Back to Journals » Clinical Interventions in Aging » Volume 12
The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis
Authors Otero M, Esain I, González-Suarez ÁM, Gil SM
Received 10 November 2016
Accepted for publication 13 January 2017
Published 14 March 2017 Volume 2017:12 Pages 505—513
DOI https://doi.org/10.2147/CIA.S127233
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Montserrat Otero,1 Izaro Esain,2 Ángel M González-Suarez,1 Susana M Gil2
1Department of Physical Education and Sport, Faculty of Education and Sport Sciences, University of the Basque Country (UPV/EHU), Vitoria-Gasteiz, 2Department of Physiology, Faculty of Medicine and Nursing, University of the Basque Country (UPV/EHU), Leioa, Bizkaia, Spain
Objective: To determine the effects of a simple exercise program on the balance and strength of postmenopausal women with osteoporosis.
Methods: This program was based on low intensity strength and balance exercises, and was carried out with simple, readily available equipment. Sixty five women were randomly assigned to either the experimental group (EG; n=33, age: 57.4±4.8 years) or the control group (CG; n=32, age: 58.8±4.5 years). Participants in the EG underwent balance and strength training for 60 min, three times/week for 6 months. Each session consisted of warm-up exercises (10 min), balance training (20 min), strength training (20 min), and cooldown (10 min). Participants from the CG were asked not to modify their usual habits during the course of the study. Static balance was evaluated using the blind monopodal stance static balance test. In contrast, dynamic balance was assessed using the “8-foot up and go” test, whereas the strength of the upper and lower limbs was measured using the “arm curl” and “30 s chair stand” tests, respectively. All these variables were assessed at baseline and upon program completion.
Results: The EG showed significant improvements (P<0.001) in static balance (21%), dynamic balance (36%), and in the strength of the upper (80%) and lower (47%) limbs in comparison to the CG after the sixth month. Participants in the CG showed significantly lower values (P<0.001) in the four tests. In addition, a significant inverse relationship between static balance and the strength of the upper (r=-0.390; P=0.001) and lower (r=-0.317; P=0.01) limbs was found.
Conclusion: The present study demonstrates that a physical exercise program based on balance and strength exercises, carried out with simple and readily available equipment, is capable of significantly improving the strength and balance of women with osteoporosis.
Keywords: fracture risk, osteoporotic fracture, training, postmenopausal women, aging, fracture prevention
Introduction
Osteoporosis is a disease which affects 22 million women in the European Union between the ages of 50 and 84 years. It is estimated that this figure will reach 33.9 million women by the year 2025.1 One in three women worldwide is at risk of suffering an osteoporotic fracture, which is precisely the most serious consequence of this disease.2 The principal cause of these fractures is falls, which in elderly people are related to, among other factors, a deteriorated sense of balance3 and low levels of muscular strength.4 Such is their importance that, in elderly people, having high levels of strength in the lower limbs and having good balance are important requisites for being independent and being able to carry out daily activities.5–7 For this reason, increasing the levels of strength and balance achieved by practicing physical exercise,3,8,9 constitutes one of the optimal preventative strategies and plays a key role in the prevention of falls,3,10,11 as demonstrated by a variety of studies.12–14 Thus, one of the priorities for both the treatment and prevention of postmenopausal osteoporosis is the improvement of strength and balance by means of practice of physical exercise, because of the implication of both these physical qualities in falls.15–17 However, some studies of the effects of physical exercise programs did not find significant improvements in the prevention of falls.18–20
Despite the known importance of physical exercise for these women, there is still no consensus regarding the characteristics of the most optimal physical exercise program to reduce risk factors for falls in women with postmenopausal osteoporosis. This is to a large extent because of the large variety of combinations employed in the duration, intensity, type of exercise, and rhythm of progression of the different programs which are currently employed.
