Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
The Effects of Inhaled Airway Directed Pharmacotherapy on Decline in Lung Function Parameters Among Indigenous Australian Adults With and Without Underlying Airway Disease
Authors Heraganahally SS , Ponneri TR, Howarth TP , Ben Saad H
Received 9 July 2021
Accepted for publication 13 September 2021
Published 29 September 2021 Volume 2021:16 Pages 2707—2720
DOI https://doi.org/10.2147/COPD.S328137
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Subash S Heraganahally,1– 3 Tarun R Ponneri,2 Timothy P Howarth,3,4 Helmi Ben Saad5
1Department of Respiratory and Sleep Medicine, Royal Darwin Hospital, Darwin, NT, Australia; 2Northern Territory Medical Program - College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia; 3Darwin Respiratory and Sleep Health, Darwin Private Hospital, Darwin, NT, Australia; 4College of Health and Human Sciences, Charles Darwin University, Darwin, NT, Australia; 5Université de Sousse, Faculté de Médecine de Sousse, Hôpital Farhat HACHED de Sousse, Laboratoire de Recherche “LR12SP09” “Insuffisance cardiaque”, Sousse, Tunisia
Correspondence: Subash S Heraganahally
Department of Respiratory and Sleep Medicine, Royal Darwin Hospital, Darwin, NT, Australia
Tel +61 8-89228888
; +61 8-89206306
Fax +61 8-89206309
Email [email protected]
Background: The trajectory of lung function decline among Indigenous patients with or without underlying chronic airway disease (COPD and concomitant bronchiectasis) and with use of inhaled pharmacotherapy, including inhaled corticosteroids (ICS), has not been reported in the past.
Methods: Adult Indigenous Australian patients identified to have undergone at least two or more lung function tests (LFTs) between 2012 and 2020 were assessed for changes in the lung function parameters (LFPs) between the first and last recorded LFTs.
Results: Of the total 1350 patients identified to have undergone LFTs, 965 were assessed to fulfil session quality, 115 (n=58 females) were eligible to be included with two or more LFTs. Among the 115 patients, 49% showed radiological evidence of airway diseases, and 77% were on airway directed inhaled pharmacotherapy. Median time between LFTs was 1.5 years (IQR 0.86,5.85), with no significant differences in LFPs noted between first and last LFT. Overall rate of change (mL/year) showed considerable variation for FVC (median − 37.55 mL/year [IQR − 159.88,92.67]) and FEV1 (− 18.74 mL/year [− 102.49,71.44]) with minimal change in FEV1/FVC (0.00 ratio/year [− 0.03,0.01]). When stratified by inhaled pharmacotherapy group, however, patients using ICS showed significantly greater rate of FEV1 decline (− 48.64 mL/year [− 110.18,62.5]) compared to those using pharmacotherapy with no ICS (15.46 mL/year [− 73.5,74.62]) and those using no pharmacotherapy (− 5.76 mL/year [− 63.19,67.34]) (p=0.022). Additionally, a greater proportion of these patients reached the threshold for excessive FEV1 decline (64%) compared to those using pharmacotherapy without ICS (44%) and those using no pharmacotherapy (52%).
Conclusion: Decline in LFPs occurs commonly among adult Indigenous population, especially, excessive so among those using inhaled pharmacotherapy containing ICS.
Keywords: Aboriginal, bronchiectasis, COPD, indigenous, inhaled corticosteroids, lung function test, ICS, LFT
Plain Language Summary
Indigenous Australians are noted to have higher prevalence of chronic respiratory disorders giving rise to higher morbidity and mortality. Airway directed inhaled pharmacotherapy, including inhaled corticosteroids (ICS) are widely utilised in the management of chronic airway disease. The efficacy of airway directed inhaled pharmacotherapy in reducing the rate of decline in lung function parameters (LFPs) has been well documented in various other ethnic non-Indigenous population, with varying outcomes. To date, there is no published literature evidence documenting the effects of airway directed pharmacotherapy on LFPs amongst an Indigenous population. This study examined the effects of inhaled pharmacotherapy on the longitudinal trends in LFPs among an adult Indigenous Australian cohort who were identified to have undergone multiple lung function tests (LFTs) with and without radiological evidence of chronic airway disease. Although, the results of the study showed that there was an overall decline in LFPs, there was no significant differences between first and subsequent LFPs over a 1.5-year period with or without radiological evidence of chronic airway disease nor with use of any type or combination of inhaled airway directed pharmacotherapy. However, excessive yearly decline in the FEV1 was noted to be substantially higher among patients using ICS containing pharmacotherapy. Hence, extreme caution may have to be exercised in using ICS in this Indigenous population until further large-scale studies are available.
