Back to Journals » Journal of Pain Research » Volume 15
The Effect of Opioid-Free Anesthesia on the Quality of Recovery After Gynecological Laparoscopy: A Prospective Randomized Controlled Trial
Authors Choi H , Song JY, Oh EJ, Chae MS, Yu S, Moon YE
Received 16 May 2022
Accepted for publication 29 July 2022
Published 3 August 2022 Volume 2022:15 Pages 2197—2209
DOI https://doi.org/10.2147/JPR.S373412
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ellen M Soffin
Hoon Choi,1 Jae Yen Song,2 Eun Jee Oh,3 Min Suk Chae,1 Sanghyuck Yu,1 Young Eun Moon1
1Department of Anesthesiology and Pain Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea; 2Department of Obstetrics and Gynecology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea; 3Department of Laboratory Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
Correspondence: Young Eun Moon, Department of Anesthesiology and Pain Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222, Banpo-daero, Seocho-gu, Seoul, 06591, Republic of Korea, Tel +82-2-22586163, Fax +82-2-5371951, Email [email protected]
Purpose: Opioid-free anesthesia (OFA) is an emerging technique that eliminates intraoperative use of opioids and is associated with lower postoperative opioid consumption and reduced adverse postoperative events. The present study investigated the effect of OFA on the quality of recovery in patients undergoing gynecological laparoscopy.
Patients and Methods: Seventy-five adult patients undergoing elective gynecological laparoscopy were randomly assigned to the OFA group with dexmedetomidine and lidocaine or the remifentanil-based anesthesia (RA) group with remifentanil. Patients, surgeons, and medical staff members providing postoperative care and assessing outcomes were blinded to group allocation. The anesthesiologist performing general anesthesia could not be blinded due to the different drug administration protocols by groups. The primary outcome was the quality of recovery measured using the Quality of Recovery-40 (QoR-40) questionnaire. Secondary outcomes were postoperative pain score, intraoperative and postoperative adverse events, and stress hormones levels.
Results: The patients in both groups had comparable baseline characteristics. The QoR-40 score on postoperative day 1 was significantly higher in the OFA group than in the RA group (155.9 ± 21.2 in the RA group vs 166.9 ± 17.8 in the OFA group; mean difference: − 11.0, 95% confidence interval: − 20.0, − 2.0; p = 0.018). The visual analog scale score at 30 min after surgery was significantly lower in the OFA group than in the RA group (6.3 ± 2.3 in the RA group vs 4.1 ± 2.1 in the OFA group; p < 0.001). The incidences of nausea and shivering in the post-anesthetic care unit were also significantly lower in the OFA group (p = 0.014 and 0.025; respectively). Epinephrine levels were significantly lower in the OFA group (p = 0.002).
Conclusion: OFA significantly improved the quality of recovery in patients undergoing gynecological laparoscopy.
Keywords: opioid-free anesthesia, quality of recovery, laparoscopy, gynecology, opioids
Introduction
Opioids are commonly used for analgesia and supplementary sedation during general anesthesia and are the most widely used agents for the treatment of acute pain in the immediate postoperative period. Opioids provide effective analgesia and stable intraoperative hemodynamics, which are valuable during the perioperative period. However, the use of opioids during the perioperative period is risky. Opioids have many potential adverse effects, including respiratory depression, postoperative nausea and vomiting (PONV), and opioid-induced hyperalgesia (OIH).1 These complications are associated with delayed patient recovery, prolonged stay in the post-anesthetic care unit (PACU), delayed hospital discharge, and unexpected hospitalization, all contributing to an increased burden on patients and resources.2 Furthermore, the “opioid crisis” is already a serious problem in North America; fentanyl overdose is now the leading cause of death in Americans aged 18–45.3 The role of perioperative opioids is important in this regard, considering that 27.0% of chronic opioids start after surgery.4
Efforts have been made to minimize the use of opioids in light of the known adverse effects of opioids in the perioperative period.5 Opioid-free anesthesia (OFA) is an extreme form of this movement in which multimodal non-opioid analgesic techniques are used to eliminate the intraoperative use of opioids.6 OFA controls intraoperative hemodynamic stability and antinociception traditionally obtained by opioids using multimodal non-opioid agents such as α-2 agonists, local anesthetics, and N-methyl-d-aspartate (NMDA) receptor antagonists.7 OFA has demonstrated feasibility in various types of surgeries and patients.8 In two meta-analyses, patients receiving OFA had a lower incidence of PONV than those receiving opioid-based anesthesia but had similar postoperative pain scores.9,10 In another meta-analysis, OFA significantly reduced adverse postoperative events with significantly lower postoperative opioid consumption.11 However, the literature on OFA is still controversial because some studies that have not shown benefits12,13 or worse outcomes.14 Now, the question is which patients and types of surgery benefit the most from the application of OFA.
Gynecological laparoscopy may be a suitable type of surgery that can maximize the benefits of OFA. The degree of pain during gynecologic surgery is considered moderate, which requires IV opioids in the perioperative period.15 However, tolerance to pain can develop with intraoperative opioids, requiring more opioids during the acute postoperative period.16 Even with increased interest in postoperative pain control, many patients experience moderate to extreme pain during the immediate postoperative period, which continues after discharge.17 Furthermore, PONV, the most common adverse effect of opioids, makes the use of IV opioids more difficult. Two non-modifiable risk factors for PONV exist in this patient population: female sex and gynecological laparoscopy.2 Therefore, alternative approaches to intraoperative opioids, such as OFA, may have a beneficial effect on the quality of recovery.