In this regard, intense training of muscular strength has been shown to be effective in improving both the strength and balance of this population.21–23 However, this type of training usually requires the use of special gymnasium machines which increase the cost of these programs, thereby impeding access to such programs by many women. Moreover, such programs cannot be carried out at home. On the other hand, it has been reported that low intensity training can produce similar improvements in the strength of the lower limbs to those achieved by high intensity training in postmenopausal women.24 In this regard, the results of another study suggest that high intensity and low intensity training regimes effectively increase muscular strength in healthy older women.25 Moreover, in frail older people, it has been reported that a low intensity strength training program can increase knee-extensor strength after 10 weeks.26
Nevertheless, there is a scarcity of research which demonstrates significant improvements in strength and balance by means of low intensity physical exercise programs in women with postmenopausal osteoporosis. For this reason, the objective of the present study was to determine the effects of a low intensity program, carried out with simple, readily available materials, on balance and strength in postmenopausal women with osteoporosis.
Methods
Study design
This project was carried out in collaboration with the Landako Health Center in the Basque Country (Northern Spain), where a list of telephone numbers of 75 women was provided who complied with the inclusion criteria of this study and who had expressed interest in knowing more about the study. Each of these women was contacted over phone to inform them about the conditions and characteristics of the study and to invite them to participate. They were contacted over phone for the second time in order to confirm their participation. A total of 68 women agreed to participate in the study. After applying inclusion and exclusion criteria, the 68 women were randomly assigned to one of the two study groups, that is, the experimental group (EG) or control group (GC). The flowchart used for the selection of participants is illustrated in Figure 1.
  | Figure 1 Flowchart illustrating the study design. |
The 68 people who agreed to participate in this study provided written informed consent. This study was approved by the Ethics Committee of the University of the Basque Country (UPV/EHU), Spain.
Participants
The final sample consisted of 65 women (three dropped out during the course of the study) between the ages of 50 and 72 years (58.1±4.6 years old) who had been diagnosed with osteoporosis and classified in accordance with World Health Organization criteria, with bone mineral density <2.5 standard deviations in comparison with young adults.27 Inclusion criteria included the following: diagnosis with postmenopausal osteoporosis, not presenting any medical contraindication for the practice of physical exercise at the moment of inclusion in the study, and not being enrolled, nor having participated in any physical exercise program for at least the previous 2 years. Exclusion criteria were menopause28 of <5 years, absence of myocardial infarction in the last year, or incapacity to do exercise.
Two groups were randomly established: EG (n=33, age =57.4±4.8 years) wherein the members participated in a physical exercise program for 24 weeks and CG (n=32, age =58.8±4.5 years) whose members were asked not to modify their daily habits during the course of the study. The participants were assigned to the EG or CG randomly using a list of alphabetically ordered names. This was done by using a six-element permutation table, taken 6 by 6. As a function of this table, participants were assigned to the EG or CG depending on whether the number assigned to them was an odd or and even number, respectively.
CG participants were informed that they would carry out a series of tests twice, with a time interval of 24 weeks between tests. During this interval, all CG participants were telephoned three times to remind them not to modify their daily habits until they had completed the second test. Upon completion of this last test, the CG participants received information about the effects of physical exercise on osteoporosis and the characteristics of the physical exercise most appropriate for them.
Three people dropped out during the course of the study: one in EG due to personal problems and two in the CG; one due to health problems (not related to the exercise program) and the other also for personal reasons. The average attendance rate at each session was 85%.
Exercise program
The physical exercise program was carried out in a room used as a prepartum and postpartum gymnasium in the same health center used routinely by the study participants. The program was directed and supervised by a technician who had a degree in Sport and Physical Exercise Sciences. The exercise schedule consisted of three sessions per week, each for 60 min and lasted for 6 months. The materials employed were individual mats, seats, balls, and ropes. Weights that were used for strength training were chosen so that anyone could use them in their own home without having to use sophisticated expensive material. These included plastic bottles of different sizes which were filled with water, sand, marbles, and stones, thus obtaining domestic dumbbells with different masses (between 0.370 and 1.350 kg). The structure of the exercise sessions was always the same and was as follows:
Basic warm-up and stretching exercises (duration: 10 min): joint mobility exercises, stretching, and walking.
Static balance exercises (duration: 10 min): exercises varying visual support, gait support, support of upper limbs, participation of lower limbs (arms alongside the body without movement, arms asymmetrically positioned with and without movement, arms symmetrically disposed with and without movement), and exercises involving the vestibular system.
