alwafi,2 Adeel Ahmed Khan1
1Saudi Board of Preventive Medicine, Ministry of Health, Makkah, Saudi Arabia; 2Department of Pharmacology and Toxicology, College of Medicine, Umm Alqura University, Makkah, Saudi Arabia
Correspondence: Daniah Bondagji, Saudi Board of Preventive Medicine, Ministry of Health, Makkah, Saudi Arabia, Tel +966566677474, Email [email protected]
Purpose: To examine the effect of long working hours on anxiety and depression among resident physicians working in Makkah, Saudi Arabia.
Methods: This is a cross-sectional study using an anonymous and confidential self-administered electronic questionnaire. Mental health status (depression and anxiety) is measured using hospital anxiety and depression scale. A multi-stage stratified sampling technique was used. Data were analyzed using the SPSS version 24.0. The Chi-square test and ordinal logistic regression (OLR) were used to test the association.
Results: A total of 258 medical residents participated in the study. The prevalence of anxiety was 39.5% (n=102) and depression was 20.9% (n=54). In multivariate OLR against anxiety, working more than 64 hours per week was significantly associated (p=0.013) with an increase in the odds of observing a higher level of anxiety (odds ratio=2.91, 95% confidence interval (CI):1.25– 6.77) compared with working up to 40 hours per week after adjusting for age, amount of sleep and exposure to injustice. For the depression multivariate OLR, it would increase the odds of observing a higher level of depression for working 41– 48, 49– 64 and more than 64 hours per week by 2.21 (95% CI:1.07– 4.58, P=0.033), 2.07 (95% CI:1.01– 4.27, P=0.049) and 2.37 (95% CI:1.03– 5.50, P=0.044) respectively, compared with working up to 40 hours per week and adjusting for the amount of sleep and exposure to injustice.
Conclusion: Resident physicians are at increased risk of developing anxiety and depression which is influenced by long working hours and a variety of other factors. Therefore, attention needs to be paid to this association. The implementation of interventions for the prevention and screening of physicians’ mental health disorders is needed.
Keywords: long working hours, mental health, anxiety, depression, physicians
Introduction
The life of physicians is extremely demanding as they are required to work for extended hours as compared to professionals in other fields.1,2 Recently, the flow of patients requiring prompt care increased drastically due to the COVID-19 pandemic; this increased the workload and duty hours among healthcare workers.3 The COVID-19 pandemic has significantly impacted the mental health of general population,4,5 as well as healthcare workers including medical students.6–8 Many studies conducted recently have shown that working for long hours has a negative impact on physical and mental health.9–11 Additionally, the workers’ quality of life including physicians is undesirably affected by long working hours. As long working hours cause sleep disturbances and affect the efficiency of an individual’s social role.12 Long working hours may also contribute to an increased risk of suicide. A Google-based approach could be used to monitor suicide since people at risk often search the internet for information and news about self-harm and suicide.13
According to the World Health Organization and the International Labour Organization (ILO), the issue of long working hours is highly prevalent, and it has become a global concern as it can take a severe toll on the health and well-being of workers.14 Therefore, a specific number of working hours have been suggested by the ILO and have been legislated for through the labor laws of many countries, including Saudi Arabia.15,16 However, not all hospitals and healthcare organizations abide by these working hours and, as a result, physicians end up working much longer beyond them.17
The advised working hours in many developed countries vary between 35 to 40 hours a week.9 The European Commission has suggested that the duration should not exceed 48 hours per week, including overtime.18 The Occupational Safety and Health Administration, defines a normal and healthy work shift as “a work period of no more than eight consecutive hours during the day, five days a week, with at least an eight-hour rest”.19 The ILO also advises that working hours should be limited to an 8-hour shift a day, and they should exceed no more than 48 hours in total per week.20 Likewise, the regulations recommended by the Saudi Ministry of Human Resources state the working hours of healthcare workers should range between 40 to 48 hours per week.16 Unfortunately, physicians in Saudi Arabia, like in other countries, work much more than these upper limits.17,21
The mental health of an individual can become severely compromised as a result of constant work pressures and related stressors.22 Working long hours is one of the main work stressors that negatively impact mental health, particularly concerning anxiety and depression.12 Among physicians, anxiety and depression, which have been found to be associated with long working hours, are the most commonly reported health issues.1,21,23 The prevalence of anxiety and depression among doctors was 25.8% and 20.5% respectively during the COVID-19 pandemic in the pooled data of a recently conducted systematic review.24 These mental health issues often result in poor concentration, work performance, and quality of care, which, in turn, increases the risk of committing medical errors.25 This necessitates the monitoring of physicians’ mental health and addressing factors that affect it negatively.