Therefore, this study aimed to determine the effects of OFA using dexmedetomidine and lidocaine on the quality of recovery in patients undergoing gynecological laparoscopy. We hypothesized that patients receiving OFA would result in a better quality of recovery than those receiving conventional remifentanil-based anesthesia (RA). Furthermore, we assessed the feasibility of OFA for gynecological laparoscopy.
Materials and Methods
Study Design
This was a prospective, parallel-group, single-blind randomized controlled trial (RCT). The study protocol was approved by the Institutional Review Board (IRB) of Seoul St. Mary’s Hospital, the Catholic University of Korea (approval number: KC20MNSI0130) on April 7, 2020. The study was conducted following the Declaration of Helsinki and registered on ClinicalTrials.gov (NCT04409964) on May 28, 2020. Full details of the study protocol have been published previously.18 Written informed consent was obtained from all participating patients before inclusion in the study. The study is reported according to the Consolidated Standards of Reporting Trials (CONSORT) 2010 Statement and the CONSORT Patient-Reported Outcomes (CONSORT PRO) Extension.19
Study Participants
Patients aged 20–65 years who were scheduled for elective gynecological laparoscopy, including hysterectomy, oophorectomy, salpingectomy, cystectomy, cyst enucleation, and uterus myomectomy at Seoul St. Mary’s Hospital, the Catholic University of Korea, were considered eligible. Exclusion criteria were emergency surgery, cancer surgery, chronic pain requiring medication, history of psychiatric disease, hypotension, bradycardia, atrioventricular block, intraventricular or sinoatrial block, body mass index >35 kg/m2, known allergies, or history of adverse events to any of the drugs used for anesthesia, pregnancy, or lactation.
Randomization and Blinding
The enrolled patients were randomized in a 1:1 ratio to the study (OFA group) or the control (RA group). A research nurse generated a block randomization scheme using stratified block randomization with a fixed block size using a web-based random number generator (www.random.org). Once a patient has been enrolled, the medical staff opened an opaque, sequentially numbered envelope containing the group allocation.
Patients and surgeons were blinded to group allocation throughout the study period. The medical staff members providing postoperative care and assessing outcomes in the PACU and the ward were also unaware of the group allocation. The anesthesiologist performing general anesthesia could not be blinded due to the different drug administration protocols by groups. However, they did not participate in postoperative care or assessment of postoperative outcomes.
Intervention
The previously published trial protocol involved the standardization of anesthesia induction and maintenance according to the clinical practice guidelines of the Enhanced Recovery After Surgery Society recommendations.20 Before starting the study, the patients were instructed on how to assess their pain intensity using a visual analog scale (VAS; 0 cm, no pain and 10 cm, the worst pain imaginable) and how to use IV patient-controlled analgesia (PCA). To improve adherence to the protocol, they were asked to request analgesia without hesitation if the VAS pain score was >4.
None of the patients received premedication. Electrocardiography, noninvasive blood pressure measurements, pulse oximetry, neuromuscular monitoring using train-of-four (TOF) stimulation, bispectral index (BIS; A-2000TM SP, Aspect Medical Systems, Norwood, MA, USA) monitoring of anesthesia depth, and Surgical Pleth Index (SPI; General Electric Healthcare, Helsinki, Finland) measurements of nociception were performed in the operating room.
The OFA group received a loading dose of IV dexmedetomidine 0.7 μg/kg for 10 min before the induction of general anesthesia, followed by a continuous infusion of 0.5 μg/kg/h, which was adjusted in steps of 0.1 μg/kg/h to maintain SBP within ± 20% of baseline. Immediately after induction of anesthesia, a bolus dose of IV lidocaine 1.5 mg/kg was administered, followed by a continuous dose of 1.5 mg/kg/h. Dexmedetomidine and lidocaine infusions were stopped at the beginning of skin suturing.
The RA group received a continuous infusion of IV remifentanil targeting an effector site concentration of 3.5 ng/mL using a target-controlled infusion (Orchestra Base Primea, Fresenius Vial, Brezins, France) before the induction of general anesthesia. After induction of anesthesia, the remifentanil infusion was adjusted in increments of 0.5 ng/mL to maintain the SBP within ± 20% of the baseline. Remifentanil infusion was stopped at the end of the skin suturing.
Based on ideal body weight, all patients received a bolus dose of IV propofol 1.5–2 mg/kg for the induction of general anesthesia. After confirmation of unconsciousness (BIS value <60), absence of an eyelash reflex, and no response to verbal stimulation, a bolus dose of IV rocuronium 0.8 mg/kg was administered, and after zero TOF twitches were achieved, orotracheal intubation was performed using a direct laryngoscope. Ventilation was controlled mechanically and then adjusted to maintain an end-tidal carbon dioxide value between 25 and 40 mmHg throughout the surgery. Additional rocuronium was administered as needed. Anesthesia was maintained with 4–6% desflurane (expired concentration) in 40% air/oxygen (total flow, 4 L/min) to maintain a BIS value between 30 and 60. A bolus dose of IV ephedrine 4 mg was administered in cases with systolic blood pressure (SBP) <80 mmHg or mean arterial pressure (MAP) <60 mmHg. If the heart rate (HR) decreased below 45 bpm, a bolus dose of IV atropine 0.25 mg was administered.