Dynamic balance exercises (duration: 10 min): exercises involving changes in visual support, the distance and direction of displacement, gait support, pavement, participation of the upper limbs, exercises varying objects which had to be manipulated while walking, and exercises involving the vestibular system.
Muscle strengthening exercises (duration: 20 min): involves varying the musculature to be exercised, its load and position.
Cooldown (10 min): stretching and relaxation.
Three phases29 were distinguished in the planning of the training of strength and balance (Table 1): phase 1, adaptation and learning of the execution technique of all the exercises involved in the program (4 weeks); phase 2 (14 weeks), centered on the improvement of muscular strength and balance; and phase 3 (6 weeks), aimed at maintaining improvements in muscular strength and balance.
Table 1 illustrates the course of the exercises which were performed. The different variables which defined the intensity of each exercise were combined and adjusted specifically as a function of the rhythm of progression of the patients. In this way, combination of the different variables (number of exercises, number of repetitions, number of series, exercise duration, rest time, velocity, and load) defined the intensity and progression of the strength and balance training. Table 1 illustrates that the velocity of execution of the balance exercises was distinct as a function of the training phase. Thus, three terms were used: slow velocity (slow walking), moderate velocity (light paced walking), and rapid velocity (walking as quickly as possible without running). The velocity of execution of the strength exercises was constant during movements (ie, during the concentric and eccentric phases) to facilitate concentration on the correct execution of the exercise. However, the velocity of execution of movements varied also as a function of the training phase. Thus, the following terms were defined: slow velocity (concentric phase, 2 s; eccentric phase, 4 s), moderate velocity (concentric phase, 1–2 s; eccentric phase, 1–2 s), and rapid velocity (concentric phase, 1 s; eccentric phase, 1 s, providing no pain was perceived).30,31
In order to achieve higher adherence to the physical exercise program, a series of strategies was carried out during the sessions including: giving plenty of positive feedback, sharing the importance of feeling secure when carrying out each of the exercises during all sessions; conversations with all participants in each of the sessions; phone calls when a person did not attend a session; and the use of music. Finally, to stimulate group cohesion, all participants were invited to an aperitif with the trainer after each session.
Study measures
Measurements were carried out twice; once before beginning the program and again after 24 weeks. All measurements were performed in the same center in which the physical exercise program was carried out. Participants were asked to use the same clothing and shoes to carry out the test before and after the intervention. The same measurement protocol was always used.32,33 First, the questionnaires were filled out (15 min), then the anthropometric measurements were carried out (5 min). Warm-up (10 min) was performed, followed by the physical tests (20–30 min). Further details of these measurements are described below.
Questionnaires
A physical activity aptitude questionnaire was used as a security measure, prior to the intervention.34 The purpose of using this questionnaire was to identify participants with any disease syndrome or risk factor which would require a more complete medical check before beginning the exercise program.
Personal data questionnaire
This questionnaire was designed ad hoc for the present study with the objective of obtaining additional information about variables such as age, number of years after menopause, and number of years with hormonal treatment.
Anthropometric measurements
Body mass and height were measured in order to calculate the corresponding body mass index (BMI). Each participant had their height (to the nearest 0.1 cm) and body mass (nearest 0.01 kg) measured using Seca instrumentation (model 869; Hamburg, Germany).
Static balance
The blind monopodal stance static balance test was used from the AFISAL-INEFC battery of tests.32 This test involved maintaining balance on one foot with eyes closed. The number of attempts (not falls) which each participant required in order to maintain balance in this position for 1 min was recorded.
Dynamic balance
The “8-foot up and go” test,33 which consists in getting up from a chair, walking as quickly as possible to a cone situated 2.4 m from the chair, going around it, and returning to sitting on the same chair, was used. The time required to complete this test was recorded.
Upper limb muscle strength
The “arm curl” test,33 which consists in carrying out the maximum number of flexions and extensions of the arm within 30 s, holding with one hand a dumbbell with a mass of 2.3 kg while being seated, was carried out. The total number of flexions of the arm was recorded.
Lower limb muscle strength
The “30 s chair stand ” test was used.33 This involved getting up from a chair and sitting down again the maximum number of times possible during 30 s, maintaining arms crossed at the level of the chest with wrists resting against the chest. The total number of stand-ups was counted.