Introduction
Respiratory disorders, including asthma, chronic obstructive pulmonary disease (COPD), bronchitis and bronchiectasis to name a few, are one of the leading causes of morbidity and mortality among Aboriginal and Torres Straits Islander populations of Australia (ATSI;1 henceforth respectfully referred to as Indigenous Australians or Indigenous people). The rates of asthma and COPD are reported to be 1.6 and 2.5 times higher, respectively among Indigenous Australians in comparison to their non-Indigenous counterparts.2–4 In the Northern territory (NT) of Australia, approximately 30% of the population self-identify as Indigenous Australians, the highest proportion compared to all other Australian states and territories.5,6 Chronic airway diseases, such as COPD and bronchiectasis are noted to be highly prevalent in the NT Indigenous population.7–11 Moreover, recently published data has shown that co-occurrence of COPD and bronchiectasis along with poor lung function parameters (LFPs) are highly prevalent among Indigenous people living in the Top end health service (TEHS) region of the NT of Australia.12–16
LFTs17 play an integral role in the diagnosis, management and monitoring of several respiratory conditions.18,19 Though natural decline in LFPs with aging is well recognised,20–22 there is evidence in the literature to suggest that decline in LFPs could be accelerated with smoking, and in the presence of pre-existing chronic respiratory conditions, in particular asthma, COPD and bronchiectasis.23–28 Although, airway directed inhaled pharmacotherapy, such as short-acting bronchodilator (SABA), short-acting muscarinic antagonists (SAMA), long-acting β-agonists (LABA), long-acting muscarinic antagonists (LAMA), and ICSs,29,30 are widely utilised and observed to be beneficial in the overall management of airway diseases, their efficacy on reducing the rate of decline of LFPs are varied.31–34 Several studies over the years have investigated the efficacy of airway directed therapy on long-term outcomes and some studies have utilised LFPs as a surrogate marker to assess if inhaled pharmacotherapy provide any additional benefits besides symptom control and exacerbation frequency.32–36
While there is evidence in the literature on longitudinal trends for LFPs and outcomes associated with airway directed pharmacotherapy among several ethnic populations, there is no current evidence on the longitudinal trends of LFPs among adult Indigenous Australians. This is despite overwhelming evidence in the literature documenting a higher burden of respiratory disease among the adult Indigenous Australian population.4,7–12 Furthermore, LFPs are noted to be significantly reduced among Indigenous Australians in comparison to non-Indigenous Australians.13–16 Thus, considering these aforementioned factors together (reduced LFPs, high burden of chronic respiratory disorders along with potential higher use of airway directed pharmacotherapy), there appears to be a critical need to investigate LFPs trajectory with and without radiological evidence of chronic airway diseases and the effects of inhaled pharmacotherapy on LFPs’ among the adult Indigenous Australian population. Therefore, the aim of this study was to assess the longitudinal trends in LFPs among an adult Indigenous Australian cohort who had undergone multiple LFTs in the TEHS region of the NT of Australia.
Methods
Setting
This study was conducted at the Respiratory and Sleep service based at the Royal Darwin hospital (RDH)/Darwin private hospital (DPH) in the TEHS region of the NT of Australia. The adult respiratory and sleep service based at RDH/DPH provides care for urban Darwin region as well as providing specialist outreach services8 to an average of 20 remote Indigenous communities each year at a frequency of one to three times per year, where 81% of NT Indigenous people reside in remote and regional communities.5,6 The respiratory service in addition to providing specialist consultation for patients with respiratory and sleep disorders, also facilitates conducting LFTs for both urban and remote Indigenous community patients. This study is a part of a larger project assessing factors influencing and implications of chest radiological findings and LFPs in the adult Indigenous Australians residing in the Top End NT of Australia.14 The project was approved by the Human Research Ethics Committee of the NT, TEHS and Menzies School of Health Research (Reference no: HREC 2019–3445). This study was conducted and reported according to strengthening reporting of health research involving Indigenous peoples,37 including consultation with Indigenous Australian representatives. Individual consent from the study participants was not obtained, as the study was retrospective in nature and no active interventions were investigated during this study. The lead investigator involved in this study is the usual specialist physician for the patients included in this study and have access to patients’ medical records, chest radiology and spirometry reports as a part of their usual medical care. Hence, separate patients’ consent to access their medical records or spirometry or radiology reports was not required and was approved by local ethics committee. The study was also conducted in accordance with the Declaration of Helsinki.
Study Participants and Inclusion Criteria
The study participants included were Indigenous Australian patients who had undergone at least two or more LFTs’ between 2012 and 2020. Patients were referred for LFTs by primary health practitioners, respiratory specialist and other specialist physicians as a part of routine clinical care. If the patients had undergone multiple LFTs during the study period, the first and the last most acceptable and reproducible LFTs were included.
Lung Function Testing and Rate of Decline in LFPs
All LFTs were performed according to the American thoracic and the European respiratory societies (ATS/ERS) guidelines/recommendations, including calibration of equipment and quality assurance.38 More details are available from previous reports from our centre.13,14 The LFTs were performed via a portable single-breath diffusing capacity device “EasyOne Pro®, ndd Medical Technologies”.39 All volume-time and flow-volume graphs were individually assessed for acceptability for session quality. Only LFTs graded as acceptable for session quality were included in this study. The following LFPs were collected: Forced expiratory volume in one second (FEV1, L), Forced vital capacity (FVC, L), and FEV1/FVC (absolute value). In our centre and faced with the lack of specific spirometric norms for the Australian Indigenous population, the LFPs predicted values were calculated using the National health and nutrition examination survey (NHANES-III) Caucasian reference set’s (“other ethnicity”).40
All patients undergoing elective spirometry testing were instructed to refrain from smoking for at least two to four hours prior to spirometry testing and to avoid using airway directed inhaled pharmacotherapy during the preceding 6–12 hours of spirometry testing. According to the global initiative for chronic obstructive lung disease criteria used in earlier burden of obstructive lung disease studies, bronchodilator responsiveness (BDR) for spirometry parameters were assessed 15–20 minutes after inhalation of 400 µg of salbutamol via a spacer.41 The presence of a clinically significant BDR was determined if there was a post-bronchodilator (BD) increase in FEV1 and/or FVC of ≥ 12% and ≥ 200 mL from the pre-BD FEV1 and/or FVC values.42
Rate of decline in LFPs was calculated as “((LFP value changes/days to subsequent LFT) × 365.25)” to give a value of mL/year. Threshold for excessive decline of FEV1 was calculated using the following method recommended by the ATS:43 (baseline predicted FEV1 – current predicted FEV1) + (0.15 × baseline absolute FEV1). The threshold was considered reached if absolute difference > calculated difference.