In this study, we hypothesize that long working hours are associated with mental health disorders especially among physician’s working day in and day out in hospitals and clinical settings. Therefore, we examined the effect of long working hours on anxiety and depression among resident physicians working in the public sector hospitals of Makkah, Saudi Arabia.
Materials and Methods
Study Setting
We conducted a cross-sectional study among physicians, including general practitioners (GPs) and residents from various specialities of all the public sector hospitals in Makkah city, Saudi Arabia. The study was conducted between September and November 2021.
Study Design and Participants’ Recruitment
A self-administered electronic questionnaire was administered. GPs and residents, either enrolled in a residency program or not, working in any medical or surgical departments in one of Makkah’s public sector hospitals were eligible for participation in this study. Physicians with higher classification, including specialists and consultants, were excluded. The participants were informed that the questionnaire was anonymous and confidential and that their information would be used for academic purposes only. Participation in the study was voluntary and the participants were not allowed to proceed to the questionnaire until they acknowledged the informed consent statement, in compliance with the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board, General Directorate of Health, Makkah (H-02-K-076-0320-273).
Sampling Strategy
A multi-stage stratified sampling technique was utilized to yield participation from all public sector hospitals (Al-Noor Specialized Hospital, King Abdullah Medical City, the Maternity and Children Hospital, King Faisal Hospital, King Abdulaziz Hospital, Hera General Hospital, Ajiyad Hospital, and the Security Forces Hospital) and all specialties to ensure sample representation. We took each hospital as a primary stratum and, according to the population of each, the size of the stratum was determined compared to the total population. Then, each hospital department was taken as the secondary stratum.
The self-reported electronic questionnaire was sent to each department, with a cover letter containing a participation request and the study purpose. The head of the department, residency program director and chief resident of each department in all the hospitals were contacted and asked to distribute the anonymous questionnaire among their residents electronically, and a reminder message was sent afterwards. All the residents were invited, and those who were keen to participate formed the study population. This approach allowed the researchers to reach almost all members of the targeted population to gain the participation of the largest possible number.
Sample Size Calculation
Resident physicians in Makkah public sector hospitals comprised about 600 residents, which represented the targeted study population. The minimum sample size to obtain a 95% confidence interval (CI) with 5% sample error and hypothesized frequency of outcome factor in the population of 50% ±5 where the population proportion is unknown is 235 participants.
The Questionnaire Tools
The electronic self-administered questionnaire, written in English, consisted of four parts: personal and demographic factors, general health, work history, and mental health status.