Statistical analysis
Statistical Package for the Social Sciences software (SPSS, IBM, version 21.0; Armonk, NY, USA) was used for data analysis. Normality of data was assessed using the Kolmogorov–Smirnov test. Mean values and standard deviations were calculated for each variable. In order to evaluate the measured changes (pre and post), 95% confidence intervals and the percentage of changes (%) were calculated. For group comparisons, Student’s t-test statistics were used for independent samples. Intragroup comparisons were carried out using the t-test for related samples. Differences between groups were analyzed by means of analysis of covariance, with post hoc Bonferroni, adjusted according to the values before the exercise program, as performed earlier by Solberg et al.35 Correlations were carried out between results obtained in the different tests after the program, by means of bivariate correlations of Pearson or Spearman. Validity of the tests has been established elsewhere.33 The intraclass correlation coefficients of the tests were between 0.948 and 0.997. For all cases, P<0.05 was considered to be the level of statistical significance.
Results
Table 2 illustrates features of the control (n=32) and experimental (n=33) groups. No statistically significant differences were found between these groups before the exercise program.
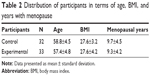  | Table 2 Distribution of participants in terms of age, BMI, and years with menopause |
Significant differences were not found with regard to the hormone treatment parameter, that is, in the CG, 65.5% of participants were undergoing hormone treatment, whereas in the EG, this figure was 63.6%.
Table 3 summarizes measurements and typical deviations of both groups for the results obtained before and after the exercise program.
As can be seen in this table, significant differences (P<0.001) were indeed observed between both groups for all tests carried out after program completion. In the upper and lower limb strength tests, significantly lower average values were found in the CG when compared to the corresponding values of EG. In the case of static and dynamic balance, the averages in EG were significantly lower than in CG.
Upon analyzing the percentage of variation in the four tests, statistically significant differences (P<0.001) were observed between CG and EG after the exercise program. EG showed a significant increase in the strength of the upper (+47.4%) and lower (+80.2%) limbs. In contrast, CG exhibited a significant decline in the strength of the upper (−15.9%) and lower (−10.5%) limbs.
The static balance of CG dropped 18.1%, that is, participants needed a higher number of attempts to pass the test. In contrast, EG improved by +36.7%, requiring fewer attempts to pass this test. Regarding dynamic balance, EG needed less time to carry out the test, improving 21.2% after the program, whereas CG needed more time (12.5%) to carry out the test.
Table 4 illustrates relationships between the different physical tests following completion of the program.
It can be seen here that there is a statistically significant association between the strength of the upper and lower limbs (r=0.890; P<0.001). In the case of dynamic balance and the two strength tests, an inverse relation was found, that is, those subjects who showed better performance in dynamic balance also exhibited better values for lower (r=−0.820; P<0.001) and upper (r=−0.849; P<0.001) limb strength.
The relation between static balance and the other analyzed parameters showed a significant inverse correlation with the strength of the lower (r=−0.390; P=0.001) and upper limbs (r=−0.371; P=0.01) and a direct relation with dynamic balance (r=0.339; P=0.006), indicating that a better balance capacity correlates with higher strength of the lower limbs.
Finally, analysis of a possible relationship between years of duration of menopause and BMI with the results obtained in the test revealed that neither of these criteria correlated with any of the results (data not shown).
Discussion
The results of the present study have shown that women with postmenopausal osteoporosis who participated in a 24-week program, based on exercises involving balance and low intensity strength, achieved a significant improvement in the strength of their upper and lower limbs, as well as in their static and dynamic balance, in comparison to women in the CG who had not altered their daily habits. The EG showed significant improvements (P<0.001) in static balance (21%), dynamic balance (36%), and in the strength of the upper (80%) and lower (47%) limbs in comparison to the CG after the sixth month. Participants in the CG showed significantly lower values (P<0.001) in the four tests. Additionally, a significant inverse relationship was found between static balance and the strength of the upper (r=−0.39; P=0.001) and lower (r=−0.317; P=0.01) limbs. It is noteworthy that the exercises carried out are easy to reproduce in any health center, sports center, or even at home, given the simple nature of the material resources employed.