Clinical Data Collection
As per standard protocol, patients’ age (on the date of testing), sex, height, weight and body mass index (BMI, kg/m2) were recorded. Smoking history was also recorded. Chest radiology, including Chest X-ray and chest computed tomography (CT) reports when available were assessed for the presence and type of underlying airway disease, in particular radiological evidence for the presence of COPD and for presence of bronchiectasis.
Inhaled Pharmacotherapy Data
All available electronic medical records were searched to document the details of any type or combination of airway directed inhaled pharmacotherapy, more specifically – SABA; SAMA; LABA; LAMA; and ICS in-between the first and last recorded LFTs. The inhaled pharmacotherapy was initiated as per the discretion of treating physician, including remote community health primary health care physicians.
Statistical Analysis
Continuous parameters were tested for normality with the Shapiro Wilks distribution test. Age, height and all LFPs were found to approximate normal distribution; however, weight, BMI, and rate of change in LFPs from first to last LFTs deviated to a significant extent, and thus were treated as non-parametric. Non-parametric parameters were presented as medians (interquartile ranges), normally distributed parameters as means (95% confidence intervals [CIs]), and categorical parameters as numbers (%). Clinical characteristics were compared between first and last recorded LFTs with proportions z-tests for categorical parameters, Students t-test for parameters approximating normal distribution and equality of medians test for non-parametric parameters. LFPs absolute and predicted values were tested between first and last LFTs and by presence of evidence for airway disease using two-sided Students t-tests while the differences by level of pharmacotherapy reported were tested via ANOVA. Rate of change was compared between participants with or without evidence of airway disease via Wilcoxon rank-sum test, and by level of pharmacotherapy reported via quantile regression. All data were analysed in STATA IC 15 (StataCorp, Texas) and alpha was set to 0.05 throughout.
Results
Study Participants
A total of 1350 Indigenous patients were identified to have undergone LFTs between 2012 and 2020, of them 965 (71.4%) were assessed to fulfil the ATS/ERS criteria for LFTs session quality, and 115 patients (50% female) had at least two LFTs, with 32 (27%) having three or more LFTs. Therefore, 115 patients who were identified to have undergone two or more LFTs were eligible to be included in this study for analysis (Figure 1).
 |
Figure 1 Study flow chart. |
LFTs and Demographic Data
Mean age of the study patients at the first LFT was 50.4 years (95% CI 48.29, 52.45) with a median time between first and last recorded LFT of 1.52 years (IQR 0.86, 5.85). The majority (90%, n=103) of patients had a history of smoking and were typically overweight or obese (62%), with minimal fluctuation in either weight or height between the first and last LFTs (Table 1). Chest radiology was available in 112 (97%) patients [Chest CT n=74 (64%), Chest X-ray n=112 (97%)] and demonstrated presence of COPD and bronchiectasis in 56 (48%) of the study patients. Pharmacotherapy data was available for 113 (98%) patients, therefore further analysis pertaining to pharmacotherapy groupings was conducted with a denominator of 113.
 |
Table 1 Clinical Characteristics of Patients with Multiple Lung Function Tests (LFTs) Recorded (n = 115) |
Lung Function Trends with or without Radiological Evidence for Airway Disease and Inhaled Pharmacotherapy
Overall, patients showed an absolute change from first to final LFT in pre-BD values of: FVC 40.91 mL (95% CI −28.31, 110.12), FEV1 50.76 mL (95% CI −3.16, 104.68), FEV1/FVC 0.02 (95% CI 0, 0.03) (Table 2). There were no statistically significant differences noted between LFPs for first or final LFT. When stratified by underlying radiological evidence for chronic airway disease, significant differences in absolute and predicted values of FVC, FEV1 and FEV1/FVC were noted (p<0.05, Supplementary Table S1 [lower values with chronic airway disease]) though no significant differences in LFPs were noted between first and last LFT for either with or without radiological evidence of airway disease (Supplementary Table S1). Further, when stratified by use of pharmacotherapy (including ICS with or without LABA or LAMA combination) significant differences in absolute and predicted values of FVC, FEV1 and FEV1/FVC were noted (p<0.05, data not shown (lowest values for participants in the ICS group) though no significant differences in LFPs were noted between first and last LFT for any type or combination of inhaled pharmacotherapy use (Supplementary Table S2).
 |
Table 2 Lung Function Parameters (LFPs) at First and Final Lung Function Test (LFT) (n = 115) |
Yearly Decline in LFPs in Relation to Radiology, Smoking and Inhaled Pharmacotherapy Use
The overall median decline rate for FEV1 was −18.74 mL/year (IQR −102.49, 71.44), with no significant difference noted between patients with/without evidence of airway disease (Table 3). The proportion of patients who exhibited significant excessive decline in FEV1,43 was observed to be 57% which varied only slightly between those with or without evidence of airway disease. A subgroup analysis was conducted to determine if smoking status (never, former, current) influenced the rate of decline in LFPs. No significant differences were noted in decline rate for any LFPs between the smoking status categories (Table 4).
 |
Table 3 Rate of Change in Lung Function Parameters (LFPs) Values (Ml/Year or %/Year for Predicted Values) Stratified by Radiological Evidence for Chronic Airway Disease |
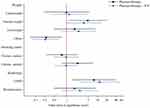
Significant variation in rate of decline was noted between differing inhaled pharmacotherapy usage (Table 5). Patients who reported pharmacotherapy use including ICS appeared to show greater decline for FVC and FEV1 values, more significantly for FEV1 pre-BD absolute and predicted values. Following adjustment for sex and evidence of airway disease, the differences noted were attenuated to approaching borderline significance (p=0.083 and p=0.079, pre-BD FEV1 absolute and predicted respectively, data not shown), though FVC post-BD absolute rate of change showed a significant association (p=0.04). Excessive FEV1 decline was observed more commonly among patients using pharmacotherapy with ICS with almost two-thirds (64%) showing excessive decline in comparison to patients using non-ICS pharmacotherapy (44%) and those using no pharmacotherapy (52%) (Table 5).