The first part contained the sample’s personal and demographic characteristics, including age, gender, nationality, marital status, financial situation and accommodation. The second part was about the participants’ general health and past medical history, including important mental health risk factors such as a family history of psychological disorders; family and social support; amount of sleep; exposure to loneliness, violence or abuse and injustice in the workplace; personality factors, like self-esteem; the ability to solve problems, and difficulties in communication. The workplace injustice was defined for the participants as being exposed to harassment, discrimination or bullying based on sociodemographic characteristics, health condition and job title in their hospitals. Information about mental health risk factors was obtained using a series of clear and simple “yes or no” questions. We also assessed the exposure to major events which was defined as being exposed to at least one of the following: marriage, divorce, death of relative or friend, new job, loss of job, accidents, long term injury, violence, bullying or bankruptcy. Working hours were assessed in the work history section using six questions. These questions were about type of duty, breaks during the shift, length and number of on-calls, weekend duties, and total working hours per week. The total working hours per week was the main independent variable. The first three parts of the questionnaire were validated by experts in the field. The last part assessed the mental health status of the participants based on depression and anxiety. The depression and anxiety levels were measured using the hospital anxiety and depression scale (HADS). HADS is a validated tool, designed in 1983 by Zigmond and Snaith to diagnose and evaluate anxiety and depression symptoms using 14 items.26 HADS consists of two scales, one for anxiety (HADS a) and the other for depression (HADS d). The scales are simple, fast and easy to complete by the participants.27 Depression and anxiety are reported on a three-point Likert scale ranging from (0–3). The standard scoring algorithm was used: anxiety = sum of items 1, 3*5*7, 9, 11*13* and depression = sum of items 2, 4, 6*8*10*12, 14, where starred items are reverse coded. The total scores on these subscales range from 0–21. A score of 0–7 is considered to be normal, 8–10 borderline, and from 11–21 as either anxious or depressed. It has been validated in many settings, including general practice and community settings in several languages and countries.28–30 HADS is recommended by the National Institute for Health and Care Excellence for the diagnosis of depression and anxiety.31
Pretesting the Questionnaire
The first three parts of the questionnaire were reviewed by experts in the field from different specialties, including occupational, psychiatric, and preventive medicine. Questions that were approved based on being understandable, relevant, and can be solved without assistance remained in the final questionnaire. A pilot study was performed using the final draft of the questionnaire by recruiting a convenience sample of 20 medical residents who were not from the study population. The clarity of the questions, as well as the ability to understand and answer them, were tested by examining the responses. The pilot participants were asked to provide their feedback on the questionnaire structure and, following their feedback, questions were again modified accordingly.
Statistical Analysis
Data were analyzed using the SPSS version 24.0. To investigate the association between long working hours and mental health status, descriptive and inferential analyses of the data were carried out. A descriptive analysis was used to describe, summarize and report the data, while inferential statistics were used to identify risk factors for depression and anxiety and to measure the association between working hours and mental health status. Mental health status (depression and anxiety) was measured using the HADS a and d (the dependent variables of the study). The Chi-square test and ordinal logistic regression (OLR) were used to test the association of all the variables with the dependent (anxiety and depression) and the main independent (total working hours per week) variables. Potential confounders were identified using the univariate OLR against depression, anxiety and total working hours to determine the regression coefficients, p-values, odds ratios (ORs) and 95% CI. In the multivariate OLR analysis, there were two main models, one for anxiety and the other for depression. The statistical significant level of < 0.05 for p-value was used.
Results
Study Participants’ Characteristics
A total of 258 medical residents from all the public sector hospitals in Makkah city participated in the study (response rate of 43%). More than half of the participants were males (n= 143, 55.4%). The median age of the participants was 29 years, ranging from 24 to 64 years. Most of the participants were ≤ 31 years (69.0%). Only 2.3% (n=6) of the participants were divorced, while those married or single were 59.7% and 38.0%, respectively. Half of the participants (n=132, 51.2%) were the main provider for their families. Table 1 shows the demographic data in detail.
 |
Table 1 Demographic Features Among Study Participants and Their Association with Anxiety and Depression |
More than half the participants had never smoked (n=144, 55.8%), while regular smokers, occasional smokers and ex-smokers were 20.9%, 17.4% and 5.8%, respectively. The vast majority of participants had no history of chronic diseases (n=203, 78.7%) and no family history of psychological disorders (n=201, 77.9%). The prevalence of obesity among the participants was 27.5% (n=71) and overweight was 32.6% (n=84). For the amount of sleep, 8.9% selected “far from enough”, 46.5% selected “not really enough”, 38.4% selected “basically enough” and only 6.2% selected “definitely enough”. For healthy lifestyle, 24.0% of the participants exercised regularly and 31.0% were on a healthy diet.