In contrast, few studies have been carried out with low intensity exercises using domestic materials, which anyone could have available to them in their houses.24–26
In order to improve muscular strength of this population, an exercise program with a minimum duration of 8 weeks appears to be necessary,36 but the type of exercise and its intensity seem to be crucial. A study by Carter et al18 was based, like the present study, on low intensity strength exercises and they reported that the EG significantly improved the strength of their lower limbs with respect to the CG. However, the improvement (7.8%) was not statistically significant when results from the EG were compared before and after the intervention. In contrast, in the present study, this improvement (80%) was statistically significant (P<0.001). This discrepancy may be due to the fact that this study lasted 4 weeks longer, or to the different combinations of exercises employed in the present study. Moreover, the test which they used (dynamometry) was different to that used in this study (30 s chair stand). A study by Chyu et al37 was similar in duration to ours, but they did not find significant improvements in the strength of the lower limbs. This may be due to the fact that Chyu’s subjects practiced Taichi. However, it is noteworthy that, in a program involving pilates, Küçükçakir et al38 did report a significant improvement in the strength of the lower limbs. Despite having been a low intensity program, the strength of the lower limbs did improve, maybe due to the more extensive duration of the program, in that case, for 48 weeks. Küçükçakir et al38 reported findings similar to this study in that they reported significantly similar improvements (P<0.001) in the strength of the lower limbs, despite the fact that this study lasted 24 weeks less. They used the same test to evaluate strength. Their participants went from performing 25.8±5.6 repetitions to 33.2±4.1 upon completing the program, whereas in the present study participants went from 13.09±1.75 repetitions to 19.27±3.07. It thus seems that for low intensity training of muscular strength, the duration of the program should be longer in order to produce improvements. Nevertheless, when the intensity of the physical exercise is high, significant improvements have been observed for periods as short as 24 weeks,24 or for even 18 weeks.22 Thus, in a study carried out by Bemben et al,24 the group which strength trained at high intensity (80% 1 repetition maximum) presented a 25% significant improvement (P<0.05) in the strength of the upper limbs and a 30% improvement in the lower limbs. The improvement was smaller than in this study, but this could be expected since they used a test of maximal strength which was not employed in this study. Teixeira et al22 reported a significant improvement (P<0.0001) in the strength of the lower limbs after only 18 weeks of intervention in which they strength trained at a high intensity (50% up to 80% of 1 repetition maximum). However, it should be remembered that for menopausal women, low intensity strength training of sufficient volume can produce similar improvements to one of higher intensity,24 probably due to the type of exercise, to the combinations of the same, and to the rhythm of progression of the exercises.
It is well known that balance training is an indispensable element to reduce the risk of falls;10 however, this should be accompanied by strength training, since strength training of the lower limbs is known to produce improvements in balance.39 Several studies have reported significant improvements in static36 and dynamic balance,22 in women with postmenopausal osteoporosis following a physical exercise program based on strength and balance training for shorter periods of time than that of the present study, that is, 8 and 18 weeks, respectively. In Teixeira’s study22 in which strength was trained at high intensity (50% up to 80% of 1 repetition maximum), static balance improved significantly (P<0.0001); however, a comparison with the present results would be complicated since in this case the test employed was that of the Berg balance scale, whereas here the blind monopodal balance test was used. However, the same test was used for measurement of dynamic balance and in both studies, significant improvements (P<0.0001) were found. Surprisingly, despite the fact that the present study was 6 weeks shorter in duration, better results were achieved. Thus, in this study, participants went from needing 5.9±0.6 s to performing the test to requiring 4.6±0.6 s (ie, 22% less time), whereas in the study by Teixeira et al22 subject times evolved from 10.7±2.2 s to 6.9±1.1 s to complete the test. In this case, the intensity of strength training seems to have been more relevant than the duration of the intervention.
This apparent discrepancy may be due to the fact that, in both cases, the intensity of strength training was higher than that used in this study. Roghani et al’s40 program also reported improvement (104.7%) in static balance (measured using the near tandem stand test) in postmenopausal women following a 6-week program. To increase the intensity of strength training, they used weighted vests (4%–8% of body weight) which are not readily available to everyone. For this reason, programs involving low intensity physical exercise are of particular interest since they require fewer material resources. In this regard, Carter et al18 reported a significant improvement in dynamic balance in a shorter program which lasted 5 months. It should be emphasized that the present study did not require the use of technical or expensive material, such as dumbbells or elastic bands, but rather used filled plastic bottles that maybe readily available to everyone.