Clinical Characteristics by Pharmacotherapy Use – Subgroup Analysis
A subgroup analysis was undertaken to understand the clinical profile of patients in relation to pharmacotherapy use, due to the variation observed in the rate of change for LFPs in this group, and also due to higher proportion of excessive FEV1 decline among patients using ICS (Table 6). Patients using ICS pharmacotherapy were significantly older and had lower BMI in comparison to patients not on any pharmacotherapy. Use of pharmacotherapy among patients demonstrating radiological abnormalities was also higher, in particular in patients with COPD and bronchiectasis in the ICS group (Figures 2 and 3). All-cause mortality data showed that significantly higher proportion of patients using ICS were deceased (19%) in comparison to patients with no pharmacotherapy or with non-ICS pharmacotherapy (0–4%) (p=0.016) by the end of the study period.
 |
Table 6 Clinical Characteristics of Patients with Multiple Lung Function Tests (LFTs) Recorded Stratified by Level of Pharmacotherapy Reported |
Discussion
To the best of our knowledge, this is the first study to document lung function trends with or without radiological evidence of chronic airway disease and the effects of airway directed inhaled pharmacotherapy amongst an adult Indigenous Australian population.
This study demonstrated several key findings:
(i) Overall, there is no statistically significant difference in the LFPs between first and subsequent LFTs over a 1.5-year period, neither with nor without radiological evidence of airway disease, nor with use of any form or combination of inhaled pharmacotherapy;
(ii) A higher proportion of patients with radiological evidence of COPD either with or without concurrent bronchiectasis are prescribed ICS pharmacotherapy;
(iii) Excessive yearly decline in FEV1 is substantially higher among patients using ICS pharmacotherapy in comparison to patients with non-ICS or no inhaled pharmacotherapy; and
(iv) All-cause mortality is higher among patients using ICS containing pharmacotherapy.
Indigenous people around the world experience a higher burden of chronic health conditions, including advanced respiratory conditions.44–46 Despite evidence in the literature to suggest chronic respiratory conditions along with poor LFPs are highly prevalent among Indigenous population, including in the adult Indigenous Australians,1,4,7–16 there is no published data examining the effects of airway directed inhaled pharmacotherapy on LFPs trajectory in this population. Hence, we believe our current study is of significant value in addressing this gap in our knowledge.
Several studies in the past have examined the effects of inhaled pharmacotherapy on LFPs among patients with airway diseases.25,26,28,29,31–36 However, there appears to be conflicting and contradicting information in the literature, in particular in relation to the utility of ICS in the management of patients with COPD. Some studies have demonstrated beneficial effects,32,34,47,48 whereas other reports have indicated potential adverse consequences with inhaled pharmacotherapy.49–54 In a similar vein, controversy exists over the use of inhaled pharmacotherapy among patients with bronchiectasis.55–59 These aspects are of significant clinical relevance in the Australian setting, where a significant proportion of Australian Indigenous patients demonstrate concurrent presence of COPD and bronchiectasis.7–9,12 Hence, lack of established evidence may give rise to an unprecedented treatment management dilemma and challenges for this Indigenous population.
Previous studies in other non-Indigenous population have demonstrated that inhaled pharmacotherapy among patients with COPD may be helpful in reducing decline in FEV1, however, the beneficial effects of inhaled pharmacotherapy in attenuating the rate of decline in FEV1 appears to fade away on longer duration of follow up (> 1 year).34–36,47,48,60 This indicates a time dependent benefit of ICS, which appears to be most effective earlier in the disease’s spectrum. Other studies have demonstrated that long term benefits of inhaled pharmacotherapy in reducing LFPs decline is more likely to be among patients with moderate-to-severe COPD, with fewer pack-years of smoking and less severe emphysema.61 Moreover, it is observed that patients with lower FEV1 at baseline may demonstrate higher decline on follow-up.62 Our study cohort demonstrates an absolute decline in LFPs over the 1.5-years, however the changes were not statistically significant (Table 2), even after adjusting for radiological evidence of airway disease and inhaled pharmacotherapy use (Supplementary Tables S1 and S2). These findings (no significant change between first and last PFTs) might be a result of having low baseline LFPs to begin with and/or as a result of our study participants having higher severity or advanced disease alongside with higher smoking prevalence. Hence, these factors may be influential in not demonstrating significant variation between the first and the subsequent LFTs in our study participants. However, as the median duration between the first and final LFT in our study was about 1.5 years, it is not clear if shorter or longer follow-up LFTs would have altered our observed outcomes.
One finding is of particular interest in this study: yearly excessive decline in LFPs was higher among patients on ICS, alongside higher overall mortality in this group. The study participants using non-ICS containing pharmacotherapy demonstrated a lesser degree of decline in LFPs (Table 4). It may be reasonable to speculate that patients being prescribed ICS may be at the higher end of the disease spectrum and inevitable to have higher overall all-cause mortality. On the other hand, long-term use of ICS may be detrimental by exacerbating recurrent airway infections/inflammation and in turn facilitating excessive decline in LFPs, especially, among those patients with concomitant COPD and bronchiectasis.
Despite limited scientific evidence on the usefulness or utility of inhaled pharmacotherapy among Indigenous population, airway directed pharmacotherapy continues to be utilised extensively and access to appropriate pharmacotherapies can be a challenge among Indigenous people living in the remote and regional communities.63 Researchers have more than often questioned whether inhaled pharmacotherapy; in particular, ICS is a friend or foe in the management of CODP.64 Moreover, management guidelines developed and recommended for other ethnic population may not be applicable or relevant to Indigenous population.