Prevalence of Anxiety and Depression
The prevalence of anxiety among the participants was 39.5% (n=102) (95% CI:33.5–45.8); the rest were borderline (27.5%, n=71, 95% CI:22.2–33.4) and normal (32.9%, n=85, 95% CI:27.2–39.0) (Table 2). For depression, the prevalence was 20.9% (n=54, 95% CI:16.1–26.4), while borderline and normal were (27.1%, n=70, 95% CI:21.8–33.0) and (51.9%, n=134, 95% CI:45.7–58.2), respectively (Table 2). In the stratified analysis, anxiety prevalence differed significantly among age groups (χ2=16.73, P=0.01): about 40.0% in both in the less than 27 years and 27 to 31 years groups, respectively; 55.1% in the age group 32 to 36 years, and 12.9% among participants older than 36 years. The prevalence of depression was higher among participants who were the main family provider (30.3%) compared to non-provider (11.1%) (χ2=16.92, P=0.000). Marital status, history of chronic disease, smoking status, and type of speciality had no statistically significant association with anxiety or depression. Table 1 details the prevalence of depression and anxiety stratified by demographic characteristics.
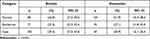 |
Table 2 Prevalence of Anxiety and Depression Among Study Participants |
Risk Factors
The participants were subdivided into four categories according to their total working hours per week (Table 3). Most of the participants did not have breaks during their duties (n=144, 55.8%): apart from those who worked up to 40 hours per week, 66.7% (n=34) of them had a break (p=0.002). However, according to the univariate OLR, the breaks during duties were not related to anxiety (p=0.505) or depression (p=0.171). About 54.7% of participants were experiencing problems at work, with a significant regression coefficient with anxiety (p=0.000), and depression (p=0.001) being recorded. However, there was no significance in the univariate OLR with total working hours per week (p=0.067).
 |
Table 3 Working Hours per Week Among Study Participants Stratified by Anxiety and Depression |
Table 4 examines the possible confounding factors through the univariate analysis using OLR against the dependent variables anxiety and depression, with the total working hours per week as the main independent variable. The variables that were found to be significant were age, amount of sleep, and injustice and these were included in the final models for adjustment.
 |
Table 4 Testing for Possible Confounders Using Univariate Ordinal Logistic Regression Against Anxiety, Depression (Dependents) and Total Working Hours per Week (Independent) |
In the multivariate OLR against anxiety (Table 5), working more than 64 hours per week was significantly associated (p=0.013) with increasing the odds of observing a higher level of anxiety by three times (OR=2.91, 95% CI:1.25–6.77) compared with working up to 40 hours per week. “Exposure to injustice” was significantly associated (p<0.0001) with increasing the odds of observing a higher level of anxiety by 3.1 (95% CI:1.73–5.44) compared to “not exposed to injustice”. Age was significantly associated: those less than 27 years (p=0.013), 27–31 years (p=0.002) and 32–36 years (p=0.001) experienced a higher level of anxiety (OR=2.93, 95% CI:1.25–6.84), (OR=3.51, 95% CI:1.58–7.79) and (OR=5.09, 95% CI:2.03–12.76) respectively, compared to those more than 36 years old. “Far from enough sleep” was also associated significantly (p=0.010) with an increase in the odds of observing a higher category of anxiety (OR=5.96, 95% CI:1.53–3.20) compared to “definitely enough sleep”.
 |
Table 5 Final Ordinal Logistic Regression Model for Anxiety Against Working Hours Adjusted for Age, Amount of Sleep, and Injustice in Workplace |
For the depression multivariate OLR model (Table 6), the regression coefficients for working hours per week categories (41–48, 49–64, and more than 64 hours) were significant compared to working up to 40 hours per week. The odds of observing a higher level of depression for working 41–48, 49–64 and more than 64 hours per week increased by 2.21 (95% CI:1.07–4.58, P=0.033), 2.07 (95% CI:1.01–4.27, P=0.049) and 2.37 (95% CI:1.03–5.50, P=0.044) respectively, compared with working up to 40 hours per week. “Injustice” also increased the odds of observing a higher category of depression by 74% (OR:1.74, 95% CI:1.02–2.96) as its regression coefficient was significant (p=0.042) compared to “not exposed to injustice.”