Laparoscopy was performed under video guidance, with three punctures in the abdomen. Intraperitoneal pressure was maintained at approximately 12 mmHg. To prevent PONV, all patients received IV dexamethasone 5 mg at the beginning of surgery and IV palonosetron 75 μg at the end of surgery. For postoperative pain control, multimodal analgesia, consisting of IV acetaminophen 1g and IV ketorolac 30 mg, was administered 30 min before the end of surgery. These non-opioid analgesics continued throughout the hospital stay in the ward. After confirming self-respiration, the patients were extubated and transferred to the PACU. If the patient complained of pain (VAS score >4) in the PACU, IV fentanyl 0.5–1 μg/kg was administered immediately. Once the acute pain was under control, IV PCA (fentanyl 15 μg/kg in normal saline 100 mL; basal rate 0 mL/h; bolus 1 mL; lock-out time 10 min) was applied to all patients and no loading dose was administered. If the patient complained of nausea and/or vomiting, IV metoclopramide 10 mg was administered. The patients were discharged to the ward when their Aldrete score was ≥9.
Outcomes
Primary Outcome
The primary outcome was the quality of recovery on postoperative day (POD) 1 measured using the Quality of Recovery-40 (QoR-40) questionnaire scores. The QoR-40 questionnaire includes five dimensions of recovery: physical comfort (12 items), emotional state (9 items), physical independence (5 items), psychological support (7 items), and pain (7 items). Each item is scored on a 5-point Likert scale (none of the time, some of the time, usually, most of the time, and all of the time). The total score on QoR-40 ranges from 40 (poorest possible recovery) to 200 (best possible recovery), and a difference of 6.3 is deemed minimal clinically important.21 The QoR-40 interviews were conducted in person by a blinded investigator trained on the QoR-40 questionnaire, visiting all patients in the ward. All patients completed the questionnaire the day before surgery and POD 1.
Secondary outcomes
To determine whether OFA had the same effects as RA, such as hemodynamic stability and sedation, we obtained intraoperative hemodynamic data (SBP, MAP, and HR), anesthetic depth (BIS), and nociception severity (SPI) data, at baseline, before intubation (at the time of unconsciousness), immediately after intubation, at the time of the incision, at the end of the surgery, and immediately after tracheal extubation. Furthermore, to assess intraoperative complications, episodes of bradycardia (<45 bpm) in association with the administration of atropine, and hypotension (SBP <80 mmHg or MAP <60 mmHg) were recorded.
Pain severity was assessed using the VAS score upon arrival at the PACU and every 15 min thereafter. Additionally, the level of sedation (awake/sedated and responsive to verbal stimuli/sedated and unresponsive to verbal stimuli), the incidence of PONV and shivering, the need for analgesics and antiemetics, and the duration of stay in the PACU were assessed. These outcomes were evaluated again 24 h after surgery. In addition, the time to the first flatus or defecation was recorded.
To assess the effect of OFA on attenuating stress response, an ancillary stress hormone study was performed on 50 enrolled patients (25 in each group). Two stress hormones (epinephrine and norepinephrine) were measured at baseline, immediately after tracheal intubation, at the time of incision, immediately after tracheal extubation, and 24 h after surgery. All blood samples were placed in tubes and centrifuged within 1 h, and plasma was separated and stored at −70°C until analysis.
Sample Size
The primary outcome was the QoR-40 score on POD 1. Based on a previous study that reported a 13-point difference in QoR-40 scores between different anesthetic techniques,22 a sample size of 34 was calculated to be necessary to achieve a power of 80% with a type I error of 0.05. An additional 15% of the participants were included to account for possible loss to follow-up. Therefore, the final sample size was 78 participants (39 in each group).
Statistical Analysis
A researcher blinded to the group allocation performed the statistical analysis of all randomized patients (intention-to-treat analysis). The Kolmogorov–Smirnov test was used to check the normality of the distribution of the quantitative variables. Independent-sample t-test or Mann–Whitney U-test was used to analyze the quantitative variables, including the primary outcome (QoR-40). Chi-square or Fisher’s exact test was used to analyze the qualitative variables. Continuous endpoints repeatedly measured during the study period were analyzed using repeated-measures two-way analysis of variance. As a sensitivity analysis, analysis of covariance (ANCOVA) was performed after controlling for preoperative QoR-40 scores. Values are expressed as mean ± standard deviation, median (IQR), or number of patients (percentage). Statistical significance was set at p < 0.05. Statistical analyses were performed with SPSS (version 18.0; IBM SPSS Inc., Chicago, IL, USA).
Results
Patients
Of the 137 patients screened from June 2020 to September 2021, 78 patients underwent randomization, and three patients (one in the RA group and two in the OFA group) did not receive the allocated intervention due to conversion to laparotomy during surgery. Therefore, a total of 75 patients (38 in the RA group and 37 in the OFA group) were included in the analysis (Figure 1).
 |
Figure 1 Consolidated standards of reporting trials (CONSORT) flowchart of the study. |
The baseline characteristics of the patients are shown in Table 1. The incidence of risk factors for PONV according to the Apfel simplified risk score was similar between the two groups (non-smoking: 89.5% in the RA group vs 94.6% in the OFA group, p = 0.674; history of PONV or motion sickness: 52.6% in the RA group vs 43.2% in the OFA group, p = 0.560). There was no difference between the two groups in the type of surgery the patients received (p = 0.325).