In this study, the authors do acknowledge that the number of study participants was less than ideal for high-powered conclusions in a study such as this. Moreover, in this study participants with normal radiology, one may not be able to come to a clear conclusion for the presence or absence of early COPD especially with smoking history or asthma. The correlation of respiratory symptoms to chest radiological could be variable or vice versa as well, especially with airway disease (symptomatic with normal radiology/asymptomatic with abnormal radiology). We chose to utilise chest radiology to document the presence or absence of chronic airway disease, due to the reason for this study being retrospective in nature and also purely relying on current or previous respiratory symptoms would have potentially lead to recall bias in the adult study participants. Furthermore, smoking rates are highly prevalent in the adult Indigenous population.14 In this study, we observed 90% of the study participants had a smoking history and only 12 did not have documented smoking history, although, due to the high smoking prevalence the likelihood of passive smoking could be very high as well. Hence, the results from the subgroup analysis in this current study documenting LFPs decline rate must be interpreted with caution. However, there is room for future prospective research.
Nevertheless, a study of this kind for the first time has highlighted that there are no significant differences between first and subsequent LFPs over a 1.5-year period among Australian Indigenous patients with or without radiological evidence of COPD with or without concurrent bronchiectasis nor with use of inhaled airway directed pharmacotherapy. However, excessive yearly decline in FEV1 is noted to be higher among patients using ICS containing pharmacotherapy alongside higher all-cause mortality in comparison to patients with non-ICS containing inhaled pharmacotherapy or no pharmacotherapy. In the light of this study, and the authors several years of experience in managing Indigenous patients with chronic health conditions,7–16,54,65–72 until and unless further prospective large scale studies are available to prove or disprove if ICS pharmacotherapy is a friend or foe in the management among Indigenous people, we sincerely recommend and advocate extreme caution in utilising ICS among the NT Indigenous population and phenotypic markers should be utilised to guide airway directed inhaled pharmacotherapy.61,64,73,74
Study Limitations
The results of this study are restricted to the study participants from the TEHS region of the NT of Australia. The results and outcomes may or may not be applicable to other Indigenous populations. The authors acknowledge that the number of study participants were less than desired for a study such as this. However, it may be reasonable to accept this legitimate limitation given the practicality and complexity involved in both advanced healthcare access and study recruitment for Indigenous Australian participants. The majority (81%) of the NTs Indigenous Australian population reside in remote or very remote communities which imposes geographical isolation and logistical challenges as many communities may only be accessed seasonally by light aircraft.5,6 Therefore, access to LFTs are limited. We also did not assess the severity of airway disease on chest radiology, which may have led to potential bias in the outcomes observed.75 Moreover, as this study was retrospective in nature predominantly investigating LFTs, respiratory symptoms were not assessed to document the symptom benefits of inhaled pharmacotherapy. We also did not examine the prevalence of asthma or asthma/COPD overlap nor adherence to inhaled pharmacotherapy. Moreover, with longer duration follow up the results observed in this population may differ. Nonetheless, this is the first ever study to document LFPs trajectory amongst an Indigenous Australian population on inhaled airway directed pharmacotherapy and provides a baseline for further prospective research.
Conclusion
Our study illustrates that Australian Indigenous patients demonstrate no significant change in LFPs in between first and subsequent LFTs over a 1.5-year time-period irrespective of presence or absence of radiological evidence for underlying airway disease nor with use of any or combination of inhaled pharmacotherapy. However, excessive yearly decline in the LFPs are substantially high both overall, and particularly so among patients using ICS containing pharmacotherapy. Until further large-scale studies are available, ICS containing pharmacotherapy has to be used wisely in this Indigenous population.
Abbreviation
ATS, American thoracic society; ATSI, Aboriginal or Torres Strait Islander; AV, Absolute value; BD, Bronchodilator; BDR, Bronchodilator responsiveness; BMI, Body mass index; CI, Confidence Interval; COPD, Chronic obstructive pulmonary disease; CT, Computed Tomography; DPH, Darwin private hospital; ERS, European respiratory society; FEV1, Forced expiratory volume in one second; FVC, Forced vital capacity; ICS, Inhaled corticosteroids; IQR, Interquartile range; LABA, Long-acting β-agonists; LAMA, Long-acting muscarinic antagonists; LFTs, Lung function tests; LFPs, Lung function parameters; LLN, lower limit of normal; NHANES III, National health and nutrition examination survey; NT, Northern territory; RDH, Royal Darwin hospital; SABA, Short-acting bronchodilator; SAMA, Short-acting muscarinic antagonists; TEHS, Top end health service.
Acknowledgments
We sincerely thank all the respiratory technologists and Respiratory Clinical Nurse Consultants from Darwin Respiratory and Sleep health and Royal Darwin Hospital, Darwin Private Hospital, Darwin, Australia, for facilitating and performing lung function testing for Indigenous study participants living in the remote and regional Indigenous communities during respiratory outreach visits. We thank Mr. Xinlin Jing, Health Information Services, Royal Darwin Hospital, Darwin, Northern Territory, Australia for helping with data collection for this study. We also extend our sincere appreciation to our Indigenous health workers, especially to Mr Izaak Thomas (Australian Indigenous Luritja descendent) from the respiratory chronic respiratory disease co-ordination division in reviewing and approving this manuscript for the appropriateness of the representation and respect in relation to the Indigenous context represented in this study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
All authors declare no conflicts of interest for this study.
