Back to Journals » Open Access Emergency Medicine » Volume 12
The Effects of Ambulance Response Time on Survival Following Out-of-Hospital Cardiac Arrest
Authors Alumran A , Albinali Hissah , Saadah A, Althumairi A
Received 11 July 2020
Accepted for publication 27 October 2020
Published 1 December 2020 Volume 2020:12 Pages 421—426
DOI https://doi.org/10.2147/OAEM.S270837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Arwa Alumran,1 Hissah Albinali,2 Amjad Saadah,1 Arwa Althumairi1
1Health Information Management and Technology Department, College of Public Health, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2Emergency Medical Service, Royal Commission Hospital, Jubail Industrial City, Saudi Arabia
Correspondence: Arwa Alumran Address: Dammam, 34221, Saudi Arabia Tel +966 1 3333 1322
Email [email protected]
Background: Patients who suffer cardiac arrest outside medical facilities are at greater risk of death and adverse medical outcomes. Cardiopulmonary resuscitation affects the survival rates of such patients, which suggests that response time may be vital to patient outcomes.
Objective: The aim of this study was to investigate the role of response time, whether more or less than 8 minutes, on the survival of patients who have suffered out-of-hospital cardiac arrest.
Methods: Data were collected from emergency cases handled by a secondary hospital in Jubail, Saudi Arabia, between January 2017 and October 2019. There were 108 out-of-hospital cardiac arrest cases, 85 of which resulted in death.
Results: Bivariate analysis showed no significant association between response time and patient outcomes; however, the odds of having a negative outcome (death) if the response time is more than 8 minutes is double the odds of dying if the response time is less than 8 minutes.
Conclusion: Ambulance response time to out-of-hospital cardiac arrest does not significantly influence the patient survival rate in the current study hospital. Other variables may have a more significant effect.
Keywords: cardiac arrest, patient outcomes, response time
Introduction
The occurrence of cardiac arrests outside medical facilities is a major health concern. This medical condition is a primary cause of uneventful deaths, especially in developed nations. The annual reported cases of out-of-hospital cardiac arrest (OHCA) in the United States and Europe were about 420 000 and 275 000, respectively.1 Surviving a cardiac arrest and reducing the adverse outcomes associated with the episode are some of the core considerations in emergency response and hospital management of the condition 1.
Timely medical attention may be critical to improving the survival rates in cases of OHCA. Past studies revealed that the timely provision of cardiopulmonary resuscitation (CPR) can influence patient survival rates and other health-related outcomes.2–7,8 Daya 2 revealed that participating in the resuscitation outcomes that emphasize CPR quality, minimization of interruptions, and standardizes post-resuscitation care led to higher survival rates of OHCA. Dispatcher-initiated telephone CPR was independently associated with improved survival and functional outcomes after OHCA.7 One possible reason for this is the reduction in the time between the occurrence of the OHCA and the performance of CPR. Rajan, Wissenberg, Folke, Hansen, Gerds, Kragholm, Hansen, Karlsson, Lippert, Køber, Gislason, Torp-Pedersen 9 examined the correlation between early CPR and OHCA survival and revealed a stable positive correlation exists between early CPR and survival rate.
The time to definitive care and time to CPR are factors affected by emergency services response. Each of these factors is significantly associated with survival in any case of cardiac arrest.10 Ambulance response time is a factor that directly affects the timeliness of CPR and admission in a health care facility.9,10 However, empirical studies that focus on the relationship between ambulance response time and patient survival in OHCA cases are lacking.
This study aimed to determine the association between ambulance response time and the survival of patients who experience out-of-hospital cardiac arrest by analysing the relationship between patients’ demographic characteristics (gender and age) and outcomes. The hypothesis is that favourable patient outcomes (survival of OHCA) are significantly associated with lower ambulance response time (<8 min).
Methods
Study Design
This study used a quantitative cross-sectional design to examine the effect of ambulance response time on patient outcomes (death from or survival of OHCA).
Study Setting
The study took place in a secondary hospital in the industrial city of Jubail in eastern Saudi Arabia. The hospital has 6 ambulances and responds to an average of 20 medical emergencies daily.
Participants
Only patients with out-of-hospital cardiac arrest were included in the study. Participants were adult and paediatric patients.
Variables
The outcome variables in the study include patients’ outcomes, whether survival of OHCA or death. Other variables assessed in this study are patients’ demographic information, including sex and age, and the emergency medical service response time measured in minutes. A cut-off of less than 8-minute response time was used as an indicator of good response time, as recommended internationally by Eisenberg, Bergner, Hallstrom 10.
Data Sources and Measurement
Participants’ information was collected from the hospital’s electronic database, which was convenient for the aim of the study. This database includes patient outcomes, demographic information, and ambulance response times, given that the ambulance service is provided by the same hospital. The number of cases that was sampled depended on the number of cardiac arrest cases that the facility handled between January 1, 2017, and October 2019.