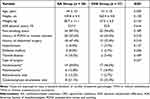 |
Table 1 Characteristics of the Patients at Baseline |
Primary Outcome
All patients completed the QoR-40 questionnaire without difficulty. The baseline QoR-40 score was not different between the two groups (180.6 ± 15.6 in the RA group vs 182.6 ± 14.8 in the OFA group; mean difference: −2.0, 95% confidence interval [CI]: −9.0, 5.0; p = 0.573; Table 2). However, the primary outcome of the study, the QoR-40 score on POD 1, was significantly higher in the OFA group than in the RA group (155.9 ± 21.2 in the RA group vs 166.9 ± 17.8 in the OFA group; mean difference: −11.0, 95% CI: −20.0, −2.0; p = 0.018). Comparison of the five domains of the QoR-40 questionnaire on POD 1 showed that the OFA group scored higher in physical comfort (45.8 ± 7.1 in the RA group vs 49.6 ± 5.4 in the OFA group; mean difference: −3.8, 95% CI: −6.7, −0.9; p = 0.011) and pain (31.2 ± 3.5 in the RA group vs 33.2 ± 2.0 in the OFA group; mean difference: −2.0, 95% CI: −3.3, −0.7; p = 0.004) compared to the RA group (Table 2).
 |
Table 2 Primary Outcome Analysis |
Secondary Outcomes
Anesthesia and Recovery Characteristics
A comparison of anesthesia and recovery characteristics between the two groups is presented in Table 3. The duration of anesthesia (154.0 ± 55.6 min in the RA group vs 138.4 ± 33.4 min in the OFA group, p = 0.145), time to eye-opening (5.1 ± 1.8 min in the RA group versus 5.4 ± 1.7 min in the OFA group, p = 0.485), and extubation (5.8 ± 2.1 min in the RA group vs 5.7 ± 1.7 min in the OFA group, p = 0.763) were similar in the two groups. Intraoperative hemodynamics (SBP, MAP, and HR), BIS and SPI values were maintained within the intended range (Figure 2). The level of sedation in the PACU did not differ between the two groups (p = 0.392), and the duration of stay in the PACU was significantly shorter in the OFA group (39.6 ± 5.6 min in the RA group vs 33.9 ± 5.6 min in the OFA group, p < 0.001).
 |
Table 3 Anesthesia and Recovery Characteristics |
Adverse Events
A comparison of adverse events between the two groups is presented in Table 4. Regarding intraoperative complications, the incidence of hypotension was significantly lower in the OFA group than in the RA group (50.0% in the RA group vs 24.3% in the OFA group, p = 0.039), but the incidence of bradycardia was similar in the two groups (15.8% in the RA group vs 2.7% in the OFA group, p = 0.108). VAS score at 30 min after surgery was significantly lower in the OFA group (6.3 ± 2.3 in the RA group vs 4.1 ± 2.1 in the OFA group, p < 0.001), and the incidence of patients that requiring rescue analgesics in the PACU was significantly lower in the OFA group (73.7% in the RA group vs 21.6% in the OFA group, p < 0.001). The incidences of nausea (23.7% in the RA group vs 2.7% in the OFA group, p = 0.014) and shivering (15.8% in the RA group vs 0% in the OFA group, p = 0.025) in the PACU were also significantly lower in the OFA group.
 |
Table 4 Adverse Events |
However, some of the differences in secondary outcomes did not last beyond 24 h after surgery (Table 4). The VAS score at 24 h after surgery was similar in the two groups (3.4 ± 1.9 in the RA group vs 3.4 ± 1.8 in the OFA group, p = 0.872), and the incidence of patients who needed rescue analgesics was also similar (81.6% in the RA group vs 73.0% in the OFA group, p = 0.539). The incidences of nausea and shivering were similar in the two groups. The time to first flatus or defecation was similar in the two groups (20.0 ± 5.2 h in the RA group vs 22.7 ± 6.8 h in the OFA group, p = 0.058).
Ancillary Stress Hormone
The ancillary stress hormone study in 50 patients revealed that the levels of epinephrine were significantly lower in the OFA group than in the RA group (p = 0.002; Figure 3). The pairwise comparison revealed that the level of epinephrine was significantly lower in the OFA group immediately after tracheal intubation (16.43 ± 9.63 pg/mL in the RA group vs 8.60 ± 3.09 pg/mL in the OFA group; p = 0.001), at the time of incision (15.61 ± 8.29 pg/mL in the RA group vs 8.83 ± 3.06 pg/mL in the OFA group; p = 0.001), and immediately after tracheal extubation (13.34 ± 5.48 pg/mL in the RA group vs 7.49 ± 3.03 pg/mL in the OFA group; p < 0.001). The levels of norepinephrine were similar between the two groups (p = 0.088; Figure 3).
Sensitivity Analysis
An ANCOVA was performed to determine the effect of OFA on POD 1 QoR-40 scores after controlling for the preoperative QoR-40 scores. After adjustment for preoperative QoR-40 scores, there was a statistically significant difference in QoR-40 scores on POD 1 between the two groups (p = 0.021).
Discussion
The present study aimed to evaluate the effect of OFA using dexmedetomidine and lidocaine on the quality of recovery in patients undergoing gynecological laparoscopy. Our findings suggest that patients who receive OFA have a better quality of recovery than those who receive opioid-based anesthesia with remifentanil. Furthermore, fewer intraoperative hypotension, and well-maintained hemodynamics and anesthetic parameters confirm that OFA is a safe and feasible technique in gynecological laparoscopy. Patients receiving OFA experienced less pain, and fewer incidences of PONV and shivering than those receiving RA in the PACU. The duration of stay in the PACU was shorter in patients who received OFA. Furthermore, patients receiving OFA showed less stress response to surgery than those receiving RA.