 |
Table 6 Final Ordinal Logistic Regression Model for Depression Against Working Hours Adjusted for Amount of Sleep and Injustice in Workplace |
Discussion
In this study, we have addressed one of the important risk factors in workplaces, long working hours and their impact on the mental health of resident physicians. About 67% of the participants experienced anxiety or were at risk of developing it, while about 48% were depressed or at risk of developing depression. The OR of anxiety for those working more than 64 hours per week was 2.9 compared with those working up to 40 hours per week, after adjusting for confounders using OLR. On the other hand, the depression OR for participants working 49–64 hours per week was 2.0 compared with those working up to 40 hours per week after adjusting for confounders using OLR. This result suggests that long working hours increased the risk of anxiety and depression.
Most of our participants worked for more than the recommended working hours.16,20 These results suggested that our physicians have longer work schedules than personnel in other professions.9 This is consistent with Hameed et al ’s findings,2 where a majority of the residents in Riyadh and Qassim province worked for 60 or more hours per week. Given these facts, we emphasize the need to find solutions for this issue. While the existence of working hours control programs is important, the implementation, monitoring and evaluation of these programs are of the utmost importance as most of the laws and regulations related to working hours are not truly applied.
We found that the prevalence of anxiety among resident physicians in our study is about four times that of the general population in Saudi Arabia.32 Alamri et al found that about 10.5% of their study participants of the general population suffered from moderate to severe features of anxiety, while the number was 39.5% among our participants.32 In this study, the proportion of anxiety and depression increased with the increase in working hours (Table 3). This indicates a dose-response relationship, which is similar to the finding of Bannai and Tamakoshi.9 Residents who worked for more than 64 hours per week are three times more likely to experience anxiety compared to residents working up to 40 hours per week. This is in accordance with previous findings among the general population and physicians that have demonstrated an association between long working hours and mental disorders.33,34 Among general workers in previous studies, long working hours were found to be related to an increase in the risk of anxiety by 1.74-fold for those who worked more than 55 hours per week compared to those who work 35–40 hours per week.33 This is the same for physicians, as was reported in a study conducted on Chinese physicians.21 They found that those working 60 hours or more per week were about twice as likely to report anxiety compared to those working 35–44 hours per week.21
The prevalence of depression in our study population was 20.9%. This is comparable to the previously published results of a study that included Saudi physicians, despite the use of a different scale, the Arabic version of Depression, Anxiety, and Stress Scale (DASS-21).32 However, the rate of depression among our participants is much lower than what was observed among frontline physicians caring for COVID-19 patients.35 Three recently published systematic reviews conducted to describe the prevalence of mental health disorders among healthcare workers dealing with COVID-19 patients reported the prevalence of depression among physicians of about 40%.36–39 This result demonstrates that the effect of the COVID-19 pandemic mostly impacted frontline physicians. However, other systematic reviews concluded that the COVID-19 pandemic affect the mental health of all health care workers and general population.4–7
According to the adjusted OLR for depression, all working hours categories of 48 hours or more were associated with more than double the odds of having depression compared to 40 hours per week (Table 6). This is not surprising as it is consistent with results from previously conducted studies on physicians in Saudi Arabia, Tunisia, Turkey, China, Japan, and Australia.2,21,23,34,39,40 However, a systematic review concluded that the association between long working hours and depression is inconclusive.41 This contradictory finding indicates the need for further prospective research with a powerful design to investigate this relationship. Despite this, no one can debate the importance of working hours regulations in maintaining the mental health and well-being of physicians.42 Prevention of mental disorders among physicians is crucial in producing decent medical care.21 To do that, adopting a systematic approach aimed at protecting physicians’ mental health and managing long working hours imposed by workplaces is mandatory.42
Age is one of the main factors related to mental disorders;43 this is consistent with our results. The proportion of anxiety decreased in older age groups and decreased markedly in the oldest age group (36 years or more). This echoes the result of a previously published study among the Saudi population.32 In an adjusted OLR, the participants aged 36 years or more had a 66% lower risk of acquiring anxiety compared to participants aged 27 years and younger (p=0.013). In our study, age was related significantly to long working hours and anxiety and considered to be a confounder; therefore, it was included for adjustment in the final model. Injustice was also added to the final models due to its significant association with long working hours and both depression and anxiety. Exposure to injustice negatively impacts emotional responses and reinforces unhealthy behaviors. These, in turn, increase the risk of depression and anxiety.44
Regarding depression, being the main family provider was significantly associated with depression (OR=2.60, 95% CI:1.61–4.20, p=0.000). This is per other studies stating that physicians’ mental status is negatively impacted as family commitments increase.45 Our study showed a significant association between the amount of sleep and the anxiety, depression and working hours categories, which is consistent with a previous study.28,46 This study highlights the need for proper working hours management to allow for adequate sleep to protect physicians’ mental health.