The importance of the combination of strength and balance training is based on the correlation which has been observed between these variables.5,41,42 Participants in the present study also showed a significant inverse relation between the strength of the lower limbs and static balance, indicating that higher levels of balance are associated with stronger lower limbs. Similarly, Vanderhoek et al43 concluded that the improvement in balance observed in their subjects was due to improvements achieved in levels of muscular strength. In the same way, in the present study, dynamic balance was also found to be inversely related to the strength of the lower limbs.
Recently, encouraging results have been reported in studies using vibration machines. Thus, Gusi et al44 as well as Iwamoto et al45 claimed that such machines achieved a significant improvement in balance; however, it should be recognized once again that such machines are not readily available to everyone. It thus seems that exercise programs based on balance and strength training at high intensities using more sophisticated materials can indeed achieve improvements in both strength and balance and in shorter times.21,43 However, the present study has demonstrated that via a physical exercise program which does not require any sophisticated material and which is available to practically anyone, significant improvements can also be achieved in both strength and balance in postmenopausal osteoporotic women who can perform these exercises even in the comfort of their own homes. For a low intensity physical exercise program to achieve statistically significant improvements in both the muscular strength and balance of these women, the characteristics of the program (duration, intensity, type of exercises, rest periods, exercise combinations, progression rhythm, etc) appear to be vitally important.
It is worthwhile noting that in the present study, as well as in others, a progressive reduction in strength,18,21,24,46 and balance,14,40 of women in the CG was observed, that is, in women who were not participating in a specific physical exercise program. Despite the fact that physical exercise has been widely recommended as an effective method for the conservation of musculoskeletal health among premenopausal and postmenopausal women,47,48 the authors insist on the importance of such physical exercise programs, since adequate training not only improves the strength and balance of women with osteoporosis, but also lack of physical exercise is clearly associated with a deterioration of these physical qualities, leading to a higher risk of falling and consequently of fractures. Future studies will be required to define with greater precision the characteristics of physical exercises which are optimal for reducing risk factors for falls.
Limitations
It would have been of interest to have employed quality of life questionnaires in order to evaluate the effects of this program of physical exercise on the different quality of life parameters of the women in this study. However, due to time and management reasons, this was not possible. In addition, in recent years interest in vitamin D and its relation to balance and falls has noticeably increased. It would have undoubtedly been of interest to have measured this variable in the present study; future studies should include measurement of vitamin D in the study design.
Conclusion
On the basis of the current findings, it is concluded that a program of physical exercise based on low intensity balance and strength exercises, carried out three days a week, during 1 h sessions for a period of 6 months and using simple, readily available, inexpensive materials, produces significant improvements in the muscular strength of the upper and lower limbs, as well as in the static and dynamic balance of women with postmenopausal osteoporosis, in comparison to those in the CG who did not participate in any exercise program.
Acknowledgments
The authors would like to express their thanks to Dr JL Balenciaga for his help and collaboration in this study, as well as to all the participants for their commitment to facilitating the research. Acknowledgements are also due to the Basque Government for having provided a predoctoral grant to Izaro Esain, enabling her participation in the present study.
Disclosure
The authors report no conflicts of interest in this work.