Although OFA has been validated and considered feasible in various types of surgery, there is still controversy about the choice of agents.1 In our study, IV dexmedetomidine and lidocaine were used as alternatives to remifentanil. Dexmedetomidine is a potent α-2 agonist with sedative, analgesic, anti-shivering, and anesthetic sparing effects. Lidocaine has been widely used intraoperatively due to its sympatholytic and analgesic effects. Generally, low-dose IV lidocaine does not cause adverse effects and is considered a safe component of intraoperative analgesia.23 OFA with dexmedetomidine and lidocaine has been successfully used in gastric,24,25 hepatobiliary,26–28 breast,29 cardiac,30 thoracic,31,32 orthopedic,33,34 and spine surgery35,36 with a reduction in postoperative pain intensity and opioid consumption, and a lower rate of postoperative complications. Considering these studies and our results, OFA with dexmedetomidine and lidocaine could benefit the general population.
However, in a recent multicenter RCT comparing opioid-based anesthesia and OFA with dexmedetomidine in patients undergoing major or intermediate surgery, OFA resulted in a greater incidence of postoperative serious adverse events than opioid-based anesthesia, and the study was terminated early due to five cases of severe bradycardia in the OFA group. Additionally, patients receiving OFA had more postoperative hypoxemia, delayed extubation, prolonged stay in the PACU, and intraoperative bradycardia. On the other hand, OFA was associated with less morphine consumption and a lower incidence of PONV, which was similar to the findings to our study.14 The high incidence of serious adverse events may have been due to higher doses of dexmedetomidine (mean dose 1.2 ± 2 μg/kg/h) than in our study (mean dose 0.63 ± 0.28 μg/kg/h).
Previous reports on OFA in gynecological surgery have shown conflicting results due to heterogeneity in terms of the OFA protocol, patient selection, and outcome. In a prospective RCT in patients undergoing elective gynecological laparoscopy, OFA with dexmedetomidine and esketamine was compared with opioid-based anesthesia with sufentanil. Contrary to the findings of our study, the incidence and severity of PONV, pain scores, and morphine consumption were equivalent in both groups.12 The reason may be due to different drug administration protocols using esketamine, and different patient populations, where the proportion of patients with risk factors for PONV was higher than in our study. In a retrospective study of patients undergoing laparoscopic hysterectomy, OFA with clonidine and ketamine was associated with less perioperative morphine equivalent use than opioid-based anesthesia with sufentanil, but with similar pain scores and incidence of PONV.37 However, the definitions and anesthetic protocols used in this study were not standardized.
The primary outcome of our study was the quality of recovery assessed using the QoR-40 questionnaire. The QoR-40 questionnaire is a global measure of the quality of recovery that incorporates five dimensions of health: physical comfort, emotional state, physical independence, psychological support, and pain.38 Generally, a 10-point difference equates to a 15% improvement in the quality of recovery.38 The validity and reliability of QoR-40 have been confirmed in previous studies, and it has been used to investigate recovery after various anesthetic and surgical techniques.39,40 The QoR-40 questionnaire is recommended by the Standardized Endpoints in Perioperative Medicine initiative as a measure of patient comfort.41 According to a study comparing OFA and opioid-based anesthesia in patients undergoing laparoscopic sleeve gastrectomy, patients receiving OFA scored higher QoR-40 scores than those receiving opioid-based anesthesia,24 which was also demonstrated in our study. Given the evidence that OFA has been feasible in different types of surgery, it will be meaningful to test the effect of OFA on the quality of recovery in other types of surgery.
The two domains that showed significant differences in our study were pain and physical comfort. Short-acting opioids, such as remifentanil, are associated with acute tolerance to opioids and/or OIH.16 Remifentanil has been reported to stimulate the overproduction of proinflammatory cytokines and reactive oxygen species, triggering the activation of neuronal NMDA receptors, which are important factors in the development of OIH.42–44 Furthermore, remifentanil induces excessive activity of matrix metalloproteinase-9, which in turn mediates extracellular matrix abnormalities, resulting in various neuropathological conditions, including OIH.45–47 In a meta-analysis of 27 studies involving 1494 patients, patients treated with high intraoperative doses of opioids reported higher postoperative pain intensity and morphine use after 24 h than those treated with lower doses.48 In our study, the presence of OIH after RA was demonstrated in the VAS score at 30 min after surgery and the incidence of patients who require rescue analgesics was higher in patients receiving RA than in those receiving OFA.