There were some limitations in this study that need to be acknowledged. We included only those residents who responded to the invitation to complete the questionnaire. It is possible that severely depressed or anxious residents may not have been interested in participating. Conversely, the residents who answered our questionnaire may have been more interested in issues related to long working hours and mental health. However, the results are not expected to be significantly affected by this factor. Another issue relates to the cross-sectional study design, which restricted the assessment of the temporality and causality of the observed associations. Furthermore, self-reported data is inevitably associated with recall bias. Therefore, longitudinal studies should be conducted in the future to confirm the conclusions of our study. Other factors that need to be addressed are affective temperaments due to their relationship with mental health. Particularly suicide risk, since affective temperaments may be independently associated with suicide.47 In a population with low suicide risk, such as ours, affective temperaments diagnosis may have a significant predictive value. This may open up opportunities for future research to clarify the role of affective temperaments and how to deal with their effects. Finally, the data was collected during the COVID-19 pandemic, which may have impacted the mental health status of the participants.
The results indicate that resident physicians working in Saudi Arabia have an increased risk of anxiety and depression due to long working hours. The Ministry of Health should be aware of the fact that long working hours could play a role in impacting the mental health of physicians. As a result, potential performance issues arise, and medical errors could occur more frequently. Thus, the need to standardize the working hours of physicians is imperative.
Conclusion
We found that resident physicians are at increased risk of developing anxiety and depression. This finding is influenced by long working hours. In addition, a variety of factors, including age, family responsibilities, social skills, speciality satisfaction, physical activity, amount of sleep, and exposure to major events, violence, injustice, and loneliness have been shown to significantly affect the risk of anxiety and depression. Attention needs to be paid to these associations and the impact of physician mental health on the quality of care. Additionally, there is a need to implement interventions for the prevention and screening of physicians’ mental health disorders to improve performance and health care outcomes.
Abbreviations
ILO, international labour organization; GPs, general practitioners; CI, confidence interval; HADS, hospital anxiety and depression scale; OLR, ordinal logistic regression; OR, odds ratio.
Ethics Approval and Informed Consent
IRB: Institutional Review Board, General Directorate of Health, Makkah (H-02-K-076-0320-273).
Consent: The participants were not allowed to proceed to the electronic questionnaire until they acknowledged the informed consent statement.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this study.
References
1. Tomioka K, Morita N, Saeki K, Okamoto N, Kurumatani N. Working hours, occupational stress and depression among physicians. Occup Med. 2011;61(3):163–170. doi:10.1093/occmed/kqr004
2. Hameed TK, Masuadi E, Asmary A, et al. A study of resident duty hours and burnout in a sample of Saudi residents. BMC Med Educ. 2018;18(1):1–6. doi:10.1186/s12909-018-1300-5
3. Muller AE, Hafstad EV, Himmels JP, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293:1134–1141. doi:10.1016/j.psychres.2020.113441
4. Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21(1):20–31. doi:10.1016/j.ijchp.2020.07.007
5. Santabárbara J, Lasheras I, Lipnicki DM, et al. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community based studies. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110207. doi:10.1016/j.pnpbp.2020.110207
6. Santabárbara J, Bueno-Notivol J, Lipnicki DM, et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110244. doi:10.1016/j.pnpbp.2021.110244
7. Olaya B, Pérez-Moreno M, Bueno-Notivol J, Gracia-García P, Lasheras I, Santabárbara J. Prevalence of depression among healthcare workers during the COVID-19 outbreak: a systematic review and meta analysis. J Clin Med. 2021;10(15):3406. doi:10.3390/jcm10153406
8. Lasheras I, Gracia-García P, Lipnicki DM, et al. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int J Environ Res Public Health. 2020;17(18):6603. doi:10.3390/ijerph17186603
9. Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40(1):5–18. doi:10.5271/sjweh.3388
10. Ervasti J, Pentti J, Nyberg ST, et al. Long working hours and risk of 50 health conditions and mortality outcomes: a multicohort study in four European countries. Lancet Reg Health Eur. 2021;11:1002–1012.