References
1. Leading causes of mortality. Australian Institute of Health and Welfare 2020. Aboriginal and Torres Strait Islander Health Performance Framework 2020 summary report. Cat. no. IHPF 2. Canberra: AIHW. Available from: https://www.indigenoushpf.gov.au/publications/hpf-summary-2020.
2. Australian institute of health and welfare. Indigenous Australians more likely to die from CHD and COPD, but some positive trends emerging - Australian Institute of Health and Welfare; 2014. Available from: https://www.aihw.gov.au/news-media/media-releases/2014/june/indigenous-australians-more-likely-to-die-from-chd.
3. Australian institute of health and welfare. Asthma. Cat. no. ACM 33. Canberra: AIHW; 2020. Available from: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/asthma.
4. Jenkins CR, Chang AB, Poulos LM, Marks GB. Asthma in Indigenous Australians: so much yet to do for Indigenous lung health. Med J Aust. 2009;190(10):530–531. doi:10.5694/j.1326-5377.2009.tb02550.x
5. Australian bureau of statistics. Estimates of Aboriginal and Torres Strait Islander Australians. Canberra, Australia: ABS; 2016.
6. Australian bureau of statistics. Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure, July 2011. Canberra: Australian Bureau of Statistics; 2013.
7. Heraganahally S, Wasgewatta SL, McNamara K, et al. Chronic obstructive pulmonary disease in Aboriginal patients of The Northern Territory of Australia: a landscape perspective. Int J Chron Obstruct Pulmon Dis. 2019;14:2205–2217. doi:10.2147/COPD.S213947
8. Kruavit A, Fox M, Pearson R, Heraganahally S. Chronic respiratory disease in the regional and remote population of the Northern Territory Top End: a perspective from the specialist respiratory outreach service. Aust J Rural Health. 2017;25:275–284. doi:10.1111/ajr.12349
9. Mehra S, Chang AB, Lam CK, et al. Bronchiectasis among Australian Aboriginal and Non-Aboriginal patients in the regional and remote population of the Northern Territory of Australia. Rural Remote Health. 2021;6390. doi:10.22605/RRH6390
10. Heraganahally SS, Silva SAMS, Howarth TM, Kangaharan N, Majoni SW. Comparison of clinical manifestation among Australian Indigenous and non‐ Indigenous patients presenting with pleural effusion. Int Med J. 2021. doi:10.1111/imj.15310
11. Heraganahally SS, Mortimer N, Howarth T, et al. Utility and outcomes among Indigenous and non-Indigenous patients requiring domiciliary oxygen therapy in the regional and rural Australian population. Aust J Rural Health. 2021. doi:10.1111/ajr.12782
12. Heraganahally SS, Wasgewatta SL, McNamara K, et al. Chronic obstructive pulmonary disease with and without bronchiectasis in Aboriginal Australians – a comparative study. Int Med J. 2020;50(12):1505–1513. doi:10.1111/imj.14718
13. Schubert J, Kruavit A, Mehra S, Wasgewatta S, Chang AB, Heraganahally S. Prevalence and nature of lung function abnormalities among Indigenous Australians referred to specialist respiratory outreach clinics in the Northern Territory. Int Med J. 2019;49:217–224. doi:10.1111/imj.14112
14. Heraganahally SS, Howarth T, White E, Sorger L, Biancardi E, Ben Saad H. Lung function parameters among Australian Aboriginal “apparently healthy” adults: an Australian Caucasian and global lung function initiative (GLI-2012) various ethnic norms comparative study. Expert Rev Respir Med. 2020;23:1–11. doi:10.1080/17476348.2021.1847649
15. Howarth TP, Saad HB, Perez AJ, Atos CB, White E, Heraganahally SS. Comparison of diffusing capacity of carbon monoxide (DLCO) and total lung capacity (TLC) between Indigenous Australians and Australian Caucasian adults. PLoS One. 2021;16(4):e0248900. doi:10.1371/journal.pone.0248900
16. Heraganahally SS, Howarth T, Mo L, Sorger L, Saad HB. Critical analysis of spirometric patterns in correlation to chest computed tomography among adult Indigenous Australians with chronic airway diseases. Expert Rev Respir Med. 2021;15(9):1229–1238. doi:10.1080/17476348.2021.1928496
17. Johnson JD, Theurer WH. A stepwise approach to the interpretation of pulmonary function tests. Am Fam Physician. 2014;89(5):359–366.
18. Ranu H, Wilde M, Madden B. Pulmonary function tests. Ulster Med J. 2011;80(2):84–90.
19. Liang BM, Lam DC, Feng YL. Clinical applications of lung function tests: a revisit. Respirology. 2012;17(4):611–619. doi:10.1111/j.1440-1843.2012.02149.x
20. Ostrowski S, Bilan A. The natural history of respiratory system function. J Physiol Pharmacol. 2004;55(Suppl 3):95–100.