References
Hernlund E, Svedbom A, Yvergard M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch of Osteoporos. 2013;8:1–115. | ||
International Osteoporosis Foundation. IOF website. Available from: http://www.iofbonehealth.org. Accessed November 23, 2015. | ||
Raeissadat SA, Sedighipour L, Pournajaf S, et al. Effect of posture training with Weighted Kypho-Orthosis (WKO) on improving balance in women with osteoporosis. J Aging Res. 2014. | ||
Ganança FF, Gazzola JM, Ganança CF, et al. Elderly falls associated with benign paroxysmal positional vertigo. Braz J Otorhinolaryngol. 2010;76:113–120. | ||
Lee DK, Kang MH, Lee TS, et al. Relationships among the Y balance test, Berg balance scale, and lower limb strength in middle-aged and older females. Braz J Phys Ther. 2015;19:227–234. | ||
Ponce-Bravo H, Ponce C, Feriche B, et al. Influence of two different exercise programs on physical fitness and cognitive performance in active older adults: functional resistance-band exercise vs. recreational oriented exercises. J Sports Sci Med. 2015;14:716–722. | ||
Sanders ME, Takeshima N, Rogers ME, et al. Impact of the S.W.E.A.T.™ water-exercise method on activities of daily living for older women. J Sports Sci Med. 2013;12:707–715. | ||
Trudelle-Jackson EJ, Jackson AW, Morrow JR. Muscle strength and postural stability in healthy, older women: implications for fall prevention. J Phys Act Health. 2006;3:292–303. | ||
Chen MS, Jiang BC. Resistance training exercise program for intervention to enhance gait function in elderly chronically ill patients: multivariate multiscale entropy for center of pressure signal analysis. Comput Math Methods Med. 2014;2014:471356. | ||
Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011;6(7):CD000333. | ||
Hsu WH, Chen CL, Kuo LT, et al. The relationship between health-related fitness and quality of life in postmenopausal women from Southern Taiwan. Clin Interv Aging. 2014;9:1573–1579. | ||
Barnett A, Smith B, Lord SR, et al. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32:407–414. | ||
Smulders E, Weerdesteyn V, Groen B, et al. Efficacy of a short multidisciplinary falls prevention program for elderly persons with osteoporosis and a fall history: a randomized controlled trial. Arch Phys Med Rehabil. 2010;91:1705–1711. | ||
Madureira MM, Takayama L, Gallinaro AL, et al. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: a randomized controlled trial. Osteoporos Int. 2007;18:419–425. | ||
Cadore EL, Rodríguez-Mañas L, Sinclair A, et al. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: a systematic review. Rejuvenation Res. 2013;16:105–114. | ||
Irez GB, Ozdemir RA, Evin R, et al. Integrating Pilates exercise into an exercise program for 65+ year-old women to reduce falls. J Sports Sci Med. 2011;10:105–111. | ||
Martínez-López EJ, Hita-Contreras F, Jiménez–Lara PM, et al. The association of flexibility, balance, and lumbar strength with balance ability: risk of falls in older adults. J Sports Sci Med. 2014;13:439–357. | ||
Carter ND, Khan KM, McKay HA, et al. Community-based exercise program reduces risk factors for falls in 65- to 75-years-old women with osteoporosis: randomized controlled trial. Can Med Assoc J. 2002;167:997–1004. | ||
Kronhed ACG, Hallberg I, Ödkvist L, et al. Effect of training on health-related quality of life, pain and falls in osteoporotic women. Adv Physiother. 2009;11:154–165. | ||
Papaioannou A, Adachi JD, Winegard K, et al. Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int. 2003;14:677–682. | ||
Nelson ME, Fiatarone MA, Morganti CM, et al. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA. 1994;272:1909–1914. | ||
Teixeira LEPP, Silva KNG, Imoto AM, et al. Progressive load training for the quadriceps muscle associated with proprioception exercises for the prevention of falls in postmenopausal women with osteoporosis: a randomized controlled trial. Osteoporos Int. 2010;21:589–596. | ||
Tolomio S, Ermolao A, Travain G, et al. Short-term adapted physical activity program improves bone quality in osteopenic/osteoporotic postmenopausal women. J Phys Act Health. 2008;5:844–853. | ||
Bemben DA, Fetters NL, Bemben MG, et al. Musculoskeletal responses to high-and low-intensity resistance training in early postmenopausal women. Med Sci Sports Exerc. 2000;32(11):1949–1957. | ||