11. Afonso P, Fonseca M, Pires JF. Impact of working hours on sleep and mental health. Occup Med. 2017;67(5):377–382. doi:10.1093/occmed/kqx054
12. Park S, Kook H, Seok H, et al. The negative impact of long working hours on mental health in young Korean workers. PLoS One. 2020;15(8):e0236931. doi:10.1371/journal.pone.0236931
13. Solano P, Ustulin M, Pizzorno E, et al. A Google-based approach for monitoring suicide risk. Psychiatry Res. 2016;246:581–586. doi:10.1016/j.psychres.2016.10.030
14. Li J, Pega F, Ujita Y, et al. The effect of exposure to long working hours on ischaemic heart disease: a systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ Int. 2020;142:105739. doi:10.1016/j.envint.2020.105739
15. International Labour Organization. International labor standards on working time. Available from: https://www.ilo.org/global/standards/subjects–covered–by–international–labour–standards/working–time/lang–en/index.htm.
16. Saudi Ministry of Human Recourses and Social Development. Health jobs regulations; July 1, 2020. Available from: https://hrsd.gov.sa/sites/default/files/14012021.pdf.
17. Hameed TK, Al Dubayee MS, Masuadi EM, Al-Anzi FG, Al Asmary NA. Prevalence of depressive symptoms and excessive daytime sleepiness in a cohort of Saudi doctors under training: a cross sectional study. J Taibah Univ Med Sci. 2021;16(5):695–699. doi:10.1016/j.jtumed.2021.05.003
18. European Commission. Employment, social affairs & inclusion, working conditions - Working time directive. Available from: https://ec.europa.eu/social/main.jsp?catId=706&langId=en&intPageId=205.
19. Occupational Safety and Health Administration. Safety and health topics, long work hours, extended or irregular shifts, and worker fatigue. Available from: https://www.osha.gov/worker-fatigue.
20. International Labour Organization. General Survey concerning working-time instruments - Ensuring decent working time for the future, information and reports on the application of conventions and recommendations; February 23, 2018. Available from: https://www.ilo.org/wcmsp5/groups/public/—ed_norm/—relconf/documents/meetingdocument/wcms_618485.pdf.
21. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M, Maeno T. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):1–8. doi:10.1186/s12909-018-1171-9
22. Virtanen M, Jokela M, Madsen IE, et al. Long working hours and depressive symptoms: systematic review and meta-analysis of published studies and unpublished individual participant data. Scand J Work Environ Health. 2018;44(3):239–250. doi:10.5271/sjweh.3712
23. Gong Y, Han T, Chen W, et al. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS One. 2014;9(7):e103242. doi:10.1371/journal.pone.0103242
24. Johns G, Samuel V, Freemantle L, Lewis J, Waddington L. The global prevalence of depression and anxiety among doctors during the covid-19 pandemic: systematic review and meta-analysis. J Affect Disord. 2022;298:431–441. doi:10.1016/j.jad.2021.11.026
25. Joules N, Williams DM, Thompson AW. Depression in resident physicians: a systematic review. Open J Depression. 2014;3(03):89–100. doi:10.4236/ojd.2014.33013
26. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
27. Stern AF. The Hospital Anxiety and Depression Scale. Occup Med. 2014;64(5):393–394. doi:10.1093/occmed/kqu024
28. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/S0022-3999(01)00296-3
29. Snaith RP. The Hospital Anxiety and Depression Scale. Health Qual Life Outcomes. 2003;1(1):29–33. doi:10.1186/1477-7525-1-29
30. Herrmann C. International experiences with the Hospital Anxiety and Depression Scale-a review of validation data and clinical results. J Psychosom Res. 1997;42(1):17–41. doi:10.1016/S0022-3999(96)00216-4
31. National Collaborating Centre for Mental Health. Common mental health disorders: the NICE guideline on identification and pathways to care, national clinical guideline number 123; May 25, 2011. Available from: https://www.nice.org.uk/guidance/cg123/resources/common-mental-health-problems-identification-and-pathways-to-care-pdf-35109448223173.