Ethical approval was obtained from the Institutional Review Board at Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB-PGS-2019-03-331). As the information used in this study does not include any identifying information from the patients; thus, a written consent from the patients was not required. Any patient-related information in the study (ie, age, and gender) is confidential, and no identifiable information is obtained. The authors would like to ensure their compliance with the Declaration of Helsinki.
Study Size
Since the study targeted patients with out-of-hospital cardiac arrest, all out-of-hospital cardiac arrest patients in the study period were included in the study.
Statistical Methods
Univariate analysis was conducted to show the descriptive summary of the results, including frequencies and percentages and means and standard deviations. Further, bivariate analysis was conducted to examine the associations between response time and survival rate and other influencing variables using the χ2 test. The χ2 test was selected because the outcome variable is grouped to either survival of OHCA or death, whereas the independent variables included response time (>8 min or <8 min), sex, and whether the patient was an adult or child. SPSS Version 25 was used to conduct the analyses.11 A P-value of less than 0.05 was considered significant.
Results
Participants
Because the inclusion criteria included participants with only an out-of-hospital cardiac arrest, 63 participants were included. These constitute all out-of-hospital cardiac arrest patients in the study period.
Descriptive Data
Table 1 presents a summary of the demographic and outcome variables. The majority were male subjects (66%, n = 71). The average age of the participants was 48 (SD = 23), whereas the youngest was 5 years old.
 |
Table 1 Patient Demographics |
Outcome Data
An overwhelming majority of the patients (79%, n = 85) succumbed to cardiac arrest or associated complications. Figure 1 shows a difference exists in patient outcome across two categories of ambulance response time. The majority of patients died regardless of ambulance response time. Only 21% (n = 23) of patients survived following out-of-hospital cardiac arrest.
 |
Figure 1 Response time and patient outcomes. |
The lowest response time was 2 minutes and the highest was 33 minutes. The mean response time for the entire sample was 8.50 minutes (SD = 5.1). We categorized response time as >8 minutes or <8 minutes, based on the international recommendation of the best response time.10 Furthermore, ambulances transported more patients to the hospital (64% of patients in the study) within 8 or fewer minutes, whereas the rest (36%) of the patients were transported within more than 8 minutes.
Main Findings
The odds of death if the response time was more than 8 minutes were 2.4 times higher compared to the response time of less than 8 minutes; that is, the odds of death, if the response time was more than 8 minutes, were more than double compared to the response time of less than 8 minutes. This association, however, is found to be not significant, as shown in Table 2 (χ2 = 2.616, Fisher exact test = 0.328, odds ratio [OR] = 2.4, 95% CI, 0.81–7.1).
 |
Table 2 Main Findings |
Further, bivariate analysis using χ2 test to assess the association between patients’ outcomes and their sex revealed no significant difference (χ2 = 1.103, P = 0.293, Fisher exact test = 0.328; Table 2). Patient’s age and its association with the outcome (ie, death or survival of OHCA) was also tested. Because the average age of patients who survived was 38, whereas the average age of patients who died was 51 (Figure 2), the 13-year mean difference was found statistically significant (t = −2.872, P = 0.006). In addition, the difference in the outcome of OHCA between adults and paediatric patients was calculated (χ2 = 1.094, P = 0.582, Fisher exact test = 0.288).
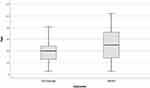 |
Figure 2 Patient’s age and outcome. |
Discussion
The study aimed to determine the association between ambulance response time and cardiac arrest patients’ survival. The study also explored the influence of patients’ sex and age on survival outcomes. The results revealed no significant association exists between response times and patient outcomes (death or survival, sex, or adult or paediatric status). The mean age of patients who died was slightly higher, which was significantly different from the mean age of the patients who survived the OHCA.
The finding from this study ascertained no significant association exists between response time and patient outcome, which differs from findings in previous studies. Previous studies have shown that the response time or period before the CPR affects resuscitation outcomes.10,12 There are several potential explanations for the difference; previous studies may have defined patient outcomes differently, whereas the current study defined patient outcomes as either death or discharge from the facility. In addition, a possibility exists that the quality of the services rendered by the emergency team varies. For instance, an emergency team that takes a long time to respond could also take a long time to prepare. Thus, the difference in the observed findings may be a manifestation of the quality of the services rendered by the emergency teams rather than the response time 13.
Although results from the current study revealed no significant difference in survival rate exists between males and females; however, the number of deaths was almost 10% higher among males compared to females in the study. The differences can possibly be explained by the differences in gender representation in the sample. The sample had a considerably higher proportion of male participants.
The current study revealed that the mean difference in the age of patients who died and those who survived was significant; older patients appeared to succumb to cardiac arrest more often than younger ones. This observation is in line with general findings on the risks of cardiac arrest increasing with age.14 Moreover, the damage caused by cardiac arrest may increase with the age of patients 15.