Differences in physical comfort are most likely due to PONV and shivering. Postoperative opioid use is one of the four risk factors for PONV in the Apfel simplified risk score,49 and the use of intraoperative and/or postoperative opioids is associated with PONV in a dose-dependent manner.2 Furthermore, since female patients undergoing gynecological laparoscopy constitute a large number of well-known risk factors for PONV, the incidence of PONV was expected to be high in the patients who participated in our study.2 Postoperative shivering is proposed to be a sign of adrenergic activation associated with acute opioid withdrawal.50 In our study, the OFA protocol may have contributed to a lower incidence of PONV and shivering due to the direct effect of eliminating intraoperative opioids, the reduction in postoperative opioid consumption, and the antiemetic effect of dexmedetomidine.50–52
Surgery elicits a systemic reaction encompassing a wide range of endocrinological, immunological, and hematological effects, namely, the stress response. Epinephrine and norepinephrine are classic markers of a stress response during anesthesia.53,54 It is well-known that inhibition of the stress response to surgery can affect postoperative outcomes by beneficial effects on organ function.20,53 Although the underlying mechanism is poorly understood, dexmedetomidine has been reported to reduce inflammatory and stress responses, possibly by attenuating cytokine production, inhibiting apoptosis, and central sympatholytic effects.54,55 It not only reduces surgical stress similar to remifentanil but also alleviates neuroinflammation. Similar to dexmedetomidine, lidocaine has been reported to decrease the levels of inflammatory cytokines.56 In our study, the beneficial effect of OFA on stress response was demonstrated through reduced levels of epinephrine.
Our study has several limitations. First, this was a single-blind study in which the anesthesiologist participating in the intraoperative management of the patients was open to group allocation. The two groups had different infusion protocols, which made it impossible for the anesthesiologist to be blinded. However, all other personnel involved in the study, especially the outcome assessor, were blinded to the group allocation. Second, there has been a lack of validated depth of anesthesia and nociception monitors during OFA. In our study, the BIS values were measured to assess the depth of anesthesia, and the SPI values were measured to monitor the severity of nociception. The BIS value has been validated during sedation with dexmedetomidine.57 The SPI value has been widely used for several years and has been reported to be more valid than other nociceptive monitors, such as the pupillary pain index and nociception level (NoL).58,59 As expected, the BIS and SPI values of patients receiving OFA were within acceptable ranges. Third, the follow-up period was only until the first day after surgery. The QoR-40 scores on the day later than the first day after surgery may have been different, considering that pain-related outcomes and adverse effects were not different between the two groups at 24 h after surgery. Future research is needed to determine whether eliminating opioids in the postoperative period, that is, opioid-free analgesia can extend the beneficial effect of OFA beyond the immediate postoperative period.
Conclusion
In conclusion, in patients undergoing gynecological laparoscopy, patients receiving OFA with dexmedetomidine and lidocaine had a better quality of recovery on POD 1 than those receiving opioid-based anesthesia with remifentanil. Physical comfort and pain were the domains that scored higher in patients receiving OFA. In future clinical trials, the focus should be on finding the most effective OFA protocol in terms of efficacy and cost, and which patients and types of surgery OFA will benefit the most.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study protocol was approved by the Institutional Review Board (IRB) of Seoul St. Mary’s Hospital, the Catholic University of Korea (approval number: KC20MNSI0130) on April 7, 2020. Written informed consent was obtained from all participants.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT; No. 2020R1G1A1008405). The funder played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shanthanna H, Ladha KS, Kehlet H, Joshi GP. Perioperative opioid administration. Anesthesiology. 2021;134(4):645–659. doi:10.1097/aln.0000000000003572
2. Gan TJ, Belani KG, Bergese S, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2020;131(2):411–448. doi:10.1213/ane.0000000000004833
3. Wide-ranging online data for epidemiologic research (WONDER). CDC, National Center for Health Statistics. Available from: http://wonder.cdc.gov.
4. Callinan CE, Neuman MD, Lacy KE, Gabison C, Ashburn MA. The initiation of chronic opioids: a survey of chronic pain patients. J Pain. 2017;18(4):360–365. doi:10.1016/j.jpain.2016.11.001
5. Wu CL, King AB, Geiger TM, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on perioperative opioid minimization in opioid-naïve patients. Anesth Analg. 2019;129(2):567–577. doi:10.1213/ane.0000000000004194
6. Bugada D, Lorini LF, Lavand’homme P. Opioid free anesthesia: evidence for short and long-term outcome. Minerva Anestesiol. 2021;87(2):230–237. doi:10.23736/s0375-9393.20.14515-2