32. Alamri HS, Algarni A, Shehata SF, et al. Prevalence of depression, anxiety, and stress among the general population in Saudi Arabia during Covid-19 pandemic. Int J Environ Res Public Health. 2020;17(24):9183. doi:10.3390/ijerph17249183
33. Virtanen M, Ferrie JE, Singh-Manoux A, et al. Long working hours and symptoms of anxiety and depression: a 5-year follow-up of the Whitehall II study. Psychol Med. 2011;41(12):2485–2494. doi:10.1017/S0033291711000171
34. Petrie K, Crawford J, LaMontagne AD, et al. Working hours, common mental disorder and suicidal ideation among junior doctors in Australia: a cross-sectional survey. BMJ Open. 2020;10(1):e033525. doi:10.1136/bmjopen-2019-033525
35. Al-Humadi S, Bronson B, Muhlrad S, Paulus M, Hong H, Cáceda R. Depression, suicidal thoughts, and burnout among physicians during the COVID-19 pandemic: a survey-based cross-sectional study. Acad Psychiatry. 2021;45(5):557–565. doi:10.1007/s40596-021-01490-3
36. Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021;121:104002. doi:10.1016/j.ijnurstu.2021.104002
37. Fernandez R, Sikhosana N, Green H, et al. Anxiety and depression among healthcare workers during the COVID-19 pandemic: a systematic umbrella review of the global evidence. BMJ Open. 2021;11(9):e054528. doi:10.1136/bmjopen-2021-054528
38. Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health. 2020;18(1):1–4. doi:10.1186/s12960-020-00544-1
39. Marzouk M, Ouanes-Besbes L, Ouanes I, Hammouda Z, Dachraoui F, Abroug F. Prevalence of anxiety and depressive symptoms among medical residents in Tunisia: a cross-sectional survey. BMJ Open. 2018;8(7):e020655. doi:10.1136/bmjopen-2017-020655
40. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290:113130. doi:10.1016/j.psychres.2020.113130
41. Watanabe K, Imamura K, Kawakami N. Working hours and the onset of depressive disorder: a systematic review and meta-analysis. Occup Environ Med. 2016;73(12):877–884. doi:10.1136/oemed-2016-103845
42. Levey RE. Sources of stress for residents and recommendations for programs to assist them. Acad Med. 2001;76(2):142–150. doi:10.1097/00001888-200102000-00010
43. Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30(1):11–22. doi:10.1017/S0033291799001452
44. Greenberg J. Organizational injustice as an occupational health risk. Acad Manag Ann. 2010;4(1):205–243. doi:10.5465/19416520.2010.481174
45. Erdur B, Ergin A, Turkcuer I, Parlak I, Ergin N, Boz B. A study of depression and anxiety among doctors working in emergency units in Denizli, Turkey. Emerg Med J. 2006;23(10):759–763. doi:10.1136/emj.2006.035071
46. Chen Y, Shen X, Feng J, et al. Prevalence and predictors of depression among emergency physicians: a national cross-sectional study. BMC Psychiatry. 2022;22(1):1–8. doi:10.1186/s12888-022-03687-8
47. Baldessarini RJ, Innamorati M, Erbuto D, et al. Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. J Affect Disord. 2017;210:19–21. doi:10.1016/j.jad.2016.12.003
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