Pruitt LA, Taaffe DR, Marcus R. Effects of a one-year high-intensity versus low-intensity resistance training program on bone mineral density in older women. J Bone Miner Res. 1995;10(11):1788–1795. | ||
Westhoff MH, Stemmerik L, Boshuizen HC. Effects of a low-intensity strength-training program on knee-extensor strength and functional ability of frail older people. J Aging Phys Act. 2000;8(4):325–342. | ||
World Health Organization. Available from: http://www.who.int/. Accessed October 5, 2015. | ||
WHO Scientific Group on Research on the Menopause in the 1990’s. WHO Technical Report Series 866; 1994. Available from: http://apps.who.int/iris/bitstream/10665/39142/1/WHO_TRS_843_eng.pdf. Accesed October 5, 2015. | ||
Ramalho F, Carnide F, Santos-Rocha R, et al. Community-based exercise intervention for gait and functional fitness improvement in an older population: Study protocol. J Aging Phys Act. 2017;15(1):84–93. | ||
Keeler LK, Finkelstein LH, Miller W, et al. Early-phase adaptations of traditional-speed vs. superslow resistance training on strength and aerobic capacity in sedentary individuals. J Strength Cond Res. 2001;15(3):309–314. | ||
Morrissey MC, Harman EA, Frykman PN, et al. Early phase differential effects of slow and fast barbell squat training. Am J Sports Med. 1998;26(2):221–230. | ||
Rodriguez FA, Gusi N, Valenzuela A, et al. Valoración de la condición física saludable en adultos (I): antecedentes y protocolos de la batería AFISAL-INEFC. Apunts: Educación Física y Deportes. 1998;52:54–75. | ||
Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. 1999;7:129–161. | ||
Rodríguez A. Estudio epidemiológico y socio-sanitario de las fracturas de cadera en el Área I. SECOT. 1995;39:255–259. | ||
Solberg PA, Kvamme NH, Raastad T, et al. Effects of different types of exercise on muscle mass, strength, function and well-being in elderly. Eur J Sport Sci. 2013;13:112–125. | ||
Nogueira T, Renovato FJ, Rúbia S, et al. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clin Rehabil. 2012;26:1021–1031. | ||
Chyu MC, James CR, Sawyer SF, et al. Effects of tai chi exercise on posturography, gait, physical function and quality of life in posmenopausal women with osteopaenia: a randomized clinical study. Clin Rehabil. 2010;24:1080–1090. | ||
Küçükçakir N, Altan L, Korkmaz N. Effects of Pilates exercises on pain, functional status and quality of life in women with postmenopausal osteoporosis. J Body Mov Ther. 2013;17:204–211. | ||
Hsu WL, Chen CY, Tsauo JY, et al. Balance control in elderly people with osteoporosis. J Formos Med Assoc. 2014;113:334–339. | ||
Roghani T, Torkaman G, Movasseghe S, et al. Effects of short-term aerobic exercise with and without external loading on bone metabolism and balance in postmenopausal women with osteoporosis. Rheumatol Int. 2013;33:291–298. | ||
Cho KH, Bok SK, Kim YJ, et al. Effect of lower limb strength on falls and balance of the elderly. Ann Rehabil Med. 2012;36:386–393. | ||
Liu-Ambrose T, Khan KM, Eng JJ, et al. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc. 2004;52:657–665. | ||
Vanderhoek KJ, Coupland DC, Parkhouse WS. Effects of 32 weeks of resistance training on strength and balance in older osteopenic/osteoporotic women. Clin Exerc Physiology. 2000;2:77–83. | ||
Gusi N, Raimundo A, Leal A. Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC Musculoskelet Disord. 2006;7:92. | ||
Iwamoto J, Sato Y, Takeda T, et al. Whole body vibration exercise improves body balance and walking velocity in postmenopausal osteoporotic women treated with alendronate: Galileo and Alendronate Intervention Trail (GAIT). J Musculoskelet Neuronal Interact. 2012;12:136–143. | ||
Silva C, Costa B, Bittencourt A, et al. Effects of high and low volume of strength training on muscle strength, muscle volume and lipid profile in postmenopausal women. J Exerc Sci Fit. 2014;12:62–67. | ||
Akune T, Muraki S, Oka H, et al. Exercise habits during middle aged are associated with lower prevalence of sarcopenia: the ROAD study. Osteoporos Int. 2014;25:1081–1088. | ||
Kim SJ, Bemben M, Bemben DA. Effects of an 8-month yoga intervention on arterial compliance and muscle strength in premenopausal women. J Sports Sci Med. 2012;11:322–330. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