7. Chia PA, Cannesson M, Bui CCM. Opioid free anesthesia: feasible? Curr Opin Anaesthesiol. 2020;33(4):512–517. doi:10.1097/aco.0000000000000878
8. Lavand’homme P, Estebe JP. Opioid-free anesthesia: a different regard to anesthesia practice. Curr Opin Anaesthesiol. 2018;31(5):556–561. doi:10.1097/aco.0000000000000632
9. Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):651–662. doi:10.1111/anae.14582
10. Salomé A, Harkouk H, Fletcher D, Martinez V. Opioid-free anesthesia benefit-risk balance: a systematic review and meta-analysis of randomized controlled trials. J Clin Med. 2021;10(10):2069. doi:10.3390/jcm10102069
11. Olausson A, Svensson CJ, Andréll P, Jildenstål P, Thörn SE, Wolf A. Total opioid-free general anaesthesia can improve postoperative outcomes after surgery, without evidence of adverse effects on patient safety and pain management: a systematic review and meta-analysis. Acta Anaesthesiol Scand. 2022;66(2):170–185. doi:10.1111/aas.13994
12. Massoth C, Schwellenbach J, Saadat-Gilani K, et al. Impact of opioid-free anaesthesia on postoperative nausea, vomiting and pain after gynaecological laparoscopy - A randomised controlled trial. J Clin Anesth. 2021;75:110437. doi:10.1016/j.jclinane.2021.110437
13. An G, Zhang Y, Chen N, Fu J, Zhao B, Zhao X. Opioid-free anesthesia compared to opioid anesthesia for lung cancer patients undergoing video-assisted thoracoscopic surgery: a randomized controlled study. PLoS One. 2021;16(9):e0257279. doi:10.1371/journal.pone.0257279
14. Beloeil H, Garot M, Lebuffe G, et al. Balanced opioid-free anesthesia with dexmedetomidine versus balanced anesthesia with remifentanil for major or intermediate noncardiac surgery. Anesthesiology. 2021;134(4):541–551. doi:10.1097/aln.0000000000003725
15. Gerbershagen HJ, Aduckathil S, Van Wijck AJM, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery. Anesthesiology. 2013;118(4):934–944. doi:10.1097/aln.0b013e31828866b3
16. Yu EH, Tran DH, Lam SW, Irwin MG. Remifentanil tolerance and hyperalgesia: short-term gain, long-term pain? Anaesthesia. 2016;71(11):1347–1362. doi:10.1111/anae.13602
17. Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 2014;30(1):149–160. doi:10.1185/03007995.2013.860019
18. Song JY, Choi H, Chae M, Ko J, Moon YE. The effect of opioid-free anesthesia on the quality of recovery after gynecological laparoscopy: study protocol for a prospective randomized controlled trial. Trials. 2021;22(1):207. doi:10.1186/s13063-021-05166-z
19. Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA. 2013;309(8):814–822. doi:10.1001/jama.2013.879
20. Nelson G, Bakkum-Gamez J, Kalogera E, et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS) Society recommendations-2019 update. Int J Gynecol Cancer. 2019;29(4):651–668. doi:10.1136/ijgc-2019-000356
21. Myles PS, Myles DB, Galagher W, Chew C, Macdonald N, Dennis A. Minimal clinically important difference for three quality of recovery scales. Anesthesiology. 2016;125(1):39–45. doi:10.1097/aln.0000000000001158
22. Lee WK, Kim MS, Kang SW, Kim S, Lee JR. Type of anaesthesia and patient quality of recovery: a randomized trial comparing propofol-remifentanil total i.v. anaesthesia with desflurane anaesthesia. Br J Anaesth. 2015;114(4):663–668. doi:10.1093/bja/aeu405
23. Estebe JP. Intravenous lidocaine. Best Pract Res Clin Anaesthesiol. 2017;31(4):513–521. doi:10.1016/j.bpa.2017.05.005
24. Ibrahim M, Elnabtity AM, Hegab A, Alnujaidi OA, El Sanea O. Combined opioid free and loco-regional anaesthesia enhances the quality of recovery in sleeve gastrectomy done under ERAS protocol: a randomized controlled trial. BMC Anesthesiol. 2022;22(1):29. doi:10.1186/s12871-021-01561-w
25. Ziemann-Gimmel P, Goldfarb AA, Koppman J, Marema RT. Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth. 2014;112(5):906–911. doi:10.1093/bja/aet551
26. Hublet S, Galland M, Navez J, et al. Opioid-free versus opioid-based anesthesia in pancreatic surgery. BMC Anesthesiol. 2022;22(1):9. doi:10.1186/s12871-021-01551-y
27. Toleska M, Dimitrovski A. Is opioid-free general anesthesia more superior for postoperative pain versus opioid general anesthesia in laparoscopic cholecystectomy? Pril. 2019;40(2):81–87. doi:10.2478/prilozi-2019-0018
28. Bakan M, Umutoglu T, Topuz U, et al. Opioid-free total intravenous anesthesia with propofol, dexmedetomidine and lidocaine infusions for laparoscopic cholecystectomy: a prospective, randomized, double-blinded study. Braz J Anesthesiol. 2015;65(3):191–199. doi:10.1016/j.bjane.2014.05.001
29. King CA, Perez-Alvarez IM, Bartholomew AJ, et al. Opioid-free anesthesia for patients undergoing mastectomy: a matched comparison. Breast J. 2020;26(9):1742–1747. doi:10.1111/tbj.13999
30. Aguerreche C, Cadier G, Beurton A, et al. Feasibility and postoperative opioid sparing effect of an opioid-free anaesthesia in adult cardiac surgery: a retrospective study. BMC Anesthesiol. 2021;21(1):166. doi:10.1186/s12871-021-01362-1
31. Selim J, Jarlier X, Clavier T, et al. Impact of opioid-free anesthesia after video-assisted thoracic surgery: a propensity score study. Ann Thorac Surg. 2021;114:218–224. doi:10.1016/j.athoracsur.2021.09.014
32. Devine G, Cheng M, Martinez G, et al. Opioid-free anesthesia for lung cancer resection: a case-control study. J Cardiothorac Vasc Anesth. 2020;34(11):3036–3040. doi:10.1053/j.jvca.2020.05.022