21. Van Oostrom SH, Engelfriet PM, Verschuren WMM, et al. Aging-related trajectories of lung function in the general population—The Doetinchem Cohort Study. PLoS One. 2018;13(5):e0197250. doi:10.1371/journal
22. Lak VWM, Skoog I, Guo X. Secular trends in lung function and its relation to survival in Swedish 75 year olds 1976–2006. Age Ageing. 2012;41:735–740. doi:10.1093/ageing/afs098
23. Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977;1(6077):1645–1648. doi:10.1136/bmj.1.6077.1645
24. Sears MR. Lung function decline in asthma. Eur Respir J. 2007;30(3):411–413. doi:10.1183/09031936.00080007
25. Leem AY, Park B, Kim YS, Chang J, Won S, Jung JY. Longitudinal decline in lung function: a community-based cohort study in Korea. Sci Rep. 2019;9:13614. doi:10.1038/s41598-019-49598-9
26. Tantucci C, Modina D. Lung function decline in COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:95–99. doi:10.2147/COPD.S27480
27. Martínez-García MA, Soler-Cataluña JJ, Perpiñá-Tordera M, Román-Sánchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non-cystic fibrosis bronchiectasis. Chest. 2007;132:1565–1572. doi:10.1378/chest.07-0490
28. Dijkstra A, Vonk JM, Jongepier H, et al. Lung function decline in asthma: association with inhaled corticosteroids, smoking and sex. Thorax. 2006;61(2):105–110. doi:10.1136/thx.2004.039271
29. Borghardt JM, Kloft C, Sharma A. Inhaled therapy in respiratory disease: the complex interplay of pulmonary kinetic processes. Can Respir J. 2018;19:2732017. doi:10.1155/2018/2732017
30. Usmani OS. Treating the small airways. Respiration. 2012;84:441–453. doi:10.1159/000343629
31. Almeida PCA, Ponte EV, Souza-Machado A, Cruz AA. Longitudinal trends in clinical characteristics and lung function of patients with severe asthma under treatment in Brazil. BMC Pulm Med. 2016;16:141. doi:10.1186/s12890-016-0302-5
32. Park HY, Lee SY, Kang D, et al. Favorable longitudinal change of lung function in patients with asthma-COPD overlap from a COPD cohort. Respir Res. 2018;19(1):36. doi:10.1186/s12931-018-0737-8
33. Lange P, Scharling H, Ulrik CS, Vestbo J. Inhaled corticosteroids and decline of lung function in community residents with asthma. Thorax. 2006;61(2):100–104. doi:10.1136/thx.2004.037978
34. Suissa S. Medications to modify lung function decline in chronic obstructive pulmonary disease: some hopeful signs. Am J Respir Crit Care Med. 2008;178(4):322–323. doi:10.1164/rccm.200805-721ED
35. Soriano JB, Sin DD, Zhang X, et al. A pooled analysis of FEV1 decline in COPD patients randomized to inhaled corticosteroids or placebo. Chest. 2007;131(3):682–689. doi:10.1378/chest.06-1696
36. Tashkin DP, Strange C. Inhaled corticosteroids for chronic obstructive pulmonary disease: what is their role in therapy? Int J Chron Obstruct Pulmon Dis. 2018;13:2587–2601. doi:10.2147/COPD.S172240
37. Huria T, Palmer SC, Pitama S, et al. Consolidated criteria for strengthening reporting of health research involving indigenous peoples: the CONSIDER statement. BMC Med Res Methodol. 2019;19:173. doi:10.1186/s12874-019-0815-8
38. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi:10.1183/09031936.05.00034805
39. NDD Medical Technologies. EasyOne Pro®; 2017. Available from: https://www.ndd.ch/en/product/easyone-pro.html.
40. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med. 1999;159(1):179–187. doi:10.1164/ajrccm.159.1.9712108
41. Cooksley NA, Atkinson D, Marks GB, et al. Prevalence of airflow obstruction and reduced forced vital capacity in an Aboriginal Australian population: the cross‐sectional BOLD study. Respirology. 2015;20:766–774. doi:10.1111/resp.12482
42. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Available from: http://www.goldcopd.org.
43. Redlich CA, Tarlo SM, Hankinson JL, et al. Official American thoracic society technical standards: spirometry in the occupational setting. Am J Respir Crit Care Med. 2014;189(8):984–994. doi:10.1164/rccm.201402-0337ST
44. State of the world’s Indigenous peoples. Indigenous peoples’ access to health services. United nations; 2018. Available from: https://www.un.org/development/desa/indigenouspeoples/wp-content/uploads/sites/19/2018/03/The-State-of-The-Worlds-Indigenous-Peoples-WEB.pdf.
45. GBD 2016 Healthcare access and quality collaborators. Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391:2236–2271.
46. Ospina MB, Voaklander DC, Stickland MK. Prevalence of asthma and chronic obstructive pulmonary disease in Aboriginal and non-Aboriginal populations: a systematic review and meta-analysis of epidemiological studies. Can Respir J. 2012;19(6):355–360. doi:10.1155/2012/825107
47. Celli BR, Anderson JA, Cowans NJ. Pharmacotherapy and lung function decline in patients with chronic obstructive pulmonary disease. A systematic review. Am J Respir Crit Care Med. 2021;203(6):689–698. doi:10.1164/rccm.202005-1854OC
48. Koarai A, Sugiura H, Yamada M, et al. Treatment with LABA versus LAMA for stable COPD: a systematic review and meta-analysis. BMC Pulm Med. 2020;20:111. doi:10.1186/s12890-020-1152-8
49. Suissa S. Inhaled corticosteroids preventing pneumonia mortality: paradox or selection bias? Eur Respir J. 2019;53:1802112. doi:10.1183/13993003.02112-2018
50. Woodhead M. Inhaled corticosteroids cause pneumonia … or do they? Am J Respir Crit Care Med. 2007;176(2):111–112. doi:10.1164/rccm.200703-492ED