The main strength of the study is that it considers not only the relationship between ambulance response time and patient outcomes but also the role of patient factors such as their age and sex. Thus, the study can be used as a basis for the identification of potential confounding factors in the relationship between response time and patients’ cardiac arrest outcomes in future studies.
The foremost limitation was that the data collection relied on the availability, completeness, and accuracy of the existing medical records. This limitation is commonly associated with the use of secondary data collection. The availability of data led to a relatively small sample size. Another weakness is that data came from only one facility. Data from several facilities would lead to generalizable findings. Moreover, several potential confounding variables were not assessed in this study because of the limited time and resources. These variables include bystander CPR, aetiology (cardiac or not), and initial rhythm (shockable or not).
Conclusion
The purpose of this study was to investigate the effects of ambulance response times on the survival of patients. The study was motivated by previous studies that tied the period before CPR to patient outcomes. The study employed a quantitative cross-sectional design that involved the use of medical records sourced from a secondary hospital in Jubail. The data analysis involved the use of the bivariate analysis for the association and independent samples.
Overall, the study showed that ambulance response times might not be highly influential on patient survival, as was initially hypothesized. Other emergency-response-related factors such as the conduct of the response teams, the facilities that they have, and the time it takes to reach a specialized facility might have influenced the findings.
There is a need for further investigation into other emergency-response-related factors that may be in play. The findings from this study suggest that focusing on response time may not be sufficient in improving cardiac arrest patient outcomes. Thus, emergency response teams should look beyond response times in their efforts to improve patient outcomes in cases involving cardiac arrest.
Acknowledgment
The authors would like to thank www.papercheck.com for their proofreading services.
Disclosure
The authors declare that they have no conflicts of interest relevant to this work.
References
1. Gräsner J-T, Lefering R, Koster RW, et al. EuReCa ONE—27 Nations, one Europe, one Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105(1):1195–1880.
2. Daya MR, Schmicker RH, Zive DM, et al. Resuscitation outcomes consortium investigators. out-of-hospital cardiac arrest survival improving over time: results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91(1):108–115. doi:10.1016/j.resuscitation.2015.02.003
3. Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest. Circulation. 2015;132(13):1286–1300. doi:10.1161/CIR.0000000000000144
4. Schewe JC, Kappler J, Heister U, et al. Outcome of out-of-hospital cardiac arrest over a period of 15 years in comparison to the RACA score in a physician staffed urban emergency medical service in Germany. Resuscitation. 2015;96(1):232–238. doi:10.1016/j.resuscitation.2015.07.025
5. Kupari P, Skrifvars M, Kuisma M. External validation of the ROSC after cardiac arrest (RACA) score in a physician staffed emergency medical service system. Scand J Trauma Resusc Emerg Med. 2017;25(1):34. doi:10.1186/s13049-017-0380-2
6. Truhlář A, Deakin CD, Soar J, et al. European resuscitation council guidelines for resuscitation 2015: section 4. cardiac arrest in special circumstances. Resuscitation. 2015;95:148–201. doi:10.1016/j.resuscitation.2015.07.017
7. Wu Z, Panczyk M, Spaite DW, et al. Telephone cardiopulmonary resuscitation is independently associated with improved survival and improved functional outcome after out-of-hospital cardiac arrest. Resuscitation. 2017;122(1):135–140. doi:10.1016/j.resuscitation.2017.07.016
8. Hasselqvist-Ax I, Riva G, Herlitz J, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307–2315. doi:10.1056/NEJMoa1405796
9. Rajan S, Wissenberg M, Folke F, et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation. 2016;134(25):2095–2104. doi:10.1161/CIRCULATIONAHA.116.024400
10. Eisenberg MS, Bergner L, Hallstrom A. Cardiac resuscitation in the community. Importance of rapid provision and implications for program planning. JAMA. 1979;241:1905–1907. doi:10.1001/jama.1979.03290440027022
11. IBM Corp. IBM SPSS Statistics for Macintosh [Computer Program]. Version 25. Armonk, NY: IBM Corp; 2017.
12. Neukamm J, Gräsner J-T, Schewe J-C, et al. The impact of response time reliability on CPR incidence and resuscitation success: a benchmark study from the German Resuscitation Registry. Neukamm et al Critical Care. 2011;15:282. doi:10.1186/cc10566
13. Hansen CM, Kragholm K, Granger CB, et al. The role of bystanders, first responders, and emergency medical service providers in timely defibrillation and related outcomes after out-of-hospital cardiac arrest: results from a statewide registry. Resuscitation. 2015;96:303–309. doi:10.1016/j.resuscitation.2015.09.002
14. Adabag AS, Luepker RV, Roger VL, Gersh BJ. Sudden cardiac death: epidemiology and risk factors. Nat Rev Cardiol. 2010;7(4):216–225. doi:10.1038/nrcardio.2010.3
15. Tweed WA, Thomaseen A, Wernberg M. Prognosis after cardiac arrest based on age and duration of coma. CMA Journal/May. 1982;126(1):1059.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