33. Urvoy B, Aveline C, Belot N, Catier C, Beloeil H. Opioid-free anaesthesia for anterior total Hip replacement under general anaesthesia: the observational prospective study of opiate-free anesthesia for anterior total hip replacement trial. Br J Anaesth. 2021;126(4):e136–e139. doi:10.1016/j.bja.2021.01.001
34. Leas DP, Connor PM, Schiffern SC, D’Alessandro DF, Roberts KM, Hamid N. Opioid-free shoulder arthroplasty: a prospective study of a novel clinical care pathway. J Shoulder Elbow Surg. 2019;28(9):1716–1722. doi:10.1016/j.jse.2019.01.013
35. Soffin EM, Wetmore DS, Beckman JD, et al. Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: a retrospective matched cohort study. Neurosurg Focus. 2019;46(4):E8. doi:10.3171/2019.1.Focus18645
36. Hwang W, Lee J, Park J, Joo J. Dexmedetomidine versus remifentanil in postoperative pain control after spinal surgery: a randomized controlled study. BMC Anesthesiol. 2015;15(1):21. doi:10.1186/s12871-015-0004-1
37. Forget P, De Kock M, Lovqvist L, Lois F. Is intraoperative opioids avoidance A utopia? A matched study in laparoscopic hysterectomy. Curr Rev Clin Exp Pharmacol. 2021;16(1):103–108. doi:10.2174/1574884715666200302122707
38. Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth. 2000;84(1):11–15. doi:10.1093/oxfordjournals.bja.a013366
39. Lee JH, Kim D, Seo D, Son JS, Kim DC. Validity and reliability of the korean version of the quality of recovery-40 questionnaire. Korean J Anesthesiol. 2018;71(6):467–475. doi:10.4097/kja.d.18.27188
40. Léger M, Campfort M, Cayla C, Lasocki S, Rineau E. Postoperative quality of recovery measurements as endpoints in comparative anaesthesia studies: a systematic review. Br J Anaesth. 2021;126(6):e210–e212. doi:10.1016/j.bja.2021.03.008
41. Myles PS, Boney O, Botti M, et al. Systematic review and consensus definitions for the Standardised Endpoints in Perioperative Medicine (StEP) initiative: patient comfort. Br J Anaesth. 2018;120(4):705–711. doi:10.1016/j.bja.2017.12.037
42. Shu RC, Zhang LL, Wang CY, et al. Spinal peroxynitrite contributes to remifentanil-induced postoperative hyperalgesia via enhancement of divalent metal transporter 1 without iron-responsive element-mediated iron accumulation in rats. Anesthesiology. 2015;122(4):908–920. doi:10.1097/aln.0000000000000562
43. Ye L, Xiao L, Yang SY, et al. Cathepsin S in the spinal microglia contributes to remifentanil-induced hyperalgesia in rats. Neuroscience. 2017;344:265–275. doi:10.1016/j.neuroscience.2016.12.030
44. Lv CC, Xia ML, Shu SJ, Chen F, Jiang LS. Attenuation of remifentanil-induced hyperalgesia by betulinic acid associates with inhibiting oxidative stress and inflammation in spinal dorsal horn. Pharmacology. 2018;102(5–6):300–306. doi:10.1159/000493144
45. Parks WC, Wilson CL, López-Boado YS. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol. 2004;4(8):617–629. doi:10.1038/nri1418
46. Kawasaki Y, Xu ZZ, Wang X, et al. Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nat Med. 2008;14(3):331–336. doi:10.1038/nm1723
47. Zhang H, Adwanikar H, Werb Z, Noble-Haeusslein LJ. Matrix metalloproteinases and neurotrauma: evolving roles in injury and reparative processes. Neuroscientist. 2010;16(2):156–170. doi:10.1177/1073858409355830
48. Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112(6):991–1004. doi:10.1093/bja/aeu137
49. Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. doi:10.1097/00000542-199909000-00022
50. Hoshijima H, Takeuchi R, Kuratani N, et al. Incidence of postoperative shivering comparing remifentanil with other opioids: a meta-analysis. J Clin Anesth. 2016;32:300–312. doi:10.1016/j.jclinane.2015.08.017
51. Grape S, Kirkham KR, Frauenknecht J, Albrecht E. Intra‐operative analgesia with remifentanil vs. dexmedetomidine: a systematic review and meta‐analysis with trial sequential analysis. Anaesthesia. 2019;74(6):793–800. doi:10.1111/anae.14657
52. Nakasuji M, Nakamura M, Imanaka N, Tanaka M, Nomura M, Suh SH. Intraoperative high-dose remifentanil increases post-anaesthetic shivering. Br J Anaesth. 2010;105(2):162–167. doi:10.1093/bja/aeq121
53. Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–117. doi:10.1093/bja/85.1.109
54. Li Y, Wang B, Zhang LL, et al. Dexmedetomidine combined with general anesthesia provides similar intraoperative stress response reduction when compared with a combined general and epidural anesthetic technique. Anesth Analg. 2016;122(4):1202–1210. doi:10.1213/ane.0000000000001165
55. Kang SH, Kim YS, Hong TH, et al. Effects of dexmedetomidine on inflammatory responses in patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2013;57(4):480–487. doi:10.1111/aas.12039
56. Weibel S, Jokinen J, Pace NL, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016;116(6):770–783. doi:10.1093/bja/aew101
57. Ki S, Lee D, Lee W, Cho K, Han Y, Lee J. Verification of the performance of the bispectral index as a hypnotic depth indicator during dexmedetomidine sedation. Anesth Pain Med. 2021;17:44–51. doi:10.17085/apm.21065
58. Ledowski T. Objective monitoring of nociception: a review of current commercial solutions. Br J Anaesth. 2019;123(2):e312–e321. doi:10.1016/j.bja.2019.03.024
59. Funcke S, Pinnschmidt HO, Wesseler S, et al. Guiding opioid administration by 3 different analgesia nociception monitoring indices during general anesthesia alters intraoperative sufentanil consumption and stress hormone release: a randomized controlled pilot study. Anesth Analg. 2020;130(5):1264–1273. doi:10.1213/ane.0000000000004388
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