51. Lopez-Campos JL, Miravitlles M, de la Rosa Carrillo D, Cantón R, Soler-Cataluña JJ, Martinez-Garcia MA. Current challenges in chronic bronchial infection in patients with chronic obstructive pulmonary disease. J Clin Med. 2020;9(6):1639. doi:10.3390/jcm9061639
52. Sibila O, Soto-Gomez N, Restrepo MI. The risk and outcomes of pneumonia in patients on inhaled corticosteroids. Pulm Pharmacol Ther. 2015;32:130–136. doi:10.1016/j.pupt.2015.04.001
53. Tashkin DP, Miravitlles M, Celli BR, et al. Concomitant inhaled corticosteroid use and the risk of pneumonia in COPD: a matched-subgroup post hoc analysis of the UPLIFT® trial. Respir Res. 2018;19(1):196. doi:10.1186/s12931-018-0874-0
54. Heraganahally SS, Ghataura AS, Er XY, Heraganahally S, Biancardi E. Excessive dynamic airway collapse: a COPD/Asthma mimic or a treatment emergent consequence of inhaled corticosteroid therapy - case series and brief literature review. Clin Pulm Med. 2020;27:175–182. doi:10.1097/CPM.0000000000000382
55. Kapur N, Petsky HL, Bell S, Kolbe J, Chang AB. Inhaled corticosteroids for bronchiectasis. Cochrane Database Syst Rev. 2018;16(5):CD000996. doi:10.1002/14651858.CD000996.pub3
56. Henkle E, Curtis JR, Chen L, et al. Comparative risks of chronic inhaled corticosteroids and macrolides for bronchiectasis. Eur Respir J. 2019;54(1):1801896. doi:10.1183/13993003.01896-2018
57. Pasteur MC, Bilton D. British thoracic society guideline for non-CF bronchiectasis on behalf of the British thoracic society bronchiectasis (non-CF) guideline group. Thorax. 2010;65:i1ei58. doi:10.1136/thx.2010.136119
58. Jeong HJ, Lee H, Carriere KC, et al. Effects of long-term bronchodilators in bronchiectasis patients with airflow limitation based on bronchodilator response at baseline. Int J Chron Obstruct Pulmon Dis. 2016;11:2757–2764. doi:10.2147/COPD.S115581
59. Chalmers JD, Aliberti S, Blasi F. Management of bronchiectasis in adults. Eur Respir J. 2015;45:1446–1462. doi:10.1183/09031936.00119114
60. Whittaker HR, Jarvis D, Sheikh MR, Kiddle SJ, Quint JK. Inhaled corticosteroids and FEV1 decline in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2019;20:277. doi:10.1186/s12931-019-1249-x
61. Snoeck-Stroband JB, Lapperre TS, Sterk PJ, GLUCOLD Study Group. Prediction of long-term benefits of inhaled steroids by phenotypic markers in moderate-to-severe COPD: a randomized controlled trial. PLoS One. 2015;10(12):e0143793. doi:10.1371/journal.pone.0143793
62. Lange P, Celli B, Agustí A, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N Engl J Med. 2015;373:111–122. doi:10.1056/NEJMoa1411532
63. Murray R. Prescribing issues for Aboriginal people. Aust Prescr. 2003;26:55–57. doi:10.18773/austprescr.2003.080
64. Agusti A, Fabbri LM, Singh D, et al. Inhaled corticosteroids in COPD: friend or foe? Eur Respir J. 2018;52:1801219. doi:10.1183/13993003.01219-2018
65. Heraganahally SS, Rajaratnam B, Silva SAAS, et al. Obstructive sleep apnoea and cardiac disease among Aboriginal patients in the Northern Territory of Australia. Heart Lung Circ. 2021. doi:10.1016/j.hlc.2021.01.007
66. Heraganahally SS, Kruavit A, Oguoma VM, et al. Sleep apnoea among Australian Aboriginal and Non- Aboriginal patients in the Northern Territory of Australia– a comparative study. Sleep. 2020;43(3):zsz248. doi:10.1093/sleep/zsz248
67. Mehra S, Ghimire RH, Mingi JJ, et al. Gender differences in the clinical and polysomnographic characteristics among Australian Aboriginal patients with obstructive sleep apnea. Nat Sci Sleep. 2020;12:593–602. doi:10.2147/NSS.S258330
68. Heraganahally SS, Kerslake C, Issac S, et al. Outcome of public hospital-funded continuous positive airway therapy device for patients with obstructive sleep apnoea: an Australian perspective study. Sleep Vigilance. 2020;4:195–204. doi:10.1007/s41782-020-00114-4
69. Heraganahally SS, Zaw KK, Tip S, et al. Obstructive sleep apnoea and adherence to continuous positive airway therapy among Australian women. Int Med J. 2020. doi:10.1111/imj.15076
70. Garg H, Er XY, Howarth T, Heraganahally SS. Positional Sleep apnea among regional and remote Australian population and simulated positional treatment effects. Nat Sci Sleep. 2020;12:1123–1135. doi:10.2147/NSS.S286403
71. Benn E, Wirth H, Short T, Howarth T, Heraganahally SS. The Top End sleepiness scale (TESS): a new tool to assess subjective daytime sleepiness among Indigenous Australian adults. Nat Sci Sleep. 2021;13:315–328. doi:10.2147/NSS.S298409
72. Heraganahally SS, Howarth TP, Sorger L. Chest computed tomography findings among adult Indigenous Australians in the Northern Territory of Australia. J Med Imaging Radiat Oncol. 2021. doi:10.1111/1754-9485.13295
73. Koleade A, Farrell J, Mugford G, Gao Z. Prevalence and risk factors of ACO (Asthma-COPD Overlap) in Aboriginal people. J Environ Public Health. 2018;9. doi:10.1155/2018/4657420
74. Contolihttps M, Morandia L, Marcob FD, Caronec M. A perspective for chronic obstructive pulmonary disease (COPD) management: six key clinical questions to improve disease treatment. Expert Opin Pharmacother. 2021;22(4):427–437. doi:10.1080/14656566.2020.1828352
75. Vimala LR, Gibikote S, Christopher DJ, Irodi A, Rajan M, Ramasami P. Correlation of digital chest radiograph parameters with pulmonary function test and BODE index for diagnosis and prognostication in Indian COPD patients. J Lung Pulmonary Respir Res. 2018;5(1):584. doi:10.15406/jlprr.2018.05.00154
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.